Abstract
Background:
Previous studies that evaluated the prevalence, awareness and treatment of hypertension in Nigeria were either localized to some specific regions of the country or non-standardized thereby making evaluation of trend in hypertension care difficult.
Methods:
We used the World Health Organization (WHO) STEPwise approach to chronic disease risk factor surveillance to evaluate in a nationally representative sample of 4192 adult Nigerians selected from a rural and an urban community in one state in each of the six geo-political zones of the country.
Results:
The overall age-standardized prevalence of hypertension was 38.1% and this varied across the geo-political zones as follows: North-Central, 20.9%; North-East, 27.5%; North-West, 26.8%; South-East, 52.8%; South-South, 44.6%; and South-West, 42.1%. Prevalence rate did not differ significantly (p > 0.05) according to place of residence; 39.2% versus 37.5 %; urban vs rural. Prevalence of hypertension increased from 6.8% among subjects less than 30 years to 63.0% among those aged 70 years and above. Awareness was better (62.2% vs. 56.6%; P = 0.0272); treatment rate significantly higher (40.9 % vs. 30.8%; P < 0.0001) and control similar (14 vs. 10.8%) among urban compared to rural residents. Women were more aware of (63.3% vs. 52.8%; P < 0.0001); had similar (P > 0.05) treatment (36.7 vs. 34.3%) and control (33.9% vs. 35.5%) rates of hypertension compared to men.
Conclusion:
Our results suggest a large burden of hypertension in Nigeria and a closing up of the rural-urban gap previously reported. This calls for a change in public health policies anchored on a primary health care system to address the emerging disease burden occasioned by hypertension.
Keywords: Prevalence, Awareness, Treatment, Control, Hypertension, Africa, Blood pressure
Introduction
In 2016, high systolic blood pressure was reported by the Global Burden of Disease Risk Factors Collaborators as a leading cause of global disease burden in both men and women [1]. In sub-Saharan Africa, emerging epidemiological data suggest that hypertension has become a major public health challenge [2,3].
Wide variation in prevalence, awareness and treatment of hypertension are reported within and between countries of the region [3,4,5,6,7,8]. Various factors ranging from non-standardization of survey methods, use of varying thresholds for diagnosis of hypertension and non-report of age standardized prevalence rates make pooling of the data generated from various studies practically impossible. The overall result is dearth of evidence to inform robust health policies targeted at control of hypertension epidemic in the region.
Nigeria is the most populous country in sub-Saharan Africa and as such her health indices contributes substantially towards defining that of the entire sub-region. The available nationwide data on the epidemiology of hypertension in Nigeria was based on the Non-communicable disease survey published in 1997 [9]. This data is not only obsolete and no longer reliable as the threshold for the diagnosis of hypertension was a blood pressure of 160/95 mmHg as against the acceptable current threshold of 140/90 mmHg. Furthermore, that report did not include data on awareness, treatment and control of hypertension across various regions of Nigeria. Although pockets of regional surveys on hypertension have been conducted in various parts of Nigeria in the past decade, these studies when pooled together to derive national estimates are prone to errors as methodologies and sampling techniques vary widely across them [6,10,11,12,13]. In addition, a critical review of the regional surveys in the light of the national data suggests a distortion in the regional variation earlier documented in the national survey.
Removing the Mask on Hypertension (REMAH) study is a nationwide survey of hypertension aimed at defining the true burden of hypertension in Nigeria. This present report is intended to evaluate the regional and urban-rural variations in the prevalence, awareness, treatment and control of hypertension in Nigeria.
Methods
Study Population
REMAH was conducted in 12 communities across six states (one state in each of the six geo-political zones) of Nigeria between March 2017 and February 2018. The general study design and methods have been described in previous details [14]. In brief, we selected participants using a multi-stage sampling technique. The first stage involves random selection of one state from the six geopolitical zones. Guided by the administrative data of the 2015 general elections of the Independent National Electoral Commission (INEC), two (2) local government areas (LGAs) consisting of urban and rural communities were selected in the second stage. We selected state capitals including Abuja Municipal Area Council (North Central), Uyo for Akwa-Ibom (South-South), Ibadan-North for Oyo (South West), Gusau for Zamfara (North-West), Gombe municipal for Gombe (North-East), and Onitsha (the commercial city of the South East) as the urban communities. In the same order, Gwagwalada, Nsit Ubium, Akinyele, Bungudu, Akko and Oyi LGAs were randomly selected for sampling the rural community in these states. In the third and fourth stage respectively, one (1) ward from which one (1) polling unit was randomly selected each from the rural and urban LGAs (Supplementary Table 1). Trained field workers invited consented individuals in each study site to a mobile clinic stationed at a designated location within the community. Using standard methods, they measured blood pressure and anthropometric parameters, and obtained history of previous diagnosis and treatment of hypertension. Out of 4665 adults invited, 4197 consented; giving a response rate of 90%. Five participants had an odd blood pressure reading and were thus excluded from the final analysis.
REMAH study complied strictly with the guidelines for conducting research in human subjects as spelt out in Helsinki Declaration [15]. The University of Abuja Teaching Hospital Health Research Ethics Committee approved REMAH study.
Diagnosis of Hypertension
Observers received training on blood pressure measurement using the British Hypertension Society Video on Blood Pressure Measurement [16]. They measured brachial blood pressure by auscultation of the Korotkoff sounds at the non-dominant arm, according to the 2013 guidelines of the European Society of Hypertension/European Society of Cardiology (ESH/ESC) [17]. After the participants had rested in the sitting position for at least 5 minutes, the observers obtained five consecutive blood pressure readings at an interval of 30 to 60 seconds. Systolic and phase V diastolic blood pressures were determined to the nearest 2 mmHg. Standard cuffs that had a 12 × 24 cm inflatable portion were used. If the upper arm circumference exceeded 31cm, larger cuffs with 15 × 35 cm bladder were used instead. To address observer dependent errors inherent in the use of mercury sphygmomanometer, we applied three quality control measures previously deployed [14,18,19], to ensure good quality blood pressure measurement. Observers were trained to avoid odd readings, consecutive identical readings and zero end-digit preference. These three parameters were checked periodically and the observers retrained whenever any deviations below the expected standards were observed. A participant’s blood pressure was the average of the five consecutive blood pressure measurements. Hypertension was defined according to the 2013 ESH/ESC guidelines as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg and/or self-report treatment of hypertension using antihypertensive medications [17]. Among participants diagnosed hypertensive, awareness of hypertension was defined as previous diagnosis of hypertension by a health worker while treatment of hypertension was defined as self-reported use of prescribed medication for management of hypertension. Control of hypertension was defined as systolic blood pressure lower than 140 mmHg and diastolic blood pressure lower than 90 mmHg in a participant receiving treatment for hypertension. The denominator used to determine the control proportion was all hypertensive patients, treated and untreated. Prehypertension was defined according to JNC VII guidelines as systolic blood pressure between 120–139 mmHg and/or a diastolic BP between 80–89 mmHg.
Other Measurements
Anthropometric measurements were done using standard methods as described in details previously [14]. Body mass index (BMI) was derived accordingly as weight in kilogram divided by the square of height measured in meters. Field workers administered a modified WHO STEPs questionnaire to collect information on relevant medical history, alcohol and cigarette consumption, and intake of medications.
Database management and statistical analysis
We used SAS software version 9.4. (SAS Institute, Cary, NC) for database management and statistical analysis. To eliminate bias due to nonresponse and complex survey design (multistaged sampling technique), we standardized the prevalence of prehypertension and hypertension according to the age and sex structure of the 2006 Nigerian population census figures grouped in 10 years category [20]. Adjustment was done by assigning survey weights obtained from this data to each subject (Supplementary Table 1). The overall and subgroup prevalence of prehypertension and hypertension according to age and BMI groups were obtained using PROC SURVEYFREQ. Similarly, PROC SURVEYLOGISTIC was used to test for trend across age and BMI groups. We used mean and SD to report central tendency and spread of data. We compared mean values and proportions of variables of interest between two independent groups using Students t-test and chi-square statistic respectively.
Results
Characteristics of participants
Out of 4192 adult Nigerians that had good quality blood pressure readings, 2377 (63.9%) were women, 661 (19.0%) had no formal education and about a quarter (23.8%) were unemployed. The mean age and body mass index (BMI) were 46.7 years and 24.4kg/m2 respectively. Overall, about one out of every three (32.2%) consumed alcohol while one out of every thirty participants (3.4%) smoked cigarette. The mean systolic and diastolic blood pressures in the overall population were 129.3 mmHg and 79.8 mmHg respectively as shown in Table 1.
Table 1.
Socio-Demographic Characteristics of Participants by Geopolitical Zone.
| Overall | N/Central | N/East | N/West | S/East | S/South | S/West | |
|---|---|---|---|---|---|---|---|
| Number of participants (%) | 4192 (100) | 653 (15.6) | 1070 (25.5) | 709 (16.9) | 489 (11.7) | 543 (13.0) | 728 (17.4) |
| Women | 2377 (63.9) | 292 (47.5) | 600 (57.4) | 360 (59.6) | 327 (69.1) | 303 (61.2) | 495 (69.7) |
| Work Status | |||||||
| Govt. Employed | 693 (15.2) | 110 (22.1) | 172 (16.2) | 156 (20.3) | 66 (10.1) | 91 (14.3) | 98 (13.9) |
| Non-govt. Employed | 315 (5.51) | 108 (14.0) | 47 (4.35) | 17 (1.93) | 73 (9.34) | 20 (2.08) | 50 (7.42) |
| Self-Employed | 2110 (55.2) | 308 (41.5) | 536 (50.2) | 214 (35.8) | 252 (57.1) | 324 (65.6) | 476 (63.6) |
| Non-Paid | 16 (0.29) | 4 (0.54) | 2 (0.20) | 1 (0.05) | 4 (0.33) | 2 (0.13) | 3 (0.49) |
| Unemployed | 1044 (23.8) | 122 (21.9) | 319 (41.9) | 123 (17.4) | 92 (23.1) | 103 (18.0) | 99 (14.6) |
| Educational Status | |||||||
| No formal Education | 661 (19.0) | 28 (6.90) | 250 (24.3) | 238 (45.4) | 24 (4.72) | 19 (3.54) | 102 (12.8) |
| Primary Education | 903 (25.5) | 84 (14.19) | 246 (22.6) | 85 (13.0) | 129 (35.4) | 189 (35.2) | 170 (22.9) |
| Secondary Education | 1157 (25.4) | 216 (33.8) | 286 (26.4) | 171 (20.4) | 154 (31.6) | 164 (30.5) | 166 (23.4) |
| Tertiary Education | 1432 (30.1) | 316 (45.1) | 287 (26.7) | 214 (21.2) | 175 (23.3) | 165 (30.7) | 275 (40.8) |
| Smoking | 165 (3.40) | 50 (5.59) | 31 (2.98) | 21 (3.20) | 18 (5.6) | 30 (4.81) | 15 (2.03) |
| Drinking Alcohol | 1451 (32.2) | 348 (47.0) | 364 (33.5) | 14 (1.79) | 230 (56.7) | 323 (58.0) | 172 (26.0) |
| Mean ± SE | |||||||
| Age, Years | 46.7 ± 0.1 | 38.0 ± 0.1 | 43.8 ± 1.7 | 40.9 ± 2.3 | 51.5 ± 2.1 | 47.0 ± 1.7 | 50.0 ± 3.2 |
| SBP, mmHg | 129.3 ± 2.1 | 118.9 ± 1.5 | 120.8 ± 5.4 | 123.9 ± 0.1 | 136.9 ± 0.3 | 135.1 ± 0.7 | 131.5 ± 3.51 |
| DBP, mmHg | 79.8 ± 0.9 | 75.5 ± 0.3 | 75.8 ± 2.0 | 75.1 ± 0.7 | 82.3 ± 0.2 | 83.3 ± 0.4 | 82.1 ± 0.1 |
| BMI, kg/m2 | 24.4 ± 0.6 | 24.5 ± 0.5 | 24.3 ± 0.6 | 22.0 ± 0.1 | 26.5 ± 1.5 | 24.2 ± 0.2 | 24.9 ± 5.7 |
Systolic and diastolic blood pressures were derived from the average of five consecutive auscultatory readings Govt-Employed = Government Employed; Non-Govt Employed = Non-Government Employed.
Prevalence of hypertension
Table 2 shows the crude and age-standardized prevalence of hypertension according to sex and place of residence. The prevalence of hypertension overall was 38.1%, 41.8% in women and 31.8% in men. The prevalence rate of 37.5% among the rural dwellers was similar (p > 0.05) to 39.2% among their urban counterparts. Of the six regions, the South-East had the highest prevalence of hypertension (52.8%) while the lowest rate of 20.9% was observed in the North-Central region. Tables 3 and 4 show the prevalence of hypertension according to different categories of age groups and BMI. Prevalence of hypertension increased steadily from 6.8% among participants aged 30 years and below to 63.0% among those 70 years and above (p for trend < 0.0001). Likewise, prevalence also increased from 29.2% among leaner participants with BMI less than 25 kg/m2 to 75.1% among those with BMI of 40 kg/m2 or more (p for trend < 0.0001).
Table 2.
Crude and age-standardized prevalence of hypertension according to sex and place of residence.
| Region | Sex | Site | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Rural | Urban | |||||||||||||
| N | nHT | Crude % |
Adjusted* % |
N | nHT | Crude % |
Adjusted % |
N | nHT | Crude % |
Adjusted % |
N | nHT | Crude % |
Adjusted % |
|
| N/Central | 361 | 87 | 24.1 | 23.0 | 292 | 53 | 18.2 | 18.6 | 196 | 39 | 19.9 | 20.0 | 457 | 101 | 22.1 | 22.1 |
| N/East | 470 | 120 | 25.5 | 24.3 | 600 | 168 | 28.0 | 29.9 | 788 | 192 | 24.4 | 25.0 | 282 | 96 | 34.0 | 34.2 |
| N/West | 349 | 69 | 19.8 | 21.5 | 360 | 95 | 26.4 | 30.4 | 398 | 109 | 27.4 | 28.2 | 311 | 55 | 17.7 | 17.5 |
| S/East | 162 | 71 | 43.8 | 38.0 | 327 | 181 | 55.4 | 59.5 | 176 | 91 | 51.7 | 53.1 | 313 | 161 | 51.4 | 52.2 |
| S/South | 240 | 98 | 40.8 | 41.1 | 303 | 138 | 45.5 | 46.8 | 321 | 144 | 44.9 | 45.1 | 222 | 92 | 41.4 | 41.6 |
| S/West | 233 | 89 | 38.2 | 37.5 | 495 | 215 | 43.4 | 44.1 | 295 | 129 | 43.7 | 44.4 | 433 | 175 | 40.4 | 41.1 |
| Overall | 1815 | 543 | 29.4 | 31.8 | 2377 | 850 | 35.8 | 41.8 | 2174 | 704 | 32.4 | 37.5 | 2018 | 680 | 33.7 | 39.2 |
N = Number in group; nHT = Number of Hypertensive subjects. * Standardized to the 2006 National Population Census.
Table 3.
Prevalence of Hypertension according to different age groups.
| Region | <30 Yrs | 30–39Yrs | 40–49Yrs | 50–59Yrs | 60–69Yrs | >70Yrs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No in Group | HT (%) | No in Group | HT (%) | No in Group | HT (%) | No in Group | HT (%) | No in Group | HT (%) | No in Group | HT (%) | |
| N/Central | 172 | 5 (4.12) | 214 | 35 (14.9) | 155 | 30 (18.4) | 77 | 16 (24.7) | 26 | 3 (11.0) | 9 | 8 (81.2) |
| N/East | 261 | 7 (2.78) | 243 | 31 (12.9) | 208 | 66 (32.1) | 136 | 57 (42.5) | 121 | 70 (57.8) | 101 | 57 (58.1) |
| N/West | 266 | 18 (6.28) | 160 | 15 (8.24) | 116 | 31 (27.1) | 88 | 44 (45.2) | 42 | 33 (81.5) | 37 | 23 (63.5) |
| S/East | 45 | 6 (12.4) | 84 | 17 (24.1) | 119 | 61 (56.2) | 128 | 87 (67.6) | 67 | 48 (63.1) | 46 | 33 (71.8) |
| S/South | 119 | 16 (12.1) | 114 | 35 (29.2) | 116 | 58 (47.9) | 85 | 53 (65.4) | 67 | 45 (65.4) | 42 | 29 (69.2) |
| S/West | 92 | 6 (6.56) | 108 | 21 (20.8) | 147 | 69 (46.5) | 155 | 83 (54.9) | 123 | 66 (53.6) | 103 | 59 (58.2) |
| Rural | 454 | 21 (6.29) | 434 | 60 (15.9) | 410 | 150 (40.5) | 333 | 155 (51.8) | 281 | 163 (61.0) | 262 | 155 (62.1) |
| Urban | 501 | 37 (7.74) | 489 | 94 (21.7) | 451 | 182 (43.3) | 336 | 201 (61.0) | 165 | 112 (59.9) | 76 | 54 (65.7) |
| Overall | 955 | 58 (6.84) | 923 | 154 (18.1) | 861 | 332 (41.7) | 669 | 356 (55.5) | 446 | 275 (60.6) | 338 | 209 (63.0) |
Hypertension was systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg and/or use of antihypertensive medication.
Table 4.
Prevalence of Hypertension according to different BMI categories.
| <25 Kg/m2 | 25-29 Kg/m2 | 30-34 Kg/m2 | 35-39 Kg/m2 | ≥40 Kg/m2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No in Group | HT (%) | No in Group | HT (%) | No in Group | HT (%) | No in Group | HT (%) | No in Group | HT (%) | |
| N/Central | 364 | 43 (10.3) | 192 | 55 (29.7) | 73 | 28 (45.3) | 18 | 12 (70.7) | 6 | 2 (26.7) |
| N/East | 665 | 136 (20.8) | 274 | 86 (32.0) | 91 | 42 (47.2) | 31 | 18 (58.2) | 9 | 6 (68.2) |
| N/West | 545 | 97 (21.5) | 126 | 43 (41.7) | 24 | 12 (47.8) | 9 | 7 (82.2) | 5 | 5 (100) |
| S/East | 157 | 20 (10.6) | 166 | 87 (54.5) | 105 | 65 (65.3) | 46 | 34 (73.9) | 15 | 12 (85.2) |
| S/South | 320 | 109 (36.7) | 146 | 72 (48.6) | 56 | 36 (63.5) | 15 | 13 (95.5) | 6 | 6 (100) |
| S/West | 426 | 154 (36.2) | 185 | 83 (44.1) | 80 | 44 (55.0) | 26 | 16 (61.1) | 11 | 7 (66.3) |
| Rural | 1466 | 384 (30.5) | 508 | 206 (46.8) | 143 | 73 (56.7) | 46 | 34 (79.8) | 11 | 7 (76.2) |
| Urban | 1011 | 209 (28.5) | 581 | 220 (40.3) | 286 | 154 (57.1) | 99 | 66 (62.9) | 41 | 31 (74.6) |
| Overall | 2477 | 593 (29.9) | 1089 | 426 (44.0) | 429 | 227 (56.9) | 145 | 100 (70.2) | 52 | 38 (75.1) |
Hypertension was systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg and/or use of antihypertensive medication.
Prevalence of Prehypertension
According to Table 5, about one fifth of the entire study population had prehypertension; 54.5% and 45.5% reside in the urban and rural area respectively. The prevalence of prehypertension was higher among participants aged less than 50 years when compared to the older ones (22.5% vs. 15.4%; p = 0.0334).
Table 5.
Age Distribution and Prevalence of Prehypertension.
| <30 Yrs | 30–39Yrs | 40–49Yrs | 50–59Yrs | 60–69Yrs | >70Yrs | Overall | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No in Group | PreHT (%) | No in Group | PreHT (%) | No in Group | PreHT (%) | No in Group | PreHT (%) | No in Group | PreHT (%) | No in Group | PreHT (%) | No in Group | PreHT (%) | |
| N/Central | 172 | 20 (13.6) | 214 | 32 (17.0) | 155 | 30 (18.4) | 77 | 16 (24.7) | 26 | 3 (11.0) | 9 | – | 653 | 101 (16.8) |
| N/East | 261 | 44 (17.3) | 243 | 46 (19.4) | 208 | 42 (19.6) | 136 | 34 (24.7) | 121 | 16 (13.2) | 101 | 9 (8.35) | 1070 | 191 (17.8) |
| N/West | 266 | 40 (9.61) | 160 | 33 (18.2) | 116 | 18 (16.4) | 88 | 12 (9.36) | 42 | 3 (5.84) | 37 | 8 (21.9) | 709 | 114 (13.4) |
| S/East | 45 | 6 (9.05) | 84 | 18 (19.1) | 119 | 33 (23.5) | 128 | 12 (8.08) | 67 | 6 (10.7) | 46 | 1 (0.54) | 489 | 76 (12.1) |
| S/South | 119 | 44 (39.2) | 114 | 35 (29.6) | 116 | 32 (27.9) | 85 | 17 (18.0) | 67 | 11 (19.6) | 42 | 6 (13.3) | 543 | 145 (26.2) |
| S/West | 92 | 28 (32.1) | 108 | 36 (32.5) | 147 | 37 (25.6) | 155 | 29 (18.4) | 123 | 24 (20.0) | 103 | 22 (20.3) | 728 | 176 (24.3) |
| Rural | 454 | 72 (16.5) | 434 | 81 (21.0) | 410 | 150 (40.5) | 333 | 62 (14.8) | 281 | 37 (13.3) | 262 | 36 (14.0) | 2174 | 365 (37.5) |
| Urban | 501 | 110 (29.2) | 489 | 119 (29.2) | 451 | 115 (27.6) | 336 | 58 (17.6) | 165 | 26 (21.1) | 76 | 10 (15.5) | 2018 | 438 (24.7) |
| Overall | 955 | 182 (21.3) | 923 | 200 (24.1) | 861 | 192 (23.0) | 669 | 120 (15.9) | 446 | 63 (15.9) | 338 | 46 (14.3) | 4192 | 803 (19.7) |
Prehypertension is a systolic blood pressure between 130–139 mmHg and/or diastolic BP between 80–89 mmHg.
Awareness of Hypertension
Six out of every ten hypertensive patients were aware of their status. More women (65.7%) compared to men (34.3%) were aware of their hypertension status (p = 0002). In comparison to the rural areas, participants in the urban area were more aware (p = 0.0099) of their status (52.2% vs. 47.8%). Figure 1 shows the awareness status according to regions.
Figure 1.
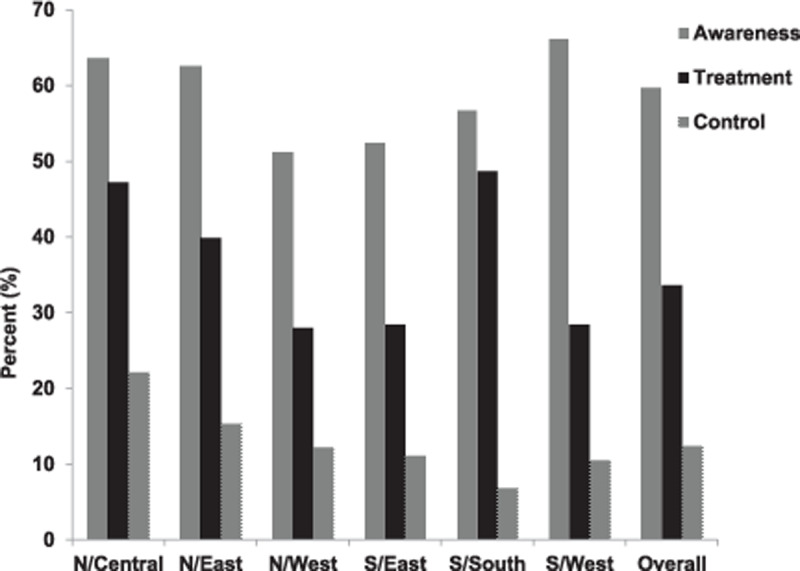
Awareness (vertical lines), treatment (solid) and control (dots) of hypertension across the six geopolitical zones and the overall population. Awareness includes subjects previously diagnosed of hypertension. Treatment includes hypertensives patients on antihypertensive medication and control includes hypertensive patients receiving treatment whose systolic and diastolic BP are less than 140 and 90 mmHg respectively.
Treatment of Hypertension
About one third of hypertensive patients (33.6%, 95%CI, 33.2–38.4%) were receiving treatment for their condition with no significant difference between women and men (36 vs 34.3%; p = 0.3573). More urban dwellers receive treatment when compared to their rural counterparts (40.9 vs. 30.8%; p < 0.0001). Figure 1 shows the treatment status according to regions.
Control of Hypertension
Among hypertensive patients, only 12.4% had their blood pressure under control. Overall, control rate among women was similar to men (12.2 vs. 12.5%; p = 0.8696). Likewise, control rate did not differ significantly between the urban (14.0) and their rural (10.8%) counterparts; (p = 0.0727). Figure 1 shows the control rate according to regions.
Hypertension Care Cascade
The care cascade shown in Figure 2 demonstrates significant loss to care at different levels along the hypertension treatment continuum. Of all hypertensive patients, 14.2% had never been screened; while about 35% of those screened remained undiagnosed. Of those diagnosed, 36% were untreated; and among the treated, two-thirds (65.4%) had uncontrolled blood pressure.
Figure 2.
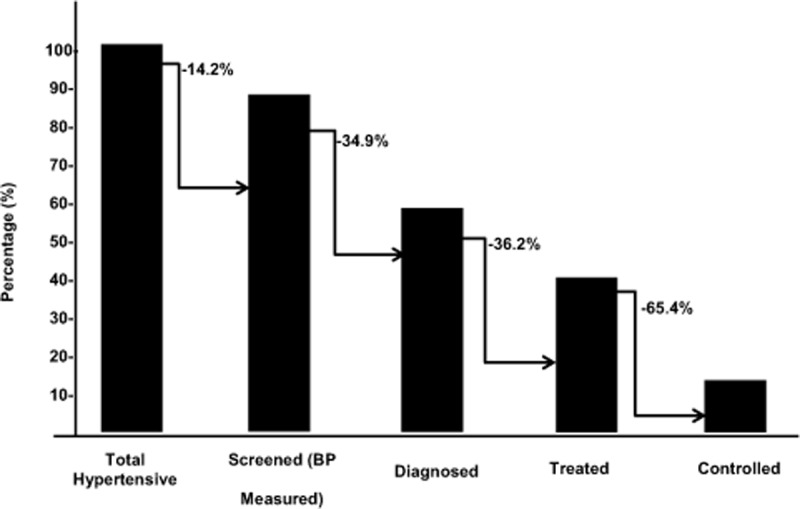
Hypertension Care Continuum Cascade. All hypertensive subjects whether diagnosed or undiagnosed is represented as 100%. Of these, 14.2% have never been screened for hypertension, 34.9% has been screened but not diagnosed, 36.2% have been diagnosed but not receiving treatment and 65.4% were treated but their blood pressure was still uncontrolled.
Discussion
The key findings of our study were that 38% of adult Nigerians aged 18 years and above were hypertensive. Out of the hypertensive subjects, 60% were aware of their status, one-third were receiving treatment and 12% had their blood pressure under control. Prevalence of hypertension ranged from 20.9% in the North-Central to 52.8% in the South-East region. Hypertension was as common in the rural as in the urban areas; however, the urban dwellers were more aware of and received treatment for the condition more than their rural counterparts.
Hitherto, the non-communicable disease survey of 1997 (NCD 97) has remained the only available primary nationwide survey data on the epidemiology of hypertension in Nigeria [9]. The survey included 19,997 Nigerians drawn from about 13 states of the country and spread across rural and urban communities. The investigators used a threshold blood pressure of 160/95 mmHg for the diagnosis of hypertension and reported that the prevalence of hypertension was 11.2%, 14% and 9.8% in overall, urban and rural areas respectively. In terms of the geographic spread, the semi-desert area corresponding to the North-West geopolitical region had the highest prevalence of hypertension. Although it is difficult to compare the present study with the NCD 97 because different diagnostic criteria were employed; the narrowed urban-rural gap and the changes in the geographic/regional distribution of the prevalence of hypertension are two aspects that deserve some discussion.
The narrowing urban-rural gap in the prevalence of hypertension may be related to the increasing urbanization of Nigerian rural areas with the attendant shift towards the lifestyle that fuel non-communicable diseases including hypertension [21]. Population growth results in dwindling land for farming thus encouraging rural dwellers to engage in more non-farm economic activities [22,23]. The non-farm activities as opposed to the manual labor driven farm activities encourage sedentary life style and consumption of high-salt processed food. A review of previous studies that evaluated the urban-rural difference in the prevalence of hypertension in South-East Nigeria [24], elsewhere in sub-Saharan Africa [25,26]; Southern America [27], and China suggest either a narrowing of the rural urban disparity or even a trend towards a higher prevalence in the rural compared to the urban areas in some of the studies [11,25,28,29]. Although prevalence of hypertension is obviously increasing in the rural populations of Nigeria, the rate of awareness and treatment has remained significantly higher in the urban as compared to the rural areas. This is consistent across the aforementioned studies conducted in different regions of the world.
Another clear difference between the current report and the 1997 NCD survey is the assertion that the prevalence of hypertension was higher in the semi-desert region compared to the rain forest region or South-East Nigeria. Our report and indeed various other systematic/narrative reviews published in the last decade which tried to analyse data obtained from individual smaller studies carried out in different parts of the Nigeria, agreed that prevalence of hypertension was highest in South-East Nigeria [4,7]. The reason for this epidemiological shift is unknown however; the effect of the Nigerian civil war whose devastating effect was majorly felt in South-East Nigeria may throw some light on this epidemiological puzzle. The war which occurred between 1967 and 1970 witnessed a high level of humanitarian crisis with hunger and famine [30,31], a condition under which most pregnant women had their babies. Children born during this period are now at the middle age of their life, the period during which hypertension and other non-communicable diseases begin to manifest. A growing body of evidence has clearly shown that the root of many NCDs in adults are traceable to unfavourable intrauterine and early childhood period [32,33,34,35]. Hult and Colleagues investigated this line of thought among 1339 adults in a southeastern city of Nigeria [36]. They compared prevalence of hypertension, diabetes mellitus and impaired glucose tolerance among the three groups subdivided based on whether the individual was born before, during or after the war. In comparison with unexposed offspring, being an offspring of a starving pregnant woman, (i.e. those born during the war) was associated with significant increases in the prevalence of hypertension (9.5% vs. 24%) and impaired glucose tolerance or diabetes (8.0% vs. 13%).
Although it is difficult to compare our result with the contemporary data emanating from other African countries due to heterogeneity in study methodology [3,26,37]; our results suggest that the prevalence of hypertension in Nigeria is among the highest in Africa. A review of the 20 countries in Africa who undertook WHO STEPs survey between 2003 and 2009 indicates that the prevalence of hypertension ranged from 8.2 % in Eritrea to 38% in Seychelles [38].
In comparison to the 1997 survey [9], our result suggests that awareness of hypertension increased by about 50% from 33.8% to 60% over a 20 year period. Although this figure is higher than the average of 52.7% reported for the developing countries [39], much lower levels were observed in the rural areas. Despite this seeming progress, this report shows a significant loss along the care continuum highlighting a high rate of unmet needs in hypertension care in Nigeria as only 12% of the hypertensive patients in Nigeria were treated and controlled. This finding is similar to the result of a 2011 health and nutrition survey in South Africa where the authors reported that only 9% of the hypertensive patients were treated and controlled [40]. Several factors ranging from access to health care, poor health seeking behaviour, dysfunctional health system, therapeutic inertia and patients’ non-adherence to prescribed therapies may be responsible for the huge loss in care of hypertension [41,42].
Our results should be interpreted within the context of the potential limitations. Sampling frame from which the participants were drawn was not known as there was no register that contained the entire inhabitants of each community studied. This would have made our sample truly random as the consent would have been given by individuals who had a prior knowledge of their hypertension status. However, we did a thorough community mobilization where the inhabitants were duly educated on the need to participate in the study irrespective of their status. Furthermore, home visits by research assistants encouraged participation. On the whole, a participation rate of 90% was achieved.
A repeat blood pressure measured after at least two weeks apart would have ensured true diagnosis of hypertension according to guideline. We however, averaged five blood pressure readings which approximates more closely to an individual’s usual blood pressure. Furthermore, we deployed standardized methodology to ensure good quality of blood pressure measurement throughout the entire period of the survey.
Perspectives
This survey came almost two decades after the NCD 97 survey and due to the obvious reasons that have already been discussed [9]; it was difficult to assess the trend in hypertension care, a process that is needed for setting priorities and targets for NCD control. It has been reported that about 28 million of NCD deaths in low and middle income countries are due to weak health systems of which lack of adequate data is a major component. To address this challenge, the “World Health Organization Global Action Plan 2013 to 2020” recommended that member nations should have a stepwise approach to surveillance (STEPS) survey or a comprehensive health examination survey every five years [43]. Nigeria and many other developing countries have not yet attained this target. This can be achieved if the STEPS survey is integrated into the National Health and Demographic survey currently running in Nigeria and other developing countries of Africa. Furthermore, data on hypertension can easily be obtained from volunteers within community groups who would be trained on how to measure blood pressure using semi-automated validated monitors.
Additional File
The additional file for this article can be found as follows:
Multi-staged Sampling of Subjects and Weighting by Design, Age and Sex.
Acknowledgements
The authors gratefully acknowledge the traditional and community leaders who supported the REMAH project by mobilizing their respective communities to participate. They include His Royal Highness (HRH) Igwe Charles Anikweze, Nnamenyi III of Awkuzu, Ven Isreal Odita, the Archdeacon, Omagba Archdeaconry (Anglican Communion) Onitsha; HRH Monday Udoewah, the clan head of Ubium Clan, Nsit Ubium LGA, Akwa Ibom State; Mr. Habila N. Garba, district head Ture District, Kaltungo Chiefdom, Kaltungo LGA, Gombe State; Alhaji Adamu Musa, chairman Shongo Housing Estate Residents’ Association (SHERA) Gombe State; HRH Alhaji Attahiru Bungudu, Emir of Bungudu, Zamfara; Prof. Oladepo Oladimeji, Department of Health Promotion and Education, University of Ibadan, and a leader of Ashi community, Bodija, Ibadan. Mrs. Maureen Amaechi provided valuable administrative and clerical support to REMAH project.
Funding Statement
National Research Fund (batch iv), Tertiary Education Trust Fund (TETFUND).
Funding Information
National Research Fund (batch iv), Tertiary Education Trust Fund (TETFUND).
Competing Interests
The authors have no competing interests to declare.
References
- 1.Risk FC. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017; 390(10100): 1345–422. DOI: 10.1016/S0140-6736(17)32366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Addo J, Smeeth L, Leon DA. Hypertension in sub-saharan Africa: a systematic review. Hypertension. 2007; 50(6): 1012–8. DOI: 10.1161/HYPERTENSIONAHA.107.093336 [DOI] [PubMed] [Google Scholar]
- 3.Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: A systematic review. BMC Cardiovasc Disord. 2013; 13: 54 DOI: 10.1186/1471-2261-13-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogah OS, Okpechi I, Chukwuonye II, Akinyemi JO, Onwubere BJ, Falase AO, et al. Blood pressure, prevalence of hypertension and hypertension related complications in Nigerian Africans: A review. World J Cardiol. 2012; 4(12): 327–40. DOI: 10.4330/wjc.v4.i12.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mugwano I, Kaddumukasa M, Mugenyi L, Kayima J, Ddumba E, Sajatovic M, et al. Poor drug adherence and lack of awareness of hypertension among hypertensive stroke patients in Kampala, Uganda: A cross sectional study. BMC Res Notes. 2016; 9: 3 DOI: 10.1186/s13104-015-1830-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekwunife OI, Udeogaranya PO, Nwatu IL. Prevalence, awareness, treatment and control of hypertension in a nigerian population. Health. 2010; 2: 731–5. DOI: 10.4236/health.2010.27111 [DOI] [Google Scholar]
- 7.Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens. 2015; 33(2): 230–42. DOI: 10.1097/HJH.0000000000000413 [DOI] [PubMed] [Google Scholar]
- 8.Akinlua JT, Meakin R, Umar AM, Freemantle N. Current Prevalence Pattern of Hypertension in Nigeria: A Systematic Review. PLoS One. 2015; 10(10): e0140021 DOI: 10.1371/journal.pone.0140021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akinkugbe OO. Non-Communicabe Diseases in Nigeria Lagos, Nigeria: Federal Ministry of Health and Social Services; 1997. [Google Scholar]
- 10.Olatunbosun ST, Kaufman JS, Cooper RS, Bella AF. Hypertension in a black population: Prevalence and biosocial determinants of high blood pressure in a group of urban Nigerians. J Hum Hypertens. 2000; 14(4): 249–57. DOI: 10.1038/sj.jhh.1000975 [DOI] [PubMed] [Google Scholar]
- 11.Okpechi IG, Chukwuonye II, Tiffin N, Madukwe OO, Onyeonoro UU, Umeizudike TI, et al. Blood pressure gradients and cardiovascular risk factors in urban and rural populations in Abia State South Eastern Nigeria using the WHO STEPwise approach. PLoS One. 2013; 8(9): e73403 DOI: 10.1371/journal.pone.0073403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Isezuo SA, Sabir AA, Ohwovorilole AE, Fasanmade OA. Prevalence, associated factors and relationship between prehypertension and hypertension: A study of two ethnic African populations in Northern Nigeria. J Hum Hypertens. 2011; 25(4): 224–30. DOI: 10.1038/jhh.2010.56 [DOI] [PubMed] [Google Scholar]
- 13.Ulasi II, Ijoma CK, Onwubere BJ, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in enugu, Nigeria. Int J Hypertens. 2011; 2011: 869675 DOI: 10.4061/2011/869675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nwakile PC, Chori BS, Danladi B, Umar A, Okoye IC, Nwegbu M, et al. Removing the mask on hypertension (REMAH) study: Design; quality of blood pressure phenotypes and characteristics of the first 490 participants. Blood Press. 2019; 1–10. DOI: 10.1080/08037051.2019.1612706 [DOI] [PubMed] [Google Scholar]
- 15.41st World Medical Assembly. Declaration of Helsinki: Recommendations guiding physicians in biomedical research involving human subjects. Bull Pan Am Health Organ. 1990; 24: 606–9. [Google Scholar]
- 16.BHS DVD on BP Measurement. 2007. Ref Type: Online Source. [Google Scholar]
- 17.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013; 34(28): 2159–219. DOI: 10.1093/eurheartj/eht151 [DOI] [PubMed] [Google Scholar]
- 18.Odili AN, Ameh VO, Ogedengbe J, Staessen JA. Quality of blood pressure phenotype in the Nigerian populaion research on environment gene and health. Blood Press Monit. 2014; 19: 220–5. DOI: 10.1097/MBP.0000000000000053 [DOI] [PubMed] [Google Scholar]
- 19.Lu YC, Li SS, Zhang HF, Odili AN, Yao WM, Gong L, et al. Quality control of the blood pressure phenotype in the Gaoyou population study. Blood Press. 2016; 25(3): 162–8. DOI: 10.3109/08037051.2015.1110936 [DOI] [PubMed] [Google Scholar]
- 20.National Population Commission (NPC) [Nigeria] and ICFMacro. Nigeria Demographic and Health Survey 2008 Abuja, Nigeria: 10-2-2013. National Population Commission and ICF Macro. [Google Scholar]
- 21.Aliyu AA, Amadu L. Urbanization, cities, and health: The challenges to Nigeria – A review. Ann Afr Med. 2017; 16(4): 149–58. DOI: 10.4103/aam.aam_1_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barrett CB, Reardon T, Webb P. Nonfarm income diversification and household livelihood strategies in rural Africa: Concepts, dynamics, and policy implications. Food Policy. 2001; 26(4): 315–31. DOI: 10.1016/S0306-9192(01)00014-8 [DOI] [Google Scholar]
- 23.Davis B, Winters P, Carletto G, Covarrubias K, Quiñones EJ, Zezza A, et al. A Cross-Country Comparison of Rural Income Generating Activities. World Development. 2010; 38(1): 48–63. DOI: 10.1016/j.worlddev.2009.01.003 [DOI] [Google Scholar]
- 24.Okpechi IG, Chukwuonye II, Tiffin N, Madukwe OO, Onyeonoro UU, Umeizudike TI, et al. Blood pressure gradients and cardiovascular risk factors in urban and rural populations in Abia State South Eastern Nigeria using the WHO STEPwise approach. PLoS One. 2013; 8(9): e73403 DOI: 10.1371/journal.pone.0073403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rush KL, Goma FM, Barker JA, Ollivier RA, Ferrier MS, Singini D. Hypertension prevalence and risk factors in rural and urban Zambian adults in western province: A cross-sectional study. Pan Afr Med J. 2018; 30: 97 DOI: 10.11604/pamj.2018.30.97.14717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Damasceno A, Azevedo A, Silva-Matos C, Prista A, Diogo D, Lunet N. Hypertension prevalence, awareness, treatment, and control in Mozambique: Urban/rural gap during epidemiological transition. Hypertension. 2009; 54: 77–83. DOI: 10.1161/HYPERTENSIONAHA.109.132423 [DOI] [PubMed] [Google Scholar]
- 27.Lamelas P, Diaz R, Orlandini A, Avezum A, Oliveira G, Mattos A, et al. Prevalence, awareness, treatment and control of hypertension in rural and urban communities in Latin American countries. J Hypertens. 2019; 37(9): 1813–21. DOI: 10.1097/HJH.0000000000002108 [DOI] [PubMed] [Google Scholar]
- 28.Song H, Feng D, Wang R, Yang J, Li Y, Gao J, et al. The urban-rural disparity in the prevalence and risk factors of hypertension among the elderly in China-a cross-sectional study. PeerJ. 2019; 7: e8015 DOI: 10.7717/peerj.8015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xing L, Jing L, Tian Y, Lin M, Du Z, Yan H, et al. Urban-Rural disparities in status of hypertension in northeast China: A population-based study, 2017–2019. Clin Epidemiol. 2019; 11: 801–20. DOI: 10.2147/CLEP.S218110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aall C. Relief, nutrition and health problems in the Nigerian-Biafran war. J Trop Pediatr (1967). 1970; 16(2): 70–90. DOI: 10.1093/tropej/16.2.70 [DOI] [PubMed] [Google Scholar]
- 31.Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993; 341(8850): 938–41. DOI: 10.1016/0140-6736(93)91224-A [DOI] [PubMed] [Google Scholar]
- 32.Leon DA, Lithell HO, Vagero D, Koupilova I, Mohsen R, Berglund L, et al. Reduced fetal growth rate and increased risk of death from ischaemic heart disease: Cohort study of 15 000 Swedish men and women born 1915-29. BMJ. 1998. 25; 317(7153): 241–5. DOI: 10.1136/bmj.317.7153.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yajnik CS. Early life origins of insulin resistance and type 2 diabetes in India and other Asian countries. J Nutr. 2004; 134(1): 205–10. DOI: 10.1093/jn/134.1.205 [DOI] [PubMed] [Google Scholar]
- 34.de Boo HA, Harding JE. The developmental origins of adult disease (Barker) hypothesis. Aust N Z J Obstet Gynaecol. 2006; 46(1): 4–14. DOI: 10.1111/j.1479-828X.2006.00506.x [DOI] [PubMed] [Google Scholar]
- 35.Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993; 341(8850): 938–41. DOI: 10.1016/0140-6736(93)91224-A [DOI] [PubMed] [Google Scholar]
- 36.Hult M, Tornhammar P, Ueda P, Chima C, Bonamy AK, Ozumba B, et al. Hypertension, diabetes and overweight: Looming legacies of the Biafran famine. PLoS One. 2010; 5(10): e13582 DOI: 10.1371/journal.pone.0013582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Longo-Mbenza B, Ngoma DV, Nahimana D, Mayuku DM, Fuele SM, Ekwanzala F, et al. Screen detection and the WHO stepwise approach to the prevalence and risk factors of arterial hypertension in Kinshasa. Eur J Cardiovasc Prev Rehabil. 2008; 15(5): 503–8. DOI: 10.1097/HJR.0b013e3282f21640 [DOI] [PubMed] [Google Scholar]
- 38.van d V, Akinyi H, Oti S, Olajide A, Agyemang C, Aboderin I, et al. Status report on hypertension in Africa--consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J. 2013; 16: 38 DOI: 10.11604/pamj.2013.16.38.3100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009; 27(5): 963–75. DOI: 10.1097/HJH.0b013e3283282f65 [DOI] [PubMed] [Google Scholar]
- 40.Berry KM, Parker WA, Mchiza ZJ, Sewpaul R, Labadarios D, Rosen S, et al. Quantifying unmet need for hypertension care in South Africa through a care cascade: Evidence from the SANHANES, 2011–2012. BMJ Glob Health. 2017; 2(3): e000348 DOI: 10.1136/bmjgh-2017-000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Milman T, Joundi RA, Alotaibi NM, Saposnik G. Clinical inertia in the pharmacological management of hypertension: A systematic review and meta-analysis. Medicine (Baltimore). 2018; 97(25): e11121 DOI: 10.1097/MD.0000000000011121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iloh GU, Ofoedu JN, Njoku PU, Amadi AN, Godswill-Uko EU. Medication adherence and blood pressure control amongst adults with primary hypertension attending a tertiary hospital primary care clinic in Eastern Nigeria. Afr J Prim Health Care Fam Med. 2013; 5(1): 446 DOI: 10.4102/phcfm.v5i1.446 [DOI] [Google Scholar]
- 43.Nyaaba GN, Stronks K, de-Graft AA, Kengne AP, Agyemang C. Tracing Africa’s progress towards implementing the Non-Communicable Diseases Global action plan 2013–2020: A synthesis of WHO country profile reports. BMC Public Health. 2017; 17(1): 297 DOI: 10.1186/s12889-017-4199-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multi-staged Sampling of Subjects and Weighting by Design, Age and Sex.


