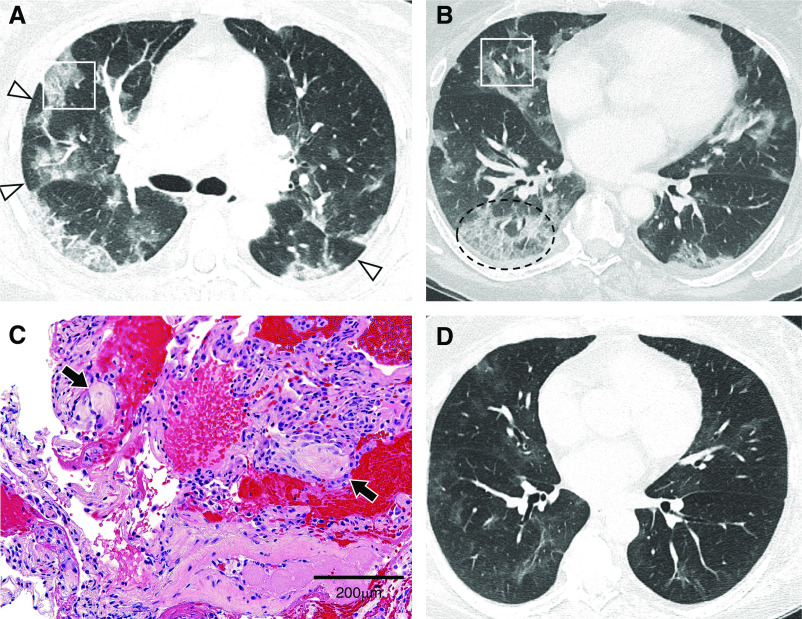
The few pathological analyses of coronavirus disease (COVID-19) pneumonia to date, mostly from autopsy studies, report diffuse alveolar damage or acute fibrinous and organizing pneumonia (1–3). In contrast, computed tomographic (CT) imaging from numerous patients with COVID-19 includes features more consistent with organizing pneumonia (OP) (4, 5). A previously healthy 61-year-old woman presented with 3 weeks of dyspnea, cough, and fevers; a nasopharyngeal RT-PCR for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and common respiratory pathogens was negative. CT imaging on Day 3 of admission demonstrated peripheral and basilar patchy opacities with perilobular sparing, consistent with an OP pattern (Figures 1A and 1B and Video 1). The patient had no signs or symptoms of an underlying rheumatologic condition and took no medications. Two days later, transbronchial biopsies throughout the right lung peripherally revealed scattered fibromyxoid plugs within distal airspaces, indicative of a histologic OP pattern (Figure 1C). RT-PCR for SARS-CoV-2 returned positive by BAL; other BAL cultures were unremarkable. The patient was started on remdesivir and made a full clinical recovery. CT imaging 26 days after presentation showed minimal residual opacities (Figure 1D and Video 2). OP findings in this case may stem from tissue sampling later in a self-limited course of mild to moderate COVID-19. Confirmed radiographically and histologically, OP, as an active and sometimes aberrant lung repair process, may represent the evolution of COVID-19 in patients with mild to moderate disease.
Figure 1.
(A) Axial computed tomographic (CT) image of the midlung zones showing areas of “perilobular” distribution (arrowheads) of pulmonary opacities in a pattern consistent with organizing pneumonia. Approximate area of transbronchial biopsy in the anterior segment of the right upper lobe (white rectangle) is shown. (B) Axial CT image of the lower-lung zones showing patchy ground-glass opacities distributed peripherally in the lungs and “crazy paving” in the posterior basal right lower lobe (dashed oval). Approximate area of biopsy in the right middle lobe (white rectangle) is shown. (C) High-power magnification of alveolated lung containing scattered fibromyxoid plugs of granulation tissue (arrows) and sparse interstitial mononuclear infiltrates, indicating organizing pneumonia (hematoxylin and eosin). Scale bar, 200 μm. (D) Follow-up CT imaging performed 26 days after presentation with the axial image at the same location as in B, near the level of the inferior pulmonary veins, demonstrates nearly resolved pulmonary opacities. Videos 1 and 2 show the entirety of both CT scans.
Video 1.
Axial computed tomographic images through the chest without contrast of the patient on hospital Day 3.
Video 2.
Axial computed tomographic images through the chest without contrast of the patient 26 days after presentation.
Supplementary Material
Footnotes
Author Contributions: Conception and design: B.P.P., K.E.S., and H.H.G. Analysis and interpretation: B.P.P., K.E.S., H.S., H.B., G.J.B., and H.H.G. Drafting the manuscript for important intellectual content: B.P.P., K.E.S., H.S., H.B., G.J.B., and H.H.G.
The uncompressed videos are accessible from this article’s supplementary material page.
Originally Published in Press as DOI: 10.1164/rccm.202004-1278IM on July 1, 2020
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Copin M-C, Parmentier E, Duburcq T, Poissy J, Mathieu D Lille COVID-19 ICU and Anatomopathology Group. Time to consider histologic pattern of lung injury to treat critically ill patients with COVID-19 infection. Intensive Care Med. 2020;46:1124–1126. doi: 10.1007/s00134-020-06057-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33:1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH.Essentials for radiologists on COVID-19: an update-radiology scientific expert panel Radiology[online ahead of print] 27 Feb 202010.1148/radiol.2020200527 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.