Abstract
Research linking economic conditions and health often does not consider children’s mental health problems, which are the most common and consequential health issues for children and adolescents. We examine the effects of unemployment rates and housing prices on well-validated child and adolescent mental health outcomes and use of special education services for emotional problems in the 2001–2013 National Health Interview Survey. We find that the effects of economic conditions on children’s mental health are clinically and economically meaningful; children’s mental health outcomes worsen as the economy weakens. The effects of economic conditions on child and adolescent mental health are pervasive, found in almost every subgroup that we examine. The use of special education services for emotional problems also rises when economic conditions worsen. Our analyses of possible mechanisms that link economic conditions to child mental health, suggest that parental unemployment cannot fully explain the relationship between economic conditions and child mental health.
Keywords: Children, Mental Health, Economic Conditions, Unemployment
1. Introduction
An extensive body of research examines the effects of economic conditions on human health. Seminal work by Ruhm demonstrated that mortality rates decline when unemployment is high, possibly because the time costs of health-producing activities also goes down (Ruhm, 2000). This original finding has been extended and challenged in subsequent research with mixed findings, except in the case of mental health. Previous research consistently finds that adult mental health outcomes worsen during economic downturns (Charles & DeCicca, 2008; Ruhm, 2005, 2015; Stevens, Miller, Page, & Filipski, 2013). A related literature examines the effects of the “Great Recession” on physical and mental health of adults (Davalos & French, 2011; McInerney & Mellor, 2012; McInerney, Mellor, & Nicholas, 2013; Seeman et al., 2018), eating habits (Dave & Kelly, 2012), suicide (Houle & Light, 2014), hospitalizations and emergency department use (Currie & Tekin, 2015), and demand for psychotropic medication (Bradford & Lastrapes, 2014). In each case, the Great Recession coincided with negative health impacts.
Overall, the existing body of research has made influential contributions towards understanding the relationship between economic conditions and adult health, but the relationship between the economy and children’s health is less-developed. Two previous studies examined the impact of changes in economic conditions (measured by state-level unemployment rates or county-level job losses) in-utero and found conflicting results for birth weight (Carlson, 2015; Dehejia & Lleras-Muney, 2004). Other research found that individuals born during recessions live, on average, several years fewer than those born during economic expansions (Van Den Berg, Lindeboom, & Portrait, 2006). Three other studies have considered child or adolescent health outcomes in relation to economic conditions. Simon and Cotti use survey data from 2004–2012 and estimate the relationship between stock market prices and child health outcomes, finding that child health worsens when stock prices rise (Cotti & Simon, 2018). Currie and Tekin use administrative hospital data from four states between 2005–2009 to estimate the relationship between home foreclosures and hospitalizations, including admissions for psychiatric diagnoses (Currie & Tekin, 2015). Their study found increases in foreclosures were associated with increases in non-elective hospital and emergency room visits (including visits for mental health conditions for children). The most comparable research to our study examined how state-level job losses affected suicidality in adolescents (Gassman-Pines, Ananat, & Gibson-Davis, 2014). Using biennial data from the Youth Risk Behavior Surveillance System, increases in the annual number of workers who lost jobs as a result of mass closings or layoffs were positively associated with adolescent suicidality (suicidal thoughts or attempts). Taken together, the limited research on economic conditions and mental health largely omitted young children, did not consider children’s mental health as a main outcome and did not consider possible mechanisms linking economic conditions and mental health for children.
Mental health problems for children and adolescents are more common than physical health problems, and poor mental health in childhood impedes human capital accumulation and future labor market outcomes more than physical conditions (Case, Fertig, & Paxson, 2005; Currie, Stabile, Manivong, & Roos, 2010; A. Goodman, Joyce, & Smith, 2011). About 11% of children aged 8–15 years have mental disorders causing severe impairment (Merikangas et al., 2010); 8% of adolescents annually experience a “severe emotional disturbance,” (Kessler et al., 2012); and nearly half of mental health conditions in adulthood initiate in childhood or adolescence (Kessler et al., 2005). Children with mental health conditions or emotional problems are more likely to use special education services, repeat grades, perform poorly on standardized tests and are less likely to complete secondary education (Currie & Stabile, 2006; Fletcher & Wolfe, 2008). Untreated mental health problems can also result in lower grades, initiation of substance use, and other risky behaviors (Busch, Golberstein, & Meara, 2014). Poor health and economic outcomes in adulthood are correlated with childhood onset of mental health disorders (Currie, 2009), and overall consequences of poor mental health in childhood exceed those of other childhood health problems (Case, Fertig, and Paxson 2005). One recent estimate suggests that child and adolescent mental health disorders cost $247 billion annually (National Research Council and Institute of Medicine, 2009), based primarily on the direct costs to individuals and families. However, the external costs are also large, as mental health problems in childhood and adolescence are linked to delinquent behavior (Busch et al., 2014), poorer academic outcomes for classmates (Aizer, 2008), and addiction and crime in adulthood (Currie & Stabile, 2009; Fergusson, Horwood, & Ridder, 2007).
Negative economic conditions can adversely affect mental health in children through several pathways. First, psychological and social stress within the household could be higher during recessions due to changes in parental employment and hours worked, a reduction or stagnation in earnings, reductions in liquid wealth, the loss of social status, and financial pressure to pay bills and debt (DeNavas-Walt, Proctor, & Smith, 2012; Hoynes, Miller, & Schaller, 2012; Kalil, 2013; Weiland & Yoshikawa, 2012). Even without any change in employment situation, poor economic conditions can increase stress for parents due to increased job insecurity among the employed and fewer opportunities for finding work among the unemployed (Carlson, 2015). Meanwhile, people unaffected by job loss but living in neighborhoods with declining social cohesion or deteriorating physical structures due to recessions may feel additional strain. Increased family stress during economic recessions may result in increasing intrafamily conflict (Conger & Donnellan, 2007) and, at the extremes, child maltreatment (Stephens-Davidowitz, 2013). In addition to stress-related pathways, other financially-related mechanisms—including reductions in income, wealth, and changes in time cost—can affect children’s mental health during recessions. For example, children’s mental health outcomes worsen when family incomes decline (Milligan & Stabile, 2011) or during spells of parental job loss (Johnson, Kalil, & Dunifon, 2010). Job losses or income declines could reduce health insurance coverage and use of mental health services (Cawley, Moriya, & Simon, 2015; Schaller & Stevens, 2015). Finally, while economic recessions may reduce time-costs for parents, spending more time with children may affect children negatively if parents are stressed during spells of unemployment, as biomarkers of child stress are correlated with parental mental health (Lupien, King, Meaney, & McEwen, 2000). We do not describe all possible mechanisms linking economic conditions and children’s mental health, but we hypothesize that deteriorating economic conditions are associated with worse mental health outcomes for children and adolescents.
In this paper, we add to the literature on the effects of economic conditions on children’s and adolescents’ mental health in several ways. We link 13 years of nationally-representative data with measures of child mental health status and use of intensive services for emotional problems to two measures of economic conditions: unemployment rates and housing prices. We find that the effects of economic conditions on children’s mental health are clinically and economically meaningful; children’s mental health outcomes worsen as the economy weakens. We also document effects of economic conditions on the use of special education services for emotional problems. The effects of economic conditions on child and adolescent mental health are pervasive, found in nearly every subgroup that we examine. We also examine potential mediators of the relationship between economic conditions and children’s mental health.
2. Methods
2.1. Data Source
To explore the relationship between economic conditions and children’s mental health, we use annual cross-sectional data from the 2001–2013 National Health Interview Survey (NHIS). Conducted by the National Center for Health Statistics (NCHS), the NHIS is nationally representative of the civilian non-institutionalized population in the United States (National Center for Health Statistics, 2013). The family core questionnaire records basic demographic, health, and disability information for each household member. One adult and one child in each household are randomly selected for a more detailed health interview. Approximately 13,000 children are selected each year for the “sample child” component of the NHIS. A knowledgeable adult provides responses about the child’s access and utilization of care, health conditions, and demographic characteristics. All responses are self-reported in a face-to-face interview.
2.2. Measures of Childhood Mental Health
Since 2001, the NHIS has collected data on the mental health of children and adolescents aged 4–17 years using measures developed in the Child Strength and Difficulties Questionnaire (SDQ) (Bourdon, Goodman, Rae, Simpson, & Koretz, 2005). The SDQ assesses psychopathology and social adjustment in young children and adolescents. The original questionnaire includes 25 core items across 5 domains (emotional symptoms, conduct problems, hyperactivity-inattention, peer problems, and prosocial behavior) and can be administered to parents, teachers and children (R. Goodman, 2001). SDQ scores are highly predictive of mental illness. For instance, 46% of children in the top decile of SDQ scores have a DSM-IV diagnoses of mental illness (as determined by an independent clinical rater), compared to 5% in the lower 90% of SDQ scores (R. Goodman, 2001). SDQ scores are highly correlated with outcomes such as the use of mental health services, special education services, or early intervention services (Pastor, Reuben, & Duran, 2012). Parent-reported SDQ scores also correlate highly with teacher and child assessments (R. Goodman, 2001).
In 2001–2013, the NHIS collected five of the 25 SDQ items, which were chosen based on their high correlations with the original five SDQ domains. The interviewer introduced the SDQ items by stating, “I am going to read a list of items that describe children. For each item, please tell me if it has been not true, somewhat true, [or] certainly true for [Sample Child] during the past 6 months.”
He/She gets along better with adults than with other children/youth.
He/She has good attention span, sees chores or homework through to the end.
He/She is often unhappy, depressed or tearful.
He/She is generally well behaved, usually does what adults request.
He/She has many worries, or often seems worried.
Each response is scored 0, 1 or 2, with higher numbers corresponding to worse outcomes. The five items are then summed to form a summary child mental health score ranging from 0 (least likely to have psychological problems) to 10 (most likely to have psychological problems). We use the SDQ score as a continuous measure of mental health severity and as a binary measure that distinguishes children with psychological problems based on the NCHS’s recommended threshold score of six or higher to predict serious psychological problems (Pastor et al., 2012). These five SDQ questions were excluded from the NHIS in 2008 and 2009 due to budget shortages, but were included in subsequent years.
The NHIS maintained a single, global measure of emotional disturbance throughout 2001–2013. This measure is the first question from the SDQ “Impact Scale,” a supplemental set of questions developed to better measure children’s degree of impairment. Psychometric research finds that this full supplemental scale also predicts independent diagnosis of DSM-IV mental illness (Goodman 1999). A knowledgeable respondent answered the following question:
Overall, do you think that [Sample Child name] has difficulties in any of the following areas: emotions, concentration, behavior, or being able to get along with other people?
Respondents indicated no (0), yes with minor (1), yes with definite (2), or yes with severe (3) difficulties. We use two outcomes based on this measure of “Emotional Difficulties”: a continuous measure of mental health severity and a binary measure that codes someone with definite or severe difficulties as having a likely psychological problem. This single item predicts psychiatric disorder nearly as well as the full Impact Supplement (R. Goodman, 1999; Pastor et al., 2012).
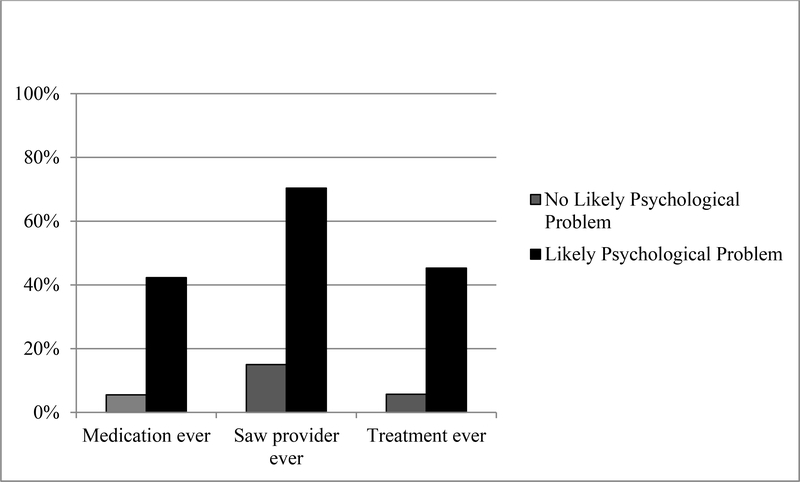
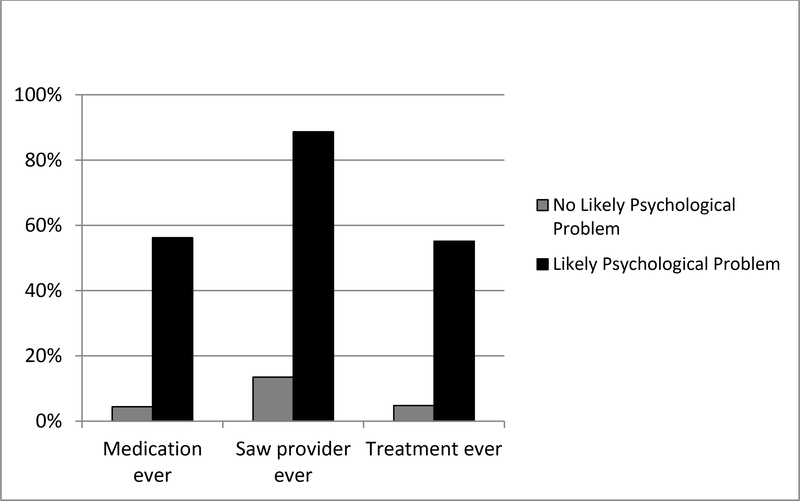
The SDQ measures have been shown to predict impairing mental health problems in children and adolescents, although the 5-item SDQ does not predict mental health problems as accurately as the original 25-item scale, and SDQ measure has greater reliability for adolescents than for children (Ringeisen, Aldworth, Colpe, Pringle, & Simile, 2015). We also demonstrate the usefulness of the NHIS’s mental health measures by comparing them with data on mental health treatment and medication use that are available in the 2005–2007 NHIS. Figures 1 and 2 illustrate the share of children reported ever taking medication for emotional problems, ever seeing or talking to a provider for emotional problems, and ever receiving treatment for emotional problems, stratified by whether there is a likely psychological problem based on the 5-question SDQ (Figure 1), and based on the Emotional Difficulty item (Figure 2). Both measures are strongly associated with mental health services utilization and treatments. For example, 45% of children with likely psychological problems (based on the SDQ) received treatment for emotional problems at some point in their lives, compared to 6% of those without a likely psychological problem outcome. About 55% of children with likely psychological problems (based on the Emotional Difficulties item) received treatment at some point in their lives, compared to 5% of those without likely psychological problems.
Figure 1.
Mental Health Outcomes by Likely Psychological Problems (based on SDQ)
Figure 2.
Mental Health Outcomes by Likely Psychological Problems (based on Emotional Difficulties)
Source: 2001–2013 National Health Interview Survey.
2.3. Statistical Analysis
We estimate the following model to assess the effect of economic conditions on children’s mental health status:
| (1) |
KidsMHijt represents a measure of child mental health status for a child i, observed in state j in quarter t. Economic Conditions measures state-level economic conditions (unemployment rate or housing price index, described below), in quarter t. The vector X includes the following child-level covariates: age, sex, and racial/ethnic group, and family-level covariates including highest level of parental education, average age of parents, and whether parents are single or married. State is a set of state fixed effects, and Quarter is a full set of 58 quarter fixed effects (44 fixed effects in the SDQ models that exclude 2008–2009). The specification in Equation 1 yields estimates of the effect of changes in economic conditions within states, over time, on child mental health. We also estimate versions of our models that include state-specific linear time trends.
We examine two measures of state-level economic conditions. The first is the unemployment rate, the most commonly used measure in studies linking economic conditions to health outcomes. Our quarterly measures of unemployment rates were extracted from the Bureau of Labor Statistics website and were defined as the percent of the population aged 16 years and older who are in the labor force but not currently employed. Our second measure of area-level quarterly economic conditions is the Freddie Mac Housing Price Index (HPI). The HPI measures state-level housing price appreciation and depreciation by tracking repeat transaction prices of one-family detached and townhome properties. The HPI has been used to link local changes in housing prices to antidepressant prescription volume among adults aged 55–64 years (Lin, Ketcham, Rosenquist, & Simon, 2013). The HPI is measured relative to a normalized base-year value of one (i.e., an HPI of 1.5 would represent housing prices 50% higher than the base year).
Our hypothesis that children might be affected by short-term changes in economic conditions (measured via unemployment and housing prices) is motivated by ample evidence that adult mental health responds to economic conditions. These effects can be direct, as in the effect of job loss on mental health (Schaller & Stevens, 2015). Even those out of the labor market also show worse mental health outcomes as unemployment increases, as shown in an analysis of older Medicare beneficiaries (McInerney & Mellor, 2012). Similarly, area level measures of housing markets are related to mental health; previous analyses found suicide rates increased with state-level foreclosure rates (Houle & Light, 2014). Evidence from a review of 100 papers show that unemployment, income decline, and debts had significant associations with poor self-reported mental health, increased rates of common mental disorders, increases in substance use disorders, and suicidal behaviors in adults (Frasquilho et al., 2016). In these adult populations, no matter how mental health was measured, changes in business cycles are correlated with changes in mental health. For these reasons, we hypothesize that these childhood measures of mental health in the NHIS would also respond to business cycles.
Unemployment rates and HPI both reflect underlying economic conditions, but could differ in the pathways through which they affect children’s mental health and the net effects on children’s mental health. Whereas unemployment rates are relatively more likely to influence pathways related to household income and employment changes, housing prices may influence wealth and credit availability for homeowning households (Campbell & Cocco, 2007). We also examined MSA-level measures of unemployment rates and HPI, but only present the results of the state-level measures. State-level measures may be subject to less measurement error and to less bias due to endogenous migration in response to poor economic conditions than more-local measures, although more-local measures may be closer approximations to the economic conditions faced by any given household (Lindo, 2015). The MSA-level results are broadly similar to the state-level results, and are available upon request.
We use the restricted-use NHIS that allowed us to link area-level variables with the NHIS data. Following much of the related literature, we use contemporaneous measures of economic conditions and mental health outcomes.1 We estimate OLS models for continuous outcomes and probit maximum likelihood estimation for binary outcomes (presented with marginal effects).2 All models use NHIS sample weights, and standard errors are clustered at the state level (Bertrand, Duflo, & Mullainathan, 2004). This research was deemed Exempt from institutional review board approval by the University of Minnesota Institutional Review Board.
3. Results
Sample summary statistics are described in Table 1. The average child’s age is 10.5 years; approximately 60% of children are non-Hispanic white, 14% are non-Hispanic black, 20% are Hispanic, 6% are “other” races or ethnicities; and approximately 28% live in single parent households. The average mental health severity based on the SDQ score is 1.7, and 4.1% of children have a likely psychological problem based on their SDQ scores. The average Emotional Difficulties item score is 0.26, and 5.1% of children have a likely psychological problem based on their Emotional Difficulty score. Few children (2.4%) use special education services for emotional or behavioral problems.
Table 1.
Summary Statistics of Children 4–17 years old, 2001–2013 National Health Interview Survey
| Sample Mean |
|
|---|---|
| Age | 10.50 |
| (SD) | (2.79) |
| Male | 0.51 |
| Non-Hispanic White | 0.60 |
| Non-Hispanic Black | 0.14 |
| Hispanic | 0.20 |
| Other non-Hispanic races | 0.06 |
| Parental education < high school | 0.13 |
| Single parent household | 0.28 |
| Quarterly State Unemployment Rate | 6.59 |
| (SD) | (1.51) |
| Quarterly State HPI | 1.31 |
| (SD) | (0.19) |
| Outcomes Based on SDQ Score: | |
| Mental Health Severity | 1.713 |
| (SD) | (1.21) |
| Likely Psychological Problem | 0.041 |
| Outcomes Based on Emotional Difficulties Item: | |
| Mental Health Severity | 0.263 |
| (SD) | (0.405) |
| Likely Psychological Problem | 0.051 |
| Any special education or early intervention services due to mental or emotional problem | 0.0237 |
Notes: Variable means with standard deviation (SD) in parentheses. SDQ is the Strengths and Difficulties Questionnaire scale, and HPI is the Freddie Mac Housing Price Index.
3.1. Main effects of economic conditions on children’s mental health status
Table 2 presents the results for the SDQ-derived outcomes. Child mental health deteriorates in a weakening economy. As state unemployment rates fall, child mental health improves (marginal effect = 0.026 decrease in SDQ score for each percentage point decrease in the state unemployment rate; Panel A, Column 1). Results for MSA-level measures are similar in size and precision but slightly smaller, in general (available upon request). The estimated impact of economic conditions is larger in magnitude when state-specific linear time trends are included (Panel A, Column 2). We also find that increases in the state-level HPI lead to significantly better (i.e. lower) SDQ scores (Panel B, Column 1), and the results are similar when state-specific time trends are included. The magnitudes of the relative effects are similar across the two measures of economic conditions. A one-standard deviation improvement in state-level unemployment rates (1.51 percentage points) and HPI (0.19) leads to a 2.3% and 2.0% improvement in SDQ scores, respectively. Columns 3 and 4 of Table 2 show the results for probit models of the likelihood of a psychological problem, based on the SDQ score.3 A one-standard deviation improvement in unemployment rates leads to an 11% reduction in the likelihood of a psychological problem. The effect of a one-standard deviation improvement in state-level HPI leads to a 6.4% drop in the likelihood of a psychological problem. The results are similar in strength and precision when state-specific time trends are included in the models (Column 4).4
Table 2.
Regression Results, Outcomes from Strenghts & Difficulties Questionnaire Scale
| Panel A. State Unemployment Rate | ||||
| Mental Health Severity (0–10) | Likely Psychological Problem (0/1) | |||
| (1) | (2) | (3) | (4) | |
| Marginal Effect | 0.0263* | 0.0434** | 0.0030** | 0.0037*** |
| (SE) | (0.0132) | (0.0163) | (0.0012) | (0.0014) |
| Mean, Dep. Var. | 1.71 | 1.71 | 0.041 | 0.041 |
| Relative Effect of 1.51 Percentage Point Drop in Unemployment Rate | −2.3% | −3.8% | −11.0% | −13.6% |
| Area-specific linear time trends | No | Yes | No | Yes |
| Panel B. State Housing Price Index | ||||
| Mental Health Severity (0–10) | Likely Psychological Problem (0/1) | |||
| (1) | (2) | (3) | (4) | |
| Marginal Effect | −0.179** | −0.185** | −0.014** | −0.014* |
| (SE) | (0.068) | (0.084) | (0.006) | (0.007) |
| Mean, Dep. Var. | 1.71 | 1.71 | 0.041 | 0.041 |
| Relative Effect of 0.19 Point Rise in Housing Price Index | −2.0% | −2.1% | −6.4% | −6.4% |
| Area-specific linear time trends | No | Yes | No | Yes |
| Sample size | 94,229 | 94,229 | 94,229 | 94,229 |
Note: Results are from OLS (Columns 1–2) and probit (Columns 3–4) models with robust standard errors clustered on the state. A fall in unemployment rate of 1.51 percentage points and a rise in HPI of 0.19 represent one standard deviation improvements in economic conditions. Covariates include age, sex, race/ethnicity, parental education, parental age, and parental marital status. Models include a full set of state fixed effects and time fixed effects.
p-value <.10
p-value<.05
p-value<.01.
A similar overall pattern of results is found for the Emotional Difficulties item in Table 3, although the relative magnitudes of the effects are slightly larger than in the SDQ-based outcome models. Decreases in unemployment rates lead to improved mental health severity (Panel A, Column 1). Increases in the state HPI, (i.e., improving economic conditions), lead to significantly improved mental health severity (Panel B, Column 1). For both unemployment rates and HPI, the point estimates are similar regardless of whether state-specific time trends are included, although the point estimate on state unemployment rates loses statistical significance when the state-specific time trends are included (Panel A, Column 2). The relative effects are similar across the two measures of economic conditions. A one-standard deviation improvement in state-level unemployment rates and HPI leads to a 4.8% and 4.7% relative improvement in mental health severity, respectively, in the models without area-specific time trends. The results are broadly similar for likely psychological problems (Table 3, Columns 3–4). A one-standard deviation improvement in state-level economic conditions leads to a 7.4% to 15.7% reduction in likely psychological problems. Finally, we find that the effects of economic conditions on the likelihood of having psychological problems is even greater than for the continuous measures of mental health severity, suggesting that economic conditions matter more for children at risk of serious mental or emotional problems.
Table 3.
Regression Results, Outcomes Based on Emotional Difficulty Score
| Panel A. State Unemployment Rate | ||||
| Mental Health Severity (0–3) | Likely Psychological Problem (0/1) | |||
| (1) | (2) | (3) | (4) | |
| Marginal Effect | 0.0084** | 0.0082 | 0.0035*** | 0.0053*** |
| (SE) | (0.0035) | (0.0053) | (0.0011) | (0.0016) |
| Mean, Dep. Var. | 0.263 | 0.263 | 0.051 | 0.051 |
| Relative Effect of 1.51 Percentage Point Fall in Unemployment Rate | −4.8% | −4.8% | −10.4% | −15.7% |
| Area-specific linear time trends | No | Yes | No | Yes |
| Panel B. State Housing Price Index | ||||
| Mental Health Severity (0–3) | Likely Psychological Problem (0/1) | |||
| (1) | (2) | (3) | (4) | |
| Marginal Effect | −0.065*** | −0.061*** | −0.020*** | −0.024*** |
| (SE) | (0.015) | (0.019) | (0.005) | (0.007) |
| Mean, Dep. Var. | 0.263 | 0.263 | 0.051 | 0.051 |
| Relative Effect of 0.19 Point Rise in Housing Price Index | −4.7% | −4.4% | −7.4% | −8.9% |
| Area-specific linear time trends | No | Yes | No | Yes |
| Sample size | 110,267 | 110,267 | 110,267 | 110,267 |
Note: Results are from OLS (Columns 1–2) and probit (Columns 3–4) models with robust standard errors clustered on the state. A fall in unemployment rate of 1.51 percentage points and a rise in HPI of 0.19 represent one standard deviation improvements in economic conditions. Covariates are described in Table 2.
p-value <.10
p-value<.05
p-value<.01.
When we exclude the family-level covariates (parental education, average age of parents, and parental marital status) from the model, the point estimates are unchanged but are slightly less precise (available upon request). The stability of the point estimates with respect to family characteristics suggests that the estimates reflect actual effects of economic conditions, rather than compositional changes driven by selective migration along the dimensions of socioeconomic status, household structure, and parental age.
3.2. Do the Effects of Economic Conditions Vary by Sex or Age?
Tables 4 and 5 present the SDQ and Emotional Difficulties Item results, respectively, after stratifying by sex and by age (4 to 11 versus 12 to 17). We assess these groups separately because of different patterns of mental health problems by sex and by age. In addition, we also expect that adolescents may have relatively stronger responses to changes in economic conditions. Adolescents are more likely than younger children to perceive stressors in the family and broader environment (McLoyd, Kaplan, Purtell, Hardaway, & Smalls, 2009); adolescents have relatively stronger physiological stress responses (Lupien, McEwen, Gunnar, & Heim, 2009); and adolescents are also more likely to be directly affected by economic conditions either in terms of actual labor market participation or near-term entry into the labor market. Falling unemployment rates and rising housing prices both have a positive impact on mental health across sexes and across ages. The relative size of the impact varies from a 1.1% non-significant decrease in mental health severity among children 4 to 11 years as HPI rises by one standard deviation, to an 18.9% decrease in the chance of having a psychological problem for females when the unemployment rate falls by one standard deviation. Throughout Tables 4 and 5, we reported the results of models without controlling for state-specific linear time trends. The estimated results are similar with state-specific linear time trends (available upon request).
Table 4.
Outcomes Based on Strengths & Difficulties Questionnaire Scale - Heterogeneous Effects by Sex and Age
| Panel A. State Unemployment Rates | ||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| OLS: Mental Health Severity (0–10) | Probit: Likely Psychological Problem (0/1) | |||||||
| Males | Females | Age 4–11 | Age 12–17 | Males | Females | Age 4–11 | Age 12–17 | |
| Marginal Effect | 0.032* | 0.021 | 0.029* | 0.026 | 0.0013 | 0.0045** | 0.0025** | 0.0042* |
| (SE) | (0.018) | (0.017) | (0.017) | (0.018) | (0.0021) | (0.0018) | (0.0011) | (0.0021) |
| Mean, Dep. Var. | 1.83 | 1.60 | 1.62 | 1.84 | 0.046 | 0.036 | 0.035 | 0.049 |
| Relative Effect of 1.51 P.P. Fall in Unemployment Rate | −2.6% | −2.0% | −2.7% | −2.1% | −4.3% | −18.9% | −10.8% | −12.9% |
| Panel B. State Housing Price Index | ||||||||
| OLS: Mental Health Severity (0–10) | Probit: Likely Psychological Problem (0/1) | |||||||
| Males | Females | Age 4–11 | Age 12–17 | Males | Females | Age 4–11 | Age 12–17 | |
| Marginal Effect | −0.173** | −0.183** | −0.093 | −0.302*** | −0.011 | −0.018** | −0.004 | −0.029*** |
| (SE) | (0.074) | (0.084) | (0.080) | (0.086) | (0.010) | (0.008) | (0.006) | (0.010) |
| Mean, Dep. Var. | 1.83 | 1.60 | 1.62 | 1.84 | 0.046 | 0.036 | 0.035 | 0.049 |
| Relative Effect of 0.19 Point Rise in Housing Price Index | −1.8% | −2.2% | −1.1% | −3.1% | −4.5% | −9.5% | −2.2% | −11.2% |
| Sample size | 48,571 | 45,658 | 51,372 | 42,857 | 48,571 | 45,552 | 51,372 | 42,761 |
Note: Robust standard errors clustered on the state. A fall in unemployment rate of 1.51 percentage points and a rise in HPI of 0.19 represent one standard deviation improvements in economic conditions. Covariates are described in Table 2.
p-value <.10
p-value<.05
p-value<.01.
Table 5.
Outcomes Based On Emotional Difficulty Score - Heterogeneous Effects by Sex and Age
| Panel A. State Unemployment Rate | ||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| OLS: Mental Health Severity (0–3) | Probit: Likely Psychological Problem (0/1) | |||||||
| Males | Females | Age 4–11 | Age 12–17 | Males | Females | Age 4–11 | Age 12–17 | |
| Marginal Effect | 0.010* | 0.006* | 0.010** | 0.008 | 0.0039** | 0.0030** | 0.0037*** | 0.0036* |
| (SE) | (0.006) | (0.065) | (0.004) | (0.006) | (0.0019) | (0.0013) | (0.0012) | (0.0019) |
| Mean, Dep. Var. | 0.313 | 0.212 | 0.249 | 0.283 | 0.064 | 0.038 | 0.046 | 0.058 |
| Relative Effect of 1.51 P.P. Fall in Unemployment Rate | −4.8% | −4.3% | −6.1% | −4.3% | −9.2% | −11.9% | −12.1% | −9.4% |
| Panel B. State Housing Price Index | ||||||||
| OLS: Mental Health Severity (0–3) | Probit: Likely Psychological Problem (0/1) | |||||||
| Males | Females | Age 4–11 | Age 12–17 | Males | Females | Age 4–11 | Age 12–17 | |
| Marginal Effect | −0.072*** | −0.056*** | −0.046*** | −0.090*** | −0.023** | −0.017** | −0.014** | −0.028*** |
| (SE) | (0.022) | (0.021) | (0.017) | (0.022) | (0.009) | (0.007) | (0.005) | (0.009) |
| Mean, Dep. Var. | 0.313 | 0.212 | 0.249 | 0.283 | 0.064 | 0.038 | 0.046 | 0.058 |
| Relative Effect of 0.19 Point Rise in Housing Price Index | −4.4% | −5.0% | −3.5% | −6.0% | −6.8% | −8.5% | −5.8% | −9.2% |
| Sample size | 56,752 | 53,515 | 59,943 | 50,324 | 56,752 | 53,351 | 59,943 | 50,324 |
Note: Robust standard errors clustered on the state. A fall in unemployment rate of 1.51 percentage points and a rise in HPI of 0.19 represent one standard deviation improvements in economic conditions. Covariates are described in Table 2.
p-value <.10
p-value<.05
p-value<.01.
3.3. True effects, or effects on parental reporting?
The estimates that we have reported thus far could represent true effects of economic conditions on mental health, or they could also represent changes in parental reporting about children’s mental health status. We approach this issue by examining whether the main results are sensitive to including parental mental health as a covariate. This approach is limited in that parental mental health is an endogenous covariate. However, if the main results were sensitive to including parental mental health, our main results could reflect changes in parental reporting as the economy and parental mental health deteriorated rather than capturing changes in children’s mental health. Adult mental health in the NHIS is measured by Kessler’s K6 instrument for serious psychological distress, which is collected from the randomly-selected “sample adult” in each household (which could be a child’s parent or other adults in the household). We code levels of parental mental health as low psychological distress (0 ≥ K6 ≥ 4), moderate psychological distress (5 ≥ K6 ≥ 12), or severe psychological (13 ≥ K6 ≥ 24). (Kessler et al., 2003). Because 26% of the Table 3 and 4 sample were missing the K6 measure, we estimate models with and without parental mental health among parents with complete data. Model estimates are insensitive to including parental mental health (Appendix Table 1), suggesting that the main results are not driven by changes in parental reporting.5
3.4. Effects on Services for Emotional or Behavioral Problems
Next, we examine the effect of economic conditions on the use of special education services for children’s emotional problems. Only one behavioral service measure is available in the NHIS throughout our study period: whether a child used special education or early intervention services in the past 12 months specifically for an emotional or behavioral problem. This question was asked of all children under 18 years from 2001 onward, yielding a substantially larger sample size than the “sample child’s” mental health questions, although we focus on ages 4–17 for consistency with our analyses of mental health status. Approximately 2.4% of children aged 4–17 year were reported to have used special education or early intervention services for emotional or behavioral problems in the past 12 months.
This measure is limited in that special education or early intervention services represent an extreme measure of service use for emotional problems, and many children using mental health services do not use or qualify for such special education services. The supply of special education and early intervention services could also be counter-cyclical, as these services are largely financed by state and local governments, where budgets are more constrained in a poor economy. If so, this measure will underestimate the true underlying demand for these services.6 On the other hand, special education and early intervention services represent very intensive services for children with mental health problems and reflect problems that are long-lasting, as the NHIS questionnaire explicitly defines emotional or behavioral problems in this context to be chronic, and not short-term, difficulties. As such, we expect that any effects for this outcome will be for children who are already on the margin of using or not using these services. The special education measure is also unlikely to be affected by biased parental reporting, since children must be evaluated by multiple adults, not just parents, to qualify for special education services. Finally, special education services are expensive and largely publicly-financed, and any increases in the use of these services indicate that poor economic conditions have direct consequences for state and local education budgets. Education costs for special education students are estimated to be 90% higher than education costs for students without special needs, and the relative expense of these services is even higher in small school districts (Chambers, Parrish, & Harr, 2004).
In probit models without state-specific linear time trends, we find that falling unemployment rates, and rising housing prices, decrease the use of special education services for emotional problems (Table 6). A one-standard deviation improvement in the state-level unemployment rate decreases the use of special education services by 5.7% relative to the mean, and a one-standard deviation increase in housing prices decreases special education use by 3.2% relative to the mean. The magnitudes of these results are sensitive to controlling for state-specific linear time trends (which yields a bigger, less precise estimated effect for unemployment rates; and a smaller, insignificant effect for housing prices).
Table 6.
Probit Models of Special Education or Early Intervention Services for Emotional or Behavioral Problems
| Panel A. Effects of State Unemployment Rate | ||
| (1) | (2) | |
| Marginal Effect | 0.00091** | 0.00113* |
| (SE) | (0.0004) | (0.00058) |
| Mean, Dep. Var. | 0.024 | 0.024 |
| Relative Effect of 1.51 Percentage Point Fall in Unemployment Rate | –5.7% | –7.1% |
| Area-Specific Linear Time Trends | No | Yes |
| Panel B. Effects of State Housing Price Index | ||
| (1) | (2) | |
| Marginal Effect | –0.0041* | –0.0015 |
| (SE) | (0.0023) | (0.0024) |
| Mean, Dep. Var. | 0.024 | 0.024 |
| Relative Effect of 0.19 Point Rise in Housing Price Index | –3.2% | –1.2% |
| Area-Specific Linear Time Trends | No | Yes |
| Sample size | 240,006 | 240,006 |
Note: Robust standard errors clustered on the state. A fall in unemployment rate of 1.51 percentage points and a rise in HPI of 0.19 represent one standard deviation improvements in economic conditions. Covariates are described in Table 2.
p-value <.10
p-value<.05
p-value<.01.
3.5. Investigating Parental Employment as a Possible Mechanism
In this section we investigate potential mechanisms linking economic conditions to children’s mental health, focusing on parental employment because job loss and unemployment are among the main ways that economic conditions affect families and households. We posit that families likely to face unemployment during recessions (usually those with lower rates of employment overall), would be more likely to report declines in child mental health as unemployment rates rise or housing prices decline. Other potential mechanisms (e.g., income, stress, parental time use) are also strongly mediated by family-level employment (Kalil, 2013). Because parental employment status may be strongly influenced by mental health of family members, we prefer to not examine employment directly. Instead, we take two complementary approaches to understand the role that parental employment plays in explaining our results.
In the first approach to assessing the mediating role of parental employment, we follow earlier research which stratifies the analysis by factors related to employment, like educational attainment and race/ethnicity, since lower socioeconomic status is likely to be related to job loss during recessions (Charles & DeCicca, 2008). Thus, if unemployment effects are stronger within subgroups most likely to experience job loss during a poor economy, it might provide some evidence that the effects we observe are mediated by household-level employment outcomes. We stratify children by the highest level of parental educational attainment in the household, defined as less than a bachelor’s degree versus at least a bachelor’s degree. We also estimate models stratified by the child’s race and ethnicity (defined as non-Hispanic white or other). Recent research documents that lower educational attainment and racial/ethnic minority groups experience greater declines in employment during economic downturns (Hoynes et al., 2012).
The effects of unemployment rates and housing prices on the SDQ and emotional difficulty outcomes are stronger and only statistically significant for lower-education families (Table 7), which is suggestive of a parental employment mechanism. In contrast, even though economic conditions affected employment outcomes for different racial/ethnic groups in different ways, we find that economic conditions affected children’s mental health across racial/ethnic groups in mostly similar ways (Appendix Tables 2–3, Columns 1–2)).
Table 7.
Probability of Likely Psychological Problem - Heterogeneous Effects by Parental Education
| Panel A. State Unemployment Rates | ||||
| (1) | (2) | (3) | (4) | |
| Probit: Likely Psychological Problem (0/1) based on SDQ Scale | Probit: Likely Psychological Problem (0/1) based on Emotional Difficulty Score | |||
| Less than College Degree | At least College Degree | Less than College Degree | At least College Degree | |
| Marginal Effect | 0.003** | 0.003 | 0.0043*** | 0.0018 |
| (SE) | (0.002) | (0.002) | (0.0014) | (0.0015) |
| Mean, Dep. Var. | 0.050 | 0.024 | 0.058 | 0.038 |
| Relative Effect of 1.51 P.P. Fall in Unemployment Rate | −9.1% | −18.9% | −11.2% | −7.2% |
| Panel B. State Housing Price Index | ||||
| Probit: Likely Psychological Problem (0/1) based on SDQ Scale | Probit: Likely Psychological Problem (0/1) based on Emotional Difficulty Score | |||
| Less than College Degree | At least College Degree | Less than College Degree | At least College Degree | |
| Marginal Effect | −0.020** | −0.004 | −0.023*** | −0.013 |
| (SE) | (0.008) | (0.007) | (0.007) | (0.009) |
| Mean, Dep. Var. | 0.050 | 0.024 | 0.058 | 0.038 |
| Relative Effect of 0.19 Point Rise in Housing Price Index | −7.6% | −3.2% | −7.5% | −6.5% |
| Sample size | 65,563 | 28,564 | 76,581 | 33,686 |
Note: Robust standard errors clustered on the state. A fall in unemployment rate of 1.51 percentage points and a rise in HPI of 0.19 represent one standard deviation improvements in economic conditions. Covariates are described in Table 2.
p-value <.10
p-value<.05
p-value<.01.
In another approach, we restrict the sample to children in two-parent families and stratify by number of unemployed parents (none or any). This approach, also shown in Appendix Tables 2 and 3 (Columns 3–4), has the clear limitation that employment is endogenous and that differences across employment status will reflect a host of other factors that may be relevant to children’s mental health. With that caveat in mind, we do not find any significant effects of economic conditions on children in two-parent families where both parents are employed, and we find similar and at times larger, and imprecisely estimated, effects for children in families with at least one unemployed parent.
We also adapt methods used by Charles and DeCicca (2008), who were concerned with the relationship between economic conditions in a market and mental health. Our aim is to assess whether children with parents who are most likely to experience employment effects of economic downturns have larger mental health effects, relative to other children. In this approach, we predicted employment status usising a baseline year of data, since we do not want business cycle effects to influence our estimate of who is likely to be employed. Using the 2001 data, we estimated the probability someone was employed (stratified by sex) as a flexible function of age, race/ethnicity, and education to generate predicted employment status for all parents.7 We used coefficients from these models, and the observed demographics of parents in each year of our data to predict employment status. We then ranked according to the probability of having employed parents in their household (two-parent households were assigned the higher employment probability of the two parents). We then re-estimate our analyses after stratifying children by bottom quintile predicted parental employment, medium-predicted parental employment (quintiles 2, 3, and 4), and top quintile parental employment. If direct employment effects of economic downturns matter most for child mental health, we would predict that children of parents in the bottom quintile of predicted employment would be most likely to experience poor mental health in a downturn, and we would expect children of parents in the top quintile of predicted employment to experience the smallest impact on mental health.
Panels A and B in Appendix Table 4 present the estimated impacts of unemployment rates on (a) whether a child has an unemployed parent and (b) annual household income. The effect of unemployment rates on the likelihood of having an unemployed parent varies across the predicted-employment groups. For parents who are most likely to be employed the probability of unemployment is unrelated to state unemployment rates (Panel A, Column 3). As expected, the likelihood of parental unemployment rises with unemployment rates for the middle-predicted employment group, but the effect is considerably larger for the low-predicted employment group. On the other hand, unemployment rates have greater absolute effects on income for higher-predicted employment families, but the relative effects compared to mean family incomes are comparable across the three predicted-employment groups (Appendix Table 4, Panel B).
Appendix Table 4 also presents the effect of economic conditions on severe psychological problems based on the SDQ and on the Emotional Difficulties item, stratified by predicted-employment of parents in Panels C and D. If our main effects were driven by parental unemployment, we would expect to see the strongest effects on children’s mental health in the lowest predicted-employment quintile, and little-to-no effects in the highest predicted-employment quintile. We do not see that pattern of results. For the likelihood of severe psychological problems, there is no effect of unemployment rates for the lowest predicted-employment quintile, and the effects for the middle- and high-predicted employment groups are similar to each other (and both are statistically significant). The pattern of results for the binary emotional difficulties outcome is different, with strongest effects in the bottom quintile of predicted employment.8 The effects for the middle- and high-predicted employment groups are the same, and both are statistically significant at p<0.10. The results for the analogous models that use HPI as the measure of economic conditions are shown in Appendix Table 5. The pattern of results is similar to what is found for unemployment rates, with one exception. Housing prices only affect children’s mental health in the middle quintiles of predicted employment. In contrast to the effects of unemployment rates, HPI does not affect mental health for children whose families have high predicted employment. Taken together, these findings suggest that parental employment may be an important mediator of the effect of economic conditions on child mental health, but that parental employment is not the sole mediator and other mechanisms may also explain the effects of economic conditions on children’s mental health.
4. Discussion
We find that measures of mental health in children deteriorate when the economy worsens. The effects of economic conditions on child mental health are comparable regardless of whether we measure economic activity with unemployment rates or housing price indices. The magnitudes of the effects are comparable to other estimated effects of economic conditions on a variety of adult health outcomes. For example, prior research finds that a one percentage point drop in state unemployment rates decreased adult suicides by 1.3% (Ruhm, 2000) and decreased the likelihood of reporting fair or poor health among older adults by 2.0% to 11.2% (McInerney & Mellor, 2012). We find that a similar fall in unemployment rates decreased levels of mental health problem severity by 1.5% to 2.5%, and the probability of clinically meaningful mental health problems fell by 6.9% to 10.4%. Our results imply that when unemployment rates rose 5 percentage points during the Great Recession, the probability of clinically meaningful child mental health problems increased by 35% to 50%. Consistent with the rise in mental health problems during recessions, the likelihood of using special education and early intervention services decreases by 3.8% to 4.2% for each percentage point drop in unemployment rates. Changes in child mental health during recessions are important not just within a child’s family but also for the school districts serving them.
When we examine the extent to which unemployment within the household explains the relationships that we document, we do not uncover evidence that consistently supports a single mechanism. Children from some types of families likely to become unemployed in a bad economy have relatively large reductions in mental health, but children from other types of families likely to become unemployed in a bad economy do not. We infer from this mixed set of results that household-level unemployment does not appear to be the sole or main driver of our results. Income losses and fears of job losses that accompany a weak economy, even among the employed, offer other plausible mechanisms to explain the child mental health effects.
One important consideration is whether the effects that we report here reflect “true” effects on child mental health status, or whether economic conditions only affect parental reporting of child mental health. We have three arguments in favor of “true” effects. First, parent-reported SDQ scores correlate well with teacher and child assessments, and with independent clinical assessments (R. Goodman, 2001). Second, child mental health outcomes move independently of parent mental health, and the effect of economic conditions on child mental health are unchanged after controlling for parental mental health. Third, we find evidence that economic conditions affect the use of special education and early intervention services for emotional problems–a more objective measure of child mental health. We cannot definitively rule out changing parental perceptions as one explanation for our findings, but our results suggest that this would be unlikely to explain more than a small share of the effects we observe.
Our models estimate short-term child mental health responses to shocks in local economic conditions, and we do not answer questions regarding economy-wide and longer-lasting economic downturns, or whether the effects on mental health are transitory or persistent. However, even short-term mental health problems can have serious consequences in childhood and adolescence (Busch et al., 2014; Currie & Stabile, 2009). Furthermore, when asking respondents about special education, the NHIS explicitly refers to services for chronic, and not short-term, difficulties, offering support for the notion that child mental health effects persist over time. The effects on special education use also represent a large effect of economic conditions on special education systems and their financing. Among the 57.1 million non-institutionalized children ages 4–17 represented annually in the 2001–2013 NHIS, approximately 1.4 million children annually received special education specifically for emotional or behavioral problems. Our estimates suggest that a standard deviation increase in unemployment rates would increase the number of children in special education by at least 80,000 nationally. Under the assumption that the difference in annual spending between a special education student and a regular education student is approximately $8,250 in 2016 dollars (Chambers et al., 2004), this implies an annual increase in spending of approximately $660 million that is largely financed by state and local governments.
Along with providing new insight into the determinants of child mental health, our results have implications for policy responses to poor economic conditions. We confirm that the consequences of a bad economy extend beyond labor market participants. These spillover effects to child mental health suggest that policy responses to weak economic conditions may have larger effects than anticipated. Interventions like extending unemployment benefits to cushion the loss of income, for example, may have benefits for child health that get overlooked. Counter-cyclical investments in children’s mental health resources may also yield important benefits, given the short- and long-term negative consequences of poor mental health in childhood. A better understanding of the mechanisms linking economic conditions to child mental health would help guide the optimal design of policy response during recessions.
Acknowledgements
This work is supported by a Grant-in-Aid from the University of Minnesota Office of the Vice President for Research and by the Minnesota Population Center grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (5R24HD041023). We are grateful for helpful feedback from Padmaja Ayyagari, David Cutler, Christopher (Kitt) Carpenter, Daniel Eisenberg, and seminar participants at ASHEcon 2016, Cornell University, Johns Hopkins University, University of Minnesota, University of Wisconsin, Vanderbilt University and Yale University. We are especially grateful to Patricia Barnes of the National Center for Health Statistics for her assistance with accessing restricted National Health Interview Survey data. This research was conducted while the authors were Special Sworn Status researchers of the US Census Bureau at the Center for Economic Studies. Research results and conclusions expressed are those of the authors and do not necessarily reflect the views of the Census Bureau or the National Center for Health Statistics.
Funding: This study was funded by a Grant-in-Aid from the University of Minnesota Office of the Vice President for Research and by the Minnesota Population Center grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (5R24HD041023).
Appendix Table 1.
Regression Results, with and without Parental Mental Health Covariates
| Panel A. State Unemployment Rate | ||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| SDQ - Mental Health Severity (0–10) | SDQ - Likely Psych. Problem (0/1) | Emotional Difficulty - Mental Health Severity (0–3) | Emotional Difficulty - Likely Psych. Problem (0/1) | |||||
| With parental MH | ||||||||
| Marginal Effect | −0.013 | 0.047** | −0.001 | 0.003* | −0.004 | 0.007 | −0.001 | 0.006*** |
| (SE) | (0.013) | (0.016) | (0.001) | (0.002) | (0.004) | (0.006) | (0.001) | (0.002) |
| W/out parental MH | ||||||||
| Marginal Effect | −0.011 | 0.048*** | −0.001 | 0.003* | −0.003 | 0.007 | −0.001 | 0.006*** |
| (SE) | (0.015) | (0.018) | (0.001) | (0.002) | (0.004) | (0.006) | (0.001) | (0.002) |
| Panel B. State Housing Price Index | ||||||||
| SDQ - Mental Health Severity (0–10) | SDQ - Likely Psych. Problem (0/1) | Emotional Difficulty - Mental Health Severity (0–3) | Emotional Difficulty - Likely Psych. Problem (0/1) | |||||
| With parental MH | ||||||||
| Marginal Effect | −0.185** | −0.220** | −0.005 | −0.011 | −0.045* | −0.058*** | −0.076 | −0.022*** |
| (SE) | (0.064) | (0.079) | (0.007) | (0.008) | (0.023) | (0.027) | (0.076) | (0.078) |
| W/out parental MH | ||||||||
| Marginal Effect | −0.240*** | −0.236** | −0.009 | −0.013 | −0.0595** | −0.062*** | −0.012 | −0.023*** |
| (SE) | (0.066) | (0.093) | (0.0065) | (0.0085) | (0.025) | (0.021) | (0.008) | (0.008) |
| Area-specific linear time trends | No | Yes | No | Yes | No | Yes | No | Yes |
| Sample size | 69,553 | 69,553 | 69,553 | 69,553 | 80,669 | 80,669 | 80,669 | 80,669 |
Note: Results are from OLS (Columns 1–2, 5–6) and probit (Columns 3–4, 7–8) models with robust standard errors clustered on the state. Covariates are described in Table 2.
p<.10
p<.05
p<.01
Appendix Table 2.
Probability of Likely Psychological Problem, based on SDQ Scale – Heterogeneous Effects by Race/Ethnicity and Parental Employment Status
| Panel A. State-level Unemployment | ||||
| (1) | (2) | (3) | (4) | |
| White | Non-white | Both Parents Working | At least 1 Unemployed Parent | |
| Marginal Effect | 0.004** | 0.003** | 0.001 | 0.006 |
| (SE) | (0.002) | (0.001) | (0.001) | (0.004) |
| Mean, Dep. Var. | 0.042 | 0.039 | 0.027 | 0.055 |
| Relative Effect of 1-SD Fall in Unemployment | −13.3% | −11.6% | −5.6% | −16.5% |
| Panel B. State-level HPI | ||||
| (1) | (2) | (3) | (4) | |
| White | Non-white | Both Parents Working | At least 1 Unemployed Parent | |
| Marginal Effect | −0.014* | −0.014 | −0.006 | −0.012 |
| (SE) | (0.007) | (0.010) | (0.008) | (0.027) |
| Mean, Dep. Var. | 0.042 | 0.039 | 0.027 | 0.055 |
| Relative Effect of 1-SD Rise in Housing Prices | −6.3% | −6.8% | −4.2% | −4.1% |
| Sample size | 46,990 | 47,219 | 39,300 | 6,335 |
Note: Results are from probit models with robust standard errors clustered on the state. SDQ is the Strengths and Difficulties Questionnaire scale. Covariates include age, sex, race/ethnicity, parental education, parental age, and parental marital status. Models include a full set of state fixed effects and time fixed effects.
p-value <.10
p-value<.05
p-value<.01.
Appendix Table 3.
Probability of Likely Psychological Problem, based on Emotional Difficulty Score - Heterogeneous Effects by Race/Ethnicity and Parental Employment Status
| Panel A. State Unemployment Rate | ||||
| (1) | (2) | (3) | (4) | |
| White | Non-white | Both Parents Working | At least 1 Unemployed Parent | |
| Marginal Effect | 0.0025 | 0.0049*** | 0.0017 | 0.0012 |
| (SE) | (0.0016) | (0.0011) | (0.0014) | (0.0044) |
| Mean, Dependent Var. | 0.056 | 0.044 | 0.035 | 0.077 |
| Relative Effect of 1-SD Fall in Unemployment Rate | −6.7% | −16.8% | −7.3% | −2.4% |
| Panel B. State Housing Price Index | ||||
| (1) | (2) | (3) | (4) | |
| White | Non-white | Both Parents Working | At least 1 Unemployed Parent | |
| Marginal Effect | −0.017* | −0.019** | −0.0088 | −0.0385* |
| (SE) | (0.009) | (0.009) | (0.0074) | (0.0219) |
| Mean, Dependent Var. | 0.056 | 0.044 | 0.035 | 0.077 |
| Relative Effect of 1-SD Rise in Housing Prices | −5.8% | −8.2% | −4.8% | −9.5% |
| Sample size | 54,425 | 55,842 | 36,460 | 40,028 |
Note: Results are from probit models with robust standard errors clustered on the state. Covariates include age, sex, race/ethnicity, parental education, parental age, and parental marital status. Models include a full set of state fixed effects and time fixed effects.
p-value <.10
p-value<.05
p-value<.01.
Appendix Table 4.
Effects of Unemployment Rate on Health and Economic Outcomes, by Household Predicted Employment
| (1) Bottom quintile of predicted employment | (2) Three middle quintiles of predicted employment | (3) Top quintile of predicted employment | |
|---|---|---|---|
| Panel A. OLS: Whether Any Parent is Unemployed and Looking for Work | |||
| Marginal Effect | 0.0155*** | 0.0117*** | 0.0025 |
| (SE) | (0.0028) | (0.0019) | (0.0018) |
| Mean, Dep. Var. | 0.106 | 0.069 | 0.034 |
| Sample size | 20,678 | 69,703 | 20,726 |
| Panel B. OLS: Family Income ($) | |||
| Marginal Effect | −692.21** | −1,454.19*** | −2,559.84** |
| (SE) | (327.64) | (431.96) | (1,109.03) |
| Mean, Dep. Var. | $32,256 | $66,154 | $108,887 |
| Sample size | 20,678 | 69,703 | 20,726 |
| Panel C. Probit: Likely Psychological Problem (based on SDQ) | |||
| Marginal Effect | −0.0011 | 0.0037** | 0.0034* |
| (SE) | (0.002) | (0.0017) | (0.0019) |
| Mean, Dep. Var. | 0.053 | 0.043 | 0.029 |
| Sample size | 17,402 | 58,946 | 17,626 |
| Panel D. Probit: Likely Psychological Problem (based on Emotional Difficulty score) | |||
| Marginal Effect | 0.0070*** | 0.0026* | 0.0027* |
| (SE) | (0.0024) | (0.0013) | (0.0016) |
| Mean, Dep. Var. | 0.053 | 0.054 | 0.042 |
| Sample size | 20,410 | 68,987 | 20,533 |
Note: Robust standard errors are clustered on the state. Covariates are described in Table 2. Household predicted employment is described in the text.
p-value <.10
p-value<.05
p-value<.01.
Appendix Table 5.
Effects of HPI on Health and Economic Outcomes, by Household Predicted Employment
| (1) Bottom quintile of predicted employment | (2) Three middle quintiles of predicted employment | (3) Top quintile of predicted employment | |
|---|---|---|---|
| Panel A. OLS: Whether Any Parent is Unemployed and Looking for Work | |||
| Marginal Effect | −0.0568*** | −0.0371*** | −0.0164 |
| (SE) | (0.0175) | (0.0106) | (0.0115) |
| Mean, Dep. Var. | 0.106 | 0.069 | 0.034 |
| Sample size | 20,678 | 69,703 | 20,726 |
| Panel B. OLS: Family Income ($) | |||
| Marginal Effect | 3155.24 | 7765.45*** | 13475.40* |
| (SE) | (2161.76) | (2175.37) | (7079.99) |
| Mean, Dep. Var. | $32,256 | $66,154 | $108,887 |
| Sample size | 20,678 | 69,703 | 20,726 |
| Panel C. Probit: Likely Psychological Problem (Strengths & Difficulties) | |||
| Marginal Effect | −0.010 | −0.0157** | −0.0087 |
| (SE) | (0.018) | (0.0078) | (0.0095) |
| Mean, Dep. Var. | 0.053 | 0.043 | 0.029 |
| Sample size | 17,402 | 58,946 | 17,626 |
| Panel D. Probit: Likely Psychological Problem (based on Emotional Difficulty) | |||
| Marginal Effect | −0.0209* | −0.0206*** | −0.0116 |
| (SE) | (0.0123) | (0.0069) | (0.0108) |
| Mean, Dep. Var. | 0.053 | 0.054 | 0.042 |
| Sample size | 20,410 | 68,987 | 20,533 |
Note: Robust standard errors are clustered on the state. Covariates are described in Table 2. Household predicted employment is described in the text.
p-value <.10
p-value<.05
p-value<.01
Footnotes
We also estimated models with lagged measures of economic conditions. Those results for lags of 1–2 quarters are generally consistent with our main results.
Negative binomial models of the SDQ score and ordered probit models of the Emotional Difficulties item yielded similar results.
Linear probability model results are similar, but we prefer probit because of the low probabilities of the outcomes.
We also examine the effects of economic conditions on the items taken from four of the SDQ’s subscales (“emotional symptoms,” “peer relationships,” “hyperactivity/inattention,” and “conduct problems.” These estimates are less precise than the main results, but economic conditions are related to all but the “conduct problems” item.
In a previous version of this paper, we estimated a bivariate probit model of the joint response of parent and child mental health to changes in economic conditions. The motivation was that if the effects on parental and child mental health move together and not independently of each other, it would be more likely that child mental health estimates reflect changes in parental reporting rather than true changes in children’s mental health. However, referees noted that patterns of parent and child responses to economic conditions might covary for a variety of reasons, and as such the bivariate probit approach is uninformative for distinguishing “true” effects from parental reporting effects. We agree with the critique and as such this analysis is omitted.
Changes in Medicaid eligibility due to economic downturns do not increase the likelihood that a child receives special education services, as special education has a different eligibility process.
We included a quadratic in age, and interacted race/ethnicity with educational attainment.
The different patterns across predicted employment groups between the SDQ and Emotional Difficulties outcomes are not explained by the missing SDQ measures in 2008–2009. The Emotional Difficulties results are nearly identical when we exclude 2008–2009.
Conflict of Interest: The authors declare that they have no conflict of interest.
Contributor Information
Ezra Golberstein, University of Minnesota.
Gilbert Gonzales, Vanderbilt University School of Medicine.
Ellen Meara, Dartmouth College and NBER.
References
- Aizer A (2008). Peer Effects, Institutions, and Human Capital Accumulation: The Externalities of ADD. NBER; Working Paper, w14354. [Google Scholar]
- Bertrand M, Duflo E, & Mullainathan S (2004). How much should we trust differences-in-differences estimates? Quarterly Journal of Economics, 119(1), 249–275. doi:Doi 10.1162/003355304772839588 [DOI] [Google Scholar]
- Bourdon KH, Goodman R, Rae DS, Simpson G, & Koretz DS (2005). The Strengths and Difficulties Questionnaire: U.S. normative data and psychometric properties. J Am Acad Child Adolesc Psychiatry, 44(6), 557–564. doi:S0890–8567(09)61631–2 [pii] 10.1097/01.chi.0000159157.57075.c8 [DOI] [PubMed] [Google Scholar]
- Bradford WD, & Lastrapes WD (2014). A Prescription for Unemployment? Recessions and the Demand for Mental Health Drugs. Health Economics, 23(11), 1301–1325. [DOI] [PubMed] [Google Scholar]
- Busch S, Golberstein E, & Meara E (2014). FDA and ABCs: The Unintended Consequences of Antidepressant Warnings on Adolescent Human Capital Outcomes. Journal of Human Resources, 49(3), 540–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JY, & Cocco JF (2007). How do house prices affect consumption? Evidence from micro data. Journal of Monetary Economics, 54(3), 591–621. [Google Scholar]
- Carlson K (2015). Fear itself: The effects of distressing economic news on birth outcomes. Journal of Health Economics, 41, 117–132. doi: 10.1016/j.jhealeco.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Case A, Fertig A, & Paxson C (2005). The lasting impact of childhood health and circumstance. Journal of Health Economics, 24(2), 365–389. doi:DOI 10.1016/j.jhealeco.2004.09.008 [DOI] [PubMed] [Google Scholar]
- Cawley J, Moriya AS, & Simon K (2015). The impact of the macroeconomy on health insurance coverage: evidence from the Great Recession. Health Econ, 24(2), 206–223. doi: 10.1002/hec.3011 [DOI] [PubMed] [Google Scholar]
- Chambers JG, Parrish TB, & Harr JJ (2004). What Are We Spending on Special Education Services in the United States, 1999–2000?. Retrieved from http://www.csef-air.org/publications/seep/national/AdvRpt1.PDF
- Charles KK, & DeCicca P (2008). Local labor market fluctuations and health: Is there a connection and for whom? Journal of Health Economics, 27(6), 1532–1550. doi:DOI 10.1016/j.jhealeco.2008.06.004 [DOI] [PubMed] [Google Scholar]
- Conger RD, & Donnellan MB (2007). An interactionist perspective on the socioeconomic context of human development. Annual Review of Psychology, 58, 175–199. [DOI] [PubMed] [Google Scholar]
- Cotti C, & Simon D (2018). The Impact of Stock Market Fluctuations on the Mental and Physical Well-Being of Children. Economic Inquiry, 56(2), 1007–1027. doi: 10.1111/ecin.12528 [DOI] [Google Scholar]
- Currie J (2009). Healthy, Wealthy, and Wise: Socioeconomic Status, Poor Health in Childhood, and Human Capital Development. Journal of Economic Literature, 47(1), 87–122. [Google Scholar]
- Currie J, & Stabile M (2006). Child mental health and human capital accumulation: The case of ADHD. Journal of Health Economics, 25(6), 1094–1118. doi:DOI 10.1016/j.jhealeco.2006.03.001 [DOI] [PubMed] [Google Scholar]
- Currie J, & Stabile M (2009). Mental Health in Childhood and Human Capital In Gruber J (Ed.), An Economic Perspective on the Problems of Dsiadvantaged Youth. Chicago: University of Chicago Press for NBER. [Google Scholar]
- Currie J, Stabile M, Manivong P, & Roos LL (2010). Child Health and Young Adult Outcomes. Journal of Human Resources, 45(3), 517–548. [Google Scholar]
- Currie J, & Tekin E (2015). Is There a Link between Foreclosure and Health? American Economic Journal-Economic Policy, 7(1), 63–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davalos ME, & French MT (2011). This Recession Is Wearing Me Out! Health-Related Quality of Life and Economic Downturns. Journal of Mental Health Policy and Economics, 14(2), 61–72. [PubMed] [Google Scholar]
- Dave DM, & Kelly IR (2012). How does the business cycle affect eating habits? Social Science & Medicine, 74(2), 254–262. doi:DOI 10.1016/j.socscimed.2011.10.005 [DOI] [PubMed] [Google Scholar]
- Dehejia R, & Lleras-Muney A (2004). Booms, busts, and babies’ health. Quarterly Journal of Economics, 119(3), 1091–1130. doi:Doi 10.1162/0033553041502216 [DOI] [Google Scholar]
- DeNavas-Walt C, Proctor B, & Smith J (2012). Income, Poverty, and Health Insurane Coverage in the United States: 2011. Retrieved from Washington, DC: [Google Scholar]
- Fergusson DM, Horwood LJ, & Ridder EM (2007). Conduct and attentional problems in childhood and adolescence and later substance use, abuse and dependence: results of a 25-year longitudinal study. Drug Alcohol Depend, 88 Suppl 1, S14–26. doi: 10.1016/j.drugalcdep.2006.12.011 [DOI] [PubMed] [Google Scholar]
- Fletcher J, & Wolfe B (2008). Child mental health and human capital accumulation: The case of ADHD revisited. Journal of Health Economics, 27(3), 794–800. doi:DOI 10.1016/j.jhealeco.2007.10.010 [DOI] [PubMed] [Google Scholar]
- Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T, & Caldas-de-Almeida JM (2016). Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health, 16, 115. doi: 10.1186/s12889-016-2720-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gassman-Pines A, Ananat EO, & Gibson-Davis CM (2014). Effects of statewide job losses on adolescent suicide-related behaviors. Am J Public Health, 104(10), 1964–1970. doi: 10.2105/AJPH.2014.302081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman A, Joyce R, & Smith JP (2011). The long shadow cast by childhood physical and mental problems on adult life. Proceedings of the National Academy of Sciences of the United States of America, 108(15), 6032–6037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R (1999). The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry, 40(5), 791–799. [PubMed] [Google Scholar]
- Goodman R (2001). Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry, 40(11), 1337–1345. doi:S0890–8567(09)60543–8 [pii] 10.1097/00004583-200111000-00015 [DOI] [PubMed] [Google Scholar]
- Houle JN, & Light MT (2014). The home foreclosure crisis and rising suicide rates, 2005 to 2010. Am J Public Health, 104(6), 1073–1079. doi: 10.2105/AJPH.2013.301774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoynes H, Miller DL, & Schaller J (2012). Who Suffers During Recessions? Journal of Economic Perspectives, 26(3), 27–47. doi:Doi 10.1257/Jep.26.3.27 [DOI] [Google Scholar]
- Johnson RC, Kalil A, & Dunifon RE (2010). Mothers’ Work and Children’s Lives: Low-Income Families After Welfare Reform. Kalamazoo, MI: W.E. Upjohn Institute for Employment Research. [Google Scholar]
- Kalil A (2013). Effects of the Great Recession on Child Development. Annals of the American Academy of Political and Social Science, 650(1), 232–249. doi:Doi 10.1177/0002716213500453 [DOI] [Google Scholar]
- Kessler RC, Avenevoli S, Costello J, Green JG, Gruber MJ, McLaughlin KA, … Merikangas KR (2012). Severity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry, 69(4), 381–389. doi: 10.1001/archgenpsychiatry.2011.160369/4/381 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, … Zaslavsky AM (2003). Screening for serious mental illness in the general population. Arch Gen Psychiatry, 60(2), 184–189. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry, 62(6), 593–602. doi:62/6/593 [pii] 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Lin HZ, Ketcham JD, Rosenquist JN, & Simon KI (2013). Financial distress and use of mental health care: Evidence from antidepressant prescription claims. Economics Letters, 121(3), 449–453. [Google Scholar]
- Lindo JM (2015). Aggregation and the estimated effects of economic conditions on health. Journal of Health Economics, 40, 83–96. doi: 10.1016/j.jhealeco.2014.11.009 [DOI] [PubMed] [Google Scholar]
- Lupien SJ, King S, Meaney MJ, & McEwen BS (2000). Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biol Psychiatry, 48(10), 976–980. doi:S0006–3223(00)00965–3 [pii] [DOI] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, & Heim C (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci, 10(6), 434–445. doi: 10.1038/nrn2639 [DOI] [PubMed] [Google Scholar]
- McInerney M, & Mellor JM (2012). Recessions and seniors’ health, health behaviors, and healthcare use: Analysis of the Medicare Current Beneficiary Survey. Journal of Health Economics, 31(5), 744–751. doi:DOI 10.1016/j.jhealeco.2012.06.002 [DOI] [PubMed] [Google Scholar]
- McInerney M, Mellor JM, & Nicholas LH (2013). Recession depression: Mental health effects of the 2008 stock market crash. Journal of Health Economics, 32(6), 1090–1104. doi:DOI 10.1016/j.jhealeco.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLoyd V, Kaplan R, Purtell K, Hardaway C, & Smalls C (2009). Poverty and Socioeconomic Disadvantage in Adolescence In Lerner R & Steinberg L (Eds.), Handbook of Adolescent Psychology (3rd ed ed., Vol. 2). Hoboken, NJ: Wiley. [Google Scholar]
- Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, & Koretz DS (2010). Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics, 125(1), 75–81. doi: 10.1542/peds.2008-2598peds.2008-2598 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milligan K, & Stabile M (2011). Do Child Tax Benefits Affect the Well-being of Children? Evidence from Canadian Child Benefit Expansions. American Economic Journal-Economic Policy, 3(3), 175–205. doi:Doi 10.1257/Pol.3.3.175 [DOI] [Google Scholar]
- National Research Council and Institute of Medicine. (2009). Preventing Mental, Emotional, and Behavioral Disorders among Young People: Progress and Possibilities. Washington, D.C.: The National Academies Press. [PubMed] [Google Scholar]
- Pastor PN, Reuben CA, & Duran CR (2012). Identifying Emotional and Behavioral Problems in Children Aged 4–17 Years: United States, 2001–2007. National Health Statistics Reports, Number 48. [PubMed] [Google Scholar]
- Ringeisen H, Aldworth J, Colpe LJ, Pringle B, & Simile C (2015). Estimating the prevalence of any impairing childhood mental disorder in the national health interview survey. Int J Methods Psychiatr Res, 24(4), 266–274. doi: 10.1002/mpr.1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm CJ (2000). Are recessions good for your health? Quarterly Journal of Economics, 115(2), 617–650. doi:Doi 10.1162/003355300554872 [DOI] [Google Scholar]
- Ruhm CJ (2005). Healthy living in hard times. Journal of Health Economics, 24(2), 341–363. doi:DOI 10.1016/j.jhealeco.2004.09.007 [DOI] [PubMed] [Google Scholar]
- Ruhm CJ (2015). Recessions, Healthy No More? Journal of Health Economics, 42(3), 17–28. [DOI] [PubMed] [Google Scholar]
- Schaller J, & Stevens AH (2015). Short-Run Effects of Job Loss on Health Conditions, Health Insurance, and Health Care Utilization. Journal of Health Economics, 43, 190–203. [DOI] [PubMed] [Google Scholar]
- Seeman T, Thomas D, Merkin SS, Moore K, Watson K, & Karlamangla A (2018). The Great Recession worsened blood pressure and blood glucose levels in American adults. Proc Natl Acad Sci U S A, 115(13), 3296–3301. doi: 10.1073/pnas.1710502115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens-Davidowitz S (2013). Unreported Victims of an Economic Downturn. Working Paper. [Google Scholar]
- Stevens AH, Miller DL, Page ME, & Filipski M (2013). The Best of Times, the Worst of Times: Understanding Pro-Cyclical Mortality. Working Paper. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Berg GJ, Lindeboom M, & Portrait F (2006). Economic conditions early in life and individual mortality. American Economic Review, 96(1), 290–302. doi:Doi 10.1257/000282806776157740 [DOI] [PubMed] [Google Scholar]
- Weiland C, & Yoshikawa H (2012). The Effects of Large-Scale Economic Change and Policies on Children’s Developmental Contexts and Developmental Outcomes. Child Development Perspectives, 6(4), 342–350. [Google Scholar]