Abstract
Aim
Contact lens wearers need to maintain optimal hygiene practices during the COVID-19 pandemic to minimise contact-lens complications including microbial keratitis and corneal infiltrative events. This online survey (UK and Ireland) explored contact lens wearers’ compliance behaviours, attitudes and concerns during the pandemic.
Method
The 60-item anonymous online survey was distributed during a 1-month period via Qualtrics (starting on 14/04/20). The survey captured: a) demographic information, b) type of lenses worn and compliance with lens wear and care procedures, c) adherence to recommendations and d) concerns associated with contact lens wear during the pandemic.
Results
Two hundred and forty seven responses were received (34.3 ± 11.7 years old, 79% female). Seventy nine percent of participants reported that they were self-isolating or rigorously following social distance advice. Fifty-six percent of participants reported using their lenses less during the pandemic. Eighty-seven percent of respondents reported following the recommended 20-second rule most times/every time and 96% used soap and water during handwashing. Eleven percent of respondents admitted not following recommendations regarding disposal of lenses and 18% would not consider ceasing lens wear if unwell (with flu/cold) during the pandemic.
Conclusion
Respondents reported wearing their contact lenses less than usual. Good compliance with handwashing was observed but soft reusable lens wearers showed a statistically significant lower compliance with lens wear and care compared to daily disposable lens wearers (p=<0.001).
Keywords: Contact lens, COVID-19, Compliance, Microbial keratitis
1. Introduction
In March 2020, the World Health Organization (WHO) declared the COVID-19 outbreak a global pandemic. COVID-19 is caused by SARS-CoV-2, a variant of coronavirus. Within the field of ophthalmology, a few case reports [1,2] have suggested the presence of viral conjunctivitis before other COVID-19 symptoms which generated concern among eye care professionals (ECPs). A joint report by the College of Ophthalmologists and the College of Optometrists [3] stated that it was unlikely that a person would present with viral conjunctivitis without other COVID-19 symptoms and this has been confirmed in larger cohort studies [4]. In accordance with this, Sun et al. [5] concluded that ‘the eye is neither a preferred organ for human coronavirus infection nor a preferred gateway of entry that enables human coronavirus to infect the respiratory tract’. As a result, Jones et al. [6] stated that there is currently no scientific evidence of an increased risk of COVID-19 for contact lens (CL) wearers compared to non-wearers. Similarly, Willcox et al. [4] emphasised that during the pandemic wearers should be reminded of good hygiene practices.
The most serious complication associated with contact lens wear is microbial keratitis (MK). In the UK, an estimated 4.1 million people wear contact lenses [7]. MK occurs in around 2 per 10,000 wearers with daily wear of soft lenses and 20 per 10,000 wearers in extended soft lens wear [8]. Modifiable risk factors associated with MK and corneal infiltrative events include poor hygiene [[9], [10], [11]] and non-compliance with lens wear and care [10]. The current recommendations for contact lens wearers are that contact lens wear is safe assuming wearers are (1) using optimal hand hygiene when handling lenses and (2) discontinue lens wear if unwell (particularly with cold or flu symptoms) [6]. Previous work during non-pandemic times highlights that non-compliance among contact lens wearers continue to be a problem worldwide [12]. Currently, there is a lack of evidence of contact lens wearers behaviours, attitudes and concerns during the COVID-19 pandemic. The aim of this study was to gather this evidence, via an online survey, from contact lens wearers based in the UK and Ireland. The study also explored whether patient demographics and/or smoking status had any relationship with compliance [10]. Having this information is critical at a time where access to community optometric practice remains limited. More importantly, this study has the potential to inform communication from ECPs to improve patient management during the pandemic, in turn reducing the likelihood of contact-lens related complications.
2. Materials and methods
2.1. Study design
Ethical approval was granted by the Faculty of Science and Engineering Research Ethics Panel at Anglia Ruskin University (Cambridge, UK, reference number FSE/FREP/19/924). Respondents gave informed consent online at the start of the survey and the study was conducted following the tenets of the Declaration of Helsinki. Only one submission from each IP address was permitted by the survey software. No identifiable data were collected and participation was voluntary. The Equator network Checklist for Reporting Results of Internet e-Surveys was used to report the methods and results of the survey.
2.2. Survey development
Items for the survey were identified through an iterative process. A list of possible questions was generated by the research team to capture: a) demographic information (sex, age, whether social distancing advice was followed); b) type of lenses worn and compliance with lens wear and care procedures during the pandemic; c) adherence to practitioner’s recommendations on safe lens wear and d) wearer’s concerns associated with lens wear during the pandemic. To ensure consistency in the responses regarding how well respondents were following social distancing advice, examples were given to explain self-isolation (if you or someone in your household has symptoms) and rigorously following social distancing advice (reducing social interactions with others). Questions regarding known modifiable behaviours associated with non-compliance in contact lens wear (e.g. failure to rub and rinse or topping off solution) were adapted from existing literature on compliance with contact lens wear and care [[13], [14], [15], [16]]. The 70 proposed questions were appraised and reduced by three UK registered optometrists (all authors of this article; MV-E, JW and PA) to a 60-item survey, by considering the face validity and content validity of each item [17]. Following item identification, the final questionnaire was reviewed by two contact lens wearers known to the investigators and within the target population to ensure interpretability. The final survey items were inputted into Qualtrics (Qualtrics, Provo, UT) and then reviewed by team members to ensure functionality. Errors identified were corrected before the launch of the survey. As each lens modality involves different care routines, some questions were only presented to respondents depending on responses to preceding questions (e.g. questions on lens case care were only presented to wearers of soft reusable lenses using skip logic). A copy of the full questionnaire can be requested by contacting the corresponding author.
2.3. Survey distribution
Eligibility criteria included adults using contact lenses living in the United Kingdom and Ireland. Recruitment was via social media outlets (British Contact Lens Association, Twitter, LinkedIn and Facebook) and was open to anyone meeting the inclusion criteria. The survey was run for a period of 1 month, starting 14th April 2020, after strict social distancing measures had been in place in the UK for three weeks.
2.4. Data analysis
Data cleaning was initially undertaken to remove cases that did not meet study eligibility (i.e. not residing in the UK). Summary reports from Qualtrics were used to summarize the closed ended questions and the Statistical Package for Social Sciences (SPSS) version 26.0 (IBM Corp, 2019) was used for descriptive statistics, including frequencies, means and standard deviations. Full compliance was defined as adherence to the modifiable behaviours shown in Table 1 for optimal lens wear and care of daily disposable soft lenses and daily wear soft reusable lenses [13,18,19].
Table 1.
Description of the seven behaviours required for full-compliance with daily disposable soft contact lenses and the thirteen behaviours required for full-compliance with soft reusable contact lenses (daily wear). N/A indicates not applicable. Adapted from [13,18,19].
| Required behaviours for full compliance | Daily disposable soft contact lens wearers | Soft reusable lens wearers (daily wear) | |
|---|---|---|---|
| Handwashing | Wash hands before inserting and removing lenses | ✓ | ✓ |
| Wash hands with soap and water | ✓ | ✓ | |
| Lens wear | Follow ECP recommendations for wearing time | ✓ | ✓ |
| Lens replacement | Follow ECP recommendations for lens replacement interval | ✓ | ✓ |
| General recommendations safe lens wear | Daily visual check before inserting lenses | ✓ | ✓ |
| Cease lens wear if unwell (cold or flu) | ✓ | ✓ | |
| Do not use lenses whilst showering | ✓ | ✓ | |
| Use care solutions | Rubbing lenses after use | N/A | ✓ |
| Rinsing lenses after rubbing them with solution | N/A | ✓ | |
| No topping-off | N/A | ✓ | |
| Lens case care | Daily lens case cleaning | N/A | ✓ |
| Storage of lens case when not in use (empty, caps off, face down) | N/A | ✓ | |
| Monthly lens case replacement | N/A | ✓ |
Bivariate associations between lens care compliance and age, sex and smoking status were analysed using chi-square statistics for categorical variables (or Fisher’s exact test if there were cases with expected counts less than 5) and Kendall’s tau-b for continuous variables. Any participant data with missing information were deleted during analyses. A significance level of p ≤ 0.05 was used for all analyses.
3. Results
3.1. Patient demographics and COVID-19 symptomatology
A total of 262 participants completed the anonymous survey online. Data received from respondents living outside of the UK and Ireland was excluded from the analysis (n = 15). The mean age of the respondents was 34.3 ± 11.7 years (range 19 - 63) and 79% were female. Ninety percent of respondents were based in England and 91% were non-smokers. Respondents were asked to what extent they were following lockdown conditions and 79% reported living under self-isolation or rigorously following social distance advice, a further 6% informally following social distance advice and 15% reported leading a near normal existence (e.g. still going to a place of work). The large majority of respondents had not had any symptoms of COVID-19 themselves (87%) nor anyone else in their household (88%).
3.2. CL worn and habits before the COVID-19 pandemic
The reported frequency of CL modality and use of lens care products for lens disinfection is presented in Table 2 . Before the pandemic, 83% of respondents bought their contact lenses from an optical store and 17% over the internet.
Table 2.
Reported frequency of CL modality worn by the respondents (n = 247) and lens care product used for contact lens disinfection (n = 75 as one respondent was excluded as they were wearing monthly contact lenses on an extended wear basis).
| Lens modality | n | Percentage | Lens care disinfection method used with soft reusable CLs | n | Percentage |
|---|---|---|---|---|---|
| Soft disposable | 161 | 65% | Multipurpose solution | 57 | 76% |
| Soft reusable | 76 | 31% | Hydrogen peroxide | 9 | 12% |
| Rigid contact lenses | 10 | 4% | Saline | 9 | 12% |
3.3. CL wear during the COVID-19 pandemic
Fifty-six percent of respondents reported using their contact lenses less during the pandemic, 39% about the same and 5% more during the pandemic. The most common reason for reduced wear was ‘less need at home’ (49%). Other reasons included ‘less effort to wear specs’ (22%), ‘fear of infection/touching eyes’ (12%), ‘to protect supply in case of running out’ (7%), ‘to rest my eyes’ (7%) and ‘to save money’ (3%).
3.4. Handwashing habits before and during the COVID-19 pandemic
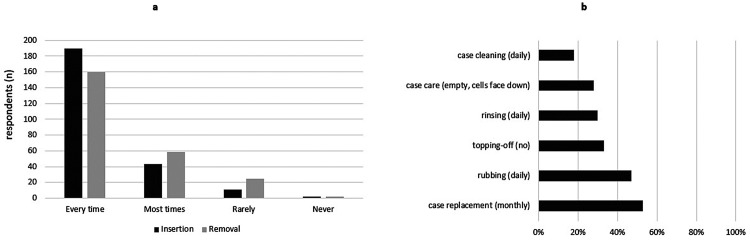
Respondents were asked questions about their handwashing habits during the pandemic: 96% reported using soap and water, 87% reported following the recommended 20-second rule most times/every time, and 82% reported washing their hands after coughing, sneezing or blowing their nose most times/every time. Sixty-three percent of participants reported their handwashing routine had changed since the start of the pandemic with their comments indicating that they were now washing their hands more thoroughly and more frequently. Fig. 1 a illustrates the distribution of the responses regarding frequency of handwashing prior to lens insertion (dark grey bars) and removal of contact lenses (light grey bars). Only 1% used antibacterial wipes to wash hands prior to lens insertion. When asked about how they dried their hands, the responses included: cloth towel shared with other family members to dry hands (48%), cloth towel only used by myself (40%), paper towel (10%) and other (2%).
Fig. 1.
a) Frequency of handwashing before contact lens insertion and before contact lens removal (n = 247) and b) Frequency of wearers with optimal behaviours associated with lens care of soft reusable lenses and lens cases.
3.5. Wearers of soft reusable contact lenses – contact lens and case care
The sub-group of respondents using multi-purpose solution with their reusable soft contact lenses was asked for further information on their lens cleaning habits. Respondents indicated sub-optimal cleaning routines: 30% of respondents never rub the lenses before soaking, 42% never rinse the lenses and 67% admitted topping off the lens case solution (rather than filling with clean solution) frequently or occasionally. Five out of 9 respondents (56%) of respondents using hydrogen peroxide solution with their reusable contact lenses admitted topping off solution occasionally or frequently.
A high percentage of respondents were also non-compliant with several aspects related to the care of the lens case: 82% did not clean the lens case daily and 72% did not keep the case empty with caps facing down when not in use. When asked what they used to clean their case, 44% responded ‘rinsing with lens solution’, 19% responded ‘tap water and/or soap’, 12% rinsed with contact lens solution and wiped with a clean tissue (optimal technique) [20] and 25% used other non-optimal methods. In contrast, most patients showed good compliance when asked about how frequently they intended to replace their storage case during the pandemic (53% at least every 3 months). Fig. 1b shows the proportion of compliant wearers for modifiable-related behaviours associated with care of soft reusable lenses and lens cases.
3.6. General recommendations for safe CL wear
First, respondents were asked if they would exceed the recommended wearing time during the pandemic (e.g. sleeping in your lenses if not recommended by your ECP) and 89% of the respondents disagreed with this statement. In contrast, 21% responded that they were not following the recommendations given by their ECP regarding disposal of their lenses (e.g. after each day if using daily disposables). Secondly, respondents were asked if during the pandemic they checked if their eyes ‘seem healthy before inserting the lenses’ and 30% of respondents admitted not taking this precaution. Twenty-six percent admitted wear contact lenses whilst showering during the pandemic. Eighteen percent of respondents would not consider ceasing lens wear during the pandemic if feeling unwell (with cold or flu symptoms). Furthermore, 13% do not own a pair of up to date spectacles.
Table 1 indicates the behaviours required for full compliance in each wearing modality and was used to further explore the data in the present study. Soft daily disposable lens wearers had a statistically significantly higher compliance ratio than users of soft reusable lenses (23.4%, p=<0.001). As shown in Table 1, reusable lens wearers had 6 additional steps to be considered fully compliant with their CL disinfection routine. Furthermore, no significant associations were found between compliance ratios and age, sex or smoking status (all p > 0.05)
3.7. Additional support during pandemic
Eighty-nine per cent of respondents have not sought any form of additional support for managing their contact lens wear during the pandemic (e.g. received support from an eye care practitioner, contacted a medical practitioner or searched for information on the internet). In addition, 70% of the respondents were not concerned about their contact lens wear during the pandemic. Thirteen percent of respondents were worried they could not attend or get help with their contact lenses/care products or attend their local optician and 9% worried they might run out of lenses/care products.
4. Discussion
The COVID-19 pandemic is evolving rapidly as new information becomes available but currently there is no scientific evidence of an increased risk of COVID-19 for CL wearers compared to non-wearers [6]. In addition, to reduce the risk of adverse events associated with CL wear, ocular scientists [6], CL-related professional associations [21], the Centre for Ocular Research and Education (CORE) [22] and the Centers for Disease Control and Prevention (CDC) [23] have strongly emphasised that contact lens wearers should continue to adhere to the recommendations provided before the pandemic in terms of hygiene and contact lens wear and care.
Data for this online survey were collected during strict lockdown restrictions, only 15% of the respondents said that they were leading a near normal existence. The contact lens wearing pattern of the sample of respondents to this online survey is in agreement with the latest worldwide data on contact lens prescribing in terms of age, sex, contact lens modality and lens care [24]. In line with another recent report [25] CL wearers in this study also reported wearing their lenses less during the pandemic. The most common reasons for reduced wear was ‘less need at home’ and ‘less effort to wear specs’.
Respondents showed good handwashing compliance with 87% following the recommended 20-second rule and 96% using soap and water. Previously, despite education about insertion and removal of lenses the handwashing behaviour of many contact lens wearers was sub-optimal. For instance, Morgan et al. [13] reported correct hand washing by about 40% of wearers and Osborn et al. [26] reported that 41% of daily disposable contact lens wearers did not wash their hands with soap before lens insertion. However, the improved compliance with handwashing in this study is not surprising given the strong recommendations of washing hands regularly to reduce the risk of contracting COVID-19. In line with this, the free text comments provided by the respondents emphasised an improved technique in terms of frequency and thoroughness when washing hands during the pandemic. In contrast, drying hands showed less consistency in the responses (48% using a towel shared with others in their household and only 10% using paper towels). In view of these findings, ECPs and the wider stakeholders in the sector (e.g. CL-related professional associations) should further educate wearers around the importance of drying hands to increase compliance with this critical step [27]. Unintentional exposure to water during lens wear was also reported, as some respondents admitted to cleaning the lens case with tap water and/or showering whilst wearing contact lenses. These non-compliant behaviours have previously been reported by others. Dumbleton et al. [16] reported 67% of respondents cleaned their lens case with tap water whilst others admitted showering whilst wearing contact lenses. In addition to this, Zimmerman et al. [28] reported showering in contact lenses was more common in soft lens wearers than gas-permeable lens wearers (86% respectively) but gas-permeable wearers were more likely to rinse or store lenses in water. Arshad et al. [27] suggested that researchers should explore the use of digital reminders to emphasise public awareness of the risks associated with water exposure during CL wear. More recently, Arshad et al. [29] has demonstrated an improvement in water-contact behaviours with the use of a no-water infographics.
In addition to handwashing, the current survey explored compliance with lens wear and care during the pandemic. Consistent with the results of Dumbleton et al. [14], this study reports that 11% of respondents lengthened the wearing period of their lenses beyond that recommended by their ECP. As a result of lockdown, CL practice has drastically changed and currently UK wearers are discouraged from attending for routine CL checks [6]. Instead, optometric practices have introduced telehealth and/or face-to-face consultations for emergency services only. In this context, adhering to ECPs recommendations is extremely important, but 18% of the respondents stated they will not consider ceasing lens wear if feeling unwell (with cold or flu symptoms). This highlights important areas to stress when remotely assessing patients to ensure they remain problem-free during the pandemic. In addition, in agreement with previous research [13,14] this study also reports a high non-compliance with lens care and lens case care (Fig. 1b). One of the limitations when using online surveys is that respondents may provide inaccurate information. In this study, 12% of respondents (Table 2) believed they were using saline as their lens care disinfection solution. This can either indicate that the respondents were not certain of which lens care solution they used or more worryingly that they in fact do use saline solution as a stand-alone disinfection product. Dumbleton et al. [16] reported that 5% of respondents from an online questionnaire also used saline as the lens care disinfection solution and approximately half of daily lens wearers re-using lenses reported using saline or the solution left in the package to store their lenses [15].
This study has found soft daily disposable lens wearers showed statistically significant better levels of compliance with lens wear and care when compared to soft reusable lens wearers (daily wear). Jones et al. [6] argued that given the reduced incidence of corneal infiltrative events in wearers of daily disposable lenses [30,31] this form of lens wear seems ideal in a time of reduced clinical provision. In agreement with this, the present results indicate that the simplicity of daily disposables offers a significant advantage as opposed to the complex steps required to achieve full compliance with reusable lenses.[18 19] However, swapping a patient to daily disposable lenses of the same stated parameters does not result in the same lens fit [32] and telemedicine is not at a stage where lens fit can be accurately assessed remotely [33], so unless the patient has worn a particular soft daily disposable contact lens before, changing during the pandemic is not a safe option. During these challenging times, practitioners have been asked to exercise their professional judgement when monitoring the care of contact lens wearers [34]. Should clinical provision remain limited over the forthcoming months, ECPs will need to ensure that contact lens wear remains safe and that whenever possible wearers are directed towards wearing lens modalities that reduce the chance of developing contact lens-related complications.
Morgan et al. [13] found similar levels of compliance with lens wear among different European countries. Given that lockdown measures have been implemented differently across the world, further work should explore whether similar CL compliance habits have been reported elsewhere. The present results may not be fully transferable to other countries undergoing different restrictions during the lockdown. In addition, given the small proportion of rigid lens wearers in the UK [24] the current study was limited to exploring compliance of soft reusable lens wearers. The current sample size has limitations but the survey closed as guidance on social distancing changed when the government message changed from "Stay at Home" to "Stay Alert". Poorer compliance in males as compared to females has previously been reported [13]. In the present study only 21% of wearers using reusable lenses with multi-purpose solution were male, so this should be kept in mind when interpreting the findings from this study. In addition, with an online survey the possibility always exists for self-report bias as well as self-selection bias where those more compliant with lens wear and care might be more likely to complete the survey. If this was the case, this will make the current findings even more significant to ECPs. Hind et al. [35] noticed that optometrists do not routinely offer written advice regarding contact lens wear and care information. Thus, another limitation of the present work is that an assumption is made that wearers have been instructed appropriately in the first instance, but it is possible that poor compliance steams from inadequate information being given during initial instruction on lens care [36].
Finally, it is worth noting that 89% of respondents did not feel the need for any additional support managing their contact lens wear during the pandemic. This indicates that respondents were not experiencing any problems and considered CL wear to be safe during the COVID-19 pandemic.
In conclusion, this study shows that lens wearers showed good compliance with handwashing during the pandemic but lens wear and care was significantly worse for reusable lens wearers than daily disposable lens wearers. ECP should continue to educate patients to ensure compliance with lens wear and care during the pandemic.
Funding
None received for this study.
References
- 1.Khavandi S., Tabibzadeh E., Naderan M., Shoar S. Corona virus disease-19 (COVID-19) presenting as conjunctivitis: atypically high-risk during a pandemic. Cont Lens Anterior Eye. 2020;43:211–212. doi: 10.1016/j.clae.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daruich A., Martin D., Bremond-Gignac D. Ocular manifestation as first sign of Coronavirus Disease 2019 (COVID-19): Interest of telemedicine during the pandemic context. J Fr Ophtalmol. 2020;43:389–391. doi: 10.1016/j.jfo.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.2020. The Royal College of Ophthalmologists, Viral conjunctivitis and COVID-19 – a joint statement from The Royal College of Ophthalmologists and College of Optometrists.https://www.rcophth.ac.uk/2020/03/viral-conjunctivitis-and-covid-19-a-joint-statement-from-the-royal-college-of-ophthalmologists-and-college-of-optometrists/ [Accessed 28 May 2020] [Google Scholar]
- 4.Willcox M.D.P., Walsh K., Nichols J.J., Morgan P.B., Jones L.W. The ocular surface, coronaviruses and COVID‐19. Clin Exp Optom. 2020 doi: 10.1111/cxo.13088. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun C.B., Wang Y.Y., Liu G.H., Liu Z. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Front Public Health. 2020;8:155. doi: 10.3389/fpubh.2020.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones L., Walsh K., Willcox M., Morgan P., Nichols J. The COVID-19 pandemic: important considerations for contact lens practitioners. Cont Lens Anterior Eye. 2020;43:196–203. doi: 10.1016/j.clae.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerr C., Chauhan K. Devizes: Association of Contact Lens Manufacturers; 2020. The ACLM contact lens year book 2020. [Google Scholar]
- 8.Stapleton F., Keay L., Edwards K., Naduvilath T., Dart J.K.G., Brian G. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115:1655–1662. doi: 10.1016/j.ophtha.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Lam D.S., Houang E., Fan D.S., Lyon D., Seal D., Wong E. Incidence and risk factors for microbial keratitis in Hong Kong: comparison with Europe and North America. Eye. 2002;16:608–618. doi: 10.1038/sj.eye.6700151. [DOI] [PubMed] [Google Scholar]
- 10.Stapleton F., Edwards K., Keay L., Naduvilath T., Dart J.K.G., Brian G. Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology. 2012;119:1516–1521. doi: 10.1016/j.ophtha.2012.01.052. [DOI] [PubMed] [Google Scholar]
- 11.Fonn D., Jones L. Hand hygiene is linked to microbial keratitis and corneal inflammatory events. Cont Lens Anterior Eye. 2019;42:132–135. doi: 10.1016/j.clae.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 12.Cho P., Boost M.V. Daily disposable lenses: the better alternative. Cont Lens Anterior Eye. 2013;36:4–12. doi: 10.1016/j.clae.2012.10.073. [DOI] [PubMed] [Google Scholar]
- 13.Morgan P.B., Efron N., Toshida H., Nichols J.J. An international analysis of contact lens compliance. Cont Lens Anterior Eye. 2011;34:223–228. doi: 10.1016/j.clae.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Dumbleton K.A., Woods C.A., Jones L.W., Fonn D. The relationship between compliance with lens replacement and contact lens-related problems in silicone hydrogel wearers. Cont Lens Anterior Eye. 2011;34:216–222. doi: 10.1016/j.clae.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Dumbleton K.A., Richter D., Woods C.A., Aakre B.M., Plowright A., Morgan P.B. A multi-country assessment of compliance with daily disposable contact lens wear. Cont Lens Anterior Eye. 2013;36:304–312. doi: 10.1016/j.clae.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Dumbleton K.A., Spafford M.M., Sivak A., Jones L.W. Exploring compliance: a mixed-methods study of contact lens wearer perspectives. Optom Vis Sci. 2013;90:898–908. doi: 10.1097/OPX.0b013e3182956c46. [DOI] [PubMed] [Google Scholar]
- 17.Pesudovs K., Burr J.M., Harley C., Elliott D.B. The development, assessment, and selection of questionnaires. Optom Vis Sci. 2007;84:663–674. doi: 10.1097/OPX.0b013e318141fe75. [DOI] [PubMed] [Google Scholar]
- 18.Efron N., Morgan P.B. Rethinking contact lens aftercare. Clin Exp Optom. 2017;100(5):411–431. doi: 10.1111/cxo.12588. [DOI] [PubMed] [Google Scholar]
- 19.Young G. Cont Lens spectr. 2020. Diligent disinfection in 49 steps.https://www.clspectrum.com/issues/2012/february-2012/reader-and-industry-forum/ [Accessed 28 May 2020] [Google Scholar]
- 20.Wu Y.T., Willcox M., Zhu H., Stapleton F. Contact lens hygiene compliance and lens case contamination: a review. Cont Lens Anterior Eye. 2015;38(5):307–316. doi: 10.1016/j.clae.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 21.British Contact Lens Association . 2020. Contact Lens Wear and coronavirus (COVID-19) guidance.https://www.bcla.org.uk/Public/Public/Consumer/Contact-Lens-Wear-and-Coronavirus-guidance.aspx/ [Accessed 28 May 2020] [Google Scholar]
- 22.Centre for Ocular Research and Education . 2020. COVID-19 and contact lenses: the facts you need to know.https://core.uwaterloo.ca/covid-19/ [Accessed 28 May 2020] [Google Scholar]
- 23.Centres for Disease Control and Prevention . 2020. Healthy contact lens wear and care.https://www.cdc.gov/contactlenses/protect-your-eyes.html/ [Accessed 28 May 2020] [Google Scholar]
- 24.Morgan P.B., Woods C.A., Tranoudis I.G., Efron N., Jones L., Merchan N.L. International contact lens prescribing in 2019. Cont Lens Spectr. 2020;(January):26–32. [Google Scholar]
- 25.Morgan P.B. Contact lens wear during the COVID-19 pandemic. Cont Lens Anterior Eye. 2020;43:213. doi: 10.1016/j.clae.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osborn G., Fonn D., Zucaro A. Hand washing behavior of 1-Day contact lens wearers. Optom Vis Sci. 2017;94 E-abstract 175345. [Google Scholar]
- 27.Arshad M., Carnt N., Tan J., Ekkeshis I., Stapleton F. Water exposure and the risk of contact lens-related disease. Cornea. 2019;38:791–797. doi: 10.1097/ICO.0000000000001898. [DOI] [PubMed] [Google Scholar]
- 28.Zimmerman A.B., Richdale K., Mitchell G.L., Kinoshita B.T., Lam D.Y., Wagner H. Water exposure is a common risk behavior among Soft and gas-permeable contact lens wearers. Cornea. 2017;36:995–1001. doi: 10.1097/ICO.0000000000001204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arshad M., Carnt N., Tan J., Stapleton F. Compliance behaviour change in contact lens wearers: a randomised controlled trial [published online ahead of print, 2020 Jun 16. doi: 10.1038/s41433-020-1015-9. [DOI] [PMC free article] [PubMed]
- 30.Chalmers R.L., Keay L., Long B., Bergenske P., Giles T., Bullimore M.A. Risk factors for contact lens complications in US clinical practices. Optom Vis Sci. 2010;87:725–735. doi: 10.1097/OPX.0b013e3181f31f68. [DOI] [PubMed] [Google Scholar]
- 31.Chalmers R.L., Hickson-Curran S.B., Keay L., Gleason W.J., Albright R. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci. 2015;56:654–663. doi: 10.1167/iovs.14-15582. [DOI] [PubMed] [Google Scholar]
- 32.Wolffsohn J., Hall L., Mroczkowska S., Hunt O.A., Bilkhu P., Drew T. The influence of end of day silicone hydrogel daily disposable contact lens fit on ocular comfort, physiology and lens wettability. Cont Lens Anterior Eye. 2015;38:339–344. doi: 10.1016/j.clae.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Nagra M., Vianya-Estopa M., Wolffsohn J.S. Could telehealth help eye care practitioners adapt contact lens services during the COVID-19 pandemic? Cont Lens Anterior Eye. 2020;43:204–207. doi: 10.1016/j.clae.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.General Optical Council . 2020. Joint regulatory statement on remote consultations and prescribing.https://www.optical.org/en/news_publications/Publications/joint-statement-and-guidance-on-coronavirus-covid19.cfm/ [Accessed 27 April 2020] [Google Scholar]
- 35.Hind J., Williams O., Oladiwura D., Macdonald E. The differences between patient and optometrist experiences of contact lens hygiene education from the perspective of a Scottish university teaching hospital. Cont Lens Anterior Eye. 2020;43:185–188. doi: 10.1016/j.clae.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 36.Wu Y., Carnt N., Willcox M., Stapleton F. Contact lens and lens storage case cleaning instructions: whose advice should we follow? Eye Contact Lens. 2010;36(2):68–72. doi: 10.1097/ICL.0b013e3181cf8aff. [DOI] [PubMed] [Google Scholar]