Angelini and colleagues, in the current edition of the Journal of the American Heart Association (JAHA),1 provide an extension of a commonly held perspective regarding the challenging and emotion‐laden consideration of sudden death in young (current and would‐be) athletes. They review data of the results of screening in adolescents and young athletes and provide important new information on the yield of cardiac magnetic resonance imaging (CMR) in diagnosing abnormalities of cardiac structure that may predispose individuals to cardiac arrest and sudden death. In particular, they highlight the high accuracy of CMR in diagnosing cardiomyopathy and anomalous origins of the coronary artery (AOCA) with an intramural course. The authors suggest the following:
Adolescence is the optimal time to assess current and future athletes with respect to cardiac abnormalities that may predispose to sudden death, and they specifically recommend CMR imaging as part of screening. They state that the prevalence of high‐risk cardiovascular conditions may be as high as 1 in 68 military recruits and suggest that mortality may be reduced by identifying individuals with these “high risk conditions” and providing “effective treatment” or withdrawal/disqualification from strenuous activities.
They contend that screening based on history and physical, and echocardiography is insufficiently accurate to detect many of the abnormalities that pose a risk for sudden death, and that screening with CMR, a highly accurate method, may be cost effective.
They recommend a societal approach to understanding the costs, benefits, and practicality of preventative screening, considering the magnitude of risk that “cannot be ignored,” and call for a large controlled study to identify outcomes following a detailed screening protocol in military recruits, randomized to history and physical alone, compared with a protocol including CMR.
This perspective addresses an important aspect of sports cardiology, particularly given the social and cultural value placed on sports, and particularly competitive sports.
Sudden cardiac death in a young athlete is often highly publicized. Athlete victims of sudden cardiac death are typically in the prime of their life and represent the epitome of physical health, and this is a tragedy to the families involved. As a result, there is a dramatic impact beyond grieving family and friends, felt by the broader sports community that stir ups considerable emotion and calls to action.
It may seem at first self‐evident that we should do all we can to identify people at potential risk of sudden death. However, to properly assess the potential consequences of a vastly expanded screening program for sudden death in young individuals, whether they become athletes or not, there are a number of considerations that must be addressed, in our view, to make a considered decision regarding all of the benefits and risks of screening in adolescents.
In 1968, Wilson and Jungner2 outlined the 10 key principles for an ideal screening program. To paraphrase this classic article, a screening program should (1) focus on common, treatable medical conditions; (2) use a suitable, cost‐effective test that can accurately detect the condition; and (3) lead to an intervention that can reduce complications of the condition without causing adverse effects by applying the intervention to individuals who will not benefit.
Therefore, we need to understand the incidence of unexpected cardiac arrest in young people, potentially related to competitive sport or exertion. Second, we need to consider what proportion of cardiac arrests in young people may be predictable with current testing. Third, we need to consider whether arbitrary restriction from sport (disqualification) is likely to have a substantial impact on the number of observed sudden deaths over the subsequent decades. Finally, we must consider the potential consequences of identifying structural heart disease that may pose a risk for sudden death, with respect to the social, psychological, health‐related, and economic outcomes for the individuals thus identified and labeled as “potentially at risk.”
The following considerations need to be emphasized when establishing a program of broad and comprehensive screening of adolescents and considering the pros and cons involved (Figure).
Figure 1. Preparticipation screening using history, physical examination, ECG, and cardiac magnetic resonance imaging as first line.
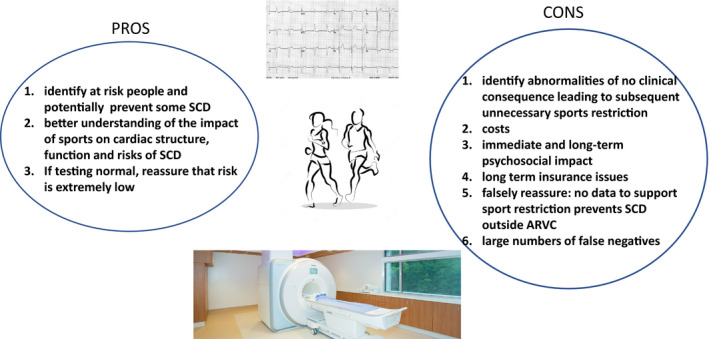
ARVC indicates arrhythmogenic right ventricular cardiomyopathy; and SCD, sudden cardiac death.
The incidence of cardiac arrest in young people, related to competitive sport, is very low: a large meta‐analysis of all available studies indicates an incidence of 0.7/100 000 per year, corroborated by recent studies.3, 4, 5 The most accurate possible screening methods available include history, physical, ECG, and CMR; when used together, these are able to identify almost every person with a relevant structural or electrical abnormality, at the time of testing, that is associated with sudden death. However, <50% of patients who ultimately have fatal cardiac arrest are identified by screening. This is because ≈30% to 40% of all sudden deaths occur in young individuals with no identifiable electrical or structural abnormalities.4, 6, 7, 8, 9 In addition, other individuals have normal testing initially but may eventually develop identifiable structural abnormalities such as myocarditis, cardiomyopathy, or coronary disease. Some may have “subclinical” arrhythmogenic right ventricular cardiomyopathy or hypertrophic cardiomyopathy, but these conditions are difficult to diagnose in adolescents because of the variable clinical phenotype during the first 2 decades of life.10 The observation of a relatively high rate of sudden death despite an intensive screening program among adolescent athletes (6.8/100 000/year in elite soccer players aged 16 years)10 illustrates the challenges of diagnostic testing in young individuals with respect to utilizing tests with optimal sensitivity in order to identify disease(s) associated with sudden cardiac death.
Among individuals identified with structural heart disease, the risk of sudden death is extremely low. In a detailed autopsy study, the annual risk of sudden death, in people with hypertrophic cardiomyopathy under the age of 45 years, is estimated to be 0.3 to 0.4/1000 patient years, with most of these sudden deaths occurring at rest.11
Using the values obtained by Angelini et al for AOCA detected by CMR, the estimated 0.44% prevalence of this condition would result in 4400 people per million diagnosed with this potentially dangerous abnormality. Eckhart et al have provided the most comprehensive estimate of risk of sudden death caused by AOCA. Among 6.3 million armed forces recruits, there were 21 sudden deaths related to AOCA.8 The prevalence identified by Angelini et al suggests that 27 772 of the 6.3 million recruits would have had a CMR diagnosis of AOCA and a death rate of 0.75 in every 1000 people with AOCA.
In other words, one would have had to screen 6.3 million recruits to identify 21 destined to have sudden death from AOCA. This translates into 1 such individual who could have been identified with CMR out of every 300 000 recruits imaged. In that study, there were 64 deaths caused by autopsy‐identified cardiovascular disease, equivalent to 13.0/100 000 recruit years. The majority died during exertion, although the intensity of the effort associated with sudden death was not specified. Even considering the 64 individuals identified with cardiac structural disease, some of whom would be challenging to identify (eg, myocarditis), one would have to screen 100 000 people to identify a single individual who is destined to die suddenly during basic training (a period of highest risk, given the physical and mental stresses involved in such training). Moreover, we have no idea if these deaths may or may not have been preventable.
Very importantly, for every such individual identified, there would have been 100 000 recruits informed they have a potentially life‐threatening disorder, restricted from activities, saddled with the anxiety and burden of knowing that they have structural heart disease, and subject to the belief that they were at some, and potentially large, risk of sudden death. Furthermore, they may have been advised to have procedures such as open heart surgery with its nontrivial risk, and the disease label may have had a very substantial impact on their economic outlook, medical insurability, self‐concept, social desirability, and potentially important consequences for their life habits with respect to a sedentary versus active lifestyle.
Most importantly, if one had “disqualified” these individuals from the armed forces, and from competitive sport, it is completely unknown what proportion would have had sudden death from other forms of strenuous activity that form part of everyday living, including recreational sport, occupational demands, and other strenuous activities associated with life in general.
Arrhythmogenic right ventricular cardiomyopathy is one of few conditions in which preventative measures (sports restriction, possibly β‐blocker therapy or even implantable cardioverter‐defibrillator implantation) appear to be protective from cardiac arrest; however, this condition is rarely seen in comprehensive autopsy studies of sudden death in young people, even with exercise or sports,4, 6, 7, 10 and may be difficult to diagnose in people <21 years of age, even with CMR.12
In considerations of screening, there is a major distinction between the sensitivity of screening history and physical in young individuals and potential athletes to “diagnose conditions associated with sudden death” versus “identifying individuals who actually suffer sudden death.” Retrospective studies of individuals who have in fact suffered cardiac arrest suggest that the incidence of premonitory symptoms, especially syncope, may be 20% to 30%.13, 14, 15, 16
Screening adolescents for sudden death results in a very challenging conundrum that may have lifelong consequences. Angelini et al suggest that “adolescence is the optimal time to ascertain the presence of high‐risk factors that could affect sports participation, either to discourage competitive exercise or to promote effective intervention.” Such a program may well identify a very small number of individuals who are “destined to die suddenly,” possibly during exercise, and in doing so lead to a recommendation of, or the mandating of abstention from competitive sport. This may conceivably reduce the future risk of sudden death (yet is completely unproven). However, there is likely to be demonstrable harm imposed on many more (a thousand or more fold) individuals, by the identification of abnormalities that either have no future health consequence, may trigger unnecessary anxiety about possible future symptoms (which can be intervened upon before a life‐threatening event), or are destined to occur but will remain unpreventable. Is there another widely accepted medical screening strategy that has these potential adverse consequences?
Unfortunately, much as we may wish for “effective interventions,” there is no evidence that in asymptomatic people in general, and athletes in particular, such interventions exist (apart from the possible, unproven benefit of exercise restriction). It is unclear how “an educated population can make definitive decisions about available alternatives,” especially when education requires knowledge we have yet to accrue, knowledge of risks that we cannot accurately calculate, and when available alternatives with known efficacy are at best scarce to nonexistent. These considerations, crucially, do not imply that screening is never of value, and we emphatically endorse shared decision making if a relevant abnormality is found by chance, after symptoms, or through “disease finding” in an “a priori” high‐risk population.17
In the discussion of screening of unselected adolescents with respect to conditions that are associated with a risk of sudden death, it is extremely important to note that we do not yet know which of these young individuals is destined to become a competitive athlete. If the recommendation, following discovery of a relevant abnormality, is to refrain from competitive sport, do we really want to inform a large cohort of young individual(s) that they may be at future risk, if they were never destined to become competitive athletes? Specifically, which sports are relevant in this discussion, performed at what intensity and under which environmental conditions? How do we perform screening in a calculated, directed way, as opposed to blanket screening in all young individuals? How do we deal with the (inevitable) false negatives that will occur, particularly for hard‐to‐diagnose conditions in adolescence such as arrhythmogenic right ventricular cardiomyopathy and hypertrophic cardiomyopathy?10 How do we respond in a sensible way to parents and families of young individuals who screen negative but nevertheless suffer sudden death?
For the vast majority of young individuals not destined to participate in competitive endurance sport, “sports restriction” would not apply, yet many would undoubtably engage in vigorous exercise or even sport that falls outside of the scope of mandated screening often proposed; sudden death rates during competitive versus recreational sports are identical.5, 18 In fact, for most people intending to participate in endurance sport, the term “sports qualification” is inappropriate. For amateur, nonprofessional, and noncollegiate sports, physicians are not in the position to “disqualify” athletes, but should be in a position to, using the concepts of shared decision making, give their best possible advice to athletes and parents (if appropriate).
Mass screening using sensitive tools such as the CMR may be an example of “opening a Pandora's box.” This does not mean that screening is of no value, but it is important for readers to be aware of the estimated absolute probability of detecting a relevant abnormality on CMR if screening were to be contemplated, and the corresponding absolute probability of sudden death if such an abnormality is found. Bayesian statistics would show that the positive predictive value of this approach would be extremely low.12
Financial cost considerations aside, it is very important to recognize that screening young people, especially if they are not yet athletes, has considerable individual and societal costs. Similar to the considerations for screening for prostatic cancer, it is essential that we ask (and answer) the questions: What happens if I test positive? Is the treatment that is likely to be offered effective? Is the treatment worse than the disease?
In this context, it is relevant to note that in jurisdictions without established screening programs, regardless of the disparate healthcare systems, the risk of sudden death during competitive sport is virtually identical to that in jurisdictions where systematic screening is undertaken.4, 19
There already exists an effective, tested, established method of preventing sports‐related sudden death. This involves a system of care and rapid response protocol at sporting venues, including rapid deployment of automated external defibrillators and designated rescuers in case of cardiac emergencies. As Angelini and colleagues correctly point out, developing policies and procedures that improve the likelihood of successful resuscitation in the case of cardiac arrest are demonstrably useful and can be deployed at a substantially lower cost than mass screening. Examples of extremely high successful resuscitation rates have been described in Japan during marathons20 (with an astonishing 100% survival rate) and in Italy during competitive sport21 (with a 93% survival rate).
With appropriate education and training, systematic protocols for response during in‐the‐field cardiac arrest, and public education, very high survival rates can be obtained. These latter strategies can of course also lead to resuscitation of bystanders and spectators as well as athletes.
Conclusions
Not all difficult problems are solvable. Screening young individuals for sudden death may be an example of many situations where all options are imperfect, and our best option is to choose the least imperfect course. This may change over the next few decades as diagnostic precision improves, but currently, our efforts are better focused upon rapid sudden cardiac death identification and automated external defibrillator use in those people who suffer a cardiac arrest, as opposed to an expensive, unproven, and time‐consuming program to identify extremely rare events.
Disclosures
Drs Dorian, Goodman, and Connelly were members of the primary panel of the Canadian Cardiovascular Society/Canadian Heart Rhythm Society Joint Position Statement on the Cardiovascular Screening of Competitive Athletes.
(J Am Heart Assoc. 2020;9:e016332 DOI: 10.1161/JAHA.120.016332.)
For Disclosures, see page 4.
References
- 1. Angelini P, Muthupillai R, Cheong B, Paisley R. We have plenty of reasons to propose new, updated policies for preventing sudden cardiac death in young athletes. J Am Heart Assoc. 2020;9:e014368 DOI: 10.1161/JAHA.119.014368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wilson JMG, Jungner G; World Health Organization . Principles and Practice of Screening for Disease. Geneva: World Health Organization; 1968. [Google Scholar]
- 3. Mohananey D, Masri A, Desai RM, Dalal S, Phelan D, Kanj M, Wazni O, Griffin BP, Desai MY. Global incidence of sports‐related sudden cardiac death. J Am Coll Cardiol. 2017;69:2672–2673. [DOI] [PubMed] [Google Scholar]
- 4. Landry CH, Allan KS, Connelly KA, Cunningham K, Morrison LJ, Dorian P; Rescu Investigators . Sudden cardiac arrest during participation in competitive sports. N Engl J Med. 2017;377:1943–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Marijon E, Tafflet M, Celermajer DS, Dumas F, Perier MC, Mustafic H, Toussaint JF, Desnos M, Rieu M, Benameur N, et al. Sports‐related sudden death in the general population. Circulation. 2011;124:672–681. [DOI] [PubMed] [Google Scholar]
- 6. Bagnall RD, Weintraub RG, Ingles J, Duflou J, Yeates L, Lam L, Davis AM, Thompson T, Connell V, Wallace J, et al. A prospective study of sudden cardiac death among children and young adults. N Engl J Med. 2016;374:2441–2452. [DOI] [PubMed] [Google Scholar]
- 7. Finocchiaro G, Papadakis M, Robertus JL, Dhutia H, Steriotis AK, Tome M, Mellor G, Merghani A, Malhotra A, Behr E, et al. Etiology of sudden death in sports: insights from a United Kingdom regional registry. J Am Coll Cardiol. 2016;67:2108–2115. [DOI] [PubMed] [Google Scholar]
- 8. Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, Potter RN, Pearse LA, Virmani R. Sudden death in young adults: a 25‐year review of autopsies in military recruits. Ann Intern Med. 2004;141:829–834. [DOI] [PubMed] [Google Scholar]
- 9. Krahn AD, Healey JS, Chauhan V, Birnie DH, Simpson CS, Champagne J, Gardner M, Sanatani S, Exner DV, Klein GJ, et al. Systematic assessment of patients with unexplained cardiac arrest: Cardiac Arrest Survivors with Preserved Ejection Fraction Registry (CASPER). Circulation. 2009;120:278–285. [DOI] [PubMed] [Google Scholar]
- 10. Malhotra A, Dhutia H, Finocchiaro G, Gati S, Beasley I, Clift P, Cowie C, Kenny A, Mayet J, Oxborough D, et al. Outcomes of cardiac screening in adolescent soccer players. N Engl J Med. 2018;379:524–534. [DOI] [PubMed] [Google Scholar]
- 11. Weissler‐Snir A, Allan K, Cunningham K, Connelly KA, Lee DS, Spears DA, Rakowski H, Dorian P. Hypertrophic cardiomyopathy‐related sudden cardiac death in young people in Ontario. Circulation. 2019;140:1706–1716. [DOI] [PubMed] [Google Scholar]
- 12. McKinney J, Johri AM, Poirier P, Fournier A, Goodman JM, Moulson N, Pipe A, Philippon F, Taylor T, Connelly K, et al. Canadian Cardiovascular Society cardiovascular screening of competitive athletes: the utility of the screening electrocardiogram to predict sudden cardiac death. Can J Cardiol. 2019;35:1557–1566. [DOI] [PubMed] [Google Scholar]
- 13. Holst AG, Winkel BG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, Svendsen JH, Haunsø S, Prescott E, Tfelt‐Hansen J. Incidence and etiology of sports‐related sudden cardiac death in Denmark–implications for preparticipation screening. Heart Rhythm. 2010;7:1365–1371. [DOI] [PubMed] [Google Scholar]
- 14. Glinge C, Jabbari R, Risgaard B, Lynge TH, Engstrøm T, Albert CM, Haunsø S, Winkel BG, Tfelt‐Hansen J. Symptoms before sudden arrhythmic death syndrome: a nationwide study among the young in Denmark. J Cardiovasc Electrophysiol. 2015;26:761–767. [DOI] [PubMed] [Google Scholar]
- 15. Krahn AD, Healey JS, Simpson CS, Chauhan VS, Birnie DH, Champagne J, Gardner M, Sanatani S, Chakrabarti S, Yee R, et al. Sentinel symptoms in patients with unexplained cardiac arrest: from the cardiac arrest survivors with preserved ejection fraction registry (CASPER). J Cardiovasc Electrophysiol. 2012;23:60–66. [DOI] [PubMed] [Google Scholar]
- 16. Johri AM, Poirier P, Dorian P, Fournier A, Goodman JM, McKinney J, Moulson N, Pipe A, Philippon F, Taylor T, et al. Canadian Cardiovascular Society/Canadian Heart Rhythm Society joint position statement on the cardiovascular screening of competitive athletes. Can J Cardiol. 2019;35:1–11. [DOI] [PubMed] [Google Scholar]
- 17. Moulson N, Dorian P, Krahn A, Virani A, Isserow S, McKinney J. Shared decision making and the cardiovascular care of athletes: is it time to get back in the game? Can J Cardiol. 2019. Available at: 10.1016/j.cjca.2019.10.013. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 18. Risgaard B, Winkel BG, Jabbari R, Glinge C, Ingemann‐Hansen O, Thomsen JL, Ottesen GL, Haunsø S, Holst AG, Tfelt‐Hansen J. Sports‐related sudden cardiac death in a competitive and a noncompetitive athlete population aged 12 to 49 years: data from an unselected nationwide study in Denmark. Heart Rhythm. 2014;11:1673–1681. [DOI] [PubMed] [Google Scholar]
- 19. Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296:1593–1601. [DOI] [PubMed] [Google Scholar]
- 20. Kinoshi T, Tanaka S, Sagisaka R, Hara T, Shirakawa T, Sone E, Takahashi H, Sakurai M, Maki A, Takyu H, et al. Mobile automated external defibrillator response system during road races. N Engl J Med. 2018;379:488–489. [DOI] [PubMed] [Google Scholar]
- 21. Aschieri D, Penela D, Pelizzoni V, Guerra F, Vermi AC, Rossi L, Torretta L, Losi G, Villani GQ, Capucci A. Outcomes after sudden cardiac arrest in sports centres with and without on‐site external defibrillators. Heart. 2018;104:1344–1349. [DOI] [PubMed] [Google Scholar]


