Abstract
Background
Acute type A aortic dissection presents with abrupt onset of pain that requires emergency surgery. However, minimal research exists on posttraumatic stress disorder (PTSD) in survivors. We aimed to quantify the prevalence and describe characteristics of PTSD in patients following dissection.
Methods and Results
A total of 295 adult survivors of surgical dissection with an email on file were administered a cross‐sectional online survey about their dissection experience; 137 returned questionnaires, and 129 (94%) responded to the 4‐item Primary Care PTSD portion of the survey that was part of a larger lifestyle survey designed to study survivors of aortic dissection and surgery. In addition to the PTSD screening, it inquired about current sexual activity, exercise habits, and employment within the preceding 30 days. At a median of 6.8 years (quartile 1=2.6, quartile 3=8.9 years) after dissection, 23% of patients (30/129) screened positive for PTSD, with 44% (57/129) stating that within the past month they felt constantly on guard or watchful or were easily startled. Of those who screened positive and matched to their electronic medical record (n=27), only 2 (7.4%) had been tested and clinically diagnosed with PTSD. Patients who screened positive for PTSD were more likely to report limited current sexual activity than those who did not (odds ratio, 5.3; 95% CI, 1.9–15 [P=0.0006]).
Conclusions
PTSD is an important mental health consideration in aortic dissection survivors. Physicians should screen these patients for PTSD at follow‐up visits to identify those who test positive and refer them for further testing and treatment, such as trauma‐focused psychotherapy or medication.
Keywords: aortic dissection, acute type A, employment, exercise, posttraumatic stress disorder, sexual activity
Subject Categories: Aortic Dissection, Quality and Outcomes
Nonstandard Abbreviations and Acronyms
- AD
aortic dissection
- PC‐PTSD
Primary Care PTSD
- PTSD
posttraumatic stress disorder
Clinical Perspective
What Is New?
Patients with acute type A aortic dissections screen positive for posttraumatic stress disorder that is associated with limited sexual activity and reduced exercise and employment.
What Are the Clinical Implications?
Patients with acute type A aortic dissection should be informed that feelings of posttraumatic stress disorder, such as being on guard, startled, and having nightmares and intrusive thoughts, may occur after their event.
Physicians should screen for this and treat when present.
Introduction
An acute type A aortic dissection classically presents with abrupt onset of severe pain.1 The initiating aortic tear instigates a series of swift, painful, and life‐threatening events—a critical care response, emergency surgery—and is a setup for posttraumatic stress disorder (PTSD). Yet PTSD has been minimally explored in survivors of acute type A aortic dissection.2, 3
PTSD is a chronic and disabling disorder that can develop after exposure to highly stressful events characterized by actual or threatened harm to self or others.4 To meet the diagnostic criteria for PTSD set out in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5), a person must experience a series of symptoms, along with distress or functional impairment (eg, social and occupational) for 1 month after exposure to a severely traumatic event. Diagnostic criteria include intrusion symptoms, persistent avoidance of stimuli, negative alterations in cognition and mood (2 required), and alterations in arousal and reactivity (2 required) associated with the traumatic event. These symptoms may limit sexual activity, exercise, or employment.
Objectives of this study were to: (1) quantify the prevalence and describe the characteristics of PTSD and (2) relate PTSD to sexual activity, exercise, and employment in survivors of surgery for type A aortic dissection. We hypothesized that PTSD prevalence would be greater than that in the general population because of the traumatic nature of an aortic dissection, and that sexual activity, exercise, and employment would be limited by fear and reduced in patients with PTSD postdissection.
Patients and Methods
Study Population
From January 1, 1980, to July 1, 2017, 763 consecutive adults were operated on for acute type A aortic dissection at the Cleveland Clinic in Cleveland, Ohio. Of these, 468 were excluded for lack of an accurate email address (n=452) or because they had died (n=16). A lifestyle online survey, modified from the International Registry of Acute Aortic Dissection lifestyle survey2 about the dissection experience, was sent to the remaining 295 patients (Figure 1). The survey included a validated 4‐item Primary Care PTSD (PC‐PTSD5) screening tool, along with questions about sexual activity, exercise habits, and employment that were written specifically for this study. All questions were optional, including patient identifiers. Use of these data for research was approved by the Cleveland Clinic's institutional review board, with patient consent completed at the beginning of the survey. The materials that support the findings of this study are available from the corresponding author upon reasonable request.
Figure 1.
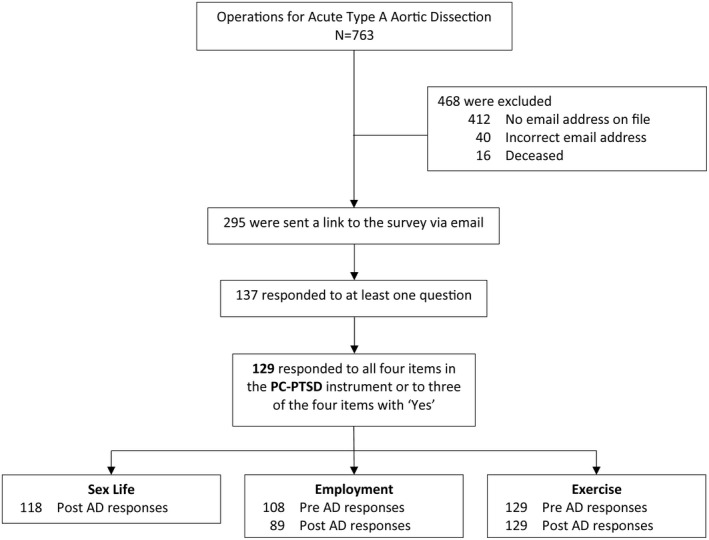
CONSORT‐style diagram of total study population, reasons for exclusion, and number of participants responding to relevant portions of the survey.AD indicates aortic dissection; and PC‐PTSD, Primary Care PTSD.
PTSD Screening Tool
The PC‐PTSD tool (Figure S1) is a validated survey used to screen for PTSD in the primary care setting.5 The 4 questions ask about nightmares; avoidance; being constantly on guard, watchful, or easily startled; and feeling numb or detached from others, activities, or surroundings in the past month. The screening survey has a sensitivity of 78% and specificity of 87% at a cutoff score of 3 with respect to the gold‐standard Clinician‐Administered PTSD Scale.5 Patients were considered to have a positive PTSD screening result if they answered “yes” to at least 3 of the 4 questions. Medical records of patients with a positive PC‐PTSD screening result were reviewed to determine whether a diagnostic workup for PTSD had been performed and PTSD documented.
Sexual Activity, Exercise, and Employment Questions
Details about sexual activity during and after dissection were gathered, along with information about exercise habits and employment before and after dissection through survey questions.
Data Analysis
All analyses were performed using SAS statistical software (SAS version 9.4, SAS Institute). Categorical variables are summarized as frequencies and percentages and continuous variables as 25th (quartile 1) and 75th (quartile 3) quartiles. Chi‐square test was used to test for associations between a positive PTSD screening result and: (1) limited current sexual activity, (2) predissection exercise, (3) postdissection exercise, and (4) postdissection employment. Because of our limited sample size, no formal hypothesis testing was performed. However, P values are provided as a matter of common practice. In addition, when estimable (number of events >3), odds ratios (ORs) and their corresponding exact 95% CIs and P values are presented to provide estimates for magnitude of association for relationships between the outcome (PTSD) and exposures of interest (postoperative complications, limited sexual activity, exercise status, and work status).
Results
Of the 295 patients surveyed, 137 returned questionnaires and 129 (94%) responded to the entire PC‐PTSD portion. Of the latter, sexual activity components were completed by 118 patients, 129 responded to questions about exercise before and after their dissection, and 74 responded to questions about employment before and after their dissection (Figure 1).
The median age at dissection was 54 years (quartile 1=46, quartile 3=65 years), the median age at survey completion was 61 years (quartile 1=54, quartile 3=70 years), and the median time between these 2 time points was 6.8 years (quartile 1=2.6, quartile 3=8.9 years) (Table 1).
Table 1.
Characteristics of Patients Matched Back to Their Medical Record
| Characteristic | Overall (N=129) | PC‐PTSD Screening | P Value | ||||
|---|---|---|---|---|---|---|---|
| Positivea (n=30) | Negativea (n=99) | ||||||
| nb | No. (%) or Median (Q1, Q3) | nb | No. (%) or Median (Q1, Q3) | nb | No. (%) or Median (Q1, Q3) | ||
| Demographics | |||||||
| Women | 72 | 19 (26) | 16 | 5 (31) | 56 | 14 (25) | 0.6c |
| Race | |||||||
| Black | 72 | 5 (6.9) | 16 | 2 (12) | 56 | 3 (5.4) | 0.3d |
| White | 72 | 64 (89) | 16 | 14 (88) | 56 | 50 (89) | 0.8c |
| Other | 72 | 1 (1.4) | 16 | 0 (0) | 56 | 1 (1.8) | >0.9d |
| Age at dissection, y | 112 | 54 (46, 65) | 25 | 49 (40, 57) | 87 | 56 (49, 66) | 0.005|| |
| Age at survey completion, y | 121 | 61 (54, 70) | 29 | 56 (49, 66) | 92 | 63 (56, 73) | 0.003|| |
| Time from dissection to completion of survey, y | 118 | 6.8 (2.6, 8.9) | 26 | 5.7 (1.6, 8.9) | 92 | 7.2 (3.0, 9.1) | 0.3|| |
Q1 indicates first quartile; and Q3, third quartile.
Posttraumatic stress disorder (PTSD) status determined by the Primary Care PTSD (PC‐PTSD) screening tool.
Patients with data available.
Pearson chi‐square test.
Fisher exact test.
Kruskal–Wallis test.
Clinical Data
Ethical concerns raised by the institutional review board allowed patients to remain anonymous, limiting our ability to match patients to the electronic medical record (72 of 129 respondents) (Table 1). Of the 72 matched respondents, 74% (n=53) were men, 89% (n=64) were white, and 6.9% (n=5) were black. Postoperative complications were defined by The Society of Thoracic Surgeons National Database, Adult Cardiac Surgery (http://www.sts.org/sts-national-database/database-managers/adult-cardiac-surgery-database/data-collection). Of the 72 patients, 43% (n=31) had no postoperative complications, 32% (n=23) had 1 postoperative complication, 15% (n=11) had 2 postoperative complications, and 9.7% (n=7) had ≥3 postoperative complications. The most common complications were atrial fibrillation (35%, n=25) and prolonged (>24 hours) ventilation (33%, n=24).
PTSD Prevalence and Characteristics
Among 129 patients with a PTSD screening assessment, 57 (44%) stated that within the past month they were constantly on guard, watchful, or easily startled; 46 (36%) felt numb or detached from others, activities, or their surroundings; and 35 of 128 (27%) stated that they had nightmares about their dissection and thought about it when they did not want to. Twenty‐four percent of patients (31/127) responded that they had tried hard not to think about their dissection and went out of their way to avoid situations that reminded them of it. In total, 30 patients (23%) screened positive for PTSD (Figure 2). The proportion of positive PTSD screening results fluctuated as time between dissection and survey response increased (Figure 3). Of the 27 patients who screened positive for PTSD in the survey and could be matched back to the electronic medical record, only 2 (7.4%) were formally diagnosed with PTSD. One of these had a PTSD diagnosis before the dissection.
Figure 2.
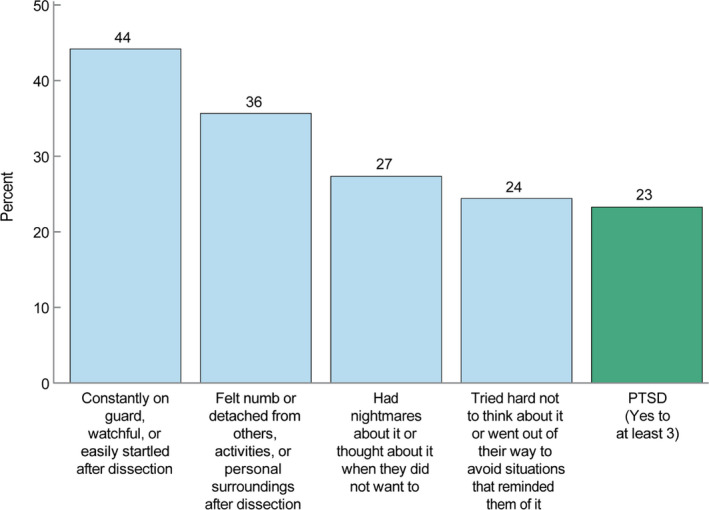
Patients with acute type A dissection and responses to posttraumatic stress disorder (PTSD) screening.Breakdown of the percentage of respondents who answered “yes” to each question on the 4‐Item Primary Care PTSD screening tool.
Figure 3.
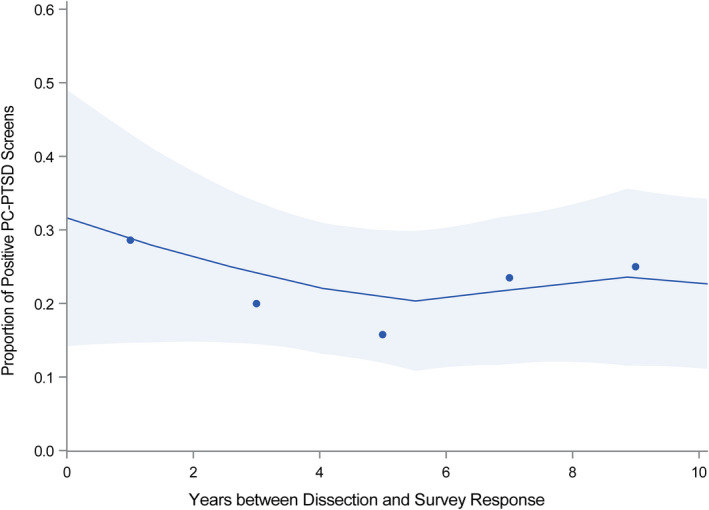
Temporal trend of positive posttraumatic stress disorder (PTSD) screening results as the time between dissection and survey response increased.Circles represent the proportion of positive PTSD screenings within 2‐year intervals since dissection, plotted at their respective midpoints. Solid line represents a nonparametric loess curve to capture nonlinearity in the relationship between the proportion of positive PTSD screenings and the time between dissection and survey response and shaded area represents a 68% confidence band equivalent to ±1 standard error.
Patients with a positive PTSD screening result tended to be younger compared with patients with a negative PTSD screening result (Table 1). However, sex, race, and time from dissection to completion of the survey were similarly distributed across the 2 groups (Table 1).
Postoperative Complications
Patients who experienced postoperative complications were more likely to have a positive PTSD screening result. Those who experienced at least 1 postoperative complication were an estimated 2.8 (0.72–13, P=0.17) times more likely to screen positive for PTSD than those who had no postoperative complications (Table 2). Furthermore, among patients who experienced at least 1 postoperative complication, those who experienced >1 were 2.3 (0.48–12, P=0.4) times more likely to screen positive for PTSD than those who had only 1 postoperative complication.
Table 2.
Summary of Associations Between PTSD and Postoperative Complications, Sexual Activity, Exercise, and Work Status in Patients With Acute Type A Dissection
| Variable | PC‐PTSD Screening | ORb (95% CI)c | P Valued | |||
|---|---|---|---|---|---|---|
| Positive (n=30) | Negative (n=99) | |||||
| na | No. (%) | na | No. (%) | |||
| Postoperative complications | ||||||
| Permanent stroke | 16 | 0 (0) | 56 | 2 (3.6) | b | >0.9 |
| Reoperation for bleeding/tamponade | 16 | 1 (6.3) | 56 | 1 (1.8) | b | 0.8 |
| Other noncardiac reoperation | 16 | 2 (13) | 56 | 1 (1.8) | b | 0.2 |
| Atrial fibrillation | 15 | 5 (33) | 50 | 19 (38) | 0.82 (0.19–3.1) | >0.9 |
| Renal failure requiring dialysis | 16 | 1 (6.3) | 56 | 2 (3.6) | b | >0.9 |
| Renal failure | 16 | 3 (19) | 56 | 4 (7.1) | 3.0 (0.38–20) | 0.4 |
| Prolonged ventilation (>24 h) | 16 | 10 (63) | 56 | 14 (25) | 5.0 (1.3–20) | 0.01 |
| At least 1 postoperative complication (≥1 vs 0) | 16 | 12 (75) | 56 | 29 (52) | 2.8 (0.72–13) | 0.17 |
| Multiple postoperative complications (>1 vs 1) | 12 | 7 (58) | 29 | 11 (38) | 2.3 (0.48–12) | 0.4 |
| Postdissection sexual activity | ||||||
| Does your diagnosis of aortic dissection limit your current sexual activity? | 27 | 18 (67) | 91 | 25 (27) | 5.3 (1.9–15) | 0.0006 |
| Exercise | ||||||
| Exercised predissection | 30 | 16 (53) | 99 | 63 (64) | 0.65 (0.26–1.6) | 0.4 |
| Exercised postdissection | 30 | 14 (47) | 99 | 60 (61) | 0.57 (0.23–1.4) | 0.3 |
| Work status | ||||||
| Employed predissection | 27 | 27 (100) | 81 | 66 (81) | b | 0.02 |
| Employed postdissection | 20 | 9 (45) | 69 | 43 (62) | 0.49 (0.16–1.5) | 0.3 |
PC‐PTSD indicates Primary Care PTSD; and PTSD, posttraumatic stress disorder.
Patients with data available.
Odds ratio (OR) not estimable owing to low number of events (<3).
Exact CI.
Exact P value.
The most common postoperative complication was atrial fibrillation, which occurred in 24 of 65 patients of whom it was known (37%), followed by prolonged ventilation for 24 hours (24/72, 33%) and renal failure (7/72, 9.7%). The odds of atrial fibrillation were similar between the 2 groups (OR, 0.82; 95% CI, 0.19–3.1 [P>0.9]); patients who had prolonged ventilation were 5 times more likely to screen positive for PTSD (1.3–20, P=0.01) and those experiencing renal failure were 3 times more likely to screen positive for PTSD (0.38–20, P=0.4).
Sexual Activity
Patients with limited current sexual activity were 5.3 (1.9–15, P=0.0006) times more likely to have a positive PTSD screening result than those who were not experiencing limited sexual activity at the time of being surveyed (Table 2).
Only 2.4% of patients (3/127) experienced their aortic dissection during sexual activity (Table 3). Sixty‐one percent of patients (76/125) reported that their dissection had affected their life in a negative way, and 36% of those (27/76) attributed this to limitations in sexual activity. Thirty‐six percent of patients (43/118) stated that having had an aortic dissection limited their current sexual activity. Reasons for this were erectile dysfunction (57%, 8/14), fear (42%, 18/43), lack of desire (26%, 11/43), and other (23%, 10/43), which included paralysis and medication effects.
Table 3.
Acute Type A Dissection Patient Survey Questions About Sexual Activity
| Question | Patient Response | na | No. (%) |
|---|---|---|---|
| What were you doing when it [aortic dissection] started? | Having sex | 127 | 3 (2.4) |
| Has your aortic dissection affected your life in a negative way? | Yes | 125 | 76 (61) |
| How? | My sexual activity is limited | 76 | 27 (36) |
| Does your diagnosis of aortic dissection limit your current sexual activity? | Yes | 118 | 43 (36) |
| Fear? | Yes | 43 | 18 (42) |
| Lack of desire? | Yes | 43 | 11 (26) |
| Erectile dysfunction (men only) | Yes | 14 | 8 (57) |
| Other reason? | Yes | 43 | 10 (23) |
Patients with data available.
Exercise, Employment, and PTSD
Patients who exercised before the dissection were less likely to screen positive for PTSD than those who did not (OR, 0.65; 95% CI, 0.26–1.6 [P=0.4]), as were patients who regularly exercised after the dissection (OR, 0.57; 95% CI, 0.23–1.4 [P=0.3]) (Table 2).
Patients who were employed after their dissection were less likely to screen positive for PTSD than those who were not (OR, 0.49; 95% CI, 0.16–1.5 [P=0.3]).
Discussion
Principal Findings
Almost half of survivors of acute type A aortic dissection still had some features of PTSD after a median of nearly 6 years following successful repair, and more than 1 in 5 patients screened positive for the disorder. PTSD symptoms are an important mental health consideration, and presence of a positive PTSD screening result in this population was 3 times that of the general population, according to the National Comorbidity Survey Replication, which estimates the lifetime prevalence of PTSD among adult Americans to be 6.8%.6
However, few of these patients had undergone a workup for their symptoms or were diagnosed and treated for PTSD. Even long after these events, they continue to have posttraumatic symptoms. Patients who screened positive for PTSD were more likely to report limited sexual activity than those without a positive screening result. There was insufficient evidence to establish an association between a positive PTSD screening result and exercise or employment.
PTSD in Cardiovascular Disease
PTSD occurs frequently in patients with cardiovascular disease who experience an acute event,7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 with 16% developing it after an acute myocardial infarction.7, 8 Even after elective coronary artery bypass grafting, 8% to 18% of patients experience PTSD during the first postoperative year.11 PTSD after cardiovascular events is associated with worse general functioning, reduced adherence to medications, and a higher likelihood of cardiac readmission.18, 20 Even individuals with partial PTSD symptoms, as reported by many of our patients, may experience functional impairment and reduced quality of life.21, 22, 23
Few studies have examined PTSD in patients with aortic dissection. Adam and colleagues3 reported findings similar to ours using 2 PTSD diagnostic tests. They showed that 65 of 206 patients (32%) scored ≥40 on the Post‐Traumatic Stress Symptoms 14 test, indicating the possibility of PTSD, and 43 additional patients were at risk for PTSD. This cohort was screened in more detail than our group. However, because of its brevity and efficiency, the 4‐question PC‐PTSD screening tool we used is more easily administered in a clinical setting given the multitude of issues that may arise during a postoperative visit.
Aortic Dissection, Sexual Activity, and PTSD
Dissection during sexual activity
It has been suggested that sexual activity, particularly in younger men, can instigate acute type A aortic dissection via arterial hypertension. In a study of 365 patients, 16% of men younger than 50 years and 11% of men older than 50 years experienced aortic dissection activity but no women experienced aortic dissection during sexual activity.24 However, we found that only 2% of patients reported that they were engaged in sexual activity at the onset of aortic dissection.
Why is sexual activity reduced after surviving surgery for dissection?
In our cohort, more than a third of patients stated that their diagnosis limited their current sexual activity. Chaddha and colleagues2 reported similar findings, with 20% of patients citing erectile dysfunction, 15% reporting lack of libido, and 13% reporting fear. Despite the physical and mental benefits of sexual activity, participation has been shown to be significantly reduced in patients with PTSD.25 PTSD may interfere with many aspects of sexual behavior, including desire, arousal, activity, consummation, and satisfaction.26, 27 Thus, not only do patients fear sexual activity after surgery for acute aortic dissection, but those with PTSD symptoms are even more unlikely to participate, losing the physical, mental, and emotional benefits of intimacy.
Aortic Dissection, Exercise, Employment, and PTSD
Lack of association between a positive PTSD screening result and reduced participation in exercise and employment may be related to the timing of the survey. It did not provide details about when patients returned to work or resumed exercise in relation to the operation. These activities could have been delayed by the presence of PTSD symptoms.
Because of the extensive time between dissection and receipt of the survey, recall may be imperfect regarding events that occurred at the time of dissection. In addition, it is possible that other patients had PTSD symptoms in the months and years following the event but symptoms may have resolved and were not captured in this cross‐sectional survey. Future studies should screen patients early postdissection to map PTSD trends over time.
Study Limitations and Strengths
This study was from a single institution with an exceptionally large volume of aortic dissections, which may limit generalizability. Our survey was voluntary and administered via email; thus, the sample is self‐selected and limited in power. The PTSD portion of the survey used a screening tool, and it is important to remember the distinction between that and more specific PTSD evaluation5 and clinical diagnosis of PTSD. In addition, the nature of this cross‐sectional follow‐up study limits conclusions to associations rather than inferences of causality. However, over 40% of respondents completed the survey, and important insights can guide patient care and further investigation.
Clinical Implications
Currently, there are no established PTSD screening guidelines for patients who survive an aortic dissection, and most physicians are unaware of the prevalence of the condition in this patient population. Physicians should screen patients with aortic dissection for PTSD at follow‐up visits. The simple screening tool could easily be implemented in a clinical setting to identify patients with symptoms of PTSD at least 1 month postoperatively.
A positive result on screening should trigger referral for more specific evaluation and treatment. For best outcomes, treatment should be initiated immediately after diagnosis. A number of evidence‐based treatments for PTSD are available. Trauma‐focused psychotherapy and serotonergic reuptake inhibitors for patients who prefer medication to psychotherapy may be indicated. As part of a multidisciplinary holistic approach to care, physicians should address sexual activity practices and emotions surrounding them with their patients with aortic dissection, including potential safety issues regarding medication interactions between antihypertensive and erectile dysfunction medications.
Conclusions
When PTSD becomes chronic, it can be associated with depression, suicidal behavior, high‐risk behaviors (eg, excessive use of alcohol and drugs or intentional engagement in dangerous activities), metabolic syndrome, and increased inflammatory response.28, 29, 30, 31, 32 Identifying PTSD in survivors of surgery for acute type A aortic dissection is critical in preventing these sequelae. Treating it may improve both quality of life and cardiovascular outcomes. We therefore recommend that physicians incorporate into follow‐up visits a health and well‐being assessment that includes PTSD screening.
Sources of Funding
This study was supported in part by the Drs Sidney and Becca Fleischer Heart and Vascular Education Chair, The Stephens Family Endowed Chair in Cardiothoracic Surgery, and Haslam Family Endowed Chair in Cardiovascular Medicine.
Disclosures
None.
Supporting information
Figure S1.
(J Am Heart Assoc. 2020;9:e015060 DOI: 10.1161/JAHA.119.015060.)
For Sources of Funding and Disclosures, see page 8.
This work was previously presented at the American Heart Association Scientific Sessions; November 10 to 12, 2018, in Chicago, IL.
References
- 1. Levy D, Le JK. Aortic dissection StatPearls. Treasure Island, FL: StatPearls Publishing; LLC; 2020. Available at: http://www.ncbi.nim.gov/books/nbk441963/. [Google Scholar]
- 2. Chaddha A, Kline‐Rogers E, Braverman AC, Erickson SR, Jackson EA, Franklin BA, Woznicki EM, Jabara JT, Montgomery DG, Eagle KA. Survivors of aortic dissection: activity, mental health, and sexual function. Clin Cardiol. 2015;38:652–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adam U, Habazettl H, Graefe K, Kuppe H, Wundram M, Kurz SD. Health‐related quality of life of patients after surgery for acute type A aortic dissection. Interact Cardiovasc Thorac Surg. 2018;27:48–53. [DOI] [PubMed] [Google Scholar]
- 4. Cahill SP, Pontoski K. Post‐traumatic stress disorder and acute stress disorder I: their nature and assessment considerations. Psychiatry (Edgmont). 2005;2:14–25. [PMC free article] [PubMed] [Google Scholar]
- 5. Freedy JR, Steenkamp MM, Magruder KM, Yeager DE, Zoller JS, Hueston WJ, Carek PJ. Post‐traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010;27:615–624. [DOI] [PubMed] [Google Scholar]
- 6. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age‐of‐onset distributions of DSM‐IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. [DOI] [PubMed] [Google Scholar]
- 7. Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta‐analytic review. PLoS One. 2012;7:e38915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ginzburg K, Solomon Z, Koifman B, Keren G, Roth A, Kriwisky M, Kutz I, David D, Bleich A. Trajectories of posttraumatic stress disorder following myocardial infarction: a prospective study. J Clin Psychiatry. 2003;64:1217–1223. [DOI] [PubMed] [Google Scholar]
- 9. Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, Goodman SG, Granger CB, Steg PG, Gore JM, et al. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6‐month postdischarge death in an international registry. JAMA. 2004;291:2727–2733. [DOI] [PubMed] [Google Scholar]
- 10. Tedstone JE, Tarrier N. Posttraumatic stress disorder following medical illness and treatment. Clin Psychol Rev. 2003;23:409–448. [DOI] [PubMed] [Google Scholar]
- 11. Doerfler LA, Pbert L, DeCosimo D. Symptoms of posttraumatic stress disorder following myocardial infarction and coronary artery bypass surgery. Gen Hosp Psychiatry. 1994;16:193–199. [DOI] [PubMed] [Google Scholar]
- 12. Stoll C, Schelling G, Goetz AE, Kilger E, Bayer A, Kapfhammer HP, Rothenhausler HB, Kreuzer E, Reichart B, Peter K. Health‐related quality of life and post‐traumatic stress disorder in patients after cardiac surgery and intensive care treatment. J Thorac Cardiovasc Surg. 2000;120:505–512. [DOI] [PubMed] [Google Scholar]
- 13. Doerfler LA, Paraskos JA, Piniarski L. Relationship of quality of life and perceived control with posttraumatic stress disorder symptoms 3 to 6 months after myocardial infarction. J Cardiopulm Rehabil. 2005;25:166–172. [DOI] [PubMed] [Google Scholar]
- 14. Meister R, Princip M, Schmid JP, Schnyder U, Barth J, Znoj H, Herbert C, von Kanel R. Myocardial infarction—stress prevention intervention (MI‐SPRINT) to reduce the incidence of posttraumatic stress after acute myocardial infarction through trauma‐focused psychological counseling: study protocol for a randomized controlled trial. Trials. 2013;14:329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Perkins‐Porras L, Joekes K, Bhalla N, Sutherland C, Pollard M. Reporting of posttraumatic stress disorder and cardiac misconceptions following cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2015;35:238–245. [DOI] [PubMed] [Google Scholar]
- 16. Hari R, Begre S, Schmid JP, Saner H, Gander ML, von Kanel R. Change over time in posttraumatic stress caused by myocardial infarction and predicting variables. J Psychosom Res. 2010;69:143–150. [DOI] [PubMed] [Google Scholar]
- 17. Meister RE, Princip M, Schnyder U, Barth J, Znoj H, Schmid JP, Wittmann L, von Kanel R. Association of trait resilience with peritraumatic and posttraumatic stress in patients with myocardial infarction. Psychosom Med. 2016;78:327–334. [DOI] [PubMed] [Google Scholar]
- 18. von Kanel R, Hari R, Schmid JP, Wiedemar L, Guler E, Barth J, Saner H, Schnyder U, Begre S. Non‐fatal cardiovascular outcome in patients with posttraumatic stress symptoms caused by myocardial infarction. J Cardiol. 2011;58:61–68. [DOI] [PubMed] [Google Scholar]
- 19. Gao W, Zhao J, Li Y, Cao FL. Post‐traumatic stress disorder symptoms in first‐time myocardial infarction patients: roles of attachment and alexithymia. J Adv Nurs. 2015;71:2575–2584. [DOI] [PubMed] [Google Scholar]
- 20. Wasson LT, Shaffer J, Alcantara C, Schwartz JE, Edmondson D. The association of posttraumatic stress disorder and quality of life during the first year after acute coronary syndrome. Int J Cardiol. 2014;176:1042–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Breslau N, Lucia VC, Davis GC. Partial PTSD versus full PTSD: an empirical examination of associated impairment. Psychol Med. 2004;34:1205–1214. [DOI] [PubMed] [Google Scholar]
- 22. Schnurr PP, Ford JD, Friedman MJ, Green BL, Dain BJ, Sengupta A. Predictors and outcomes of posttraumatic stress disorder in World War II veterans exposed to mustard gas. J Consult Clin Psychol. 2000;68:258–268. [PubMed] [Google Scholar]
- 23. Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154:1114–1119. [DOI] [PubMed] [Google Scholar]
- 24. Gansera L, Deutsch O, Szameitat L, Eichinger W, Gansera B. Aortic dissections type A during sexual intercourse in male patients: accident or systematic coincidence? Examination of 365 patients with acute aortic dissection within 20 years. Thorac Cardiovasc Surg. 2016;64:133–136. [DOI] [PubMed] [Google Scholar]
- 25. Yehuda R, Lehrner A, Rosenbaum TY. PTSD and sexual dysfunction in men and women. J Sex Med. 2015;12:1107–1119. [DOI] [PubMed] [Google Scholar]
- 26. Letourneau EJ, Resnick HS, Kilpatrick DG, Saunders BE, Best CL. Comorbidity of sexual problems and posttraumatic stress disorder in female crime victims. Behav Ther. 1996;27:321–336. [Google Scholar]
- 27. Nunnink SE, Goldwaser G, Afari N, Nievergelt CM, Baker DG. The role of emotional numbing in sexual functioning among veterans of the Iraq and Afghanistan wars. Mil Med. 2010;175:424–428. [DOI] [PubMed] [Google Scholar]
- 28. Senneseth M, Alsaker K, Natvig GK. Health‐related quality of life and post‐traumatic stress disorder symptoms in accident and emergency attenders suffering from psychosocial crises: a longitudinal study. J Adv Nurs. 2012;68:402–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Taft CT, Kaloupek DG, Schumm JA, Marshall AD, Panuzio J, King DW, Keane TM. Posttraumatic stress disorder symptoms, physiological reactivity, alcohol problems, and aggression among military veterans. J Abnorm Psychol. 2007;116:498–507. [DOI] [PubMed] [Google Scholar]
- 30. Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, Stewart A, Schlenger WE, Wells KB. Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1997;154:1690–1695. [DOI] [PubMed] [Google Scholar]
- 31. Cohen BE, Marmar C, Ren L, Bertenthal D, Seal KH. Association of cardiovascular risk factors with mental health diagnoses in Iraq and Afghanistan war veterans using VA health care. JAMA. 2009;302:489–492. [DOI] [PubMed] [Google Scholar]
- 32. Weiss T, Skelton K, Phifer J, Jovanovic T, Gillespie CF, Smith A, Umpierrez G, Bradley B, Ressler KJ. Posttraumatic stress disorder is a risk factor for metabolic syndrome in an impoverished urban population. Gen Hosp Psychiatry. 2011;33:135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1.


