Abstract
Recently, the research on pain-related disability has increasingly paid attention to the psychological and social factors that may influence the biological condition. In the current study, we aimed to explore attachment styles, self-esteem, and quality of life in individuals with a diagnosis of fibromyalgia. Participants were 371 diagnosed women, with a mean age of 42.7 years (standard deviation = 10.6). The average number of years since diagnosis was 7.4 years (standard deviation = 2.4) years. To assess attachment, quality of life, and self-esteem, women responded, respectively, to the Relationship Questionnaire, the World Health Organization Quality of Life Questionnaire, and the Rosenberg Self-Esteem Inventory. Our results showed that secure attachment relationships and high self-esteem represent protective factors for quality of life of women with fibromyalgia, while the contrary emerged for insecure attachments and low self-esteem. The understanding of the psychological components that contribute to fibromyalgia may improve the effectiveness of interventions.
Keywords: attachment styles, chronic pain, fibromyalgia, quality of life, self-esteem, women
Fibromyalgia (FM) is a chronic widespread pain disorder that predominantly affects women (Legand et al., 2019; Rudin, 2019; Tavares et al., 2020). Due to the musculoskeletal pain, FM can result in quality of life (QoL) deterioration and impairment (Walker and Littlejohn, 2006). Indeed, this rheumatic illness is characterized by not only fatigue and pain but also difficulties with daily living movements, going from basic tasks to more complex responsibilities such as work and social relationships (Verbrugge and Juarez, 2006).
Previous studies on the consequences of rheumatic disorders emphasized the medical and biological perspective (Walker and Littlejohn, 2006). However, more recently, researchers tried to recognize the roles of social, demographic, physiological, and psychological factors with respect to chronic physical illness (Verbrugge and Juarez, 2006). In this regard, the World Health Organization (WHO) supported the International Classification of Functioning (ICF), incorporating a more complete bio-psycho-social framework of disability, health, and health-related conditions (WHO). Consequently, the ICF takes a neutral position about etiology and permits scholars to achieve causal inferences through suitable scientific methods, trying to remove conventions that biological dysfunction is the critical viewpoint of QoL (Cieza et al., 2004).
This approach is determinant since FM’s etiology and development are still unidentified, and high comorbidity and heterogeneity increase difficulties in studying FM (Chamie, 1995; Su et al., 2015).
Undeniably, FM is a complex bio-psycho-social condition influenced by several psychological aspects, such as fear relating to pain, beliefs about pain, self-esteem, anxiety, depression, lack of social support, affect differentiation, resilience, coping strategies, and emotion regulation (Dima et al., 2013; Tunks et al., 2008), that may even result in an increased risk for suicidality (Amir et al., 2000; Dreyer et al., 2010), a cross-cutting concern of mental problems (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM 5), American Psychiatric Association (APA), 2013).
Thus, to mitigate the negative consequences of FM on the person’s functioning, it is crucial to acknowledge the psychological factors that may be implicated.
Adult attachment styles
Empirical studies suggest that adult attachment styles are linked to pain-related disabilities (MacDonald and Kingsbury, 2006; Meredith et al., 2006).
Attachment investigators have recognized four attachment styles that differ along two dimensions: attachment anxiety (degree to which individuals worry about being unvalued or rejected by significant others) and attachment avoidance (the degree to which persons are at ease with affective closeness in significant relationships). Securely attached individuals are low on both dimensions, preoccupied individuals are high in anxiety and low in avoidance, dismissing persons are high in avoidance but low in anxiety, and fearful persons are high on both (Collins and Read, 1990). Moreover, secure persons have a positive model of both self and others; those with a fearful attachment have a negative image of both self and others. Preoccupied persons have a negative image of self and a positive image of others, and those with a dismissive attachment have a positive image of self and a negative image of others (Bartholomew and Horowitz, 1991; Griffin and Bartholomew, 1994).
It has been proved that about 65 percent of people in normative samples are securely attached, whereas 35 percent are insecurely attached (Mickelson et al., 1997); in chronic pain patients, these percentages seem to be reversed (Kowal et al., 2015; Meredith, 2016).
Some studies showed that attachment anxiety is related to a negative perception of one’s pain-coping capacity, lower somatic pain levels, and decreased experiences of control over pain (Sullivan et al., 2001). Individuals with anxious or avoidant attachment have been found to report greater levels of negative pain beliefs (McWilliams and Asmundson, 2007). Also, other studies showed that chronic insecurely attached pain patients reported significantly higher levels of pain intensity as well as pain-related suffering and less pain self-efficacy than chronic securely attached pain patients (MacDonald and Kingsbury, 2006; Meredith et al., 2006).
In the context of FM, it has been documented that individuals with insecure attachment styles are exceptionally represented (Hallberg and Carlsson, 1998). In particular, Peñacoba et al. (2017) revealed that women with a diagnosis of FM presented lower rates of secure attachment style (69.9% vs 86%), higher avoidant (19.8% vs 7.4%), and anxious–ambivalent attachment (10.3% vs 6.6%) compared to healthy women.
QoL in FM
Women with a diagnosis of FM report several clinical problems, such as tiredness, sleep perturbations, stiffness, skin sensitivity, irritable bowel syndrome, cognitive disturbance, headaches, fluid retention, paresthesia, restless legs, and anxiety/depressive symptoms. These enduring physical and psychological manifestations may affect the patients’ QoL (Galvez-Sánchez et al., 2019; Verbunt et al., 2008). Compared to other patients with a chronic disease (e.g. osteoarthritis, rheumatoid arthritis, systemic lupus erythematosus, myocardial infarction, chronic obstructive pulmonary disease, congestive heart failure, hypertension, and diabetes), FM patients refer the poorer health condition (see Lee et al., 2017).
Internationally, numerous studies have confirmed the effect of several factors on the QoL of women with a diagnosis of FM. Among these variables, the most relevant are age, educational level, number of children, comorbidity with a rheumatologic diseases (Linares et al., 2008), employment status (Reisine et al., 2004), depression, anxiety, self-efficacy, and social support (Alok et al., 2014; Lee et al., 2017; Pagano et al., 2004; Tander et al., 2008).
However, it is important to underline that both objective and subjective factors that refer to general satisfaction with life or its components must be considered in understanding the impact of FM on the reported QoL (Bowling et al., 2002). In particular, the relationships between adult attachment styles and QoL in FM patients still need to be investigated. Also, according to attachment theory (Bowlby, 1977), the link between attachment and QoL may be mediated by several pathways, one of which is self-esteem (Brennan and Bosson, 1998).
Self-esteem
Self-esteem plays a crucial role in the QoL of FM patients, influencing disease complications (Galvez-Sánchez et al., 2019).
Self-esteem is
the degree to which the qualities and characteristics contained in one’s self- are perceived to be positive. It reflects a person’s physical self-image, view of his or her accomplishments and capabilities, and values and perceived success in living up to them, as well as the ways in which others view and respond to that person. (Granito, 2007)
It has been demonstrated that there is a major decrease in self-esteem and self-efficacy in FM patients (Galvez-Sánchez et al., 2018). Poor self-esteem may consequently influence overall FM patients’ impairment. For this reason, it is important to be evaluated.
Significant research indicates that insecure attachment is related to lower self-esteem in comparison with secure attachment styles (Collins and Read, 1990; Foster et al., 2007). Consequently, FM patients with insecure attachment style may be prone to low self-esteem, which in turn may result in reduction of QoL (Galvez-Sánchez et al., 2019).
Therefore, the present study was conducted with the aim of improving current knowledge and understanding of attachment styles and their connection with self-esteem and QoL in individuals with a diagnosis of FM. Specifically, we hypothesized a significant link between insecure attachment styles, low self-esteem, and poor QoL. In particular, according to Bartholomew and Horowitz’s adult attachment model (1991), it was postulated that preoccupied and fearful attachment styles would be associated with lower self-esteem and poorer QoL.
Method
Participants
Participants were 371 women with a physician’s diagnosis of FM. The age of the participants ranged from 27 to 62 years, with a mean age of 42.7 years (standard deviation (SD) = 10.6). The average number of years since diagnosis was 7.4 years (SD = 2.4).
Most participants were married (80.3%), 10.8 percent were separated, 7.8 percent were single, and 1.1 percent were widowed. In terms of education level, most of our sample had a high school diploma (48.8%), followed by 39.7 percent who completed a university degree and 11.5 percent, a doctorate or post-doctorate degree. The sample was composed solely of Italian Caucasian women. No incentives were given to the study participants. The sampling was non-probabilistic and involved women who voluntarily participated in the research.
Measures
Adult attachment styles
The Relationship Questionnaire (RQ; Bartholomew and Horowitz, 1991) was used to assess adult attachment styles. The RQ comprises four different paragraphs describing the secure, dismissing, preoccupied, and fearful attachment styles. Participants evaluated themselves on each of the four attachment styles using a scale ranging from 1 (disagree strongly) to 7 (agree strongly). The RQ as a measure of adult attachment has been commonly used and has shown satisfactory validity as measured with concurrent self- and friend-reports of interpersonal functioning (Bartholomew and Horowitz, 1991), as well as longitudinal observer-based assessments of personality and behavioral characteristics (Klohnen and Bera, 1998).
QoL
The World Health Organization Quality of Life Questionnaire (WHOQOL-BREF; World Health Organization, 2011; Italian version, Girolamo et al., 2000) was used to assess the QoL. The scale consisted of 26-items rated on a 5-point Likert-type scale (from 1 = not at all to 5 = completely). The WHOQOL-BREF assesses QoL in four areas: physical health (PHY, 7 items), psychological health (PSY, 6 items), social relationships (SR, 3 items), and environment (EN, 8 items). Two of the items provide a component quantifying Overall QoL/health. The WHOQOL-BREF has been utilized to evaluate QoL in individuals with many diseases as chronic fatigue syndrome (Van Heck and Vries, 2002). Higher scores show a higher perceived QoL. Data from many states showed good internal consistency reliability and construct validity for the international WHOQOL-BREF (Skevington et al., 2004).
Self-esteem
The Rosenberg Self-Esteem Inventory (RSEI, Rosenberg, 1965; Italian version by Prezza et al., 1997) was used to assess global self-esteem. The scale consisted of 10-items rated on a 4-point Likert-type scale (from 1 = strongly agree to 4 = strongly disagree). The participants responded to items about their positive (e.g. I feel that I have a number of good qualities) and negative (e.g. I certainly feel useless at times) feelings about the self. Higher scores show a higher global self-esteem. The RSEI has generally demonstrated good psychometric properties (Curbow and Somerfield, 1991).
Recruitment and procedure
Participants were recruited from online sources. We posted announcements on FM online communities. The statement specified that we were carrying out “a research on women with a diagnosis of FM.” To participate, the women were required to be at least 18 years old and had previously received a certified diagnosis of FM. The ad then offered a linkage to the anonymous online survey. After giving consent, the women completed the next three pages of the survey, which included items to evaluate the above screening criteria. Women who were eligible were permitted to continue the study. Women who did not meet the eligibility conditions were thanked for their time. All applicants were informed about their rights as a study participant and participation was anonymous.
Data analyses
Statistical analysis was done with SPSS and Amos 21. The data were preliminarily screened for errors and outliers. Multiple imputation (MI; Galbraith, 2012) was applied to operate missing data. Prior to execution of MI, the data were evaluated to verify that absent values were missing at random (MAR). Subsequently, the level of missing data was analyzed to assure that less than 10 percent of data were lacking across scale scores. The assumption of MAR was met, and the percentage of missing data across scales (2%–4%) was appropriate. Twenty-five multiply imputed data sets were generated.
We explored the distribution of all study variables. Descriptive and correlation analysis were performed. Subsequent to conducting correlations among the study variables, tests of mediation were performed through a structural equation model (SEM). Four models were tested to examine self-esteem as a potential mediator of the relation between attachment style and QoL. Each model comprised one hypothetical observed independent factor (attachment style), one observed mediator factor (self-esteem), and one latent dependent factor (QoL). The QoL latent factor was measured using the four subscales of the WHOQOL-BREF (PHY, PSY, SR, and EN).
To evaluate the hypothesized model, numerous indicators were taken into consideration (Kline, 2015). Since the χ2 statistic is susceptible to sample size, other fit indicators have been measured: the comparative fit index (CFI), the Tucker–Lewis index (TLI), the standardized root mean square residual (SRMR), and the root mean square error of approximation (RMSEA), along with its 90 percent confidence interval (CI). It is suggested that good fit indicators for CFI and TLI are greater than .90, and for SRMR and RMSEA, less than .08 (Markus, 2012). A bootstrapping procedure using 1500 subsamples was done to assess the statistical significance of each path coefficient.
Results
Preliminary analyses
Descriptive statistics (mean and SD) and correlations for all model variables are presented in Table 1. At the bivariate level, supporting hypotheses, secure attachment style was correlated with high self-esteem as well as with high physical, psychological, social, and environmental health. Conversely, dismissing, preoccupied, and fearful attachment styles were associated with low self-esteem as well as with low physical, psychological, social, and environmental health. Finally, high self-esteem levels were associated with high physical, psychological, social, and environmental health.
Table 1.
Descriptive statistics and inter-scale correlations.
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.SA | 3.1 | 1.8 | – | ||||||||
| 2.DA | 2.8 | 1.9 | −.11* | – | |||||||
| 3.PA | 3.6 | 2 | −.19** | .30*** | – | ||||||
| 4.FA | 3.5 | 2.2 | −.47*** | −.6 | .10* | – | |||||
| 5.SE | 26.4 | 5.7 | .29*** | −.17** | −.21*** | −.16** | – | ||||
| 6.PHY | 19 | 3.3 | .20*** | −.12* | −.13* | −.11* | .24*** | – | |||
| 7.PSY | 17.2 | 3.4 | .29*** | −.18*** | −.22*** | −.22*** | .48*** | .44*** | – | ||
| 8.SR | 7.6 | 2.7 | .38*** | −.20*** | −.28*** | −.21*** | .40*** | .37*** | .57*** | – | |
| 9.EN | 14.9 | 3.9 | .33*** | −.20*** | −.13* | −.18** | .35*** | .41*** | .52*** | .51*** | – |
SA: secure attachment style; DA: dismissing attachment style; PA: preoccupied attachment style; FA: fearful attachment styles; SE: self-esteem; PHY: physical health; PSY: psychological health; SR: social relationships; EN: environment.
p < .05; **p < .01; ***p < .001.
Tests of mediation
Four structural models were used to assess the effect of each attachment style and self-esteem on QoL.
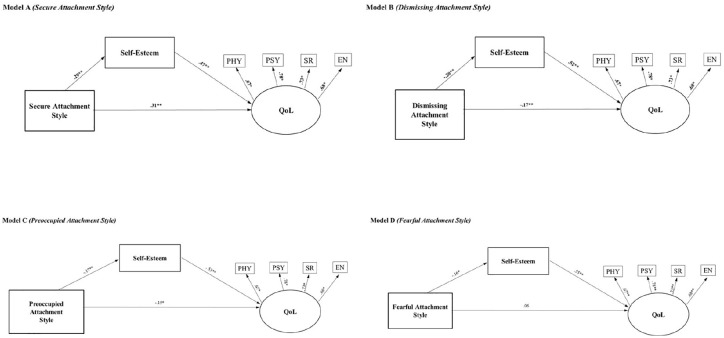
Specifically, the models estimated the direct effect of each attachment style (Models A, B, C, and D) on self-esteem, the direct and indirect effects of each attachment style on QoL, and the direct effect of self-esteem on QoL. Table 2 illustrates the indirect effects of self-esteem on the associations between each attachment style and QoL. Figure 1 graphically shows the relationship for each of the attachment styles, self-esteem, and QoL.
Table 2.
Standardized direct and indirect effects.
| Attachment styles | Self-esteem |
QoL |
|
|---|---|---|---|
| Direct | Direct | Indirect | |
| Secure attachment style | .29**
CI = .19 to.37 |
.31**
CI = .20 to.40 |
.14**
CI = .09 to.19 |
| Dismissing attachment style | −.21**
CI = −.31 to −.09 |
−.17**
CI = −.27 to −.08 |
−.11**
CI = −.17 to −.05 |
| Preoccupied attachment style | −.17**
CI = −.27 to −.07 |
−.15* CI = −.26 to −.06 |
−.09* CI = −.17 to −.05 |
| Fearful attachment style | −.16**
CI = −.25 to −.06 |
−.06 CI = −.16 to .05 |
−.09* CI = −.14 to −.03 |
The confidence intervals (CIs) are based on the findings from bootstrapping analysis (1500 samples).
p < .01.; **p < .001.
Figure 1.
Path models.
The relationship between attachment styles (secure, dismissive, preoccupied, and fearful) and QoL mediated by self-esteem. The coefficients shown are standardized.
Model A (secure attachment style)
The results of the path model were good (χ2 = 18.33, df = 8, p = .02, CFI = .98, incremental fit index (IFI) = .98, RMSEA = .06 (90% CI = .02, .09), SRMR = .03). Secure attachment style had significant direct effect on self-esteem as well as direct and indirect effects on QoL. Also, self-esteem had statistically significant direct effect on QoL.
These results showed that women’ attachment secure style affected both directly and indirectly, through self-esteem, QoL.
Model B (dismissing attachment style)
The results of the path model were appropriate (χ2 = 16.66, df = 8, p = .03, CFI = .98, IFI = .98, RMSEA = .05(90% CI = .01, .09), SRMR = .03). Dismissing attachment style had significant direct and indirect effects on QoL. Dismissing attachment style had significant direct effect on self-esteem and self-esteem had statistically significant direct effect on QoL. These results showed that women’ attachment dismissing style affected both directly and indirectly, through self-esteem, QoL.
Model C (preoccupied attachment style)
The results of the path model were very good (χ2 = 11.98, df = 8, p = .15, CFI = .99, IFI = .99, RMSEA = .04 (90% CI = .00, .08), SRMR = .03). Preoccupied attachment style had significant direct and indirect effects on QoL. Preoccupied attachment style had significant direct effect on self-esteem and self-esteem had statistically significant direct effect on QoL. These results showed that women’ attachment preoccupied style affected both directly and indirectly, through self-esteem, QoL.
Model D (fearful attachment style)
The results of the path model were good (χ2 = 16.93, df = 8, p = .03, CFI = .98, IFI = .98, RMSEA = .06 (90% CI = .02, .09), SRMR = .03). It should be observed that there was no significant direct effect of fearful attachment style on QoL. Fearful attachment style had only significant indirect effect on QoL. Fearful attachment style had significant direct effect on self-esteem and self-esteem had statistically significant direct effect on QoL. These results showed that women’ attachment fearful style affected indirectly, through self-esteem, QoL. Women with FM with fearful attachment levels are prone to lower self-esteem which may, in turn, lower their QoL.
Discussion
Our findings support the notion that psychological characteristics are critical in understanding FM pathology. Improving knowledge of variables that either aggravate or impede coping with chronic pain conditions, such as FM, is a crucial interest of health psychology.
The QoL relies on the aspects of physical, psychological, environments, and social wellbeing. These features are linked to self-esteem that is compromised due to the social impairment connected to having a chronic disease (Brorsson et al., 2001).
Some empirical studies have documented the relationship between attachment style and physical and psychological symptoms reported by FM patients (MacDonald and Kingsbury, 2006; Meredith et al., 2006). However, to our knowledge, this is the first study to evaluate whether self-esteem mediates the relationship between attachment style and QoL in a sample of women with a diagnosis of FM.
Low self-esteem, in chronic illness, has a negative effect on women’ interpersonal relations, feelings, and emotions. In FM patients, several research studies have proved that self-esteem is considerably lower compared to healthy persons (Galvez-Sánchez et al., 2018; Garaigordobil, 2015).
Women suffering from FM, due to the feeling of loss of self-control, are predisposed to low self-esteem, which in turn will result in reduction of QoL and increase in prevalence of mental problems and physical illnesses. In line with attachment theory, secure attachment relationships may promote positive feelings of self-worth (Allen, 2018).
In our study, it was found that there was a significantly different effect on levels of self-esteem between women with secure and insecure attachment style. Secure attachment style was found to be related to higher levels of self-esteem, while insecure attachment style was found to be linked with lower self-esteem levels.
In support of our hypotheses and in accordance with Bartholomew and Horowitz (1991), our results showed that self-esteem is an important issue, linking attachment styles and QoL in women with FM.
Secure, dismissing, and preoccupied attachment styles were also directly associated with QoL, as secure/insecure attachment may lead to the success or failure of protective factors for health.
It is plausible that securely attached FM patients define themselves, perceive others in more positive terms, and react to pain with less distress, spending more time thinking of positive aspects of their life. Conversely, insecurely attached women with a diagnosis of FM may perceive themselves and others in more negative terms and react to pain with more suffering, focusing on the negative aspects, neglecting the positive part of their life.
In sum, our results showed that secure attachment relationships and high self-esteem represent protective factors for QoL of women with a diagnosis of FM, whereas the contrary emerged as regards insecure attachments and low self-esteem.
However, contrary to expectation, women’s fearful attachment style was not directly related to QoL, but only indirectly through self-esteem. Indeed, fearful attachment is characterized by both a negative model of the self and of the other; these features would put fearfully attached individuals at higher risk for psychological functioning (Vismara et al., 2019). However, being this attachment style the most disorganized, it is also the most unpredictable. In one study, for instance, fearful and dismissing attachment styles were not significantly associated with pain-related disability in patients with chronic widespread pain (Davies et al., 2009).
Limitations and future studies
Despite the interesting results regarding the predictive validity of adult attachment styles over self-esteem and QoL in women with FM, these findings should be taken with caution due to the following limitations.
First, the cross-sectional design of this study does not allow any conclusions regarding directionality of relationships. The results should be verified and supported by additional research studies, including longitudinal study.
Second, all measures were based on self-reports, so we could not prevent social desirability bias. The accuracy of self-reported attachment styles may be improved by using other measures of attachment (e.g. adult attachment interview; Main et al., 2002).
Third, physical symptoms, such as pain or fatigue, are more common in women who do not have social support (Neugebauer and Katz, 2004); among women with FM, attachment styles and self-esteem may be the stronger predictors for increased QoL, but social support could have a potential regulating effect (Jakobsson and Hallberg, 2002). Therefore, to provide a more complete model, future studies should include measures of perceived social support. Finally, the sample is limited to only FM online communities. Future research should recruit women with FM who may have requested assistance from other sources of care.
Our results suggest the need for additional research to provide integrated theoretical models to understand the mechanisms underpinning the QoL of women with a diagnosis of FM.
Regardless of these limitations, the research findings provide evidence regarding the importance of adult attachment and self-esteem in contributing to the QoL in women with a diagnosis of FM. These findings, therefore, may improve the understanding of how these psychological variables may contribute to psychological functioning of FM patients, enhancing the effectiveness of treatment in the context of this disability.
Indeed, attachment-informed interventions may constitute a useful and efficacious means to promote psychological and physical health (Mikulincer and Shaver, 2012; Palitsky et al., 2013 Pietromonaco and Beck, 2019). At the level of primary preventive programs, enhancing attachment security since infancy and childhood should be a priority to hinder malaise and favor a good QoL. At the level of secondary and tertiary prevention, identifying the individual’s attachment pattern could allow to precociously detect those at risk of adjustment difficulties to FM prior to intervention. Finally, at the level of treatment, acknowledging the individual’s attachment style may support more successful intervention since it considers the specific needs of the patient (Lewczuk et al., 2018; Meredith et al., 2008).
The study of these clinical programs may be considered one of the most promising domains of research in FM.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Compliance with ethical standards: All procedures performed in the present study involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all participants included in the study.
ORCID iD: Cristina Sechi  https://orcid.org/0000-0001-8900-6983
https://orcid.org/0000-0001-8900-6983
References
- Allen JG. (2018) Attachment in Adulthood. Mentalizing in the Development and Treatment of Attachment Trauma. pp. 59–109. Routledge. [Google Scholar]
- Alok R, Das SK, Agarwal GG, et al. (2014) Practical utility of cognitive behaviour therapy in patients of fibromyalgia. Indian Journal of Rheumatology 9: S64. [Google Scholar]
- American Psychiatric Association (APA) (2013) Diagnostic and Statistical Manual of Mental Disorders (5th edn). Washington, DC: APA. [Google Scholar]
- Amir M, Neumann L, Bor O, et al. (2000) Coping styles, anger, social support, and suicide risk of women with fibromyalgia syndrome. Journal of Musculoskeletal Pain 8(3): 7–20. [Google Scholar]
- Bartholomew K, Horowitz LM. (1991) Attachment styles among young adults: A test of a four-category model. Journal of Personality and Social Psychology 61(2): 226–244. [DOI] [PubMed] [Google Scholar]
- Bowlby J. (1977) The making and breaking of affectional bonds. British Journal of Psychiatry 130(3): 201–210. [DOI] [PubMed] [Google Scholar]
- Bowling A, Banister D, Sutton S, et al. (2002) A multidimensional model of the quality of life in older age. Aging & Mental Health 6(4): 355–371. [DOI] [PubMed] [Google Scholar]
- Brennan KA, Bosson JK. (1998) Attachment-style differences in attitudes toward and reactions to feedback from romantic partners: An exploration of the relational bases of self-esteem. Personality and Social Psychology Bulletin 24(7): 699–714. [Google Scholar]
- Brorsson B, Bernstein SJ, Brook RH, et al. (2001) Quality of life of chronic stable angina patients 4 years after coronary angioplasty or coronary artery bypass surgery. Journal of Internal Medicine 249(1): 47–57. [DOI] [PubMed] [Google Scholar]
- Chamie M. (1995) What does morbidity have to do with disability? Disability and Rehabilitation 17(7): 323–337. [DOI] [PubMed] [Google Scholar]
- Cieza A, Stucki G, Weigl M, et al. (2004) ICF core sets for chronic widespread pain. Journal of Rehabilitation Medicine 36: 63–68. [DOI] [PubMed] [Google Scholar]
- Collins NL, Read SJ. (1990) Attachment and adult romantic relationships. PsycEXTRA Dataset. DOI: 10.1037/e334462004-001. [DOI] [Google Scholar]
- Curbow B, Somerfield M. (1991) Use of the Rosenberg self-esteem scale with adult cancer patients. Journal of Psychosocial Oncology 9(2): 113–131. [Google Scholar]
- Davies KA, Macfarlane GJ, McBeth J, et al. (2009) Insecure attachment style is associated with chronic widespread pain. Pain 143(3): 200–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dima AL, Gillanders DT, Power MJ. (2013) Dynamic pain–emotion relations in chronic pain: A theoretical review of moderation studies. Health Psychology Review 7(Supl. 1): S185–S252. [Google Scholar]
- Dreyer L, Kendall S, Danneskiold-Samsøe B, et al. (2010) Mortality in a cohort of Danish patients with fibromyalgia: Increased frequency of suicide. Arthritis & Rheumatism 62(10): 3101–3108. [DOI] [PubMed] [Google Scholar]
- Foster JD, Kernis MH, Goldman BM. (2007) Linking adult attachment to self-esteem stability. Self and Identity 6(1): 64–73. [Google Scholar]
- Galbraith S. (2012) Applied missing data analysis by Craig K Enders. Australian & New Zealand Journal of Statistics 54(2): 251–251. [Google Scholar]
- Galvez-Sánchez CM, Duschek S, Reyes del Paso GA. (2019) Psychological impact of fibromyalgia: Current perspectives. Psychology Research and Behavior Management 12: 117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvez-Sánchez CM, Reyes del Paso GA, Duschek S. (2018) Cognitive impairments in fibromyalgia syndrome: Associations with positive and negative affect, alexithymia, pain catastrophizing and self-esteem. Frontiers in Psychology. Epub ahead of print 22 March DOI: 10.3389/fpsyg.2018.00377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garaigordobil M. (2015) Predictor variables of happiness and its connection with risk and protective factors for health. Frontiers in Psychology. Epub ahead of print 12 August DOI: 10.3389/fpsyg.2015.01176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girolamo GD, Rucci P, Scocco P, et al. (2000) Quality of life assessment: Validation of the Italian version of the WHOQOL-Brief. Epidemiologia e Psichiatria Sociale 9(1): 45–55. [DOI] [PubMed] [Google Scholar]
- Granito VJ. (2007) APA dictionary of psychology. PsycEXTRA Dataset. DOI: 10.1037/e510732010-007. [DOI] [Google Scholar]
- Griffin DW, Bartholomew K. (1994) Relationship scales questionnaire. PsycTESTS Dataset. Available at: https://doi.apa.org/doiLanding?doi=10.1037%2Ft10182-000
- Hallberg LR-M, Carlsson SG. (1998) Anxiety and coping in patients with chronic work-related muscular pain and patients with fibromyalgia. European Journal of Pain 2(4): 309–319. [DOI] [PubMed] [Google Scholar]
- Jakobsson U, Hallberg IR. (2002) Pain and quality of life among older people with rheumatoid arthritis and/or osteoarthritis: A literature review. Journal of Clinical Nursing 11(4): 430–443. [DOI] [PubMed] [Google Scholar]
- Kline RB. (2015) Principles and Practice of Structural Equation Modeling. New York, NY: Guilford Publications. [Google Scholar]
- Klohnen EC, Bera S. (1998) Behavioral and experiential patterns of avoidantly and securely attached women across adulthood: A 31-year longitudinal perspective. Journal of Personality and Social Psychology 74(1): 211–223. [DOI] [PubMed] [Google Scholar]
- Kowal J, McWilliams LA, Péloquin K, et al. (2015) Attachment insecurity predicts responses to an interdisciplinary chronic pain rehabilitation program. Journal of Behavioral Medicine 38(3): 518–526. [DOI] [PubMed] [Google Scholar]
- Lee J-W, Lee K-E, Park D-J, et al. (2017) Determinants of quality of life in patients with fibromyalgia: A structural equation modeling approach. PLoS ONE 12(2): e0171186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legand M, Brennstuhl MJ, Machado J, et al. (2019) Prise en charge psychothérapeutique de la fibromyalgie: Une revue systématique. Douleurs: Évaluation—Diagnostic—Traitement 20(3): 89–108. [Google Scholar]
- Lewczuk K, Kobylińska D, Marchlewska M, et al. (2018) Adult attachment and health symptoms: The mediating role of emotion regulation difficulties. Current Psychology. Available at: https://link.springer.com/article/10.1007/s12144-018-0097-z
- Linares MCU, Ruiz-Pérez I, Pérez MJB, et al. (2008) Analysis of the impact of fibromyalgia on quality of life: Associated factors. Clinical Rheumatology 27(5): 613–619. [DOI] [PubMed] [Google Scholar]
- MacDonald G, Kingsbury R. (2006) Does physical pain augment anxious attachment? Journal of Social and Personal Relationships 23(2): 291–304. [Google Scholar]
- McWilliams LA, Asmundson GJG. (2007) The relationship of adult attachment dimensions to pain-related fear, hypervigilance, and catastrophizing. Pain 127(1): 27–34. [DOI] [PubMed] [Google Scholar]
- Main M, Goldwyn R, Hesse E. (2002) Adult Attachment Scoring and Classification Systems, Version 7.1. (Unpublished manuscript). Berkeley, CA: University of California. [Google Scholar]
- Markus KA. (2012) Principles and practice of structural equation modeling by Rex B. Kline. Structural Equation Modeling: A Multidisciplinary Journal 19(3): 509–512. [Google Scholar]
- Meredith P, Ownsworth T, Strong J. (2008) A review of the evidence linking adult attachment theory and chronic pain: Presenting a conceptual model. Clinical Psychology Review 28(3): 407–429. [DOI] [PubMed] [Google Scholar]
- Meredith P, Strong J, Feeney JA. (2006) Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain 123(1): 146–154. [DOI] [PubMed] [Google Scholar]
- Meredith PJ. (2016) Attachment theory and pain. In: Hunter J and R., Maunder R. (eds) Improving Patient Treatment with Attachment Theory: A Guide for Primary Care Practitioners and Specialists. Cham: Springer, pp. 55–73. [Google Scholar]
- Mickelson KD, Kessler RC, Shaver PR. (1997) Adult attachment in a nationally representative sample. Journal of Personality and Social Psychology 73(5): 1092–1106. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR. (2012) An attachment perspective on psychopathology. World Psychiatry 11(1): 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neugebauer A, Katz PP. (2004) Impact of social support on valued activity disability and depressive symptoms in patients with rheumatoid arthritis. Arthritis Care & Research 51(4): 586–592. [DOI] [PubMed] [Google Scholar]
- Pagano T, Matsutani LA, Ferreira EAG, et al. (2004) Assessment of anxiety and quality of life in fibromyalgia patients. Sao Paulo Medical Journal 122(6): 252–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palitsky D, Mota N, Afifi TO, et al. (2013) The association between adult attachment style, mental disorders, and suicidality: Findings from a population-based study. The Journal of Nervous and Mental Disease 201(7): 579–586. [DOI] [PubMed] [Google Scholar]
- Peñacoba C, Perez-Calvo S, Blanco S, et al. (2017) Attachment styles, pain intensity and emotional variables in women with fibromyalgia. Scandinavian Journal of Caring Sciences 32(2): 535–544. [DOI] [PubMed] [Google Scholar]
- Pietromonaco PR, Beck LA. (2019) Adult attachment and physical health. Current Opinion in Psychology 25: 115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prezza M, Trombaccia FR, Armento L. (1997) La scala dell’autostima di Rosenberg. Traduzione e validazione italiana [Rosenberg self-esteem scale. Italian translation and validation]. Bollettino di Psicologia Applicata 223: 35–44. [Google Scholar]
- Reisine S, Fifield J, Walsh S, et al. (2004) Employment and quality of life outcomes among women with fibromyalgia compared to healthy controls. Women & Health 39(4): 1–19. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. (1965) Rosenberg self-esteem scale. PsycTESTS Dataset. Available at: https://doi.apa.org/doiLanding?doi=10.1037%2Ft01038-000
- Rudin NJ. (2019) Fibromyalgia. In: Abd-Elsayed A. (ed.) Pain. Cham: Springer, pp. 693–697. [Google Scholar]
- Skevington SM, Lotfy M, O’Connell KA. (2004) The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Quality of Life Research 13(2): 299–310. [DOI] [PubMed] [Google Scholar]
- Su C-H, Chen J-H, Lan J-L, et al. (2015) Increased risk of coronary heart disease in patients with primary fibromyalgia and those with concomitant comorbidity—A Taiwanese population-based Cohort study. PLoS ONE 10(9): e0137137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan MJL, Thorn B, Haythornthwaite JA, et al. (2001) Theoretical perspectives on the relation between catastrophizing and pain. The Clinical Journal of Pain 17(1): 52–64. [DOI] [PubMed] [Google Scholar]
- Tander B, Cengiz K, Alayli G, et al. (2008) A comparative evaluation of health related quality of life and depression in patients with fibromyalgia syndrome and rheumatoid arthritis. Rheumatology International 28(9): 859–865. [DOI] [PubMed] [Google Scholar]
- Tavares LF, Germano Maciel D, Pereira Barros da Silva TY, et al. (2020) Comparison of functional and isokinetic performance between healthy women and women with fibromyalgia. Journal of Bodywork and Movement Therapies 24(1): 248–252. [DOI] [PubMed] [Google Scholar]
- Tunks ER, Weir R, Crook J. (2008) Epidemiologic perspective on chronic pain treatment. The Canadian Journal of Psychiatry 53(4): 235–242. [DOI] [PubMed] [Google Scholar]
- Van Heck GL, Vries JD. (2002) Quality of life of patients with chronic fatigue syndrome. Journal of Chronic Fatigue Syndrome 10(1): 17–35. [Google Scholar]
- Verbrugge LM, Juarez L. (2006) Profile of arthritis disability: II. Arthritis & Rheumatism 55: 1102–1113. [DOI] [PubMed] [Google Scholar]
- Verbunt JA, Pernot DH, Smeets RJ. (2008) Disability and quality of life in patients with fibromyalgia. Health and Quality of Life Outcomes 6(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara L, Presaghi F, Bocchia M, et al. (2019) Attachment patterns in subjects diagnosed with a substance use disorder: A comparison of patients in outpatient treatment and patients in therapeutic communities. Frontiers in Psychiatry 10: 807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker JG, Littlejohn GO. (2006) Measuring quality of life in rheumatic conditions. Clinical Rheumatology 26(5): 671–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2011) SpringerReference. [Google Scholar]