Abstract
Purpose
COVID-19 pandemic is a World Health Organization day-to-day work and has a significant crisis on the physical and mental health of humans. However, little is known about the mental health crisis of the pandemic in Sub-Saharan countries. Therefore, this study aimed to determine the magnitude of psychological problems and associated factors among communities living in Addis Ababa, Ethiopia.
Methods
A community-based cross-sectional study design was conducted from March 10 to 30, 2020. Data were collected from 420 respondents selected using a consecutive sampling technique. An online self-administered and Depression, Anxiety, and Stress Scale (DASS-21) survey during the initial phase of the pandemic was conducted to assess the presence of psychological problems for the last two weeks in response to the infection.
Results
The magnitude of the psychological problem from moderate to severe levels was 66.4%. The predictor variables of the outcome were female gender, above the secondary level of education, monthly income below 3000 ETB, and more than three family size at 95% CI, P<0.05.
Conclusion
At the time of the initial COVID-19 pandemic in Ethiopia, nearly two-thirds of the respondents reported moderate to severe levels of psychological problems. Therefore, working on those identified factors would be vital to promote the mental resilience of a community towards the pandemic.
Keywords: anxiety, depression, stress, coronavirus, psychological problem
Introduction
The 2019 coronavirus disease (COVID-19) pandemic has first occurred in Wuhan city of China.1 It has a wide coverage and death report as compared to the 2012 first Middle East respiratory syndrome (MERS) outbreak in Saudi Arabia.2 The distribution of the virus at a global level is about 6,175,207 cases (224,172 deaths), in Africa 74,663 cases (973 deaths), and Ethiopia 2336 cases (32 deaths).3 The pandemic is the global public health emergency due to its rapid transmission, the increment of the confirmed case, and death.4 It is highly contagious and transmits to humans through respiratory droplets, human body contact, surface contact, and symptoms were fever, cough, fatigue, breathing difficulty.5
The incubation period of the virus was from 2 to 11 days, and this helps for a quarantine period of duration for suspected cases.6 Individuals with other chronic medical conditions or age greater than 65 years were highly vulnerable to be infected and showed poor treatment outcome.7
The prevention strategies of the virus were to limit physical contact to the extent of home lockdown, avoid public meetings, minimize the number of passengers during transportation, and talk with keeping one-meter social distance, use of a facemask, and frequent hand washing with soaps and water.8
The most common mental and psychosocial disturbances seen during the previous outbreaks occurred in a different part of the world were hopelessness, anger, loss of interest, fear of death, the difficulty of initiating and maintaining sleep, loss of appetite, and anxiety.9–11 The current pandemic causes suicide, stress, confusion, anger, fear, frustration, boredom, financial loss, and stigma among confirmed cases and communities living in the world.12
During this pandemic period, having mental and psychological problems leads to poor self-hygiene, appetite, sleep, immunity status, and commitment to obey commands recommended by health professionals that all enhance the susceptibility for infection.13,14
After the occurrence of the pandemic, in Italy, 38%,15 china 53.8%,16 Australia 78%,17 France 38.6%18 and India 25.3%19 of the respondents were developed mild to moderate psychological distress including anxiety, stress and depression.
The contributing factors for experiencing mental and psychological problems in response to the pandemic were female gender, older age, medical comorbidity, poor social support, more family size, low-income status, and educational level.15–18
To manage the mental health impacts of the pandemic, scholar recommends to limit the sources of stress, break the isolation with online communication media, regular sleep, and diet patterns, focus on the benefit of separation, ask professional for outpatient and inpatient mental health service.20,21 The mental health impact of this pandemic in developing countries might be significant due to limited resources, unintegrated health-care systems, and a lack of skilled health-care providers. Despite this fact, there are no adequate studies conducted in this regard. Therefore, this study aimed to determine the magnitude of psychological problems in response to the pandemic and its associated factor among communities living in Addis Ababa, the Capital city of Ethiopia. The results of this study will serve to generate appropriate mental health crisis management guidelines for the promotion of the psychosocial wellbeing of a community in response to the pandemic.
Methods
Study Design, Setting and Period
This study was a community-based cross-sectional study design conducted from March 10–30 at Addis Ababa, Capital city of Ethiopia, and the first Ethiopian city in which COVID-19 confirmed cases reported. Currently, six million peoples were living in the city.
Study Participants
The source of the population for this study was all social media users (Facebook and telegram) living in the town, Addis Ababa, and all users during the study period were study populations. The exclusion criteria of the study were all users less than 18 years of age.
Sample Size and Sampling Technique
The sample size was calculated using the single proportion formula by considering p value of the previous study done in china on the same pandemic 53.8%.16 The single proportion formula of cross-sectional study design (n = required sample size n= Z (α/2) 2 pq/d2) was used.
To calculate final sample size, P= 0.54, q (1-p) = 0.46, 95% CI and 5% margin of error was used.
n = required sample size n= Z (α/2) 2 pp./d2, p= 0.54
= (1.96) (1.96) (0.54) (0.46)/(0.05) (0.05) = 382
N = non-response rate 10% =38, the total sample size was, 382+ 38 = 420
The sampling technique was consecutive sampling.
Data Collection Procedures and Instruments
Two-master’s level of mental health and computer science professionals were involved in data collection using online self-administered questioner. After the preparation of the online data formats of the questioner, then sent to each respondent telegram and Facebook inbox messages, and they sent back to us as a reply after filling the questioner. The first part of the questioner was about the socio-demographic characteristics of the study participants. The second part of the questioner was Depression, Anxiety, and Stress Scale (DASS-21) used to determine the current mental health status of respondents in response to the COVID-19 pandemic. It has 21 items scored (0–3) and three subscales (anxiety, depression, and stress). The question item 21, 17, 16, 13, 10, 5, and 3 were items of the depression subscale. The score of depression subscale was Normal (0–9), Mild depression (10–12), Moderate depression (13–20), severe depression (21–27), and Extremely severe depression (28–42). Questions item 20, 19, 15, 9, 7, 4, and 2 were items of the anxiety subscale. The score of anxiety subscale was Normal (0–6), Mild (7–9), Moderate (10–14), Severe (15–19), and extremely severe (20–42). Questions items 18, 14, 12, 11, 8, 6, and 1 were items of the stress subscale. The score of stress subscale was Normal (0–10), Mild stress (11–18), Moderate stress (19–26), severe stress (27–34), and Extremely severe stress (35–42).22,23
The third part of the questioner was the current knowledge, attitude, and awareness (KAP) about the coronavirus (COVID-19). It has 20 items adopted from the world health organization.24
Data Quality Control
The English version of the questioner first translated into Amharic, the official language of the study area, and then back-translated to English to check the consistency of the English version questioner. The data collectors used the Amharic version of the questioner for data collection.
The investigator conducted a pretest among 21 respondents before one week of the actual data collection. The researcher trained both the data collectors and supervisors for about four days about the purpose of the study. The supervisors checked all the data collectors at an online survey cite about the completeness of the questioner and discarded the incomplete before data entry.
Statistical Analysis
The data coded, entered, and checked on Epi-Data Version 3.4 and exported to SPSS (Statistical Package for Social Science) version 24 for analysis. A Bivariate logistic regression analysis at a p-value of ≤0.25 used to identify the association of each independent variable with the outcome variables. Bivariate logistic regression at p-value ≤0.25, used to identify variables candidate for multiple logistic regression analysis. Multivariable logistic regression analysis at p-value ≤0.05, used to control the possible effect of confounders and identify independent predictors of the outcome variable. Hosmer and Lemeshow goodness of fit test was used to check the model fitness.
Result
Socio-Demographic Characteristics
One-third of the respondents have a single marital status, and nearly two-thirds of the respondents have more than a secondary level of education. The mean age onset and monthly income of the respondents were 27 years and 3000 ETB, respectively (Table 1).
Table 1.
Socio-Demographic Characteristics of Respondents Who Use Facebook and Telegram and Living in Addis Ababa, Ethiopia 2020 (N = 420)
| Variables | Category | Frequency(n=420) | Percentage (%) |
|---|---|---|---|
| Sex | Male | 189 | 45 |
| Female | 231 | 55 | |
| Marital status | Single | 186 | 44.2 |
| Married | 90 | 21.4 | |
| Divorced | 84 | 20 | |
| Widowed | 60 | 14.2 | |
| Educational status | Primary | 44 | 10.4 |
| Secondary | 120 | 28.5 | |
| More-than secondary | 256 | 60.9 | |
| Occupation | Unemployed | 96 | 22.8 |
| Housewife | 60 | 14.2 | |
| Student | 95 | 22.62 | |
| Private work | 89 | 21.1 | |
| Government employee | 80 | 19.0 | |
| Family size | One | 113 | 26.9 |
| Two | 105 | 25 | |
| Three and above | 202 | 48 |
Knowledge, Attitude, and Practice About Coronavirus
All respondents heard about the coronavirus, and their source of information was Facebook, TV, radio, Telegram, families, and friends. Nearly two-thirds of respondents were thinking, as coronavirus is very dangerous. One-third of the respondents reported as they used preventive measures such as washing their hands, wearing a facemask, and keeping a social distance (Table 2).
Table 2.
Knowledge, Attitude and Practice Response of Respondents About Corona Virus Who Were Using Facebook and Telegram and Living in Addis Ababa (N=420)
| Question Item | Frequency | Percent |
|---|---|---|
| Have you ever heard about the new coronavirus disease? (COVID-19) | ||
| Yes | 420 | 100 |
| No | 0 | 0 |
| What do you know about the new coronavirus disease? | ||
| I do not know anything | 25 | 5.9 |
| It’s a virus that can cause a disease | 341 | 81.1 |
| It’s a government’s programme | 39 | 9.2 |
| It’s a TV/radio campaign | 15 | 3.5 |
| What kind of information have you received about the disease? | ||
| How to protect yourself from the disease? | 32 | 7.6 |
| Symptoms of the new coronavirus disease | 56 | 13.3 |
| How it is transmitted | 58 | 13.8 |
| What to do if you have the symptoms | 47 | 11.1 |
| Risks and complications | 30 | 7.1 |
| Both protection and transmission | 180 | 42.8 |
| All of the information above | 17 | 4 |
| Where did you hear about the new coronavirus from? What channels or sources? |
||
| Facebook only | 45 | 10.7 |
| Telegram only | 15 | 3.5 |
| From Radio, Television, health workers, Telegram, Facebook and friend or family members information channel | 380 | 90.4 |
| Which channels/who do you trust the most to receive information related to coronavirus? (one or more options) | ||
| Government Facebook, telegram television, Radio | 43 | 10.2 |
| Private Facebook and telegram page | 36 | 8.5 |
| Community Health professional | 15 | 3.5 |
| Family members and friends | 30 | 7.1 |
| Both of government social media network and community health professionals | 286 | 68 |
| All of the above | 10 | 2.3 |
| How dangerous do you think the new coronavirus risk is? | ||
| Very dangerous | 270 | 64.2 |
| More or less dangerous | 134 | 31.9 |
| Is not dangerous | 16 | 3.8 |
| Who do you think is at highest risk to get the coronavirus? | ||
| Children under 5 years old | 52 | 12.3 |
| Adolescents up to 15 years old | 45 | 12.8 |
| Youth | 25 | 5.9 |
| Adults | 30 | 7.1 |
| Elderly persons | 90 | 21.4 |
| Pregnant women | 12 | 2.8 |
| Both under 5 years old and elders | 150 | 35.7 |
| All of them equally | 16 | 3.8 |
| Do you think you are likely to become sick with the new coronavirus? | ||
| Yes | 52 | 12.3 |
| No | 56 | 13.3 |
| Don´t know | 312 | 74.2 |
| How does the coronavirus spread? | ||
| Blood transfusion | 12 | 2.8 |
| Droplets from infected people | 41 | 9.7 |
| Airborne | 50 | 11.9 |
| Direct contact with infected people. | 60 | 14.2 |
| Touching contaminated objects/surfaces | 67 | 15.9 |
| Sexual intercourse contact | 4 | 0.9 |
| Contact with contaminated animals | 6 | 1.4 |
| Mosquito bites | 0 | |
| Eating contaminated food | 7 | 1.6 |
| Drinking unclean water | 11 | 2.6 |
| Do not know | 3 | 0.7 |
| From direct contact from infected people droplet, air borne, and contaminated objects/surface | 145 | 34.5 |
| From all of the above | 14 | 3.3 |
| What are the main symptoms? | ||
| Fever | 45 | 10.7 |
| Cough | 78 | 18.5 |
| Shortness of breath and breathing difficulties | 34 | 8 |
| Muscle pain | 52 | 12.3 |
| Headache | 31 | 7.3 |
| Diarrhea | 21 | 5 |
| Do not know | 6 | 1.4 |
| No symptoms | 10 | 2.3 |
| Fever, cough, shortness of breath, muscle pain, headache and diarrhea | 143 | 34 |
| Do you know how to prevent it? (One or more options) | ||
| Sleep under the mosquito net | 3 | 0.7 |
| Wash your hands regularly using alcohol or soap and water | 75 | 17.8 |
| Drink only treated water | 36 | 8.5 |
| Cover your mouth and nose when coughing or sneezing | 45 | 10.7 |
| Avoid close contact with anyone who has a fever and cough | 59 | 14 |
| Eliminate standing water | 12 | 2.8 |
| Cook meat and eggs well | 16 | 3.8 |
| Avoid unprotected direct contact with live animals and surfaces in contact with animals | 5 | 1.1 |
| Do not know | 7 | 1.6 |
| All of this including washes your hands regularly using alcohol or soap and water, cover your mouth and nose when coughing or sneezing and Avoid close contact with anyone who has a fever and cough | 162 | 38.5 |
| What have you and your family done to prevent becoming sick with coronavirus in the recent days? | ||
| Washing hands regularly using alcohol-based cleaner or soap/water | 123 | 29.2 |
| Covering mouth and nose when coughing or sneezing | 54 | 12.8 |
| Avoid close contact with anyone who has a fever and cough | 47 | 11.1 |
| Eliminate standing water | 5 | 1.1 |
| Cook meat and eggs well | 6 | 1.4 |
| Avoid unprotected direct contact with live animals and surfaces in contact with animals. | 8 | 1.9 |
| Do not know | 9 | 2.1 |
| All above the above | 168 | 40 |
| Do you consider important to take actions to prevent the spread of coronavirus in your community? | ||
| Yes | 412 | 98 |
| No | 0 | 0 |
| Do not know | 8 | 2 |
| What to do if you or someone from your family has symptoms of this disease? | ||
| I will look for a more experienced relative to advise me on what to do | 74 | 17.6 |
| I will go to the hospital/health unit | 120 | 28.5 |
| I will go to the neighborhood nurse | 46 | 10.9 |
| I will buy medicines at the market | 35 | 8.3 |
| I will look for the traditional healer | 134 | 31.9 |
| I would stay in quarantine | 11 | 2.6 |
| What more would you like to know about the disease? | ||
| How to protect yourself from the disease? | 15 | 3.5 |
| Symptoms of the new coronavirus disease | 32 | 7.6 |
| How it is transmitted | 56 | 13.3 |
| What to do if you have the symptoms | 104 | 24.7 |
| Most at risk groups | 53 | 12.6 |
| How to treat it | 93 | 22.1 |
| All of the above | 67 | 15.9 |
| Do you think the coronavirus disease is generating stigma against specific people? To whom? | ||
| Yes | 390 | 92.8 |
| No | 30 | 7.1 |
| If yes) Which group is being dis-criminated in your community because of coronavirus? | ||
| Chinese | 85 | 20.2 |
| Italians | 95 | 22.6 |
| Asian | 56 | 13.3 |
| Americans | 80 | 19 |
| Ethiopians came from abroad | 47 | 11.1 |
| Those who cough due to different reason | 57 | 13.5 |
| For the past 2 weeks do you have either one or more of the following symptoms cough, fever, sore throat, myalgia, dizziness, breathing difficulty and chili’s? | ||
| Yes | 130 | 30.9 |
| No | 290 | 69.1 |
| Past two-week recent contact with persons who came from abroad | ||
| Yes | 353 | 84% |
| No | 67 | 16% |
Prevalence of Psychological Problem
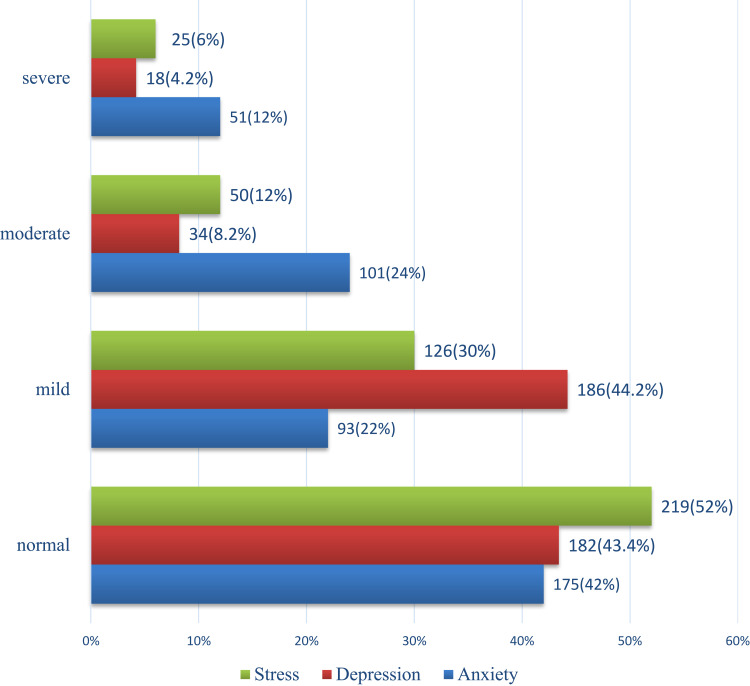
Nearly two-thirds (66.4%) of the respondents had moderate to severe levels of a psychological problem, 36% anxiety, 12.4% depression, and 18% stress (Figure 1).
Figure 1.
The current psychological problem in response to COVID-19 among respondents living in Addis Ababa, Ethiopia (N=420).
Factors Associated with Psychological Problems
During multivariate logistic regression analysis, the independent predictor variables were Gender, educational status, monthly income, family size, contact with the person came abroad, and history of chills and fever at p< 0.05 (Table 3).
Table 3.
Factors Associated with Psychological Problem in Response to COVID-19 Pandemic Among Respondents Living in Addis Ababa, Ethiopia 2020 (N=420)
| Variables | Bivariate Logistic Regression | Multivariable Logistic Regression | ||||
|---|---|---|---|---|---|---|
| Stress | Anxiety | Depression | Stress | Anxiety | Depression | |
| Crude Odds Ratio | Crude Odds Ratio | Crude Odds Ratio | Adjusted Odds Ratio | Adjusted Odd Ratio | Adjusted Odd Ratio | |
| Sex | ||||||
| Male | 1 | 1 | 1 | 1 | 1 | 1 |
| Female | 2.24 P=(0.23) |
1.45 P=(0.12) |
1.75 p=0.05 |
2.56(2.01–3.45) ** | 1.34(1.21–1.95)* | 1.63(1.34–2.45)* |
| Marital status | ||||||
| Single | 1 | 1 | 1 | 1 | 1 | 1 |
| Married | 1.28 P=(0.45) |
2.31 P=0.63 |
3.45 P=0.75 |
|||
| Divorced | 0.841 (P=0.35) |
1.56 P=0.61 |
2.89 P=0.90 |
|||
| Widowed | 5.15 (p=0.67) |
1.67 P=0.59 |
3.14 P=0.78 |
|||
| Separated | 1.38 (P=0.71) |
2.13 P=0.59 |
3.21 P=0.83 |
|||
| Educational status | ||||||
| Primary | 1 | 1 | 1 | 1 | 1 | 1 |
| Secondary level of education | 2.68 P=0.34 |
2.13 P=0.57 |
2.49 P=0.65 |
|||
| More than secondary | 2.90 P=0.05 |
1.72 P=0.05 |
2.21 P=0.02 |
2.73(2.12–3.16)** | 1.69(1.34–2.56)** | 2.23(2.12–2.92)** |
| Occupation | ||||||
| Unemployed | 1 | 1 | 1 | |||
| Housewife | 4.24 P=0.49 |
2.91 P=0.76 |
2.73 P=0.42 |
|||
| Student | 3.56 P=0.71 |
2.99 P=0.54 |
1.23 P=0.94 |
|||
| Private work | 1.67 P=0.59 |
2.73 P=0.39 |
0.232 P=0.51 |
|||
| Government employee | 2.89 P=0.63 |
2.12 P=0.41 |
2.81 P=0.50 |
|||
| Monthly income | ||||||
| ≥3000 ETB | 1 | 1 | 1 | 1 | 1 | |
| Below 3000 ETB | 2.87 P=0.001 |
2.12 P=0.02 |
2.01 P=0.01 |
2.73 (2.23–3.12)** | 2.07(1.93–2.94)** | 1.82(1.72–2.90)** |
| Family size | ||||||
| 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2 | 1.12 P=0.28 |
1.32 P=0.31 |
1.10 P=0.35 |
|||
| ≥ 3 | 1.56 P=0.08 |
1.30 P=0.12 |
1.39 P=0.21 |
1.51(1.32–1.76)* | 1.25(1.21–1.41)* | 1.23(1.13–1.62)** |
| Past two-week History of headache, chills, fever, sore throat and cough | ||||||
| Yes | 4.42 P=0.001 |
3.21 P=0.01 |
2.73 P=0.02 |
4.12(3.21–5.89) ** | 3.05(2.78–3.13)** | 2.45(2.31–3.48)** |
| No | 1 | 1 | 1 | 1 | 1 | 1 |
| Past two-week recent contact with persons who came from abroad | ||||||
| Yes | 2.35 P=0.05 |
3.32 P=0.02 |
2.12 P=0.01 |
2.12(2.10–2.83)** | 2.67(2.13–3.12)** | 1.59 (1.12–1.74)* |
| No | 1 | 1 | 1 | 1 | 1 | 1 |
Notes: Crude odds ratio p ≤ 0.25, were selected for multi variable regression, adjusted odd ratio p ≤ 0.05 selected for independent predictor for the outcome variable. 1.00 remained for reference category, *Significance at p-value <0.05, **Significance at p-value <0.001.
Abbreviations: OR, odds ratio; CI, confidence interval.
Discussion
This study found that 66.4% of the respondents were experienced moderate to severe form psychological problems, including stress, anxiety, and depression in response to COVID-19 pandemic. This result was very high and implicated, as there is a need for immediate mental health crisis intervention.
This study finding was higher than the study done in Italy, 38%,15 china 53.8%,16 Australia 78%,17 France 38.6%,18 and India 25.3%.19 It might be due to the difference in socioeconomic, cultural, and environmental factors such as literacy, norms, attitudes, and resources contribute to coping with the psychological crisis of the pandemic.
This study found that being female gender was the independent predictor for the psychological problem in response to the pandemic. This finding was consistent with other studies done in Italy,15 France,18 and china.16 Naturally, females have a low level of tolerance for stressful situations. In Ethiopia, females have a high responsibility for the health of the family.
The current research found that having more than a secondary level of education had two times more to develop the psychological problem as compared to those who had primary level education. This result was inconsistent with the studies done in Russia25 and China.26 It might be due to a chance to work outside the home through contact with different people and high expectations from the community and government in controlling and preventing the pandemic with limited resources.
This study found that monthly income less than 3000 ETB had two times the odds of having psychological problems. This finding was similar to a study done in Saudi Arabia.27 Among low-income respondents, the socioeconomic impact of a virus might be much significant to the extent of unable to buy safety measures of prevention, such as facemask, soaps, and sanitizers. In-addition during this pandemic period, they were not able to fulfill their basic needs of day-to-day life.
The current study found that having more than three family size at home was associated with psychological problems in response to the pandemic, and this is in agreement with a study done in India.19 The number of family member contribute to contracting the virus due to the high chance of contact with different people.
This study revealed that respondents with the past two weeks of chills, fever, cough, and dizziness over the past two weeks had three times increased the odds of having psychological problems in response to the pandemic. This finding was similar to the study done in China.16 A similar presentation of the current symptoms with coronavirus symptoms leads to misinterpretation of being infected with the virus.
The odds of developing psychological problem among those who had recent contact with peoples who came abroad were two times higher than as compared to those who no history of contact with foreign peoples. This result supported by the studies done in Italy.15 In Ethiopia, the first confirmed case was a man who came from Japan, and thus contacting foreign peoples and came from abroad would result in a high chance of worry about getting the infection.
Limitation of the Study
It was a cross-sectional study design, challenging to conclude regarding causality and alternative explanations of the findings. The data collection method of this study was an online-administered questioner that is prone to information bias.
Conclusions
Most of the respondents (66.4%) had a psychological problem, and the modifiable factors of this study were monthly income below 3000 ETB, current symptoms of chills, fever, cough, and dizziness and having recent contact with people who came from abroad.
Therefore, government and private health sector organizations were highly responsible for preventing and controlling the mental health crisis of the pandemic through transmitting up-to-date and specific information through different social media about the prevention of the virus, what to do if the symptoms occur to themselves, family and community. There should be a continuous supply of precautionary preventive equipment, including facemask, water, soap, alcohol, and sanitizer for those who had more than three family members and low income. The mental health professional should give on-call, outpatient, and inpatient mental health services for clients who developmental and psychological problems in response to the epidemic.
The pandemic task force groups of the country might use these findings to formulate an emergency mental health intervention guideline to promote the psychological resilience of a community in response to the COVID-19 pandemic.
Acknowledgment
The author would like to thank study participants, facilitators, and the peoples living in Addis Ababa Ethiopian Tele Communication Corporation and Dilla University for their cooperation, and made the study possible. The authors have no support or funding to report.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; COVID-19, coronavirus disease 2019; DAAS, Depression, Anxiety and Stress Scale; ETB, Ethiopian birr.
Data Sharing Statement
The datasets analyzed for this study are available from the corresponding author on reasonable request.
Compliance with Ethical Standards
All procedures undertaken during data collection were per the ethical review board of Dilla University and the Helsinki Declaration. The ethical review board of Dilla University approved the study. The data collector discussed with the respondents that participating in this study was voluntary, and if you decide not to participate, there will not be any negative consequences.
The data collector obtained online informed consent from each participant before the data collection.
Disclosure
The author declares no potential conflicts of interest concerning the research, authorship, and publication of this article.
References
- 1.Heymann DL. A novel coronavirus outbreak of global health concern. Lancet Psychiat. 2020;395:15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aleanizy FS, Mohmed N, Alqahtani FY, Ali R, Hadi E. Outbreak of Middle East respiratory syndrome coronavirus in Saudi Arabia: a retrospective study. BMC Infect Dis. 2017;17(23):1–7. doi: 10.1186/s12879-016-2137-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Level R, Level G, High V, High V, High V. Coronavirus disease 2019 (COVID-19). 2020;2019. [Google Scholar]
- 4.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMC Health Serv Res. 2020;408(January):2020. [DOI] [PubMed] [Google Scholar]
- 5.Guo Y, Cao Q, Hong Z, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil Med J. 2020;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019- nCoV) infections among travelers from Wuhan, China. Eur J Infect Dis Surveil Epidemiol Prev Control. 2020;25(5):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. Guidelines for investigation of cases of human infection with Middle East respiratory syndrome coronavirus. World Health. 2013;(July) [Google Scholar]
- 8.Management C, Description T. Novel coronavirus (COVID-19) v1 novel coronavirus (nCoV) v1. World Health Organ. 2020;3–6. [Google Scholar]
- 9.Hall RCW, Hall DM, Chapman MJ. The 1995 Kikwit Ebola outbreak: lessons hospitals and physicians can apply to future viral epidemics. J Ment Health. 2008;30:446–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rubin GJ, Potts HW, Michie S. The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 national telephone surveys in the UK. Health Technol Assess (Rockv). 2010;14(34):183–266. doi: 10.3310/hta14340-03 [DOI] [PubMed] [Google Scholar]
- 11.Sim K, Huak Y, Nah P, Choon H, Wen S. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res. 2020;68(January):195–202. doi: 10.1016/j.jpsychores.2009.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li W, Yang Y, Liu Z, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732–1738. doi: 10.7150/ijbs.45120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Based E, Health P. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Health. 2003;57(11):857–863. doi: 10.1136/jech.57.11.857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moccia L, Janiri D, Pepe M, et al. Affective Temperament, Attachment Style, and the Psychological Impact of the COVID-19 Outbreak: An Early Report on the Italian General Population. Brain, Behavior, and Immunity. 2020:S0889–1591(20)30586–9. doi: 10.1016/j.bbi.2020.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2019;17(march):1729–1732. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newby J, O’Moore K, Tang S, Christensen H, Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. MedRxiv. 2020;2020(05):03.20089961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chaix B, Delamon G, Guillemasse A, Brouard B, Bibault JE. Psychological distress during the COVID-19 pandemic in France: a national assessment of at-risk populations. MedRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmad A, Rahman I, Agarwal M. Factors influencing mental health during COVID-19 outbreak: an exploratory survey among indian population. MedRxiv. 2020. [Google Scholar]
- 20.Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1):e32. doi: 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zarghami M. Psychiatric aspects of coronavirus (2019-nCoV) infection. Iran J Psychiatry Behav Sci. 2020;14(1):2019–2021. [Google Scholar]
- 22.Le TA, Quynh M, Le T, et al. Multi-level predictors of psychological problems among methadone maintenance treatment patients in difference types of settings in Vietnam. BMC Psychiatry. 2019;4(73):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lovibond SH&L. Manual for the Depression Anxiety & Stress Scales. Second ed. Sydeney: psychological foundation; 1995:1–2. [Google Scholar]
- 24.Austrian K, Pinchoff J, Tidwell JB, et al. COVID-19 related knowledge, attitudes, practices and needs of households in informal settlements in Nairobi, Kenya. [Preprint]. Bull World Health Organ. 2020. doi: 10.2471/BLT.20.260281 [DOI] [Google Scholar]
- 25.Sorokin MY, Kasyanov ED, Rukavishnikov GV, et al. Structure of anxiety associated with the COVID-19 pandemic in the Russian-speaking sample: results from on-line survey. MedRxiv. 2020;1. [Google Scholar]
- 26.Liang L, Ren H, Cao R, et al. The effect of COVID-19 on youth mental health. Psychiatr Q. 2020;21:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alkwiese M, Alsaqri SH, Aldalaykeh M, Hamzi M, Mahdi M, Shafie Z. Anxiety among the general population during coronavirus-19 disease in Saudi Arabia: implications for a mental support program. MedRxiv. 2020;1. [Google Scholar]