Abstract
Background:
Neurosurgical procedures are associated with profound blood loss that necessitates need for intraoperative and postoperative blood transfusion. Excessive ordering of blood based on physicians' habitual practice may lead to unintentional misuse of blood bank services. For the optimal use of blood resources, transfusion practices have to be appropriate.
Aims:
The aim of this study is to study the cross match to transfusion ratio and to review the blood utilization practices (transfusion index and maximal surgical blood order schedule) in elective neurosurgical procedures.
Settings and Design:
A prospective, observational study comprising 740 patients undergoing elective neurosurgical procedures.
Materials and Methods:
Blood requisition forms and patient records were analyzed of patients undergoing elective neurosurgical procedures from December 2017 to December 2018. A review and note was made of the patient's age, sex, and diagnosis. The number of units prepared, cross matched, and transfused were noted.
Statistical Analysis:
Statistical analysis was performed with the IBM SPSS software version 21.0. Blood utilization indices were computed and expressed as percentage.
Results:
A total of 740 patients underwent elective surgical procedures. Among these, 346 patients were requested to prepare 614 units of blood. Out of these 740 patients, there were 56 patients who were in the pediatric age group. A total of 178 units were transfused in 102 patients. One hundred and forty-two units were transfused in the intraoperative period, whereas as 36 units were transfused in the postoperative period.
Conclusion:
There is an efficient usage of blood for patients undergoing surgery for meningiomas, posterior fossa tumors, spinal dysraphism, and craniovertrebral junctional anomalies. However, the blood resources were poorly utilized in patients undergoing surgery for subarachnoid hemorrhage and pituitary tumors. A revision of blood transfusion policy within the hospital is needed.
Keywords: Cross match, neurosurgical patients, transfusion practices
INTRODUCTION
Many neurosurgical procedures are associated with blood loss and the ordering of blood products is a common practice in the neurosurgical operating room. As blood components are rare resource, transfusion services need to be monitored.[1] Different types of neurosurgical procedures may have different transfusion requirements depending on the surgical procedure to be performed and the physiological status of the patient. The use of blood products has declined over the past two decades due to the improvement in the surgical skills and better technological advancement. However, at many centers, the conventional practice of unnecessary blood requisitions continues. Any blood bag which is ordered by the operating room physicians becomes unavailable for other patients who require transfusion.[2] An optimal Maximal Surgical Blood Order Schedule (MSBOS) for elective neurosurgical procedures may cause a marked decrease in workload and financial expenditure.[3,4] A cross-match to transfusion ratio (CTR) of >2.5 may be prevalent in many neurosurgical operating rooms, indicating that an excessive cross-matching of blood is being ordered for by the physicians.[5] As the probability of transfusion for a given surgical procedure (%T) of 30% or more is considered as appropriate,[6,7] a review of the surgical blood ordering in neuroanesthesia practice is mandatory to optimize the blood-ordering schedules in neuroanesthesia practice.
The primary aim of this study was to study the CTR in patients undergoing neurosurgical procedures. The secondary aim of the study was to review the blood utilization practices (transfusion index and MSBOS) in elective neurosurgical procedures. Our hypothesis was that there is a practice of excessive ordering of blood products in our institute in patient's undergoing neurosurgical procedures. This study was planned to help in the formulation of a rationale blood-ordering practice in neuroanesthesia practice, based on the outcome of the study.
MATERIALS AND METHODS
This study was conducted in the department of neurosurgery and division of neuroanesthesia of a tertiary care hospital in Northern India. This prospective, observational, cross-sectional study was conducted in all those patients who underwent elective neurosurgical procedures from December 2017 to December 2018. The study was conducted according to the declaration of Helsinki after taking consent from all patients whose data were collected.
A time period from December 2017 to December 2018 was selected to conduct the study. During this period, a total of 740 patients underwent elective surgical procedures were enrolled. All patients scheduled for elective neurosurgical procedures were planned for the blood ordering schedule and cross matching by the operating surgeon. The patients were reviewed by the attending anesthesiologists (ZA) 1 day before surgery where the general condition of the patient including the blood ordering schedule was assessed. The surgical team was asked to arrange the additional units of blood, if need was felt for the same on the preanesthetic visit. Intraoperatively and postoperatively, the need for transfusion was assessed by the attending anesthesiologist on the basis of a combination of factors including the estimation of intraoperative blood loss associated with changes in hemodynamic parameters as tachycardia, hypotension, and transfusion trigger. The transfusion trigger was calculated on the basis on maximum allowable blood loss (MABL) which was calculated using the following formula:
MABL = ABL= (EBV × [Hi-Hf])/Hi
where:
EBV = Estimated blood volume
Hi = Initial hemoglobin
Hf = Final hemoglobin
MABL = EBV After the completion of the surgical procedure, the patient's records were collected and analyzed by the nonattending anesthesiologist (TK) on the next postoperative day. A review and note were made of the patient's age, sex, and diagnosis. In addition the number of units prepared, cross matched, and transfused were noted. Data was entered and analyzed using the SPSS Version 16.0 (SPSS Inc., Chicago, Illinois, USA) software. Blood utilization indices were computed with the following equations:
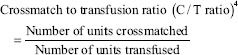
A ratio of 2.5 and below indicates the significant blood usage with minimal loss of the resources.
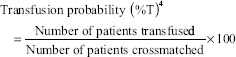
A value of 30% and above signifies a significant blood usage.
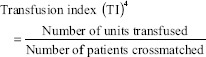
A value of 0.5 or more indicates significant blood utilization.
Maximal Surgical Blood Order Schedule (MSBOS)4 = 1.5 × TI
In our study, blood was considered to be not utilized when the blood prepared for the patient was not used in the intraoperative or immediate postoperative (till discharge from the hospital) period.
Statistical analysis
The sample size was calculated on the basis of the following formula  where n is the sample size, Z is the statistic corresponding to level of confidence, P is expected prevalence, and d is precision (corresponding to effect size). Based on the study conducted by Hall et al.[8] with a red cell transfusion usage at 46.9%, a confidence interval (∞) of 95% (z = 1.96) with a margin of error (d) at 0.05, a sample size of 383 was required.
where n is the sample size, Z is the statistic corresponding to level of confidence, P is expected prevalence, and d is precision (corresponding to effect size). Based on the study conducted by Hall et al.[8] with a red cell transfusion usage at 46.9%, a confidence interval (∞) of 95% (z = 1.96) with a margin of error (d) at 0.05, a sample size of 383 was required.
RESULTS
During the study period, a total of 740 patients underwent elective surgical procedures. Out of these 740 patients, there were 56 patients who were in the pediatric age group with age <12 years, whereas as 684 were having an age >12 years. Among these 346 patients (56.35%) were requested to prepare 614 units of blood [Table 1]. Patients being operated for ventriculoperitoneal shunts, sterotactic biopsy, laminectomy and discectomy and chronic subdural hematoma were not made to prepare any units of blood. Blood grouping and cross matching were only done for these patients. The average age of the patients was 35.7 ± 13.1 years, with a maximum age of 83 years and a minimum age of 5 days. Out of the study population, there were 537 males (72.56%) who underwent surgery under general anesthesia. The blood was prepared during the admission of the patient in the neurosurgery ward in the preoperative period. Depending upon the nature of surgery, requisite amount of blood was prepared ranging from 1 unit to 3 units. A total of 178 units were transfused (out of 614 units of blood prepared) in 102 patients. One hundred and forty-two units were transfused in the intraoperative period, whereas as 36 units were transfused in the postoperative period during their stay in neurosurgical intensive care unit.
Table 1.
Patient characteristics
| Patient characteristic | Number |
|---|---|
| Total number of patients | 740 |
| Pediatric patients | 56 |
| Adult patients | 684 |
| Gender | |
| Males | 537 |
| Females | 203 |
| Patients requested to prepare blood | 346 |
| Total units of blood prepared | 614 |
| Total amount of blood transfused | 178 |
| Total number of patients transfused | 102 |
| Total amount of blood transfused intra-operatively | 142 |
| Total amount of blood transfused postoperatively | 36 |
Among the study population, it was observed that the intracranial tumors were operated most frequently (n = 215) at our center. Preoperatively, blood products were ordered for meningiomas, cerebellopontine angle tumors, high-grade glioma (glioblastomamuliforme), and gliomas. It was observed that astrocytoma or oligodendroglioma, pituitary tumors stereotactic biopsies of intracranial tumors were infrequently associated with blood transfusion and resulted in a higher wastage of blood products while as meningiomas, cerebellopontine angle tumors, and glioblastomamultiforme were associated with the increased rates of blood transfusion [Table 2]. The CTR for pituitary tumors was high (10.12), whereas for meningiomas and posterior fossa tumors, it was low (1.93 and 1.71 respectively). Sub arachnoid hemorrhage patients scheduled for craniotomy and clipping of the aneurysmal vessel were prepared for preoperative ordering of blood but were associated with improper (a high CTR of 14.28) utilization. Patients undergoing clipping for aneurysmal subarachnoid hemorrhages rarely received transfusion in the intraoperative period or postoperative period [Table 3].
Table 2.
Characteristics of the surgical population and the blood prepared
| Nature of surgical procedure | Number of patients | Number of blood units prepared | Number of patients transfused | Number of blood units transfused |
|---|---|---|---|---|
| Intracranial tumors | 215 | 432 | 79 | 138 |
| Pituitary tumors | 81 | 162 | 10 | 16 |
| Posterior fossa tumors and cerebellopontine angle tumors | 30 | 60 | 20 | 35 |
| Meningiomas | 42 | 112 | 32 | 58 |
| Supratentorial tumors | 49 | 98 | 17 | 29 |
| Sterotactic biopsy | 13 | 0 | 0 | 0 |
| Subarachnoid hemorrhage | 62 | 100 | 3 | 7 |
| Laminectomy and discectomy | 335 | 0 | 2 | 3 |
| Craniovertebral junction anomaly and Arnold Chiari malformation | 6 | 6 | 2 | 3 |
| Compression fracture of spine (dorsal and lumbar spine) | 23 | 23 | 2 | 5 |
| Chronic SDH | 20 | 0 | 0 | 0 |
| Spinal cord tumors | 27 | 27 | 3 | 5 |
| Spinal dysraphism | 26 | 26 (100 ml units) | 11 | 17 |
| Ventriculoperitoneal shunt | 26 | 0 | 0 | 0 |
| Total | 740 | 614 | 102 | 178 |
SDH=Subdural hematoma
Table 3.
Usage of blood
| Nature of surgical procedure | Units cross matched (number of units prepared) | Units transfused | CT ratio | Transfusion probability (%) | TI | MSBOS |
|---|---|---|---|---|---|---|
| Intracranial tumours | 432 | 138 | 3.1 | 18.28 | 0.31 | 0.46 |
| Pituitary tumours | 162 | 16 | 10.12 | 6.17 | 0.09 | 0.13 |
| Posterior fossa tumours and cerebellopontine angle tumours | 60 | 35 | 1.71 | 33.33 | 0.58 | 0.87 |
| Meningiomas | 112 | 58 | 1.93 | 28.57 | 0.51 | 0.76 |
| Supratentorial tumours | 98 | 29 | 3.37 | 17.34 | 0.29 | 0.43 |
| Sterotactic biopsy | 0 | 0 | - | - | - | - |
| Subarachnoid hemorrage | 100 | 7 | 14.28 | 3.00 | 0.07 | 0.10 |
| Ventriculperitoneal shunts | 0 | 0 | - | - | - | - |
| Laminectomy and discectomy | 0 | 3 | - | - | - | - |
| Chronic SDH | 0 | 0 | -- | - | - | - |
| Spinal cord tumours | 27 | 5 | 5.4 | 11.11 | 0.18 | 0.27 |
| Spinal dysraphism | 26 | 17 | 1.52 | 42.70 | 0.65 | 0.97 |
| Craniovertebral junction anomaly and Arnold chirai malformation | 6 | 3 | 2 | 33.33 | 0.5 | 0.75 |
| Compression fracture of spine (dorsal and lumbar spine) | 23 | 5 | 4.6 | 8.69 | 0.21 | 0.31 |
| Total | 614 | 178 | 3.44 | 16.61 | 0.28 | 0.42 |
CT=Cross match to transfusion, TI=Transfusion index, MSBOS=Maximal surgical blood order schedule
Patients undergoing surgery for the compression fracture (at thoracic and lumbar level) were made to prepare for blood products. They received blood products in the intraoperative period were associated with proper utilization (CTR of 4.6) of blood products. Patients undergoing surgery for laminectomies and dissectomies at lumbar and cervical levels were not made to undergo the preparation of blood products in the preoperative period. Furthermore, these patients were not in need for transfusion requirement in the intraoperative period. Unfortunately, three patients (whose blood products were not prepared in the preoperative period) who underwent surgery for laminectomy and discectomy were in need of blood transfusion due to chronic anemia and blood loss in the intraoperative period.
Patients undergoing pediatric neurosurgical procedures as craniostenosis, repair of encephocele, and meningomyelocele also underwent preoperative ordering of blood. However, the blood products were invariably used in the pediatric population as many of these patients were anemic and had significant blood loss intraoperatively. This group of patients was associated with better utilization of blood products with a CTR of 1.52 in patients undergoing surgery for spinal dysraphism.
DISCUSSION
Transfusion of blood and blood products is a very common practice in neurosurgical practice. In neurosurgical procedures associated with profound blood loss, transfusion of blood products helps in optimization of the physiological variables of the patient. The primary aim of our study was to see the CTR in patients undergoing various neurosurgical procedures. Among the cranial surgical procedures, it was observed that an optimal CTR of (<2.5) and an optimal transfusion index (>0.5) was observed in patients undergoing surgery for posterior fossa tumors, cerebellopontine angle tumors, meningiomas while as in patients undergoing surgery for pituitary tumors, supratentorial tumors, subarachnoid hemorrhage, craniovertebral junction anomaly, arnold chiari malformation there was a practice of over ordering of blood products in our institute. Among the patients undergoing spinal surgical procedures, an over ordering and underutilization was seen in craniovertebral junction anomaly, Arnold Chiari malformation, spinal cord tumors, and compression fracture of spine.
An attempt to study the utilization of the blood products may be helpful in reducing the wastage of the blood resources with a reduction in the cost. Over-ordering of blood is common in the clinical practice. Friedman et al. in 1976 found that that the range of utilization was 5%–40%.[9] Later studies from Saudi Arabia showed that only 30% of crossmatched blood was used in the elective surgery.[10] Underutilized figures of blood utilization were reported from Ethiopia, (43.8%),[11] North India (41%),[12] and Kuwait (13.6%).[13] Ambroise et al.[14] reported a decline in the usage of whole blood and an increase in the use of fresh-frozen plasma (FFP) and platelets over the years. Packed red blood cells were mainly used for treating injury and poisoning conditions, platelets and FFP were preferred for infectious and parasitic diseases. Similarly, reports from India[15] and Egypt[16] showed effective utilization of the blood products. Our study showed similar results with a high utilization ratio.
Previous studies have attempted to define the blood utilization parameters in a heterogeneous surgical population. Our study is the probably the first study that has focused to evaluate the blood utilization parameters in a homogenous population consisting of neurosurgical patients. Patients undergoing surgery for intracranial procedures, tumors had a blood utilization ratio of 74%. This was more in patients with meningioma and glioblastoma multiform. The patients with small cortical tumors such as low-grade frontal gliomas rarely required transfusion. This subgroup of patients in the intracranial tumors had a low utilization ratio. Hence, we feel cross matching may be only required in this group of patients while as procurement of blood can only be ordered if the need arises. Similarly, with an improvement in surgical skills, intraoperative rupture of the aneurysm is rarely encountered. The incidence of transfusion has markedly decreased in patients with subarachnoid hemorrhage. Unfortunately, we still continue to order cross matching of blood for the patients. A better practice would be to decide about the transfusion based on the anatomy of the aneurysm on the basis of computerized angiography or digital subtraction angiography. An aneurysm with an accessible anatomy may not need transfusion while as a difficult to access aneurysm (at risk of intraoperative rupture) may be in need of preparation for blood transfusion.[17] Similarly, patients undergoing surgery for ventriculoperitoneal shunts and cranioplasties had no blood arranged in the preoperative period. Although none of the adult patients undergoing ventriuloperitoneal shunts were in need of blood transfusion, two patients undergoing cranioplasties had a requirement for blood transfusion products.
Patients undergoing spinal surgical procedures for laminectomies and discectomies did not undergo any ordering of the blood for surgical procedure. However, two of these patients received blood transfusion for which the blood was ordered in the intraoperative period.
A common strategy to evaluate the blood utilization in an institution is the determination of the CTR. This concept was put forward by Boral and Henry in 1975.[18] This ratio is normally taken as 1. A ratio of <2.5 is an indicator of effective blood utilization. In our study, overall CTR was 3.44. It was the best for patients with spinal dysraphism with a CTR of 1.52 followed by posterior fossa tumors (1.71) and meningiomas (1.93). There was a lot of blood wastage in patients with subarachnoid hemorrhage (CTR 14.28 and pituitary tumors 10.12). Although overall CTR in our study was higher than the reported from the UK (2.1),[8] United States of America (2.36),[19] and Nigeria (2.2);[2] however, the subgroup analysis revealed that there was a proper utilization of blood products in patients with spinal dysraphism, meningiomas, and posterior fossa tumors.
The transfusion probability (%T) is an indicator of appropriate transfusion practices and a value of >30 are indicative of appropriate transfusion. The overall %T in our study was 16.61% which indicates an inappropriate utilization of blood products. This low value was due to varied utilization data from different subsets of neurosurgical population. If we evaluate the subsets of our study population, patients with spinal dysraphism (42.70%) had the highest probability of need for blood transfusion followed by posterior fossa tumors (33.33%), craniovertebral junction anomalies (33.33%), and meningiomas (28.57%). It was observed from our patient population that patients with subarachnoid hemorrhage (3.00%) and pituitary tumors (6.17%) had a low transfusion probability. The transfusion probability in spinal dysraphism, posterior fossa tumors, craniovertebral junction anomalies, and meningiomas are similar to the transfusion probabilities in nonsurgical populations published by Belayneh et al.[11] and Bhutia et al.[20] In our study, significant blood usage with a transfusion index of >0.5 was seen in spinal dysraphism, posterior fossa tumors, and craniovertebral junction anomalies. Similarly, the minimum blood ordering schedule was the highest for spinal dysraphism followed by posterior fossa tumors, meningiomas, and craniovertebral junction anomaly.
The main limitation of our study was that it was a single-centered study. The findings may be different in other institutes depending on the prevalent institutional practices. One of the anesthesiologists who were involved in data collection and patient management was aware of the study being done which may have added to the bias. The experience of the surgeon may have influenced the decision of blood ordering, as a novice neurosurgeon may like to arrange more blood.
A multicenter study aimed at comparing the transfusion practices across multiple centers in India may be helpful in comparing the transfusion practices in these institutes. This could help in the formulation of protocols for blood ordering in neurosurgical procedures and minimize the wastage of blood products ensuring their optimal utilization.
CONCLUSION
It was observed from our study, that there is an efficient usage of blood for patients undergoing surgery for meningiomas, posterior fossa tumors, spinal dysraphism, and craniovertebral junctional anomalies. The blood resources were poorly utilized in patients undergoing surgery for subarachnoid hemorrhage and pituitary tumors. We recommend preparing of blood points in the preoperative period for patients undergoing surgery for meningiomas, posterior fossa surgeries, and pediatric neurosurgery while as in patients undergoing surgery for pituitary tumors, laminectomies and stereotactic biopsies grouping and cross matching should be done. While implementing these criteria, we must also keep in consideration the surgeons skills, the preoperative hemoglobin levels and the comorbidities of the patient. A revision of blood transfusion policy within the hospital needs to be made to reduce the wastage of the resources.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Grey DE, Finlayson J. Red cell transfusion for iron-deficiency anaemia: A retrospective audit at a tertiary hospital. Vox Sang. 2008;94:138–42. doi: 10.1111/j.1423-0410.2007.01010.x. [DOI] [PubMed] [Google Scholar]
- 2.Subramanian A, Sagar S, Kumar S, Agrawal D, Albert V, Misra MC. Maximum surgical blood ordering schedule in a tertiary trauma center in Northern India: A proposal. J Emerg Trauma Shock. 2012;5:321–7. doi: 10.4103/0974-2700.102391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin JS, Chen YJ, Tzeng CH, Lyou JY, Lee CH. Revisiting of preoperative blood ordering policy – A single institute's experience in Taiwan. J Chin Med Assoc. 2006;69:507–11. doi: 10.1016/S1726-4901(09)70319-3. [DOI] [PubMed] [Google Scholar]
- 4.Friedman BA. An analysis of surgical blood use in United States hospitals with application to the maximum surgical blood order schedule. Transfusion. 1979;19:268–78. doi: 10.1046/j.1537-2995.1979.19379204208.x. [DOI] [PubMed] [Google Scholar]
- 5.Thabah R, Sailo LT, Bardoloi J, Lanleila M, Lyngdoh NM, Yunus M, et al. Maximum surgical blood order schedule' in a newly set-up tertiary care hospital. Anaesth Pain Intensive Care. 2013;17:28–32. [Google Scholar]
- 6.Mead JH, Anthony CD, Sattler M. Hemotherapy in elective surgery: An incidence report, review of the literature, and alternatives for guideline appraisal. Am J Clin Pathol. 1980;74:223–7. doi: 10.1093/ajcp/74.2.223. [DOI] [PubMed] [Google Scholar]
- 7.Iyer SS, Shah J. Red blood cell transfusion strategies and maximum surgical blood ordering schedule. Indian J Anaesth. 2014;58:581–9. doi: 10.4103/0019-5049.144660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall TC, Pattenden C, Hollobone C, Pollard C, Dennison AR. Blood transfusion policies in elective general surgery: how to optimise cross-match-to-transfusion ratios. Transfus Med Hemother. 2013;40:27–31. doi: 10.1159/000345660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman BA, Oberman HA, Chadwick AR, Kingdon KI. The maximum surgical blood order schedule and surgical blood use in the United States. Transfusion. 1976;16:380–7. doi: 10.1046/j.1537-2995.1976.16476247063.x. [DOI] [PubMed] [Google Scholar]
- 10.Sowayan SA. Use of blood in elective surgery: An area of wasted hospital resource. Ann Saudi Med. 1994;14:326–8. doi: 10.5144/0256-4947.1994.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Belayneh T, Messele G, Abdissa Z, Tegene B. Blood requisition and utilization practice in surgical patients at university of Gondar hospital, Northwest Ethiopia. J Blood Transfus. 2013;2013:1–5. doi: 10.1155/2013/758910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subramanian A, Rangarajan K, Kumar S, Sharma V, Farooque K, Misra MC. Reviewing the blood ordering schedule for elective orthopedic surgeries at a level one trauma care center. J Emerg Trauma Shock. 2010;3:225–30. doi: 10.4103/0974-2700.66521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basnet RB, Lamichhane D, Sharma VK. A study of blood requisition and transfusion practice in surgery at Bir Hospital. Postgrad Med J NAMS. 2009;9:14–9. [Google Scholar]
- 14.Ambroise MM, Ravichandran K, Ramdas A, Sekhar G. A study of blood utilization in a tertiary care hospital in South India. J Nat Sci Biol Med. 2015;6:106–10. doi: 10.4103/0976-9668.149101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vibhute M, Kamath SK, Shetty A. Blood utilisation in elective general surgery cases: Requirements, ordering and transfusion practices. J Postgrad Med. 2000;46:13–7. [PubMed] [Google Scholar]
- 16.Ibrahim SZ, Mamdouh HM, Ramadan AM. Blood utilization for elective surgeries at main University Hospital in Alexandria, Egypt. J Am Sci. 2011;7:683–9. [Google Scholar]
- 17.Chowdhury T, Cappellani RB, Sandu N, Schaller B, Daya J. Perioperative variables contributing to the rupture of intracranial aneurysm: An update. Scientific World J. 2013;2013:1–7. doi: 10.1155/2013/396404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boral LI, Henry JB. The type and screen: A safe alternative and supplement in selected surgical procedures. Transfusion. 1977;17:163–8. doi: 10.1046/j.1537-2995.1977.17277151923.x. [DOI] [PubMed] [Google Scholar]
- 19.Alghamdi S, Gonzalez B, Howard L, Zeichner S, LaPietra A, Rosen G, et al. Reducing blood utilization by implementation of a type-and-screen transfusion policy a single-institution experience. Am J Clin Pathol. 2014;141:892–5. doi: 10.1309/AJCPX69VENSKOTYW. [DOI] [PubMed] [Google Scholar]
- 20.Bhutia SG, Srinivasan K, Ananthakrishnan N, Jayanthi S, Ravishankar M. Blood utilization in elective surgery-requirements, ordering and transfusion practices. Natl Med J India. 1997;10:164–8. [PubMed] [Google Scholar]


