Abstract
Background: Transgender individuals experience unique vulnerabilities to intimate partner violence (IPV) and may experience a disproportionate IPV burden compared with cisgender (nontransgender) individuals.
Objectives: To systematically review the quantitative literature on prevalence and correlates of IPV in transgender populations.
Search Methods: Authors searched research databases (PubMed, CINAHL), gray literature (Google), journal tables of contents, and conference abstracts, and consulted experts in the field. Authors were contacted with data requests in cases in which transgender participants were enrolled in a study, but no disaggregated statistics were provided for this population.
Selection Criteria: We included all quantitative literature published before July 2019 on prevalence and correlates of IPV victimization, perpetration, or service utilization in transgender populations. There were no restrictions by sample size, year, or location.
Data Collection and Analysis: Two independent reviewers conducted screening. One reviewer conducted extraction by using a structured database, and a second reviewer checked for mistakes or omissions. We used random-effects meta-analyses to calculate relative risks (RRs) comparing the prevalence of IPV in transgender individuals and cisgender individuals in studies in which both transgender and cisgender individuals were enrolled. We also used meta-analysis to compare IPV prevalence in assigned-female-sex-at-birth and assigned-male-sex-at-birth transgender individuals and to compare physical IPV prevalence between nonbinary and binary transgender individuals in studies that enrolled both groups.
Main Results: We identified 85 articles from 74 unique data sets (ntotal = 49 966 transgender participants). Across studies reporting it, the median lifetime prevalence of physical IPV was 37.5%, lifetime sexual IPV was 25.0%, past-year physical IPV was 16.7%, and past-year sexual IPV was 10.8% among transgender individuals. Compared with cisgender individuals, transgender individuals were 1.7 times more likely to experience any IPV (RR = 1.66; 95% confidence interval [CI] = 1.36, 2.03), 2.2 times more likely to experience physical IPV (RR = 2.19; 95% CI = 1.66, 2.88), and 2.5 times more likely to experience sexual IPV (RR = 2.46; 95% CI = 1.64, 3.69). Disparities persisted when comparing to cisgender women specifically. There was no significant difference in any IPV, physical IPV, or sexual IPV prevalence between assigned-female-sex-at-birth and assigned-male-sex-at-birth individuals, nor in physical IPV prevalence between binary- and nonbinary-identified transgender individuals. IPV victimization was associated with sexual risk, substance use, and mental health burden in transgender populations.
Authors’ Conclusions: Transgender individuals experience a dramatically higher prevalence of IPV victimization compared with cisgender individuals, regardless of sex assigned at birth. IPV prevalence estimates are comparably high for assigned-male-sex-at-birth and assigned-female-sex-at-birth transgender individuals, and for binary and nonbinary transgender individuals, though more research is needed.
Public Health Implications: Evidence-based interventions are urgently needed to prevent and address IPV in this high-risk population with unique needs. Lack of legal protections against discrimination in employment, housing, and social services likely foster vulnerability to IPV. Transgender individuals should be explicitly included in US Preventive Services Task Force recommendations promoting IPV screening in primary care settings. Interventions at the policy level as well as the interpersonal and individual level are urgently needed to address epidemic levels of IPV in this marginalized, high-risk population.
PLAIN-LANGUAGE SUMMARY
Intimate partner violence (IPV) is a pervasive public health issue that can result in physical injury, mental illness, and even homicide. Less attention has been paid to IPV in transgender individuals, whose gender differs from the sex they were assigned at birth. We searched for existing studies about the prevalence and correlates of IPV victimization, perpetration, or service utilization in transgender populations. We found 85 relevant articles. Transgender individuals face high rates of IPV: on average, across studies, some 1 in 6 transgender individuals reported physical IPV, and 1 in 10 reported sexual IPV in the past year. Transgender people were 2.2 times more likely to experience physical IPV and 2.5 times more likely to experience sexual IPV than were cisgender people recruited for the same study. IPV victimization was linked to worse sexual health, mental health, and substance abuse outcomes in transgender individuals, pointing to IPV as a potential driver of health disparities. This study suggests that transgender people should be meaningfully included in IPV screening programs, and more should be done to increase access to resources such as domestic violence shelters. Future research should test IPV prevention interventions for this population that is disproportionately affected by violence.
Intimate partner violence (IPV)—defined as physical violence, sexual violence, stalking, psychological aggression, or coercive control by a current or former intimate partner1—is a pervasive public health issue that often results in physical injury, mental illness, negative sexual and reproductive health outcomes, and even homicide.2,3 Globally, IPV has disproportionate prevalence, severity, and impact on cisgender (i.e., individuals whose gender aligns with their sex assigned at birth [SAB]) women, affecting roughly 1 in 3 women, but also affects cisgender men.3–5 Emerging research demonstrates that transgender individuals (i.e., individuals whose gender is different from their SAB, including transgender men, transgender women, and nonbinary individuals) experience high levels of IPV victimization.6–12 An estimated 25 million people worldwide are transgender.13
In addition to common antecedents of IPV, including relationship stress and substance use,14 transgender individuals experience unique “trans-related vulnerability” to IPV and thus may be disproportionately affected by IPV compared with cisgender individuals.10,15,16 Abusers can seek to undermine transgender partners by misgendering them (using incorrect pronouns), exploiting insecurities linked to societal stigma (e.g., fear of not finding love outside the relationship because of transgender identity), or threatening to “out” them (i.e., reveal transgender identity to others) as a form of blackmail.9,15,17 Transgender individuals are also more likely to experience multiple sources of social isolation (e.g., rejection by family and friends) and economic vulnerability (e.g., employment discrimination or homelessness) that can increase dependency on a violent partner. These issues are more common among transgender individuals of color and disabled individuals.10,15 When seeking help from domestic violence shelters, police, or medical providers, transgender individuals are likely to face additional discrimination on the basis of gender identity.15,16,18,19
In the 2015 US Transgender Survey (n = 27 715), 54% reported some form of lifetime IPV: 35% physical IPV (e.g., being hit or slapped), 24% severe physical IPV (e.g., being beaten, burned, or harmed with a weapon), and 19% sexual IPV (e.g., being forced to do something sexual that was unwanted) by a partner, all rates comparable to or greater than those documented in the US population at large and cisgender women globally.2,3,15 Given rising recognition of epidemic levels of violence against transgender individuals globally,20,21 we undertook a global systematic review synthesizing the existing quantitative literature on the prevalence, correlates, and health outcomes of IPV victimization and perpetration, and on IPV service utilization in transgender populations.
METHODS
Full methods are included in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org). To identify articles for inclusion, we used PubMed and CINAHL database searches, forward and backward citation searches, hand searching journal and conference abstracts, Google searches for gray literature, and expert consultation. The database search was updated in November 2017 and again in July 2019 before publication. Articles were included if they were original research and contained quantitative data on IPV victimization, perpetration, or service utilization prevalence or correlates specifically for transgender individuals, or if authors were willing to provide data for transgender subsample(s) when contacted. Two independent reviewers (S. M. P., M. M., S. K., E. M.) conducted the screening for each article, and 1 reviewer conducted the extraction (S. M. P., S. K., M. M., E. M.), which another reviewer double-checked (S. M. P., E. M., S. K., M. M.). We requested data from authors for articles that did not present disaggregated IPV data for transgender subsample(s) but indicated that they had enrolled transgender participants. We extracted data with a standardized database collecting
IPV victimization prevalence,
IPV perpetration prevalence,
demographic correlates of victimization or perpetration,
health outcomes associated with victimization or perpetration,
utilization of IPV services (i.e., help seeking following an IPV incident with domestic violence shelters, medical providers, police, or others), and
methodological characteristics.
We extracted data on all IPV types (physical, sexual, and psychological and other forms of IPV [e.g., stalking]). We categorized IPV type as “any IPV” if the assessment tool combined multiple types of IPV into 1 question (e.g., “Has your partner hit you or forced you to have sex?”), if the article asked about IPV generally (e.g., “Have you ever experienced domestic violence?”), or if an article provided a summary statistic combining multiple types of IPV after reporting prevalence of each type separately.
We used random effects meta-analysis (metabin command in R [R Foundation for Statistical Computing, Vienna, Austria]) to compare any, physical, and sexual IPV prevalence in transgender participants versus (1) all cisgender participants, (2) cisgender men participants, and (3) cisgender women participants in studies that included a cisgender comparison group. We also used random effects meta-analysis to compare (1) any IPV, physical IPV, and sexual IPV prevalence in assigned-female-sex-at-birth (AFAB; may identify as male, man, nonbinary, etc.) and assigned-male-sex-at-birth (AMAB; may identify as female, woman, nonbinary, etc.) transgender participants and (2) physical IPV prevalence in binary- and nonbinary-identified transgender individuals in studies that reported IPV prevalence separately for each group.
RESULTS
From a review of more than 1229 records, 85 articles from 74 unique study data sets met all inclusion criteria (Appendix C, Figure A, available as a supplement to the online version of this article at http://www.ajph.org), representing 1 273 989 participants, including 49 966 transgender participants across studies (Appendix B, Table A, available as a supplement to the online version of this article at http://www.ajph.org). The median total sample size (inclusive of cisgender participants) across studies was 499 (interquartile range [IQR] = 150–2042), and the median transgender sample size was 91 (IQR = 29–232). Most included studies were conducted in the United States (73%; n = 54/74) and other high-income countries (Spain,22 Australia,23–25 Scotland,9 Canada,26–28 and France29: 12%; n = 9/74; Appendix B, Table A). The remainder were from middle-income settings (Thailand,8 South Africa,30,31 Jamaica,11 India,32 China,7 Brazil,33,34 Mexico,35 Haiti,36 and countries across Latin America37: 15%; n = 11/74). The majority of studies were peer-reviewed (88%; n = 65/74), and the remainder were reports from advocacy and research organizations9,23,26,38–41 (10%; n = 7/74) or unpublished data from a state survey.42,43
Among the 71 unique studies that enrolled transgender individuals rather than service providers, AMAB individuals participated in 78% (n = 55/71),6–9,11,15,22,23,26,29–38,40,42,44–77 and AFAB individuals participated in 44% (n = 31/71) of studies.6,9,15,22,23,26,29,31,35,37,38,40,42,47–52,56,61,62,65–67,71–75,78 While 28% (n = 20/71) of studies explicitly reported inclusion of nonbinary individuals,6,9,15,26,35,38,40,47,50–52,62,65–67,71–73,75,78 this is likely an underestimate attributable to frequent lack of disaggregation of nonbinary participants. Authors from 30 of the 71 studies did not publish disaggregated IPV data for transgender participants or other information necessary for inclusion in the review, but they provided these data when contacted.7,17,24,26,29–31,33–38,42,43,47,48,61,62,66,70,72,74,76,77,79–83 We excluded more than 40 articles representing more than 3000 transgender participants because, although they contained IPV data and recruited transgender participants, the authors were unresponsive to requests for disaggregated statistics for transgender participants.
Studies were predominantly cross-sectional convenience samples (Appendix B, Table B) recruited from diverse sites and usually multiple sites per study. A mix of self- (62%; n = 44/71) and interviewer-administered (34%; n = 24/71) data collection tools were used, with the majority of self-administered studies (61%; n = 27/44) occurring online. While some studies generically described staff as “trained,” only 230,58 explicitly reported training in population-specific cultural competency. None explicitly reported training study staff about sensitive IPV assessment. Although 66% (n = 47/71)7–9,11,15,17,23,26,28,29,32,34–36,38,40–46,48,49,51,52,54–60,62,64,66–69,71–73,77–79,84,85 of studies demonstrated some evidence of community engagement (i.e., “a process of inclusive participation that supports . . . authentic partnership” between researchers and community members affected by the research86(p1383)), extent of community-engagement methods varied greatly (see Appendix B, Table B for details).
Definitions of “intimate partner” also varied, including by relationship duration and whether sexual intimacy was required. While IPV was predominantly assessed using behavioral measures (e.g., “Has a boyfriend or girlfriend ever hit, slapped, or physically hurt you on purpose?”), 17% (n = 12/71)11,29,31,32,35,38,44,48,55,56,58,70 of studies used nonbehavioral measures (e.g., “Have you ever experienced domestic violence?”), and 4% (n = 3/71)24,53,84 measured domestic violence service utilization without directly assessing IPV victimization experience. Seven percent (n = 5/71) of studies9,39,45,64,87 developed transgender-specific IPV items (e.g., partner insulted them by telling them they were not a “real” woman or man), including 1 study that validated a trans-specific IPV measure.87 Twenty-three studies (32%)6,7,11,15,29,31,35,36,38,50,51,53,58,63–65,67–69,74,77,78,88 reported using a 2-step measure89 (i.e., 2 items separately assessing SAB and gender identity) to determine gender identity of participants.
Intimate Partner Violence in Transgender Populations
Lifetime report of experiencing any IPV ranged from 6.3%56 to 83.3%80 across 28 unique studies7,9,11,15,23,26,28,33,34,38,44,50–52,56,64–68,74,76–78,80,85,90,91 reflecting heterogeneous study populations and assessment tools (Table 1). Lifetime physical IPV ranged from 10.5%74 to 66.7%80 (median = 37.5%34,37) across 16 studies.9,15,23,34,37,42,43,54,57,58,60,66,74,77,80,87 Lifetime sexual IPV ranged from 5.0%22 to 66.7%80 (median = 25.0%57) across 14 studies.9,15,22,23,37,57,60,64,66,74,77,80,87
TABLE 1—
Prevalence of Any, Physical, or Sexual Intimate Partner Violence Victimization by Recall Period Among Transgender Individuals
| Article | Recall Period | Gender | Any IPV, % (No./Total No.) | Physical IPV, % (No./Total No.) | Sexual IPV, % (No./Total No.) |
| Lifetime | |||||
| Bazargan and Galvan44 | Lifetime | AMAB TG | 56.8 (125/220) | NA | NA |
| Castro et al.33,a | Lifetime | AMAB TG | 26.7 (8/30) | NA | NA |
| De Boni et al.34,a | Lifetime | AMAB TG | 41.7 (10/24) | 37.5 (9/24) | NA |
| DeVylder et al.80,a | Lifetime | TG (NS) | 83.3 (5/6) | 66.7 (4/6) | 66.7 (4/6) |
| Fernández-Rouco et al.22 | Lifetime, aged > 14 y | AMAB TG, AFAB TG | NA | NA | 5.0 (6/120) |
| FORGE38 | Lifetime | AMAB TG | Dating violence: 5.8 (8/138) | NA | NA |
| IPV/DV: 29.0 (40/138) | |||||
| FORGE38 | Lifetime | AFAB TG | Dating violence: 23.3 (47/202) | NA | NA |
| IPV/DV: 36.1 (73/202) | |||||
| FORGE38 | Lifetime | TG (NS) | Dating violence: 31.9 (29/91) | NA | NA |
| IPV/DV: 38.5 (35/91) | |||||
| Garthe et al.64 | Lifetime | AMAB TG | 41.7 (78/187) | NA | 16.0 (30/187) |
| Goldenberg et al.65 | Lifetime | AMAB TG | 43.6 (34/78) | NA | NA |
| Goldenberg et al.65 | Lifetime | AFAB TG | 30.4 (7/23) | NA | NA |
| Goldenberg et al.65 | Lifetime | NB | 60.0 (18/30) | NA | NA |
| Henry et al.66,a | Lifetime | AMAB TG | 72.4 (21/29) | 34.5 (10/29) | 17.2 (5/29) |
| Henry et al.66,a | Lifetime | AFAB TG | 76.9 (20/26) | 61.5 (16/26) | 46.2 (12/26) |
| Henry et al.66,a | Lifetime | NB | 65.2 (15/23) | 30.4 (7/23) | 34.8 (8/23) |
| Holt42,a | Lifetime | AMAB TG, AFAB TG | NA | 16.2 (55/340) | NA |
| Holt43,a | Lifetime | AMAB TG, AFAB TG | NA | 14.8 (26/176) | NA |
| James et al.15 | Lifetime | AMAB TG, AFAB TG, NB | 53.1 (14217/26 780) | 34.4 (9333/27 166) | 19.3 (5316/27 557) |
| Kattari et al.50 | Lifetime | AMAB TG, AFAB TG, NB | 37.8 (2438/6456)b | NA | NA |
| Keuroghlian et al.51,c | Lifetime | AMAB TG, AFAB TG | 33.1 (150/452) | NA | NA |
| Logie et al.11,a | Lifetime | AMAB TG | 37.5 (51/136) | NA | NA |
| Logie et al.28 | Lifetime | TG (NS) | 10.0 (1/10) | NA | NA |
| Langenderfer-Magruder et al.52 | Lifetime | AMAB TG, AFAB TG | 31.1 (38/122) | NA | NA |
| Martinez-Velez et al.67 | Lifetime | AMAB TG, AFAB TG, TG (NS) | 55.8 (29/52) | NA | NA |
| McDowell et al.78,d | Lifetime | AFAB TG | 66.4 (99/149) | NA | NA |
| Mimiaga et al.68 | Lifetime | AMAB TG | 41.7 (78/187) | NA | NA |
| Nemoto et al.58 | Lifetime | AMAB TG | NA | 22.0 (125/568) | NA |
| Peitzmeier et al.87,d | Lifetime | AFAB TG | NA | 39.5 (58/147) | 51.0 (75/147) |
| Pitts et al.23 | Lifetime | AMAB TG | 36.4 (24/66) | 16.7 (11/66) | 3.0 (2/66) |
| Pitts et al.23 | Lifetime | AFAB TG | 61.8 (21/34) | 26.5 (9/34) | 8.8 (3/34) |
| Qureshi et al.56 | Lifetime | AMAB TG, AFAB TG | 6.3 (2/32) | NA | NA |
| Reisner et al.85 | Lifetime | AMAB TG, AFAB TG | 25.8 (8/31) | NA | NA |
| Reisner et al.91,c | Lifetime | AFAB TG | 41.0 (71/173) | NA | NA |
| Risser et al.57 | Lifetime | AMAB TG | NA | 50 (34/67)e | 25 (17/67)e |
| Roch et al.9 | Lifetime | AMAB TG, AFAB TG | 80.0 (48/60) | 45.0 (27/60) | 46.7(28/60) |
| Salazar et al.58 | Lifetime | AMAB TG | NA | 55.4 (51/92) | NA |
| Swan et al.37,a | Lifetime | AMAB TG | NA | 37.5 (3/8) | 50.0 (4/8) |
| Taliaferro et al.74,a | Lifetime | AMAB TG | 22.9 (134/585) | 10.4 (61/587) | 13.0 (76/585) |
| Taliaferro et al.74,a | Lifetime | AFAB TG | 30.1 (410/1362) | 10.5 (143/1362) | 18.2 (249/1368) |
| Turell60 | Lifetime | AMAB TG | NA | 42.9 (3/7) | 28.6 (2/7) |
| Veale et al.26 | Lifetime | AMAB TG, AFAB TG | 27.0 (203/751)e | NA | NA |
| White Hughto et al.90,c | Lifetime | AMAB TG, AFAB TG | 33.3 (137/412) | NA | NA |
| Wilton et al.76,a | Lifetime | AMAB TG | 15.4 (2/13) | NA | NA |
| Yamanis et al.77,a | Lifetime | AMAB TG | 50.0 (19/38) | 21.1 (8/38) | 23.1 (9/39) |
| Zhang et al.7 | Lifetime | AMAB TG | 65.6 (40/61) | NA | NA |
| Past year | |||||
| Bukowski et al.92,f | Past year | AMAB TG | NA | 44.7 (220/492) | NA |
| Clements-Nolle et al.46 | Past year | AMAB TG, AFAB TG | NA | 18.9 (36/190) | NA |
| Griner et al.93,g | Past year | TG (NS) | NA | 10.3 (21/204) | 10.8 (22/204) |
| Hoxmeier94 | Past year | AMAB TG, AFAB TG | NA | 3.8 (3/79) | 6.3 (5/79) |
| Johns et al.82,h | Past year | TG (NS) | NA | 33.8 (593/1752) | 29.1 (374/1287) |
| Langenderfer-Magruder et al.62,a | Past year | AMAB TG, AFAB TG | 60 (9/15) | NA | NA |
| Mizuno et al.53 | Past yeari | AMAB TG | 3.7 (7/166)b | NA | NA |
| Scheer et al.72,a | Past year | AMAB TG | NA | 15.6 (5/32) | 9.4 (3/32) |
| Scheer et al.72,a | Past year | AFAB TG | NA | 19.0 (12/63) | 15.9 (10/63) |
| Scheer et al.72,a | Past year | NB | NA | 16.1 (22/137) | 13.1 (18/137) |
| Scheer et al.72,a | Past year | TG (NS) | NA | 16.1 (10/62) | 11.3 (7/62) |
| Smith et al.59 | Past year | AMAB TG | NA | NA | 3.2 (2/63) |
| Sterzing et al.73 | Past year | AMAB TG | NA | 11.8 (2/19)j | NA |
| Sterzing et al.73 | Past year | AFAB TG | NA | 15.1 (7/47) | NA |
| Sterzing et al.73 | Past year | AMAB NB | NA | 14.7 (7/52) | NA |
| Sterzing et al.73 | Past year | AFAB NB | NA | 12.6 (24/189) | NA |
| Valentine et al.6 | Past year | AMAB TG | 12.1 (19/157) | 8.9 (14/157) | 7.6 (12/157) |
| Valentine et al.6 | Past year | AFAB TG | 6.6 (11/167) | 4.8 (8/167) | 3.0 (5/167) |
| Valentine et al.6 | Past year | NB | 8.2 (16/194) | 5.2 (10/194) | 5.2 (10/194) |
| Valentine et al.6 | Past year | TG (NS) | 9.1 (18/197) | 5.6 (11/197) | 5.1 (10/197) |
| Walls et al.75 | Past year | AMAB TG | NA | 39.7 (25/63) | NA |
| Walls et al.75 | Past year | AFAB TG | NA | 27.5 (28/102) | NA |
| Walls et al.75 | Past year | NB | NA | 48.5 (32/66) | NA |
| Whitfield et al.83,g | Past year | TG (NS) | NA | 10.0 (20/201) | 10.4 (21/201) |
| Woulfe et al.17,a | Past year | TG (NS) | NA | 9.2 (13/142) | 11.3 (16/142) |
| Zalla et al.36,a | Past year | AMAB TG | NA | 33.9 (37/109) | NA |
| Other recall periods | |||||
| Askevis-Leherpeux et al.29,a | During an “index period” during which gender incongruence or distress may have been particularly prominent | AMAB TG, AFAB TG | 8.7 (6/69) | NA | NA |
| Bhochhibhoya et al.79,a | By current or recent dating partner while in college | TG (NS) | NA | NA | 37.5 (3/8) |
| Campbell et al.31,a | During an “index period” during which gender incongruence or distress may have been particularly prominent | AMAB TG, AFAB TG | 3.5 (2/57) | NA | NA |
| Cantor et al.40 | Since enrollment (graduate students) | AMAB TG, AFAB TG | 17.8 (87/490) | 8.6 (42/490) | NA |
| Cantor et al.40 | Since enrollment (undergraduates) | AMAB TG, AFAB TG | 22.8 (207/908) | 9.7 (88/908) | NA |
| Cantor et al.40 | Since start of 2014 term (graduate students) | AMAB TG, AFAB TG | 10.2 (50/490) | NA | NA |
| Cantor et al.40 | Since start of 2014 term (undergraduates) | AMAB TG, AFAB TG | 15.3 (139/908) | NA | NA |
| Dank et al.95 | Ever with current or most recent partner | AMAB TG, AFAB TG | NA | 88.9 (16/18) | 61.1 (11/18) |
| Edwards et al.47,a | Past 2 y | NB | NA | 30.4 (7/23) | NA |
| Edwards et al.47,a | Past 2 y | AMAB TG | NA | 50.0 (2/4) | NA |
| Edwards et al.47,a | Past 2 y | AFAB TG | NA | 40.0 (4/10) | NA |
| Fedina et al.81,a | Since enrollment | TG (NS) | NA | NA | NA |
| Flentje et al.48 | Current | AFAB TG | 30.8 (4/13) | NA | NA |
| Flentje et al.48 | Current | AMAB TG | 13.6 (3/22) | NA | NA |
| Guadamuz et al.8 | Other | AMAB TG | NA | NA | 4.2 (20/474) |
| Lane et al.30,a | Past 6 mo | AMAB TG | 0 (0/6) | NA | NA |
| Logie et al.96 | Adulthood | AMAB TG | 26.5 (36/137) | NA | NA |
| Nemoto et al.54 | Ever, aged < 18 y | AMAB TG | NA | NA | 2.5 (14/564) |
| Nemoto et al.54 | Adulthood | AMAB TG | NA | NA | 4.9 (28/568) |
| Odo and Hawelu55 | Other | AMAB TG | 20.0 (20/100)k | NA | NA |
| Parsons et al.69 | Past 5 y | AMAB TG | 65.1 (138/212) | NA | NA |
| Petering et al.70,a | Past 3 mo | AMAB TG | NA | 0 (0/3) | NA |
| Reuter et al.88,l | Up to 3 partners in the past 6 mo | AMAB TG | 66.7 (6/9) | 44.4 (4/9) | NA |
| Reuter et al.88,l | Up to 3 partners in the past 6 mo | AFAB TG | 0 (0/7) | 0 (0/7) | NA |
| Robles et al.35,a | During an “index period” during which gender incongruence or distress may have been particularly prominent | AMAB TG, AFAB TG, NB | 11.2 (28/250) | NA | NA |
| Sinha et al.32 | Past 3 mo | AMAB TG | NA | NA | 5.6 (5/90) |
| Smith et al.59 | Adolescence (aged 12–17 y) | AMAB TG | NA | NA | 3.2 (2/63) |
| Smith et al.59 | Adulthood (aged ≥ 25 y) | AMAB TG | NA | NA | 9.5 (6/63) |
| Smith et al.59 | Young adulthood (aged 18–24 y) | AMAB TG | NA | NA | 15.9 (10/63) |
| Spittal et al.24,a | Other | AMAB TG, AFAB TG | 5.7 (5/88)b | NA | NA |
| Whitton et al.61,a,l | Up to 3 partners in the past 6 mo at any of 6 study visits | AMAB TG | 66.7 (8/12) | 50.0 (6/12) | 50.0 (6/12) |
| Whitton et al.61,a,l | Up to 3 partners in the past 6 mo at any of 6 study visits | AFAB TG | 50.0 (4/8) | 50.0 (4/8) | 25.0 (2/8) |
| Zakrison et al.97 | Current | AMAB TG, AFAB TG | 100.0 (1/1) | NA | NA |
| Zhang et al.7,a | Ever with current partner | AMAB TG | NA | 31.0 (9/29) | 61.9 (13/21) |
Note. AFAB = assigned-female-at-birth; AMAB = assigned-male-at-birth; DV = domestic violence; IPV = intimate partner violence; NA = information not available; NB = nonbinary or genderqueer; SAB = sex assigned at birth; TG = transgender; TG (NS) = transgender (not specified)—transgender, but gender identity or SAB of participants not available. Articles with prevalence estimates for multiple recall periods or populations are reported on multiple rows. Samples of exclusively IPV survivors reporting prevalence of specific types of IPV (e.g., Heintz et al.49 and Scheer and Baams71) are not included as any IPV prevalence is 100%. “Any IPV” indicates either a single question that includes multiple types of IPV (e.g., “Has your partner hit you or forced you to have sex?”) or a summary measure of IPV across multiple types of IPV assessed in the study. Studies with AMAB TG or AFAB TG participants may include NB participants under those terms without necessarily assessing for nonbinary identity or providing disaggregated prevalence estimates for nonbinary participants. Gender is standardized across studies as AMAB TG, AFAB TG, or NB regardless of language the original study may have used around gender (e.g., “transmasculine individuals” or “transgender women”) for greater consistency.
Some prevalence data not published in article; authors provided data upon contact.
Prevalence defined as percentage of individuals who accessed a domestic violence service. Other articles that used the same data set (the National Transgender Discrimination Survey) were not reported again in this table.
Articles used the same data set.
Articles used the same data set.
Prevalence given in article, number/total number is approximate.
Bukowski et al.92 article with larger sample size represented in Table 1 because the other Bukowski et al.63 article uses a subsample from the same data set.
Articles use the same data set and, therefore, Whitfield et al.83 sample is not represented in the text of the results when summarizing findings around past-year prevalence, to avoid double-counting this study sample.
Weighted prevalence estimates reported by Johns et al.82 in the article were 26.4% for physical IPV and 22.9% for sexual IPV. Raw data were obtained from the authors.
Recall period vague in article.
Sterzing et al.73 used multiple imputation to report prevalence estimates. Numerators are approximated by applying the percentage to the reported sample size (denominator) and rounding.
“By informal count” “at least 20” of 100 transgender participants experienced IPV.
Articles used the same data set.
Past-year physical IPV ranged from 3.8%92 to 44.7%93 (median = 16.7%72) across 11 studies.6,17,36,46,72,73,75,82,92–94 Past-year sexual IPV ranged from 3.2%59 to 29.1%82 (median = 10.8%93) across 7 studies.6,17,59,72,82,93,94 Twenty-three studies measured IPV prevalence using other reference periods, including partnership-based time periods or time since enrollment in college.7,8,24,29–32,35,40,47,48,54,55,59,61,69,70,79,81,88,95–97
Twenty-four studies6,7,9,15,17,23,37,40,41,60,64,66,71,72,74,77,80,81,83,87,88,93–95 assessed prevalence of psychological and other types of IPV, including threats (ranging from 19.8% to 60.0%9), psychological IPV (8.9%53–83.3%80), controlling behaviors (1.8%6–60%9), isolation (5.4%6–30%9), stalking (0.8%40–28.6%60), and abuse targeting gender identity (17.6%64–73.3%9) (reference periods vary; see Appendix B, Table C for details). These forms of abuse were usually as or more prevalent than physical or sexual IPV.
Transgender vs Cisgender Disparities
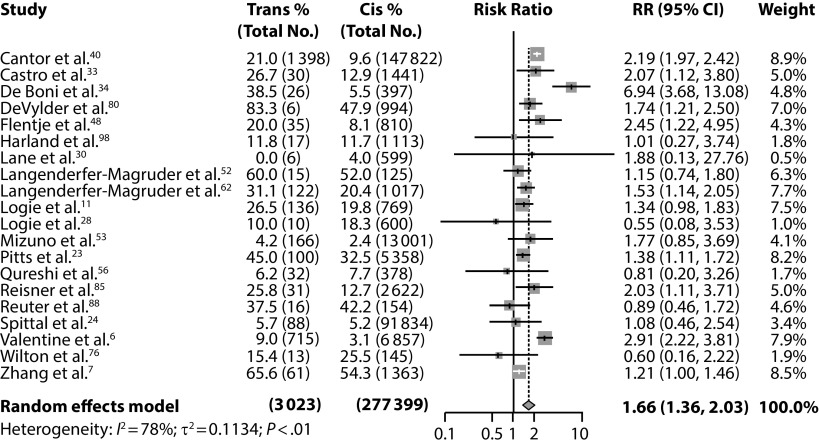
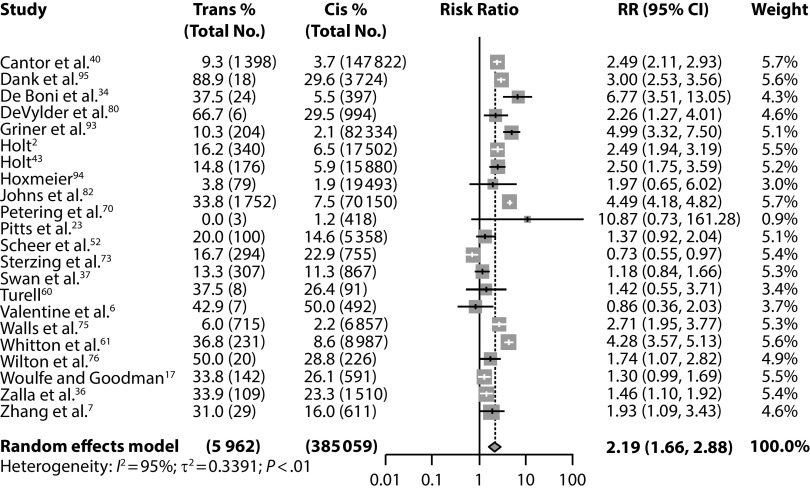
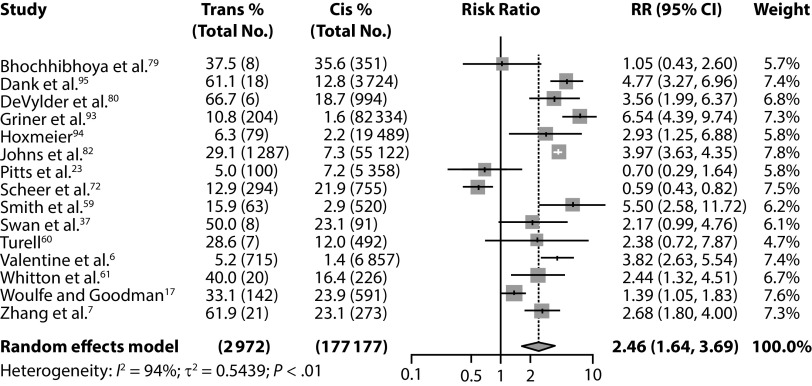
Transgender participants were 1.66 times more likely to experience any IPV than were cisgender participants (95% confidence interval [CI] = 1.36, 2.03) across 20 studies enrolling 3023 transgender and 277 399 cisgender participants (Figure 1).6,7,23,24,30,40,48,52,53,56,85,88 Transgender participants were more than twice as likely to experience both physical IPV (risk ratio [RR] = 2.19; 95% CI = 1.66, 2.88; n = 5962 transgender participants; n = 385 059 cisgender participants across 21 studies; Figure 2) and sexual IPV (RR = 2.46; 95% CI = 1.64, 3.69; n = 2972 transgender participants; n = 177 177 cisgender participants across 15 studies; Figure 3) as compared with cisgender participants. Cisgender comparison groups for studies in these meta-analyses were (1) lesbian, gay, and bisexual (LGB) men and women17,23,37,52,56,60–62,72,73,88,96; (2) men and women living with HIV or other populations with a higher-than-population-average proportion of LGB individuals6,33,36,48,53,59,70,85; (3) men who have sex with men7,30,34; or (4) general population men and women.24,28,40,42,43,75,79,80,82,93–95,98 Transgender participants had greater IPV disparities compared with cisgender men, than compared with cisgender women, but had significantly higher IPV prevalence compared with both groups (Appendix C, Figures B–G). School-based samples of middle-school, high-school, or college students were some of the largest studies and featured the largest transgender–cisgender disparities in physical IPV (RR = 2.89; 95% CI = 2.20, 3.80; Appendix C, Figure H) and sexual IPV (RR = 3.91; 95% CI = 2.74, 5.59; Appendix C, Figure I).
FIGURE 1—
Forest Plot Comparing Prevalence of Any Intimate Partner Violence Victimization Between Transgender and Cisgender Participants Across 20 Studies That Included Transgender and Cisgender Participants
Note. CI = confidence interval; RR = risk ratio.
FIGURE 2—
Forest Plot Comparing Prevalence of Physical Intimate Partner Violence Victimization Between Transgender and Cisgender Participants Across 21 Studies That Included Transgender and Cisgender Participants
Note. CI = confidence interval; IPV = intimate partner violence; RR = risk ratio. Whitton et al.61 provided transgender prevalence data, but not cisgender prevalence data, upon request. Cisgender prevalence is estimated by applying their reported adjusted odds ratio of 2.46 (95% CI = 1.24, 4.92). Reuter et al.88 reported comparison data, but it is not included because it was published in an earlier report with a smaller sample size from the same data set as Whitton et al.61 Whitfield et al.83 and Griner et al.93 used data from the same study; only Griner et al.93 was included in the meta-analysis. Woulfe et al.17 included past-year and adult IPV. The estimates for adult IPV were included because they had the greatest number of events for estimate stability. Johns et al.82 and Zalla et al.36 provided unweighted prevalence data; the raw number/total number is reported here and differs from weighted prevalence percentage reported in the original articles.
FIGURE 3—
Forest Plot Comparing Prevalence of Sexual IPV Victimization Between Transgender and Cisgender Participants Across 15 Studies That Included Transgender and Cisgender Participants
Note. CI = confidence interval; IPV = intimate partner violence; RR = risk ratio. Johns et al.82 provided unweighted prevalence data; the raw number/total number is reported here and differs from weighted prevalence percentage reported in the original article. Smith et al.59 included estimates for victimization during adolescence, young adulthood, adulthood, and past year. The estimates for young adulthood were included here because they had the greatest number of events for estimate stability. Results were qualitatively similar when other time periods were used in a sensitivity analysis. Whitfield et al.83 and Griner et al.93 used data from the same study; only Griner et al.93 was included in the meta-analysis. Woulfe et al.17 included past-year and adult IPV. The estimates for adult IPV were included because they had the greatest number of events for estimate stability. Whitton et al.61 provided transgender prevalence data but not cisgender prevalence data when requested from the authors. Cisgender prevalence was estimated by applying their reported adjusted odds ratio of 3.42 (95% CI = 1.85, 6.33).
Sixteen studies measured psychological or other forms of IPV in transgender and cisgender participants.6,7,17,23,37,40,41,60,71,72,83,88,93–95,98 Psychological or other forms of IPV were significantly more prevalent for transgender than for cisgender participants6,7,23,40,41,83,93–95 in some studies, but differences were not significant in others.17,37,71,72,98
Demographic and Health Correlates
There was no significant difference in the prevalence of any IPV (RR = 0.88; 95% CI = 0.68, 1.14; n = 1087 AMAB participants; n = 1835 AFAB participants), physical IPV (RR = 1.02; 95% CI = 0.77, 1.34; n = 1018 AMAB participants; n = 2007 AFAB participants), or sexual IPV (RR = 0.57; 95% CI = 0.27, 1.20; n = 869 AMAB participants; n = 1658 AFAB participants) between AMAB and AFAB participants (Appendix C, Figures J–L). Just 7 studies provided disaggregated prevalence estimates for nonbinary and binary transgender participants.6,47,65,66,72,73,75 There was no significant difference in physical IPV victimization between nonbinary and binary transgender participants (Appendix C, Figure M; RR = 1.03; 95% CI = 0.74, 1.44; n = 661 nonbinary participants; n = 664 binary participants across 5 studies).
IPV victimization was associated with disability,15 homelessness,15 immigration status,15 race/ethnicity15,54 (though not in all studies65), incarceration,65 and undergraduate versus graduate status (Appendix B, Table D).40 IPV victimization was not associated with social gender transition91 or self-esteem.45,65 IPV victimization was associated with bullying,90 family assault,90 family harassment,90 general victimization,45 repeated gender-related victimization,65 and everyday discrimination90 (depending on model parameters91).
Eleven studies11,15,45,46,51,58,63,65,90–92 measured associations between some type of IPV and sexual health, substance use, or mental health outcomes in a population of transgender individuals (Appendix B, Table E). Any IPV victimization is significantly associated with sexual risk measures (partner count,91 transactional sex,11,15,65 sexually transmitted infection diagnosis,91 unprotected sex45,91), substance use (recent substance use,51 polysubstance abuse,45 substance use treatment51), and mental health (depression,90 posttraumatic stress disorder,91 avoidant coping90) in transgender populations. There was mixed evidence of an association between any IPV victimization and HIV status.45,65
Physical IPV victimization was associated in individual studies with HIV viral suppression,63 sex work,15 and depressive symptoms,92 but unassociated with HIV status,65 HIV diagnosis,63 and inconsistent condom use.46 No study examined health correlates of sexual IPV, and just 1 reported any correlates of psychological or other forms of IPV.15
Perpetration by Transgender Individuals
Four small studies (n = 837–3847) measured IPV perpetration by transgender participants (Appendix B, Table F).37,47,85,95 Two studies noted that while transgender individuals (n = 17 and n = 31) reported higher prevalence of victimization compared with cisgender participants, they also reported higher perpetration85,95; 1 study found no significant difference in perpetration.37
Service Provision to Transgender Populations
We did not identify any study that developed or tested an IPV prevention intervention with transgender participants. Twelve studies provided data on IPV service provision to transgender survivors (Appendix B, Table G).15,23,25,27,50,52,53,71,84,99–101 Discrimination at domestic violence shelters was common and significantly associated with being AMAB versus AFAB,15,99 being perceived as transgender,100 having a disability,50 and identifying as American Indian, multiracial, or Latino versus White.50 Ford et al. found that service providers (ranging from shelter staff to law enforcement officials) reported feeling uncomfortable serving transgender clients,101 and Du Mont et al. found that sexual assault forensic nurses were unprepared to work with transgender patients,27 though Riggs et al. demonstrated that a training intervention can increase service providers’ skills in working with transgender women.25
DISCUSSION
Evidence synthesized in this review demonstrates that transgender individuals are at 2 to 3 times higher risk of physical and sexual IPV compared with cisgender individuals, regardless of SAB. Several studies also suggest high risk of psychological and other forms of IPV, including a growing number that document trans-specific forms of IPV. Echoing research in cisgender men and women in which gender disparities in victimization are most pronounced for sexual IPV and less pronounced for physical and psychological IPV,2 we found the largest gender disparities between transgender and cisgender populations were in sexual IPV victimization. However, transgender individuals were still more than twice as likely as were cisgender individuals to experience even physical IPV. Population-level IPV disparities may be even higher than estimated in this review, as LGB individuals were overrepresented in most cisgender comparison samples; LGB populations may have elevated IPV prevalence relative to heterosexuals.4 Indeed, studies with some of the largest disparities came from large, school-based samples in which the cisgender comparison group included mostly heterosexual individuals.42,43,75,82,83,93 Our review demonstrates that IPV is a risk factor for multiple health conditions, including poor sexual health, poor mental health, and substance use in transgender populations. The high IPV prevalence documented in this review indicates an urgent need for research and interventions for primary and secondary prevention of IPV in transgender populations.
Although this review identifies substantive research on IPV in transgender populations, the literature is still emerging, with the majority of studies occurring within the past 10 years in high-income settings. Because considerable funding for both transgender health and violence research comes from HIV funding, study populations were disproportionately high risk and AMAB. Despite this, the largest studies were community-based or school-based surveys that enrolled transgender communities broadly, not just those most at risk for HIV. Studies recruited from diverse and oftentimes multiple sites; IPV prevalence can vary greatly by site, representing a potential source of bias. However, we are not aware of any population-based violence-focused survey, from the Demographic and Health Surveys domestic violence module to the US National Intimate Partner Violence and Sexual Violence Survey, that assesses transgender identity and has the sample size to report transgender-specific estimates. Just 2 representative population-based studies were included in this review; both were high-school based samples with nonvalidated gender identity measures and limited focus on violence.75,82
Until the systematic exclusion of transgender individuals from population-based surveillance ends (i.e., until gender identity measures are routinely included in population-based violence surveys, violence measures that have been validated in transgender populations are created and included in population-based surveys, interviewers are trained to work respectfully with transgender participants, and investment in oversampling occurs to allow for reporting of transgender-specific prevalence estimates), transgender individuals will not have access to the same level of evidence around IPV that cisgender individuals do. Until such a time, large surveys with multipronged community-engaged recruitment strategies (e.g., US Transgender Survey15) represent compelling evidence.
Extant literature on IPV in transgender populations is hampered by numerous limitations. First, disaggregated information is often not provided for transgender and cisgender individuals when they are enrolled in the same study. There were 45 additional articles we could not include because of lack of disaggregated data. There is also significant heterogeneity in how transgender and IPV are defined, making it difficult to compare study populations and outcomes. Worst are studies in which the interviewer assigns the participant gender based on appearance,8 but even single-item assessments, such as providing gender options of “male,” “female,” and “transgender,” can result in substantial misclassification bias.102
One fifth of studies used nonbehavioral measures of IPV—known to underestimate prevalence compared with measures that ask about specific abusive behaviors103—or did not state the source of their measures. Even validated behavioral measures may underestimate prevalence in transgender populations, as they were developed for heterosexual cisgender women and may lack content validity.87,104 Research to validate IPV measures for lesbian, gay, bisexual, transgender, or queer populations broadly17,72 or transgender populations specifically87 is nascent. Lack of interviewer training in sensitively assessing IPV, particularly with transgender individuals, may have resulted in underestimation of IPV prevalence, perhaps differentially in transgender individuals. Standardizing measures of IPV will decrease heterogeneity, and more attention to disaggregated prevalence estimates for transgender subpopulations (e.g., AMAB, AFAB; nonbinary; racial/ethnic groups) in future research will allow for less heterogeneous estimates of prevalence by subpopulation.
We did not identify any study that developed or tested the efficacy of transgender-specific IPV primary prevention interventions. IPV prevention often focuses on school- and college-aged individuals broadly or cisgender women specifically.105 Evidence suggests that IPV victimization may be high over the life course for transgender individuals, with IPV disparities already emerging in middle and high school–28,42,43,73–75,82,95 and college-aged40,83,93,94 transgender individuals, making interventions aimed at adolescents critical. Peer education around what IPV looks like for transgender communities may prevent abuse and empower survivors. Some HIV prevention interventions for transgender women incorporate healthy relationship modules10; such studies could be leveraged to include a greater focus on IPV prevention. Interventions that have been shown to reduce IPV against cisgender women in global settings, such as community mobilization, economic empowerment, and cash transfer interventions,106 could be adapted for transgender individuals, albeit with careful implementation research to address the potential for increasing abuse depending on local context. Structural interventions, such as laws reducing barriers to legal name and gender marker changes or antidiscrimination legislation within housing and employment, could reduce vulnerability to IPV by increasing access to resources and decreasing dependency on abusive partners.
In secondary IPV prevention and response, more research is needed on service provision to transgender IPV survivors, including interventions with providers that can improve quality of care. Only 1 US study25 tested an intervention to improve transgender competency among domestic violence service providers and police, despite documentation of extensive maltreatment.15 Innovative community-based IPV response in high- and low-income settings could include “crisis response teams” (similar to those that have been formed within sex worker communities), transgender survivor support groups, and self-help materials created by and for transgender survivors. Health care providers are the most common people that cisgender women first disclose to when seeking formal help for IPV,5 but clinical settings are often sites of abuse and revictimization for transgender individuals.15 The US Preventive Services Task Force only recommends routine IPV screening in primary care settings for “women of childbearing age”107; similarly, the World Health Organization’s 2013 clinical recommendations make no mention of transgender individuals.5 Making clinical guidelines and clinical care more inclusive for transgender patients is critical.
Despite calls in the violence literature to intervene with abusive partners rather than victims,106 no studies included in the review explored the characteristics of abusive partners for transgender victims of IPV. In addition, only 4 small studies measured IPV perpetration by transgender individuals. Despite their advantages, behavioral measures of IPV have been criticized for giving the impression that cisgender women and men perpetrate IPV equally, even though women are more likely to use violence in self-defense and are less likely to cause injury or psychological impact.108 This fundamental critique applies to the 3 articles that compared cisgender and transgender participants’ IPV perpetration.37,85,95 Work to understand typologies of IPV, the prevalence of bidirectional violence, and how minority stress may affect violence perpetration in transgender populations will develop our understanding of this area.
While it is clear that transgender individuals are at greater risk of IPV than cisgender individuals, few studies examined demographic correlates of IPV within transgender communities. Twenty-eight unique data sets had more than 150 transgender participants and could support subgroup and risk factor analyses. Rather than viewing transgender individuals as a homogenous group, an intersectional lens should be used to understand how SAB, nonbinary gender identity, sexual orientation, race/ethnicity, disability, and other social categories may synergistically affect IPV risk within transgender communities. Medical and social transition status, examined in only 1 study,91 are key correlates to explore to identify potential critical periods for intervention. While there was no evidence of a significant difference in sexual IPV prevalence in AMAB compared with AFAB transgender individuals or in physical IPV prevalence in binary compared with nonbinary transgender individuals, only 5 studies informed each of these comparisons; more data are needed to understand whether a disparity truly exists.
Psychological and other forms of IPV (e.g., financial abuse, stalking) were, in some studies, more prevalent among transgender than cisgender participants. These types of IPV were less frequently measured than physical or sexual IPV. In cisgender populations, psychological IPV has gained attention as a driver of negative mental, physical, and sexual health outcomes of similar or greater magnitude than physical or sexual IPV.109 Qualitative data suggest that psychological IPV may be a more prominent component of abuse against transgender than cisgender individuals, as abusers leverage trans-related vulnerability to gain power and control.19 This trans-specific IPV often co-occurs with, but differs from, physical and sexual IPV, and is associated with excess mental health burden.87 Greater study of the prevalence, context, and impact of psychological IPV in transgender populations is warranted.
The direction of the disparity observed between transgender and cisgender participants was consistent across studies: 20 out of 23 studies that measured physical or sexual IPV in transgender and cisgender individuals found greater prevalence of IPV in transgender than in cisgender participants. However, clinical, methodological, and statistical heterogeneity was substantial, resulting in variability in the magnitude of the disparity estimated by each study. In studies in which the cisgender comparison group was at relatively low baseline risk of IPV (e.g., primarily heterosexual male and female students), we observed disparities as great as 6.5 times greater risk in transgender individuals.93 In studies in which baseline prevalence of IPV in the whole population is already relatively high (e.g., among lesbian, gay, bisexual, and queer cisgender individuals recruited from IPV-related forums),17 transgender–cisgender disparities were smaller. Our meta-analytic estimates average across these diverse studies. Disparities may be smaller or greater than this meta-analytic average in a particular population of interest, depending on baseline rates of IPV in the population. Regardless of the precise magnitude of the disparity, the implications for practice are that clinicians and service providers should take additional care to screen for IPV and offer affirming services to this at-risk population.
A strength of this review was contacting authors for disaggregated prevalence data for transgender participants. The review presents data that are publicly available for the first time from more than 40% of included studies and leverages data from almost 50 000 transgender respondents across studies. Limitations of this review include lack of covariate adjustment in meta-analyses. Meta-analyses combine estimates from different populations of transgender individuals, yielding high heterogeneity and potentially obscuring differences in subpopulations by providing a single estimate of disparities between cisgender and transgender populations. English-language searches may have missed literature from non-Anglophone countries and results may not be applicable to low-income settings.
Available evidence demonstrates that IPV is an epidemic facing transgender populations globally and highlights the existence of a dramatic disparity in physical and sexual IPV victimization between transgender and cisgender individuals, particularly cisgender men but also cisgender women. Physical, sexual, and mental health inequities21 faced by transgender individuals may be partially driven by these higher levels of violence. To address this critical public health and human rights concern, efforts are needed to develop transgender-specific, transgender-inclusive, and transgender-led interventions for IPV prevention, screening, reporting, and response in transgender populations worldwide.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
This study is a systematic review of published research and is not considered human participant research.
REFERENCES
- 1.Breiding MJ, Basile KC, Smith SG, Black MC, Mahendra RR. Intimate partner violence surveillance: uniform definitions and recommended data elements, version 2.0. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 2.Black MC, Basile KC, Breiding MJ . The National Intimate Partner and Sexual Violence Survey: 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 3.Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 4.Walters ML, Chen J, Breiding MJ. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 findings on victimization by sexual orientation. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 5.Geneva, Switzerland: World Health Organization; 2013. Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. [PubMed] [Google Scholar]
- 6.Valentine SE, Peitzmeier SM, King DS et al. Disparities in exposure to intimate partner violence among transgender/gender nonconforming and sexual minority primary care patients. LGBT Health. 2017;4(4):260–267. doi: 10.1089/lgbt.2016.0113. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, Best J, Tang W et al. Transgender sexual health in China: a cross-sectional online survey in China. Sex Transm Infect. 2016;92(7):515–519. doi: 10.1136/sextrans-2015-052350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guadamuz TE, Wimonsate W, Varangrat A et al. Correlates of forced sex among populations of men who have sex with men in Thailand. Arch Sex Behav. 2011;40(2):259–266. doi: 10.1007/s10508-009-9557-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roch A, Morton J, Ritchie G. Edinburgh, Scotland: LGBT Youth Scotland and The Scottish Transgender Alliance; 2010. Out of sight, out of mind? Transgender people’s experiences of domestic abuse. [Google Scholar]
- 10.Wirtz AL, Poteat TC, Malik M, Glass N. Gender-based violence against transgender people in the United States: a call for research and programming. Trauma Violence Abuse. 2020;21(2):227–241. doi: 10.1177/1524838018757749. [DOI] [PubMed] [Google Scholar]
- 11.Logie CH, Wang Y, Lacombe-Duncan A et al. Factors associated with sex work involvement among transgender women in Jamaica: a cross-sectional study. J Int AIDS Soc. 2017;20(1):21422. doi: 10.7448/IAS.20.01/21422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown T, Herman J. Intimate Partner Violence and Sexual Abuse Among LGBT People. Los Angeles, CA: The Williams Institute; 2015. [Google Scholar]
- 13.Winter S, Diamond M, Green J et al. Transgender people: health at the margins of society. Lancet. 2016;388(10042):390–400. doi: 10.1016/S0140-6736(16)00683-8. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Intimate partner violence: risk and protective factors. 2017. Available at: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/riskprotectivefactors.html. Accessed January 1, 2020.
- 15.James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi Ma. Washington, DC: National Center for Transgender Equality; 2016. The report of the 2015 US Transgender Survey. [Google Scholar]
- 16.Goodmark L. Transgender people, intimate partner abuse, and the legal system. Harv Civ Rights-Civil Lib Law Rev. 2013;48:51. [Google Scholar]
- 17.Woulfe JM, Goodman LA. Identity abuse as a tactic of violence in LGBTQ communities: initial validation of the identity abuse measure. J Interpers Violence. 2018 doi: 10.1177/0886260518760018. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 18.Grant JM, Mottet L, Tanis JE, Harrison J, Herman J, Keisling M. Washington, DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2011. Injustice at every turn: a report of the National Transgender Discrimination Survey. [Google Scholar]
- 19.Guadalupe-Diaz XL. Orlando, FL: University of Central Florida; 2013. Victims outside the binary: transgender survivors of intimate partner violence. [Google Scholar]
- 20.Lee M. Washington, DC: Trans People of Color Coalition; 2017. A time to act: fatal violence against transgender people in America 2017: human rights campaign. [Google Scholar]
- 21.Schuster MA, Reisner SL, Onorato SE. Beyond bathrooms—meeting the health needs of transgender people. N Engl J Med. 2016;375(2):101–103. doi: 10.1056/NEJMp1605912. [DOI] [PubMed] [Google Scholar]
- 22.Fernández-Rouco N, Fernández-Fuertes AA, Carcedo RJ, Lázaro-Visa S, Gómez-Pérez E. Sexual violence history and welfare in transgender people. J Interpers Violence. 2017;32(19):2885–2907. doi: 10.1177/0886260516657911. [DOI] [PubMed] [Google Scholar]
- 23.Pitts M, Smith A, Mitchell A, Patel S. Melbourne, Australia: Australian Research Center in Sex, Health, and Society, La Trobe University; 2006. Private lives: a report on the health and wellbeing of GLBTI Australians. [Google Scholar]
- 24.Spittal MJ, Fedyszyn I, Middleton A et al. Frequent callers to crisis helplines: who are they and why do they call? Aust N Z J Psychiatry. 2015;49(1):54–64. doi: 10.1177/0004867414541154. [DOI] [PubMed] [Google Scholar]
- 25.Riggs DW, Fraser H, Taylor N, Signal T, Donovan C. Domestic violence service providers’ capacity for supporting transgender women: findings from an Australian workshop. Br J Soc Work. 2016;46(8):2374–2392. [Google Scholar]
- 26.Veale JSE, Frohard-Dourlent H, Dobson S, Clark B. the Canadian Trans Youth Health Survey Research Group. Being safe, being me: results of the Canadian Trans Youth Health Survey. Vancouver, BC: Stigma and Resilience Among Vulnerable Youth Centre. School of Nursing, University of British Columbia; 2015. [Google Scholar]
- 27.Du Mont J, Kosa SD, Solomon S, Macdonald S. Assessment of nurses’ competence to care for sexually assaulted trans persons: a survey of Ontario’s Sexual Assault/Domestic Violence Treatment Centres. BMJ Open. 2019;9(5):e023880. doi: 10.1136/bmjopen-2018-023880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Logie CH, Lys CL, Mackay K, MacNeill N, Pauchulo A, Yasseen AS., 3rd Syndemic factors associated with safer sex efficacy among northern and Indigenous adolescents in Arctic Canada. Int J Behav Med. 2019;26(4):449–453. doi: 10.1007/s12529-019-09797-0. [DOI] [PubMed] [Google Scholar]
- 29.Askevis-Leherpeux F, de la Chenelière M, Baleige A et al. Why and how to support depsychiatrisation of adult transidentity in ICD-11: a French study. Eur Psychiatry. 2019;59:8–14. doi: 10.1016/j.eurpsy.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Lane T, Osmand T, Marr A et al. The Mpumalanga Men’s Study (MPMS): results of a baseline biological and behavioral HIV surveillance survey in two MSM communities in South Africa. PLoS One. 2014;9(11):e111063. doi: 10.1371/journal.pone.0111063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campbell MM, Fresán A, Addinall RM et al. Experiences of gender incongruence and the relationship between social exclusion, psychological distress, and dysfunction among South African transgender adults: a field-study for ICD-11. Ann Clin Psychiatry. 2018;30(3):168–174. [PubMed] [Google Scholar]
- 32.Sinha A, Goswami DN, Haldar D, Mallik S, Bisoi S, Karmakar PR. Sexual behavior of transgenders and their vulnerability to HIV/AIDS in an urban area of eastern India. Indian J Public Health. 2017;61(2):141–143. doi: 10.4103/ijph.IJPH_248_14. [DOI] [PubMed] [Google Scholar]
- 33.Castro R, De Boni RB, Luz PM et al. Health-related quality of life assessment among people living with HIV in Rio de Janeiro, Brazil: a cross-sectional study. Qual Life Res. 2019;28(4):1035–1045. doi: 10.1007/s11136-018-2044-8. [DOI] [PubMed] [Google Scholar]
- 34.De Boni RB, Machado IK, De Vasconcellos MTL et al. Syndemics among individuals enrolled in the PrEP Brasil Study. Drug Alcohol Depend. 2018;185:168–172. doi: 10.1016/j.drugalcdep.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 35.Robles R, Fresán A, Vega-Ramírez H et al. Removing transgender identity from the classification of mental disorders: a Mexican field study for ICD-11. Lancet Psychiatry. 2016;3(9):850–859. doi: 10.1016/S2215-0366(16)30165-1. [DOI] [PubMed] [Google Scholar]
- 36.Zalla LC, Herce ME, Edwards JK, Michel J, Weir SS. The burden of HIV among female sex workers, men who have sex with men and transgender women in Haiti: results from the 2016 Priorities for Local AIDS Control Efforts (PLACE) study. J Int AIDS Soc. 2019;22(7):e25281. doi: 10.1002/jia2.25281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Swan LET, Henry RS, Smith ER, Aguayo Arelis A, Rabago Barajas BV, Perrin PB. Discrimination and intimate partner violence victimization and perpetration among a convenience sample of LGBT individuals in Latin America. J Interpers Violence. 2019 doi: 10.1177/0886260519844774. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 38.FORGE. Atlanta, GA: Morehouse School of Medicine; 2011. Transgender individuals’ knowledge of and willingness to use sexual assault programs, unpublished survey data. [Google Scholar]
- 39.James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. Washington, DC: National Center for Transgender Equality; 2016. Executive summary of the report of the 2015 US Transgender Survey. [Google Scholar]
- 40.Cantor D, Fisher B, Chibnall SH . Washington, DC: Association of American Universities Washington; 2015. Report on the AAU campus climate survey on sexual assault and sexual misconduct. [Google Scholar]
- 41.Landers SJ, Gilsanz P. Boston, MA: Commonwealth of Massachusetts, Department of Public Health; 2009. The health of lesbian, gay, bisexual and transgender (LGBT) persons in Massachusetts: a survey of health issues comparing LGBT persons with their heterosexual and non-transgender counterparts. [Google Scholar]
- 42.Holt M. Madison, WI: Dane County Youth Commission; 2012. Dane County Youth Assessment 2012, unpublished data. [Google Scholar]
- 43.Holt M. Madison, WI: Dane County Youth Commission; 2015. Dane County Youth Assessment 2015, unpublished data. [Google Scholar]
- 44.Bazargan M, Galvan F. Perceived discrimination and depression among low-income Latina male-to-female transgender women. BMC Public Health. 2012;12(1):663. doi: 10.1186/1471-2458-12-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R. Adolescent Medicine Trials Network for HIV/AIDS Interventions. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–1757. doi: 10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clements-Nolle K, Guzman R, Harris SG. Sex trade in a male-to-female transgender population: psychosocial correlates of inconsistent condom use. Sex Health. 2008;5(1):49–54. doi: 10.1071/sh07045. [DOI] [PubMed] [Google Scholar]
- 47.Edwards KM, Littleton HL, Sylaska KM, Crossman AL, Craig M. College campus community readiness to address intimate partner violence among LGBTQ+ young adults: a conceptual and empirical examination. Am J Community Psychol. 2016;58(1-2):16–26. doi: 10.1002/ajcp.12068. [DOI] [PubMed] [Google Scholar]
- 48.Flentje A, Leon A, Carrico A, Zheng D, Dilley J. Mental and physical health among homeless sexual and gender minorities in a major urban US city. J Urban Health. 2016;93(6):997–1009. doi: 10.1007/s11524-016-0084-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heintz AJ, Melendez RM. Intimate partner violence and HIV/STD risk among lesbian, gay, bisexual, and transgender individuals. J Interpers Violence. 2006;21(2):193–208. doi: 10.1177/0886260505282104. [DOI] [PubMed] [Google Scholar]
- 50.Kattari SK, Walls NE, Speer SR. Differences in experiences of discrimination in accessing social services among transgender/gender nonconforming individuals by (dis)ability. J Soc Work Disabil Rehabil. 2017;16(2):116–140. doi: 10.1080/1536710X.2017.1299661. [DOI] [PubMed] [Google Scholar]
- 51.Keuroghlian AS, Reisner SL, White JM, Weiss RD. Substance use and treatment of substance use disorders in a community sample of transgender adults. Drug Alcohol Depend. 2015;152:139–146. doi: 10.1016/j.drugalcdep.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Langenderfer-Magruder L, Whitfield DL, Walls NE, Kattari SK, Ramos D. Experiences of intimate partner violence and subsequent police reporting among lesbian, gay, bisexual, transgender, and queer adults in Colorado: comparing rates of cisgender and transgender victimization. J Interpers Violence. 2016;31(5):855–871. doi: 10.1177/0886260514556767. [DOI] [PubMed] [Google Scholar]
- 53.Mizuno Y, Frazier EL, Huang P, Skarbinski J. Characteristics of transgender women living with HIV receiving medical care in the United States. LGBT Health. 2015;2(3):228–234. doi: 10.1089/lgbt.2014.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nemoto T, Bödeker B, Iwamoto M. Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. Am J Public Health. 2011;101(10):1980–1988. doi: 10.2105/AJPH.2010.197285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Odo C, Hawelu A. Eo na Mahu o Hawai’i: the extraordinary health needs of Hawai’i’s Mahu. Pac Health Dialog. 2001;8(2):327–334. [PubMed] [Google Scholar]
- 56.Qureshi RI, Zha P, Kim S et al. Health care needs and care utilization among lesbian, gay, bisexual, and transgender populations in New Jersey. J Homosex. 2018;65(2):167–180. doi: 10.1080/00918369.2017.1311555. [DOI] [PubMed] [Google Scholar]
- 57.Risser JM, Shelton A, McCurdy S et al. Sex, drugs, violence, and HIV status among male-to-female transgender persons in Houston, Texas. Int J Transgenderism. 2005;8(2–3):67–74. [Google Scholar]
- 58.Salazar LF, Crosby RA, Jones J, Kota K, Hill B, Masyn KE. Contextual, experiential, and behavioral risk factors associated with HIV status: a descriptive analysis of transgender women residing in Atlanta, Georgia. Int J STD AIDS. 2017;28(11):1059–1066. doi: 10.1177/0956462416686722. [DOI] [PubMed] [Google Scholar]
- 59.Smith LR, Yore J, Triplett DP, Urada L, Nemoto T, Raj A. Kaiser Permanente Community-Based HIV Test and Treat Study Team. Impact of sexual violence across the lifespan on HIV risk behaviors among transgender women and cisgender people living with HIV. J Acquir Immune Defic Syndr. 2017;75(4):408–416. doi: 10.1097/QAI.0000000000001423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Turell SC. A descriptive analysis of same-sex relationship violence for a diverse sample. J Fam Violence. 2000;15(3):281–293. [Google Scholar]
- 61.Whitton SW, Newcomb ME, Messinger AM, Byck G, Mustanski B. A longitudinal study of IPV victimization among sexual minority youth. J Interpers Violence. 2016;34(5):912–945. doi: 10.1177/0886260516646093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Langenderfer-Magruder L, Walls NE, Whitfield DL, Brown SM, Barrett CM. Partner violence victimization among lesbian, gay, bisexual, transgender, and queer youth: associations among risk factors. Child Adolesc Social Work J. 2016;33(1):55–68. [Google Scholar]
- 63.Bukowski LA, Chandler CJ, Creasy SL, Matthews DD, Friedman MR, Stall RD. Characterizing the HIV care continuum and identifying barriers and facilitators to HIV diagnosis and viral suppression among Black transgender women in the United States. J Acquir Immune Defic Syndr. 2018;79(4):413–420. doi: 10.1097/QAI.0000000000001831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Garthe RC, Hidalgo MA, Hereth J et al. Prevalence and risk correlates of intimate partner violence among a multisite cohort of young transgender women. LGBT Health. 2018;5(6):333–340. doi: 10.1089/lgbt.2018.0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goldenberg T, Jadwin-Cakmak L, Harper GW. Intimate partner violence among transgender youth: associations with intrapersonal and structural factors. Violence Gend. 2018;5(1):19–25. doi: 10.1089/vio.2017.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Henry RS, Perrin PB, Coston BM, Calton JM. Intimate partner violence and mental health among transgender/gender nonconforming adults. J Interpers Violence. 2018 doi: 10.1177/0886260518775148. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Martinez-Velez JJ, Melin K, Rodriguez-Diaz CE. A preliminary assessment of selected social determinants of health in a sample of transgender and gender nonconforming individuals in Puerto Rico. Transgend Health. 2019;4(1):9–17. doi: 10.1089/trgh.2018.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mimiaga MJ, Hughto JMW, Biello KB et al. Longitudinal analysis of syndemic psychosocial problems predicting HIV risk behavior among a multicity prospective cohort of sexually active young transgender women in the United States. J Acquir Immune Defic Syndr. 2019;81(2):184–192. doi: 10.1097/QAI.0000000000002009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Parsons JT, Antebi-Gruszka N, Millar BM, Cain D, Gurung S. Syndemic conditions, HIV transmission risk behavior, and transactional sex among transgender women. AIDS Behav. 2018;22(7):2056–2067. doi: 10.1007/s10461-018-2100-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Petering R, La Motte-Kerr W, Rhoades H, Wenzel S. Changes in physical assault among adults moving into permanent supportive housing. J Interpers Violence. 2019 doi: 10.1177/0886260519844775. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 71.Scheer JR, Baams L. Help-seeking patterns among LGBTQ young adults exposed to intimate partner violence victimization. J Interpers Violence. 2019 doi: 10.1177/0886260519848785. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Scheer JR, Woulfe JM, Goodman LA. Psychometric validation of the identity abuse scale among LGBTQ individuals. J Community Psychol. 2019;47(2):371–384. doi: 10.1002/jcop.22126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sterzing PR, Ratliff GA, Gartner RE, McGeough BL, Johnson KC. Social ecological correlates of polyvictimization among a national sample of transgender, genderqueer, and cisgender sexual minority adolescents. Child Abuse Negl. 2017;67:1–12. doi: 10.1016/j.chiabu.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 74.Taliaferro LA, McMorris BJ, Rider GN, Eisenberg ME. Risk and protective factors for self-harm in a population-based sample of transgender youth. Arch Suicide Res. 2019;23(2):203–221. doi: 10.1080/13811118.2018.1430639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Walls NE, Atteberry-Ash B, Kattari SK, Peitzmeier S, Kattari L, Langenderfer-Magruder L. Gender identity, sexual orientation, mental health, and bullying as predictors of partner violence in a representative sample of youth. J Adolesc Health. 2019;64(1):86–92. doi: 10.1016/j.jadohealth.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 76.Wilton L, Chiasson MA, Nandi V et al. Characteristics and correlates of lifetime suicidal thoughts and attempts among young Black men who have sex with men (MSM) and transgender women. J Black Psychol. 2018;44(3):273–290. [Google Scholar]
- 77.Yamanis T, Malik M, Del Río-González AM et al. Legal immigration status is associated with depressive symptoms among Latina transgender women in Washington, DC. Int J Environ Res Public Health. 2018;15(6):1246. doi: 10.3390/ijerph15061246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McDowell MJ, Hughto JMW, Reisner SL. Risk and protective factors for mental health morbidity in a community sample of female-to-male trans-masculine adults [erratum in BMC Psychiatry. BMC Psychiatry. 2019;19(1):45. doi: 10.1186/s12888-018-2008-0. 2019;19(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bhochhibhoya S, Maness SB, Cheney M, Larson D. Risk factors for sexual violence among college students in dating relationships: an ecological approach. J Interpers Violence. 2019 doi: 10.1177/0886260519835875. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 80.DeVylder JE, Jun H-J, Fedina L et al. Association of exposure to police violence with prevalence of mental health symptoms among urban residents in the United States. JAMA Netw Open. 2018;1(7):e184945. doi: 10.1001/jamanetworkopen.2018.4945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fedina L, Backes BL, Sulley C, Wood L, Busch-Armendariz N. Prevalence and sociodemographic factors associated with stalking victimization among college students. J Am Coll Health. 2019:1–7. doi: 10.1080/07448481.2019.1583664. [DOI] [PubMed] [Google Scholar]
- 82.Johns MM, Lowry R, Andrzejewski J et al. Transgender identity and experiences of violence victimization, substance use, suicide risk, and sexual risk behaviors among high school students—19 states and large urban school districts, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(3):67–71. doi: 10.15585/mmwr.mm6803a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Whitfield DL, Coulter RWS, Langenderfer-Magruder L, Jacobson D. Experiences of intimate partner violence among lesbian, gay, bisexual, and transgender college students: the intersection of gender, race, and sexual orientation. J Interpers Violence. 2018 doi: 10.1177/0886260518812071. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kattari SK, Walls NE, Whitfield DL, Langenderfer-Magruder L. Racial and ethnic differences in experiences of discrimination in accessing social services among transgender/gender-nonconforming people. J Ethn Cult Divers Soc Work. 2017;26(3):217–235. [Google Scholar]
- 85.Reisner SL, White JM, Bradford JB, Mimiaga MJ. Transgender health disparities: comparing full cohort and nested matched-pair study designs in a community health center. LGBT Health. 2014;1(3):177–184. doi: 10.1089/lgbt.2014.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ahmed SM, Palermo A-GS. Community engagement in research: frameworks for education and peer review. Am J Public Health. 2010;100(8):1380–1387. doi: 10.2105/AJPH.2009.178137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Peitzmeier SM, Hughto JMW, Potter J, Deutsch MB, Reisner SL. Development of a novel tool to assess intimate partner violence against transgender individuals. J Interpers Violence. 2019;34(11):2376–2397. doi: 10.1177/0886260519827660. [DOI] [PubMed] [Google Scholar]
- 88.Reuter TR, Newcomb ME, Whitton SW, Mustanski B. Intimate partner violence victimization in LGBT young adults: demographic differences and associations with health behaviors. Psychol Violence. 2017;7(1):101–109. doi: 10.1037/vio0000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.The GenIUSS Group. Los Angeles, CA: The Williams Institute; 2014. Best practices for asking questions to identify transgender and other gender minority respondents on population-based surveys. [Google Scholar]
- 90.White Hughto JM, Pachankis JE, Willie TC, Reisner SL. Victimization and depressive symptomology in transgender adults: the mediating role of avoidant coping. J Couns Psychol. 2017;64(1):41–51. doi: 10.1037/cou0000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Reisner SL, White Hughto JM, Pardee D, Sevelius J. Syndemics and gender affirmation: HIV sexual risk in female-to-male trans masculine adults reporting sexual contact with cisgender males. Int J STD AIDS. 2016;27(11):955–966. doi: 10.1177/0956462415602418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bukowski LA, Hampton MC, Escobar-Viera CG et al. Intimate partner violence and depression among Black transgender women in the USA: the potential suppressive effect of perceived social support. J Urban Health. 2019;96(5):760–771. doi: 10.1007/s11524-019-00355-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Griner SB, Vamos CA, Thompson EL, Logan R, Vázquez-Otero C, Daley EM. The intersection of gender identity and violence: victimization experienced by transgender college students. J Interpers Violence. 2017 doi: 10.1177/0886260517723743. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 94.Hoxmeier JC. Sexual assault and relationship abuse victimization of transgender undergraduate students in a national sample. Violence Gend. 2016;3(4):202–207. [Google Scholar]
- 95.Dank M, Lachman P, Zweig JM, Yahner J. Dating violence experiences of lesbian, gay, bisexual, and transgender youth. J Youth Adolesc. 2014;43(5):846–857. doi: 10.1007/s10964-013-9975-8. [DOI] [PubMed] [Google Scholar]
- 96.Logie CH, Wang Y, Marcus N et al. Syndemic experiences, protective factors, and HIV vulnerabilities among lesbian, gay, bisexual and transgender persons in Jamaica. AIDS Behav. 2019;23(6):1530–1540. doi: 10.1007/s10461-018-2377-x. [DOI] [PubMed] [Google Scholar]
- 97.Zakrison TL, Ruiz X, Gelbard R et al. Universal screening for intimate partner and sexual violence in trauma patients: an EAST multicenter trial. J Trauma Acute Care Surg. 2017;83(1):105–110. doi: 10.1097/TA.0000000000001495. [DOI] [PubMed] [Google Scholar]
- 98.Harland KK, Peek-Asa C, Saftlas AF. Intimate partner violence and controlling behaviors experienced by emergency department patients: differences by sexual orientation and gender identification. J Interpers Violence. 2018 doi: 10.1177/0886260518812070. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rodriguez A, Agardh A, Asamoah BO. Self-reported discrimination in health-care settings based on recognizability as transgender: a cross-sectional study among transgender US citizens. Arch Sex Behav. 2018;47(4):973–985. doi: 10.1007/s10508-017-1028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Seelman KL. Unequal treatment of transgender individuals in domestic violence and rape crisis programs. J Soc Serv Res. 2015;41(3):307–325. [Google Scholar]
- 101.Ford CL, Slavin T, Hilton KL, Holt SL. Intimate partner violence prevention services and resources in Los Angeles: issues, needs, and challenges for assisting lesbian, gay, bisexual, and transgender clients. Health Promot Pract. 2013;14(6):841–849. doi: 10.1177/1524839912467645. [DOI] [PubMed] [Google Scholar]
- 102.Bauer GR, Braimoh J, Scheim AI, Dharma C. Transgender-inclusive measures of sex/gender for population surveys: nixed-methods evaluation and recommendations. PLoS One. 2017;12(5):e0178043. doi: 10.1371/journal.pone.0178043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ellsberg M, Heise L, Peña R, Agurto S, Winkvist A. Researching domestic violence against women: methodological and ethical considerations. Stud Fam Plann. 2001;32(1):1–16. doi: 10.1111/j.1728-4465.2001.00001.x. [DOI] [PubMed] [Google Scholar]
- 104.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 105.Basile KC, DeGue S, Jones K . Atlanta, GA: Division of Violence Prevention, National Center for Injury Prevention and Control; 2016. STOP SV: a technical package to prevent sexual violence. [Google Scholar]
- 106.Ellsberg M, Arango DJ, Morton M et al. Prevention of violence against women and girls: what does the evidence say? Lancet. 2015;385(9977):1555–1566. doi: 10.1016/S0140-6736(14)61703-7. [DOI] [PubMed] [Google Scholar]
- 107.Moyer VA US Preventive Services Task Force. Screening for intimate partner violence and abuse of elderly and vulnerable adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;158(6):478–486. doi: 10.7326/0003-4819-158-6-201303190-00588. [DOI] [PubMed] [Google Scholar]
- 108.Langhinrichsen-Rohling J. Controversies involving gender and intimate partner violence in the United States. Sex Roles. 2010;62(3-4):179–193. [Google Scholar]
- 109.Basile KC, Arias I, Desai S, Thompson MP. The differential association of intimate partner physical, sexual, psychological, and stalking violence and posttraumatic stress symptoms in a nationally representative sample of women. J Trauma Stress. 2004;17(5):413–421. doi: 10.1023/B:JOTS.0000048954.50232.d8. [DOI] [PubMed] [Google Scholar]