The COVID-19 Public Health Emergency caused a rapid escalation of telehealth services accompanied by loosening of telehealth restrictions by governmental and regulatory oversight offices [1, 2]. The rapid escalation required a swift response from health-care providers and systems to enact operational changes to provide safe, effective care. Obstetrical patients with pregnancies complicated by a fetal anomaly require multidisciplinary subspecialty consultation and follow-up. Our Neonatology group rapidly instituted telemedicine synchronous video visits to provide effective outpatient neonatology prenatal consultation at the UPMC (University of Pittsburgh Medical Center) Center for Advanced Fetal Diagnostics (CAFD), which provides care to an average of 250 patients with complex fetal conditions per year.
Rapid implementation of the neonatology perinatal consult telehealth service was directed by a team consisting of an IT representative, a lead physician with expertise in telehealth, an administrative assistant, and clinic staff. We already had a HIPPA-secure platform through Epic® (Verona, Wisconsin, USA) in place, and the team worked to provide access and direction on use to providers. A process guide for real-time, synchronous video visits and billing guidance was created for the physicians. Patient familiarization with telemedicine visits varied, so instruction documents were sent prior to the visit and contact was made by clinic staff to ensure patient access and ability to participate in the visit. If a patient was unable to access the platform, then a telephone visit was scheduled.
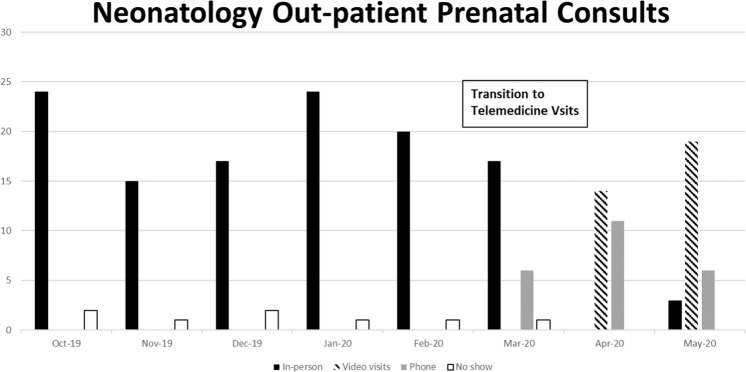
In our experience, barriers to effective consultation fell into two categories: providing a secure, reliable tele-connection and creating a therapeutic relationship in the digital environment. Poor connection leading to loss of communication frustrated patients and providers. Some encounters had to transition from a video visit to an audio-only visit due to patient technical issues, lack of internet access or proper smart device, but no telehealth visits were unable to be completed due to technical issues. At times, providers found completing the complex and nuanced conversations required by these consults difficult. However, multiple patients gave unsolicited positive feedback noting the convenience of having appointments from home, the ability for more family members to attend, and the advantage of not having to find childcare or pay for travel. Other encouraging observations of our process implementation included a 100% show rate for Neonatology prenatal consults (Fig. 1), increased access for patients, decreased time and travel burden for patients, and increased use of synchronous video visits as users became more familiar with the technology.
Fig. 1. Neonatology outpatient consults from October 2019 to May 2020 stratified by visit type.
Distribution of number of In-person visits (solid black shading), Video visits (hatched shading), Telephone only visits (solid gray shading), and No-show visits (solid white shading) per month before the COVID-19 Pandemic (Oct 19–Feb 20) and during the beginning of the COVID-19 Pandemic (Mar 20–May 20).
Barriers such as technology and maintaining quality will continue to require attention, and the potential for loss of reimbursement and ability for patients to participate in consults from home are threats to telehealth program sustainability if previous rules from CMS and the state are reinstated after the COVID-19 PHE. These threats highlight the importance of telemedicine advocacy. We will continue to study the outcomes of the program to ensure that high-quality care is provided and advocate for telemedicine during and after the COVID-19 PHE.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.HHS, Health Resources and Services Administration (HRSA). Telehealth programs. https://www.hrsa.gov/rural-health/telehealth/index.html. Accessed May 2020.
- 2.Office for Civil Rights (OCR): HIPAA, Civil Rights, and COVID-19. HHS.gov 2020. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Accessed May 9, 2020.