Abstract
In this article, subarachnoidal hemorrhage developing in a case with Covid-19-related pneumonia was evaluated. In the presence of respiratory system infection signs such as cough and weakness in patient who present with sudden loss of consciousness, performing lung imaging as well as performing brain computerized tomography scan can allow the detection of an underlying Covid-19 infection.
Keywords: Covid-19, Subarachnoidal hemorrhage, Computed tomograpy, Emergency
Introduction
Coronaviruses are enveloped, positive single-stranded large RNA viruses that infect humans but also infect a wide variety of animals. In December 2019, it was determined that pneumonia, in which the lower respiratory tract of patients was affected, was caused by the new coronavirus (Covid-19) in Wuhan, China. This newly detected virus has been identified as acute respiratory syndrome coronavirus (Covid-19) (Li et al. 2020).
It is known that human coronaviruses can pass from the respiratory tract to the central nervous system through transneural and hematogenous ways and cause encephalitis and neurological diseases. Covid-19 was demonstrated by showing the gene sequence that passed into cerebrospinal fluid, and it was emphasized that neurological diseases should be considered.(Hospital BD 2020) In this article, subarachnoid hemorrhage developing in patient with Covid-19-related pneumonia was evaluated.
Case
A 50-year-old male patient was admitted to the emergency department due to impaired consciousness. According to the medical history taken from their relatives, they stated that patient had complaints of weakness and especially dry cough for the last week and that his consciousness suddenly closed approximately 1 h before admitting to the emergency department. It was stated that he did not have concomitant disease. In the physical examination of the patient at the time of admission, Glasgow coma score was found to be 4 (E: 1, M: 2, V: 1). The patient’s blood pressure was 170/90 mm Hg, heart rate 115 beats/min, fever 36.7 °C, respiratory rate 20/minute, and oxygen saturation in the room air with pulse oximeter was 70%. Lung examination revealed crackles in both hemithorax. Other physical examination findings were normal. Laboratory findings of the patient are shown in Table 1. The patient was intubated quickly. Intravenous access was made with an 18-gauge catheter from both antecubital regions. The patient was connected to the mechanical ventilator in synchronous intermittent mandatory ventilation. Cranial and thorax computed tomography imaging was performed. In the cerebral tomography, it is determined that there was subarachnoidal hemorrhage in the bilateral parasagittal area originating from the Willis polygon, which opens into the ventricles and extends to the 3rd ventricle (Fig. 1a). Computed thorax tomography shows widespread patch-like pneumonic infiltration and ground-glass areas in both lung apexes (Fig. 1b). Swabs from the oral and nasopharyngeal region of the patient were taken to perform the Covid-19 PCR test. The patient was hospitalized in our hospital’s Covid-19 intensive care unit, considering subarachnoidal hemorrhage and Covid-19-associated pneumonia. The patient died on the 83rd day of hospitalization.
Table 1.
Laboratory values of the patients on admission
| Category | Values of patient | Normal range |
|---|---|---|
| White blood cells (μL) | 26.000 | 3.600–10.200 |
| Hemoglobin (g/dL) | 16.7 | 12.5–16.3 |
| Hematocrit (%) | 47.3 | 36.7–47.1 |
| Platelets (/μL) | 299.000 | 152.000–348.000 |
| Glucose (mg/dL) | 206 | 74–106 |
| Aspartate transaminase (U/L) | 32 | 5–50 |
| Alanine transaminase (U/L) | 42 | 5–50 |
| Lactate dehydrogenase (U/L) | 311 | 5–248 |
| Blood urea nitrogen (mg/dL) | 38 | 17–43 |
| Creatinine (mg/dL) | 1.10 | 0.67–1.17 |
| Sodium (mmol) | 137 | 136–146 |
| Potassium (mmol/L) | 4.19 | 3.5–5.5 |
| Calcium (mg/dL) | 9.2 | 8.8–10.6 |
| C-reactive protein (mg/L) | 9.0 | 0–5 |
| High sensitivity troponin I (ng/L) | 259 | 0–16 |
| Creatinine kinase-MB (μg/L) | 5.2 | 0.6–6.3 |
| Prothrombin time (sec) | 11.3 | 10.5–14.5 |
| APTT (sec) | 21.0 | 25–34 |
| INR | 0.92 | 0.8–1.2 |
| Arterial blood gases | ||
| pH (mm Hg) | 7.317 | 7.35–7.45 |
| pO2 (mm Hg) | 59.2 | 83–108 |
| pCO2 (mm Hg) | 48.5 | 35–45 |
| HCO3 (mEq/L) | 22.5 | 22–28 |
Fig. 1.
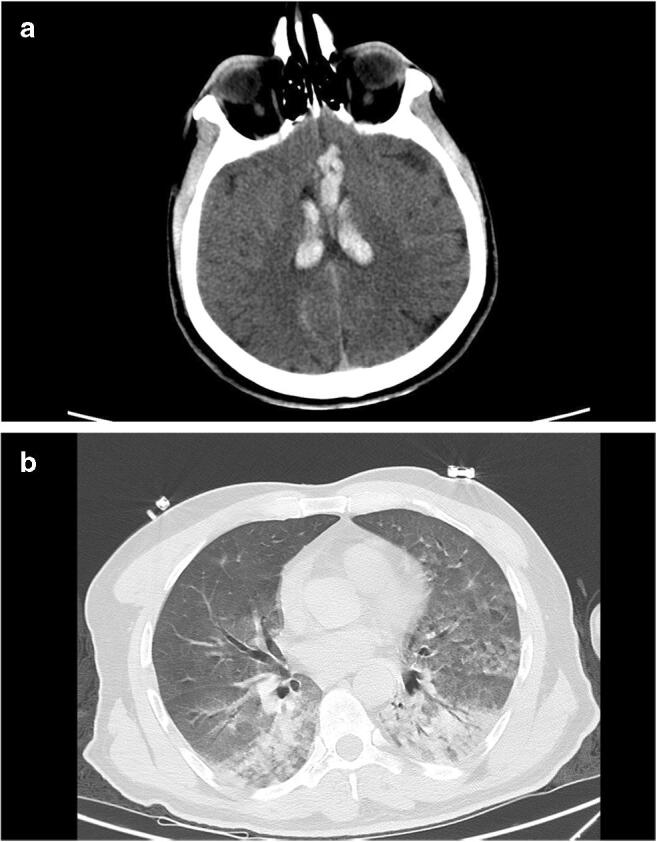
(a) Subarachnoid hemorrhage into the brain’s ventricular system of the patient. (b) Computed tomography image of the patient
Discussion
Covid-19 is a new type of beta-coronavirus that causes fever, cough, shortness of breath, and muscle weakness, and its clinical findings are highly severe in patients with advanced age and comorbidities. Although a mild symptomatic course is observed in most of the cases, it has affected the world today and has become a primary health problem with its high contagious rate and its ability to cause pulmonary complications such as acute respiratory distress syndrome, which may require intensive care.
Clinical assessment is mostly on the respiratory system due to the fact that Covid-19 can cause acute and mortal pneumonia and the respiratory distress it causes. The presence of dyspnea, cough, and fever-like symptoms and the presence of bilateral patch-style ground-glass opacities on computed thorax tomography lead the clinician to diagnosis. However, today it is known that coronaviruses are not limited to the respiratory system. It has been shown in studies that all beta-coronavirus species have neuroinvasive properties. Although the blood-brain barrier protects the central nervous system against exogenous pathogens, coronavirus species can spread to the central nervous system through hematogenous, transneuronal routes and cause neurological diseases. Increasing evidence indicates that coronaviruses first penetrate the peripheral nerve endings, reaching the central nervous system with a retrograde spread through the synapses. Although this transsinaptic transfer has been shown in the SARS-CoV virus, it is quite possible that Covid-19 has similar potential due to its high similarity in its structure. There are case series in which severe neurological symptoms such as cerebrovascular disease and worsening of consciousness are reported in the majority of Covid-19-positive patients who have severe clinical course.(Yan-Chao et al. 2020)
In our case admitted to the emergency department with worsening of consciousness, subarachnoid was detected. No predisposing condition for subarachnoid hemorrhage was detected in patient. However, in medical history of patients, the presence of a resistant dry cough that has been ongoing for a while before the application is noteworthy. It is possible that the subarachnoid hemorrhage developing in the patient is due to the increase in the intraluminal pressure of the radiculomedullar veins that pass into the subarachnoid space. Studies have indicated that sudden pressure increase and rupture of these vessels due to severe cough may lead to spontaneous subarachnoid hemorrhages.(Oji et al. 2013) Considering the typical findings in BT imaging, it is also possible that dry cough resistant to lower respiratory tract infection caused these bleeding.
In the diagnosis of Covid-19, real-time polymerase chain reaction (PCR) tests can be pseudo-negative, although it is the gold standard, whereas in the thorax computed tomographies of the patients, up to 96% pathological images can be observed. For this reason, the clinical diagnosis, where imaging findings are used, is becoming more and more important regardless of rT-PCR. Although subarachnoidal hemorrhage was detected in case, the clinical history and tomography images of the patients suggest the diagnosis of SARS-CoV-2.(Dasheng et al. 2020) When we evaluate this information, regardless of the reason, in the presence of an anamnesis suggesting respiratory system infection such as cough and weakness in patients who come with sudden loss of consciousness, performing lung imaging as well as the performing brain computerized tomography can allow detection of an underlying Covid-19 infection.
Availability of data and materials
Data and materials are reachable from hospital automation information systems.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interests.
Footnotes
Any part of this paper is not under consideration for publishing or published in anywhere else.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Akkan Avci, Email: drakkanavci@gmail.com.
Onder Yesiloglu, Email: dronderyesiloglu@gmail.com.
Begum Seyda Avci, Email: begumtngnr@hotmail.com.
Hilmi Erdem Sumbul, Email: erdemsumbul@gmail.com.
Satuk BugraYapici, Email: satukbugrayapici@gmail.com.
Adnan Kuvvetli, Email: adnankuvvetli@hotmail.com.
Burcak Cakır Pekoz, Email: burcakpekoz@gmail.com.
Hayri Cinar, Email: drhayricinar@gmail.com.
Salim Satar, Email: salim.satar@yahoo.com.
References
- Dasheng L, Dawei W, Jianping D, Nana W, He H, Haiwang X, et al. False-negative results of real-time reverse-transcriptase polymerase chain reaction for severe acute respiratory syndrome coronavirus 2: role of deep-learning-based ct diagnosis and insights from two cases. Korean J Radiol. 2020;21(4):505–508. doi: 10.3348/kjr.2020.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hospital BD (2020). http://www.bjdth.com/html/1/305/307/index.html?messageId=3665 Accessed 04 Mar 2020
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oji Y, Noda K, Tokugawa J, Yamashiro K. Spontaneous spinal subarachnoid hemorrhage after severe coughing: a case report. J Med Case Rep. 2013;7:274. doi: 10.1186/1752-1947-7-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan-Chao L, Wan-Zhu B, Tsutomu H. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020;92:1–4. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and materials are reachable from hospital automation information systems.


