Abstract
The medical system of Hong Kong has been heavily affected by COVID-19. Adaptations are necessary to continue clinical care, education, and research, while minimising the risk of infection of our staff and students. Here, we report our early experience in response to the challenge posed by the COVID-19 pandemic.
The translational potential of this article
This perspective can help to disseminate knowledge from an orthopaedic unit in a university hospital on overcoming the challenges of the COVID-19 pandemic, including clinical practice, education of medical students, and research.
Keywords: Clinical service, COVID-19, Education, Orthopaedics, Research
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a newly discovered coronavirus. The first confirmed case of COVID-19 identified in Hong Kong was on 23 January 2020. The Hong Kong government, in response, heightened the emergency level with the suspension of schools and hospital visiting arrangements on the 25 January 2020 in an attempt to reduce the regional spread of the virus. The first COVID-19 death was reported on 4 February 2020, and the hospitals adjusted their non-emergency medical service to reduce crowding of hospital areas on 12 February 2020. Even when faced with the threat of a second wave of COVID-19 cases arising from import-related infection starting on 19 March 2020, with the number of confirmed cases exceeding 1000 on 11 April 2020, Hong Kong’s handling of the pandemic was a relative success. However, since July, Hong Kong has been facing a third wave of COVID-19 infections. To date (18 July 2020), there have been 1886 confirmed cases, with 12 deaths, and 1294 patients have successfully completed treatment and been discharged. With meticulous care and stringent infection control, to date, there have been no confirmed cases of health care workers contracting COVID-19 from the workplace. Throughout this pandemic, the medical system of Hong Kong has inevitably been heavily affected, including orthopaedics services.
University hospitals have a responsibility to society, with objectives including clinical patient care, education, and research [1,2]. Although orthopaedic surgeons are not amongst the front-line staff in the fight against COVID-19, we must make changes to our practice in order to keep our staff and students safe. As the Department of the Orthopaedics and Traumatology of the Chinese University of Hong Kong (CUHK), we report our early experiences and adaptations made in response to the COVID-19 pandemic. Our experience can potentially benefit surgical communities who similarly have elective and emergency cases, as well as other medical professions who are involved with education and research.
Clinical
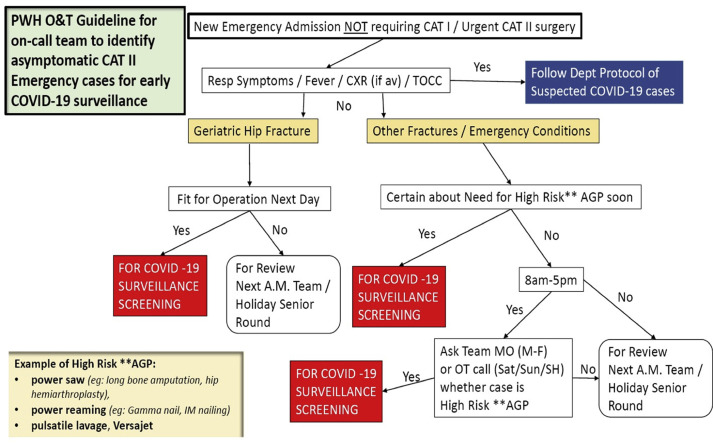
Since the initial confirmed case of COVID-19, there has been a significant impact on orthopaedic clinical services and workplace environments. There has been a growing emphasis on hand hygiene and protective wear, leading to increased use of personal protective equipment (PPE), face masks, alcohol-based sanitiser, and gloves. Patients going to the hospital are all asked a thorough Travel, Occupation, Cluster, and Contact (TOCC) history. Hospital management protocols have also been implemented for admissions and transfer into the orthopaedic wards (Fig. 1 ).
Fig. 1.
Current Prince of Wales Hospital Orthopaedics and Traumatology guideline for the on-call team.
The Orthopaedics departments also have heightened infection control measures for surgical procedures. In view of the uncertainty we could potentially face, elective, non-urgent orthopaedic operations have been postponed, with operations only performed for life-threatening or limb-threatening conditions. Patients requiring emergency operations are arranged for a COVID-19 test if deemed high risk. With evidence suggesting aerosol-generating procedures (AGPs) might have a high risk of transmission, for procedures such as intubation [3] and operations that require a power saw, power reaming, or pulsatile lavage [4], the use of N95 respirators with full PPE is required, while personnel within the operating theatre during these procedures are minimised. Towards the end of June 2020, we have accumulated over 300 postponed operations. Since April 2020, with a more stable supply of N95 respirators and PPE, elective surgeries have gradually been reinstated. The first elective surgeries to resume were the non-emergency but debilitating conditions, including patients with anterior cruciate ligament (ACL) tears requiring ACL reconstructions and patients with spinal stenosis for decompressive surgeries. In the months that followed, accompanied by the absence of outbreaks in Hong Kong, elective surgeries have resumed their normal numbers and scopes. The backlog cases have yet to be fully cleared, but our University Hospital, the Prince of Wales Hospital, is looking into the implementation of additional elective surgery sessions during out-of-office hours once the pandemic situation settles.
Regarding orthopaedic in-patient testing of COVID-19, as of July 2020, the departmental policy is for liberal testing of all suspicious cases. Thus, all febrile patients admitted to the orthopaedic ward will undergo COVID-19 tests. Test results are now available within several hours, and patients are isolated in the single-bed cubicle whilst awaiting the results; once negative, they will be allowed back into the general cubicle. An initial proposal to routinely test all pre-operative patients was not adopted due to the cost-effectiveness issues. Regarding resuscitation and major trauma call situations, all staff are required to be fully geared in PPE and N95 respirators while performing CPR or assessing a trauma patient in the Accident and Emergency Department (AED) resuscitation room.
The specialist outpatient clinic service has been maintained, but the attendance has dropped by around 40% due to the hesitation of patients coming to the hospital. The Clinical Management System (CMS), Hospital Authority, which allows clinicians to view patient electronic records, also had an additional travel history indicator implemented to prevent inaccurate reporting of travel history from patients. The indicator has information from the Hong Kong Immigration Department as a reference to facilitate taking patient travel history in the past 30 days. If TOCC is positive and fever is present, the patient is escorted to the AED. However, if the patient has a fever and no TOCC or the patient has no fever but TOCC, then the decision as to whether the patient is attended to is subject to the orthopaedic surgeon in charge.
Medical education
As one of the two medical schools in the region, CUHK carries a responsibility to continue the education of our 1500 medical students (~250 per year). All visitors and non-essential staff were prohibited from entering the hospital premises. This visitor ban also applied to all medical students; therefore, no ward or clinic-based education was permitted. In addition, to reduce the risk of infection, all face-to-face teaching (including those in non-clinical areas) was strongly discouraged; it was ultimately decided that teaching would be conducted online.
Although the Orthopaedic and Traumatology Department already had a robust amount of learning material, mostly implemented after the previous SARS outbreak [5], they were typically didactic lecture presentations and clinical examination videos [6]. In response to this, the department designed new teaching material and started using cloud-based video conferencing to replace the lost clinical sessions. Synchronous, real-time, online teaching was selected because it enabled a more dynamic exchange and superior active engagement of the students, with immediate feedback. We utilised cloud-based video-communication software that could support up to 300 real-time participants.
The first online orthopaedic teaching session was on 4 February 2020, and since then, over 80 sessions have been conducted. Attendance often exceeded the traditional bedside teaching, with over 100 participants routinely sitting in sessions originally intended for a group of 16 students. The format of the online teaching varied and included lecture-style sessions, demonstration of clinical skills and clinical case discussion with real/surrogate patients, real-time polling, and interactive questions and answers [7].
Examinations for medical students have been affected globally, with Italy opting to cancel all exams, while the United Kingdom announced the option of early provisional registration for medical students to facilitate their earlier admission to the health service as practicing doctors [8]. Locally, we have opted to proceed with the examinations, albeit with modifications. Adhering to infection control and social distancing recommendations, clinical bedside examinations with real patients were cancelled. More marks were given for the written papers, and surrogate patients were trained for the objective structured clinical exam (OSCE).
Telemedicine is the practice of remote patient care with the aid of modern technology. The use of telemedicine is not official for clinical use in our unit, but we are able to use it for the teaching of medical students. Our unit has set up the teaching of medical students via online clinics, with consent from patients. Due to COVID-19, hospital guidelines have set up restrictions for medical students, leading to a significant decrease in the amount of clinical exposure in wards and clinics. With the use of a live-feed camera at our clinic, we are able to see patients together with our medical students. The students also have the opportunity to take histories and to discuss real-time management with the patient and tutor. 3 More conveniently, tutors are also able to demonstrate physical examination techniques and clinical signs to the students. The advancement of technology used in medicine has made teaching medical students feasible during this time. However, the authors believe that face-to-face clinical examination and interaction with patients is still an important core value of medicine.
Research
Research is a key area for the CUHK, but, inevitably, the research activities at the CUHK have been affected by COVID-19. The CUHK has implemented special work arrangement measures for social distancing. Except for providing essential clinical and supportive services, all research personnel were asked to work from home. After 2 March 2020, staff members were allowed to return to the office with mandatory use of face masks and alternating work hours to reduce physical meetings. Online forms, including a health declaration and 14-day surveillance forms, were compulsory upon returning to work during this outbreak and peak period. All laboratories were closed, and research students required a special application for returning to the office.
Since non-essential visits have been restricted, clinical research projects have been suspended. Projects in their early stages may be affected since subjects may not be recruited, while others may be affected by the interrupted treatments or missing assessment appointments. For basic science research, both in vivo animal studies and in vitro studies have been affected due to the closure of laboratories, travel restrictions, and quarantine measures. All experiments started on live animals with extended ageing periods would have missed some time-point(s) for treatment or assessment. The time-points may require adjustments if possible; otherwise, the animals need to be sacrificed at a humane endpoint and replaced accordingly. Similar delay and replacement experiments are also affecting in vitro experiments.
Furthermore, research projects involving international collaboration are affected as the outbreak of COVID-19 is taking a sequential surging pattern across the world. As research institutes across the world are taking on travel restrictions and work-from-home measures, these research projects are expected to be delayed.
The COVID-19 pandemic has brought exceptional challenges to Hong Kong, including an economic toll. The Hong Kong government has responded to the needs of the public and society by providing anti-epidemic funds to help businesses stay afloat, to keep workers employed, to relieve financial burdens of individuals and businesses, and to assist the recovery of the economy once the epidemic is contained.
Since the beginning of this year, the government has launched three rounds of measures, totalling $287.5 billion, to assist affected industries and the public.
The unemployment rate of the community has been affected and increased to 5.9% in May, which is likely to rise with the continuous waves of COVID-19 infections. Although the university hospital is publicly funded and has no immediate plans for any budget cuts or salary reductions, it is of great importance for the hospital to continue providing quality health care that is affordable to the public in these difficult times.
Conclusion
As the number of confirmed COVID-19 cases continues to increase globally, it is important for health care workers to share their experience to aid in the fight against this viral pandemic. We share our experience from the perspective of a university hospital as the Department of Orthopaedics and Traumatology of CUHK.
The early experience we have shared here is by no means the final model. It is of great importance for us to adjust and adapt to the status of the pandemic in order to provide an effective service to the community. This experience may potentially benefit surgical specialties that similarly have elective and emergency cases, as well as other medical specialities that are involved with education and research.
Conflict of Interest
All authors declare no potential conflicts of interest.
Acknowledgements/Funding statement
We acknowledge Gene Chi-Wai Man, the Scientific Officer of the Evidence-Based Orthopaedic (EBO) Programme at CUHK, for his assistance in editing this manuscript. None of the authors have funding to declare.
References
- 1.Trybou J., Gemmel P., Desmidt S., Annemans L. Fulfillment of administrative and professional obligations of hospitals and mission motivation of physicians. BMC Health Serv Res. 2017;17(1):28. doi: 10.1186/s12913-017-1990-0. [In English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewkonia R.M. The missions of medical schools: the pursuit of health in the service of society. BMC Med Educ. 2001;1:4. doi: 10.1186/1472-6920-1-4. [In English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PloS One. 2012;7(4) doi: 10.1371/journal.pone.0035797. [In English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong K.C., Leung K.S. Current concepts review: transmission and prevention of occupational infections in orthopaedic surgeons. J Bone Joint Surg. 2004;86A(5):1065–1076. doi: 10.2106/00004623-200405000-00029. [In English] [DOI] [PubMed] [Google Scholar]
- 5.Leung J.Y.C., Kumta S.M., Jin Y., Yung A.L.K. Short review of the flipped classroom approach. Med Educ. 2014;48(11):1127. doi: 10.1111/medu.12576. [In English] [DOI] [PubMed] [Google Scholar]
- 6.Kyriakoulis K., Patelarou A., Laliotis A., Wan A.C., Matalliotakis M., Tsiou C. Educational strategies for teaching evidence-based practice to undergraduate health students: systematic review. J Educ Eval Health Prof. 2016;13:34. doi: 10.3352/jeehp.2016.13.34. [In English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung J.Y.C., Critchley L.A.H., Yung A.L.K., Kumta S.M. Introduction of virtual patients onto a final year anesthesia course: Hong Kong experience. Adv Med Educ Pract. 2011;2:71–83. doi: 10.2147/AMEP.S13037. [In English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joint statement: early provisional registration for final year medical students. General Medical Council; United Kingdom: 2020. https://www.gmc-uk.org/news/news-archive/early-provisional-registration-for-final-year-medical-students Available at: Accessed April 1, 2020. [Google Scholar]