Abstract
Background
People with higher socioeconomic status generally enjoy better cardiovascular health across the life course than those with lower status. However, recent studies of upward mobility, where a child goes on to achieve higher socioeconomic status than his or her parents, suggest that it entails a tradeoff between better psychological well‐being and worse cardiometabolic health. In this study, we consider further evidence of this tradeoff in 2 multidecade studies, asking how upward income mobility relates to subsequent perceived stress, depressive symptoms, and metabolic syndrome. We ask parallel questions about downward mobility. Finally, given shifting patterns of mobility in recent generations, we also consider whether mobility's association with health outcomes differs for individuals born in the middle and later parts of the 20th century.
Methods and Results
We analyzed prospective data from Add Health (National Longitudinal Study of Adolescent Health; N=7542) and MIDUS (Midlife in the United States Study; N=1877). In both studies, evidence of the tradeoff was observed. Upward mobility presaged lower perceived stress and fewer depressive symptoms, in combination with higher metabolic syndrome rates. In contrast, downward mobility presaged worse outcomes on all health indicators. The magnitude of the mobility–health associations was similar across cohorts.
Conclusions
These findings provide evidence that upward income mobility is associated with a tradeoff between well‐being and cardiometabolic health. The similarity of the findings across cohorts suggests that this tradeoff is a generalized consequence of ascending the socioeconomic hierarchy, at least for Americans born in the middle and later parts of the 20th century.
Keywords: depression, metabolic syndrome, socioeconomic position
Subject Categories: Primary Prevention, Race and Ethnicity, Pediatrics
Clinical Perspective
What Is New?
Because high socioeconomic status is associated with fewer health problems than lower status, it is commonly believed that as people's financial conditions improve, so will their health.
However, the results in this study suggest that upward mobility entails a tradeoff in which improving financial conditions forecast higher psychological well‐being but worse cardiometabolic health.
What Are the Clinical Implications?
Upward mobility is not always beneficial for cardiometabolic health, even if it improves economic standing and mental health.
Nonstandard Acronyms and Abbreviations.
Add Health National Longitudinal Study of Adolescent Health
CES‐D Center for Epidemiologic Studies‐Depression Scale
MetS metabolic syndrome
MIDUS Midlife in the United States Study
SES socioeconomic status
Introduction
People with higher socioeconomic status (SES) tend to enjoy better health outcomes across the life course than those with lower SES. This socioeconomic gradient is present for outcomes that include depression, heart disease, functional limitations, and longevity.1, 2, 3, 4 Because of these robust health advantages, the findings of several recent studies of upward mobility—where a child goes on to achieve higher SES than his or her parents—are surprising. These studies indicate that upward mobility may entail a tradeoff between aspects of well‐being and physical health.5, 6, 7, 8, 9 In a study that followed >13 000 adolescents into adulthood, Gaydosh and colleagues found that obtaining a 4‐year college degree was associated with lower depression at ages 24 to 32. However, when rates of metabolic syndrome (MetS) were considered, the effects of college differed markedly across demographic groups. For white participants, a college education was associated with the expected advantage for metabolic health, and these benefits were also present for participants from middle‐ and high‐SES backgrounds. But for minority participants raised in lower SES households, a college degree forecasted higher rates of MetS at ages 24 to 32, relative to demographically similar peers without a college degree.10 These apparent “tradeoffs” of upward mobility have been observed in several other cohorts, with physical health outcomes that include diabetes mellitus, cardiovascular risk, and upper respiratory infection.5, 6, 7, 8, 9
Despite the consistency of these observations, important questions remain about their generalizability and interpretation. First, studies in this evolving literature have primarily focused on educational mobility, considering the long‐term well‐being and physical health of youth from disadvantaged backgrounds who nevertheless obtain college degrees. However, there are reasons to hypothesize that educational mobility entails unique challenges that do not accompany financial mobility. Research indicates that first‐generation college students face distinctive forms of stress that go beyond financial strain and academic difficulties. These stressors can include social isolation, identity conflicts, status uncertainty, and outright discrimination.11, 12, 13 It remains uncertain whether the health tradeoff observed in previous research is specific to upward mobility achieved through education versus a more generalized consequence of climbing the socioeconomic hierarchy. In this study, we utilize 2 multidecade longitudinal studies to address this question, asking how mobility defined by income relates to perceived stress, depressed mood, and MetS in adulthood.
Second, studies in this literature have primarily focused on Americans born after 1980, raising questions about whether the apparent health tradeoffs of upward mobility are cohort‐specific. Given shifting labor market demands, stagnant wages, wealth inequality, and reduced public funding of education, rates of upward mobility have declined markedly in recent generations. Two‐thirds of Americans born in the 1940s and 1950s attained higher SES than their parents, but less than half the children born in the 1970s and 1980s did so.14, 15 Based on these trends, one could hypothesize that contemporary youth seeking upward mobility face more obstacles and have fewer resources compared with their historical peers. If that is true, any mobility‐related health tradeoffs could be larger in recent cohorts compared with earlier ones.
In contrast, downward mobility has become more prevalent since the 1940s and 1950s.14, 15 These changing norms have reduced the stigma associated with downward mobility. Accordingly, one might hypothesize any resulting health consequences to be smaller in recent versus earlier cohorts. Families are also providing their grown children with more financial insulation in recent years, as reflected by the increasing proportion of young adults who return home after finishing college.16 This trend would also presumably soften any health impact of downward mobility in recent versus earlier cohorts.
Finally, while the health patterns observed in this literature have been characterized as a tradeoff, this interpretation has not been substantiated with formal analysis. In other words, upwardly mobile participants displayed fewer depressive symptoms and higher MetS at the group level compared with those with stable SES. Nevertheless, it remains unclear whether, at the person level, these health outcomes actually diverge in the manner implied by the conclusion about tradeoff. In this study, we address that question by quantifying tradeoff at the level of the individual.
Methods
Samples
We used data from Add Health (National Longitudinal Study of Adolescent to Adult Health) and MIDUS (Midlife in the United States Study). Both studies have online repositories from which the measures and data sets we use can be obtained (MIDUS, http://midus.wisc.edu; Add Health, https://www.cpc.unc.edu/projects/addhealth). Launched in 1994–1995, Add Health is a nationally representative sample of American adolescents who were enrolled at ages 11 to 20 years and most recently assessed at ages 24 to 32 years. Four waves of data are publicly available. We used data from wave 1, which included 20 745 adolescents ages 11 to 20 years, and wave 4, which reassessed 14 800 of those participants at ages 24 to 32 years. The analytic sample in this study includes 7542 individuals with complete data on relevant variables at waves 1 and 4. Compared with the larger sample, these individuals were more likely to be non‐Hispanic white (60.9% versus 53.0%) and less likely to live in low‐income families at wave 1 (15.2% versus 18.4%).
MIDUS is a national study of midlife Americans. Launched in 1995–1996, it enrolled 7108 noninstitutionalized Americans ages 25 to 78. From 2004 to 2006, 75% of surviving respondents participated in a follow‐up. Biological data were collected from a subset of these participants, who traveled to a general clinical research center for an overnight visit. Individuals in the biomarker substudy had more education than the overall MIDUS sample but were comparable on other demographics (age, sex, race, income).17 In 2011–2014, MIDUS added another 3577 adults to the cohort, aged 25 to 74 years. Of this new group, 863 participated in a biomarker substudy. Accordingly, the total MIDUS analytic sample in this study includes 1877 individuals who had complete data on all relevant variables.
Both studies obtained written informed consent from participants and approval from the institutional review boards of participating institutions.
Life‐Course Socioeconomic Conditions
To harmonize analyses across studies, we created 4 groups of participants based on their socioeconomic conditions during childhood (lower/higher) and currently (lower/higher). We refer to these groups as consistent life‐course disadvantage (lower status at both time points), upward mobility (lower status in childhood but higher in currently), downward mobility (higher status in childhood and lower in currently), and consistent life‐course advantage (higher status at both time points).
Childhood SES
In Add Health, we used prospectively collected data to stratify the sample into lower‐ and higher‐SES groups using a wave 1 family income of less than $16,000, which was roughly the federal poverty threshold for a family of 4 in 1994–1995, when participants were a mean age of 16 years. MIDUS did not have such data available, and, as a whole, its sample had relatively high childhood SES. To have sufficient cell sizes for analysis, we had to define childhood SES in this sample using a combination of parent educational attainment (retrospectively collected) and family welfare receipt (measured with a retrospective yes/no question asking whether the family received welfare during the participant's childhood or adolescence). The lower‐SES group included participants who either had received welfare during childhood or whose parents both had education of less than a high school diploma.
Current Adult SES
At wave 4, Add Health did not release data on household composition; therefore, we relied on personal income to define SES, using a threshold of $15,000, which was ≈150% of the federal poverty line for single‐occupant households in 2008, when participants were a mean age of 29 years. In MIDUS, we defined adult SES using a household income of ≤200% of the federal poverty line (considering household composition) at the time participants’ health was assessed (when participants were a mean age of 53 years). In sensitivity analyses, we raised the Add Health threshold to 200% and the MIDUS threshold to 250% of the respective federal poverty lines. As Figure S1 shows, when mobility was defined in this more stringent manner, the same tradeoff pattern was observed.
Health Status in Adulthood
We considered 3 health outcomes in adulthood that were common to both studies: perceived stress, depression, and MetS. In Add Health, these outcomes were measured at wave 4, when participants averaged 28.9±1.70 years of age. In MIDUS, they were assessed at a mean age of 53.4±12.53 years.
Perceived Stress
Both studies used Cohen's scale to measure perceived stress18, 19 over the previous month. Add Health used the 4‐item version (Cronbach's α=0.72) and MIDUS used the 10‐item version (Cronbach's α=0.86). Both versions capture the degree to which respondents find their lives to be stressful and uncontrollable. To make results comparable across studies, we standardized scores so they had a mean value of 0 and standard deviation of 1.
Depression
Both studies used the Center for Epidemiologic Studies‐Depression Scale (CES‐D),20 which measures depression over the previous week. MIDUS administered the full 20‐item scale (coefficient α=0.89). Following convention,20 we defined scores of ≥16 as indicative of significant depression. Because depressive symptoms are experienced along a continuum of severity, we also conducted secondary analyses using total CES‐D scores. Add Health administered a brief 5‐item version of the CES‐D (Cronbach's α=0.79), containing these items: “You were bothered by things that usually don't bother you”; “You could not shake off the blues, even with help from your family and your friends”; “You had trouble keeping your mind on what you were doing”; “You felt depressed”; “You felt sad.” We averaged responses to these items to create a continuous indicator of depression severity. However, because this version of the CES‐D does not have an established cutoff for significant depression, we used participants’ reports of whether they had ever been diagnosed with depression by a health professional (coded as 0=no and 1=yes). To make results comparable across studies, we standardized CES‐D scores so they had a mean of 0 and standard deviation of 0.
Metabolic Syndrome
MetS was diagnosed according to criteria from the International Diabetes Federation.21 To qualify, an individual must show central adiposity, defined by ethnic and sex‐specific cutoffs for waist circumference (for those of Europid and African descent, who make up nearly full MIDUS sample, cutoffs are >94 cm for men and ≥80 cm for women). At least 2 of 4 additional components must also be present: (1) raised blood pressure (systolic ≥130 mm Hg or diastolic ≥85 mm Hg); (2) raised triglycerides (≥150 mg/dL); (3) raised fasting glucose (≥100 mg/dL); (4) lowered HDL (high‐density lipoprotein) levels (<40 mg/dL in men and <50 mg/dL in women). Because Add Health did not measure fasting glucose and releases lipid values only in deciles, we used modified criteria validated in past research to diagnose MetS.10, 22 Central adiposity was coded as present for participants with a measured waist circumference ≥80 cm (female) or ≥94 cm (male). Elevated blood pressure was defined by self‐report of antihypertensive medication use, diagnosis of hypertension by a physician, or measured resting values >130 mm Hg systolic or >85 mm Hg diastolic. Following previous analyses of Add Health,10 we substituted glycated hemoglobin for fasting glucose, using the cutoff of ≥5.7% established in other epidemiologic cohorts,23 and defined lipids based on normative age‐related trends.10, 22 More specifically, elevated triglycerides were coded as present for males in the top 3 deciles of the sample distribution and females in the top 2 deciles. Similarly, lowered HDL was coded as present for males in the bottom 2 deciles and females in the bottom 3 deciles.
Our primary outcome was diagnosis of MetS. However, recognizing that expression of this disorder falls along a continuum of severity,24 we also performed sensitivity analyses on a secondary outcome representing the number of signs for which a participant exceeded the International Diabetes Federation threshold (range of 0–5).
Person‐Level Tradeoff
Previous studies have been interpreted as suggesting that upward mobility is associated with a tradeoff between well‐being and MetS, but this has not been formally tested. To fill this gap, we computed a dichotomous tradeoff variable at the person level. A value of 1 was assigned to participants who manifested the presumptive tradeoff—the absence of significant depression (as defined above for each study)—coupled with the presence of MetS (as defined above for each study). A value of 0 was assigned to participants who did not present in this manner, that is, who displayed any other combination of significant depression and MetS.
Statistical Analysis
Covariates
All models included covariates reflecting age, sex, and race/ethnicity. Age reflected years at the time of adult health assessment. Sex reported at the baseline wave of each study was coded as male (1) or female (0). Similarly, in the first wave of each study, participants reported on their race/ethnicity. Three dummy variables were created to reflect self‐identification as (1) black, non‐Hispanic; (2) Hispanic, any race; and (3) any other race, non‐Hispanic. The reference category included participants who self‐identified as white, non‐Hispanic. Multiracial participants were classified by their first choice of racial/ethnic category.
Hypothesis Testing
Analyses were performed in SPSS (IBM Corp), using generalized estimating equations with robust standard errors. We specified linear probability distributions for continuous outcomes (perceived stress, depressive symptoms), and logit probability distributions for binary outcomes (significant depression, MetS diagnosis). For binary outcomes, risk ratios (RRs) were calculated using each group's estimated marginal mean from the generalized estimating equations (ie, the covariate‐adjusted percentage of cases that were positive for the diagnosis.) For models that considered the number of MetS signs, a Poisson probability distribution was specified. In Add Health models, we used individual sample weights from wave 4 and generalized estimating equation models that specified clustering at the level of school to account for oversampling of smaller population groups and nonindependence of observations among participants attending the same schools. In MIDUS, family was specified as a clustering variable to account for the presence of sibling pairs.
All models included age, sex, and race/ethnicity as covariates, along with the 4‐level group variable reflecting life‐course socioeconomic trajectory. To examine whether group effects varied by self‐identified racial category, we estimated additional models that included the interaction terms life‐course group×non‐Hispanic white, life‐course group×non‐Hispanic black, and life‐course group×Hispanic, any race.
Results
Preliminary Analyses
Table 1 describes characteristics of the samples. As is clear, Add Health is a racially diverse sample of young adults who were born in the late 1980s and early 1990s. In contrast, MIDUS participants were born in the 1930s through 1950s and were middle‐aged adults at the health assessment. Relative to Add Health, MIDUS was less racially diverse, with participants predominantly self‐identifying as white.
Table 1.
Characteristics of Samples
| Add Health (N=7542) | MIDUS (N=1877) | |
|---|---|---|
| Years study began | 1994–1995 | 1995–1996 |
| Age at study entry, y | 16.03±1.67 | 46.24±11.83 |
| Age at adult health assessment, y | 28.91±1.70 | 53.38±12.53 |
| Female, % | 3799 (50.4) | 1018 (54.2) |
| White, non‐Hispanic | 4595 (60.9) | 1464 (78.0) |
| Black, non‐Hispanic | 1351 (17.9) | 266 (14.2) |
| Hispanic, any race | 1162 (15.4) | 66 (3.5) |
| High school graduate or less | 1519 (20.1) | 416 (22.2) |
| Bachelor's degree or more | 2640 (35.0) | 907 (48.3) |
| Consistently advantaged (higher income in childhood and currently) | 5555 (73.7) | 1182 (63.0) |
| Upwardly mobile (lower income in childhood only) | 890 (11.8) | 274 (14.6) |
| Downwardly mobile (lower income currently only) | 840 (11.1) | 274 (14.6) |
| Consistently disadvantaged (lower income in childhood and currently) | 257 (3.4) | 147 (7.8) |
| Likely clinical depression | 1316 (17.4) | 306 (16.3) |
| MetS diagnosis | 1885 (25.0) | 699 (37.2) |
| MetS signs | 1.80±1.15 | 2.12±1.34 |
Data are shown as mean±SD or n (%). Add Health indicates National Longitudinal Study of Adolescent Health; MetS, metabolic syndrome; and MIDUS, Midlife in the United States Study.
The samples had similar prevalence of significant depression (17% and 16%), defined in Add Health as being diagnosed with the disorder and in MIDUS as a score ≥16 on the CES‐D. MetS was 1.5 times as common in MIDUS (37%) versus Add Health (25%), consistent with age‐related trends in the prevalence of this condition.25 Table S1 presents health outcomes stratified by life‐course socioeconomic trajectory.
Upward Mobility and Adult Health
Perceived Stress
In both studies, perceived stress differed across groups defined by life‐course SES (Add Health: χ²[3]=73.5, P<0.00001; MIDUS: χ²[3]=17.7, P=0.001; Figure 1). There was no indication that this relationship was moderated by self‐identified racial category (for interactions, P values: Add Health, 0.09–0.56; MIDUS, 0.16–0.62). Table 2 presents contrast analyses across the sample, comparing upwardly mobile participants with those who experienced consistent life‐course advantage and consistent life‐course disadvantage. In Add Health, upward mobility was associated with a modest but reliable increase in perceived stress (0.17 SD), relative to consistent life‐course advantage. In MIDUS, this difference was considerably smaller (0.04 SD), and the CI included the null value. In both studies, upwardly mobile participants had lower perceived stress than individuals with consistent life‐course disadvantage (scores lower by −0.25 to −0.31 SD).
Figure 1. Adult health outcomes in each study as a function of life‐course socioeconomic group.
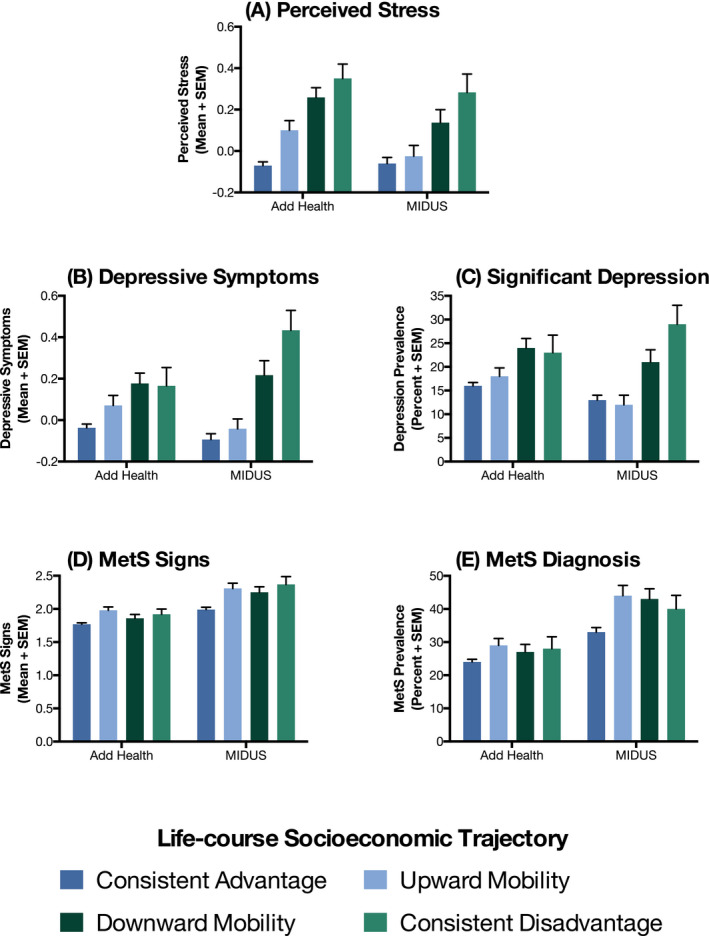
Outcomes depicted include psychological stress (A), depression (B and C), and metabolic syndrome (MetS; D and E). Values are adjusted for age, sex, race, and ethnicity. Add Health indicates National Longitudinal Study of Adolescent Health; and MIDUS, Midlife in the United States Study.
Table 2.
Results of Planned Contrasts for Perceived Stress
| Add Health Sample | MIDUS Sample | |||
|---|---|---|---|---|
| Contrast 1: UM vs CA | Contrast 2: UM vs CD | Contrast 1: UM vs CA | Contrast 2: UM vs CD | |
| Upwardly mobility and adult perceived stress | 0.17 (0.07–0.27) | −0.25 (−0.42 to −0.08) | 0.04 (−0.07 to 0.16) | −0.31 (−0.51 to −0.11) |
| Contrast 1: DM vs CA | Contrast 2: DM vs CD | Contrast 1: DM vs CA | Contrast 2: DM vs CD | |
|---|---|---|---|---|
| Downward mobility and adult perceived stress | 0.33 (0.23–0.43) | −0.09 (−0.26 to 0.08) | 0.20 (0.06 to 0.34) | −0.15 (−0.35 to 0.06) |
Values shown are mean difference scores between groups and 95% CIs. CA indicates consistently advantaged; CD, consistently disadvantaged; DM, downwardly mobile; and UM, upwardly mobile.
Depression
In both studies, the prevalence of significant depression varied according to life‐course SES (Add Health: χ²[3]=20.1 P<0.0002; MIDUS: χ²[3]=20.9 P=0.0001; Figure 1), with no indication of effect moderation by self‐identified racial category (for interactions, P values: Add Health, 0.18–0.96; MIDUS: 0.39–0.99). Contrast analyses indicated that in both samples, upwardly mobile participants were less likely to experience significant depression compared with those with consistent disadvantage (18% versus 23% in Add Health; 12% versus 29% in MIDUS; Table 3). However, upwardly mobile participants had depression rates comparable to those of individuals with consistent advantage. These patterns suggest that upward mobility attenuates the risks of adult depression conferred by exposure to childhood disadvantage.
Table 3.
Results of Planned Contrasts for Significant Depression and MetS
| Upward Mobility | Add Health Sample | MIDUS Sample | ||
|---|---|---|---|---|
| Contrast 1: UM vs CA | Contrast 2: UM vs CD | Contrast 1: UM vs CA | Contrast 2: UM vs CD | |
| Significant depression | 1.13 (0.96–1.31) | 0.78 (0.60–1.01) | 0.92 (0.65–1.62) | 0.41 (0.27–0.62) |
| MetS | 1.21 (1.08–1.35) | 1.04 (0.83–1.29) | 1.33 (1.14–1.55) | 1.10 (0.86–1.69) |
| Downward Mobility | Contrast 1: DM vs CA | Contrast 2: DM vs CD | Contrast 1: DM vs CA | Contrast 2: DM vs CD |
|---|---|---|---|---|
| Significant depression | 1.50 (1.31–1.72) | 1.04 (0.81–1.35) | 1.62 (1.24–2.13) | 0.72 (0.52–1.02) |
| MetS | 1.13 (1.00–1.27) | 0.96 (0.77–1.21) | 1.30 (1.11–1.53) | 1.08 (0.84–1.36) |
Values shown are risk ratios with 95% CIs. CA indicates consistently advantaged; CD, consistently disadvantaged; DM, downwardly mobile; MetS, metabolic syndrome; and UM, upwardly mobile.
Because depressive symptoms are experienced along a continuum of severity, we reconducted the contrast analyses utilizing continuous scores. Depressive symptoms varied according to life‐course SES (Add Health: χ²[3]=23.0 P<0.00004; MIDUS: χ² [3]=38.3, P=0.00001; Figure 1). Contrast analyses in MIDUS yielded patterns similar to those reported for significant depression (see Table S2). In other words, upwardly mobile participants had depressive symptoms comparable in severity to individuals with consistent advantage, and their symptom profile was markedly better relative to those with consistent disadvantage (0.47 SD lower). The Add Health patterns were different. Upwardly mobile participants had more severe depressive symptoms (0.11 SD) than individuals with consistent advantage but comparable to those with consistent disadvantage.
Metabolic Syndrome
Rates of MetS varied according to life‐course SES in MIDUS (χ²[3]=14.6 P=0.002) but not Add Health (χ²[3]=6.7, P=0.081; Figure 1). Neither study showed evidence of effect moderation by self‐identified racial category (for interactions, P values: Add Health, 0.08–0.84; MIDUS: 0.18–0.67). Despite the different patterns in omnibus tests, the results of contrast analyses were similar across studies (Table 3). Upwardly mobile participants had higher MetS prevalence compared with individuals with consistent advantage (29% versus 24% in Add Health; 44% versus 33% in MIDUS). In fact, their rates were modestly higher than individuals with consistent life‐course disadvantage (29% versus 28% in Add Health; 44% versus 40% in MIDUS), although the CIs around RRs included the null.
Like depression, MetS falls along a continuum of severity, so we reconducted the analyses with an outcome variable reflecting the number of metabolic signs exceeding the diagnostic threshold. In both studies, this variable differed according to life‐course SES (Add Health: χ²[3]=16.3, P=0.001; MIDUS: χ²[3]=23.0, P=0.00006; Figure 2). The results of contrast analyses were identical to those presented for diagnosis of MetS (see Table S2). In other words, upwardly mobile participants had more metabolic signs than individuals with consistent advantage (on average, 0.20 more in Add Health, and 0.32 more in MIDUS). They were statistically comparable to participants with consistent life‐course disadvantage.
Figure 2. Proportion of participants in each study who display presumptive tradeoff as a function of life‐course socioeconomic group.
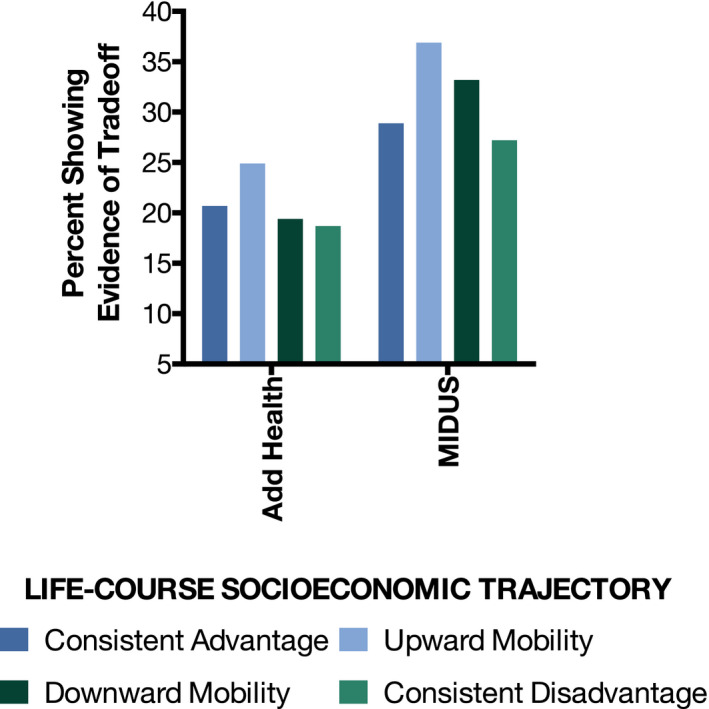
Tradeoff is defined as the absence of significant depression coupled with the presence of metabolic syndrome. Add Health indicates National Longitudinal Study of Adolescent Health; and MIDUS, Midlife in the United States Study.
Person‐Level Tradeoff
These findings suggest that upward mobility is associated with a tradeoff between well‐being and MetS. However, patterns at the aggregate level do not always mirror those at the individual level, so we reconducted the analyses with a new outcome variable reflecting the presumptive tradeoff: the absence of significant depression, along with presence of MetS. In both studies, the prevalence of this tradeoff differed across groups (Add Health: χ²[3]=10.8 P<0.013; MIDUS: χ²[3]=8.3 P=0.04; Figure 2), and the highest rates were seen among upwardly mobile participants. In terms of RRs, upwardly mobile participants were 21% to 27% more likely to show the tradeoff pattern compared with the consistently advantaged (Add Health: RR: 1.21 [95% CI, 1.06–1.37]; MIDUS: RR: 1.27 [95% CI, 1.07–1.52]) and 34% to 36% more likely to do so compared with the consistently disadvantaged (Add Health: RR: 1.34 [95% CI, 1.01–1.77]; MIDUS: RR: 1.36 [95% CI, 1.00–1.84]).
Downward Mobility and Adult Health
Perceived Stress
In both samples, downwardly mobile participants reported higher perceived stress than participants with consistent life‐course advantage (on average, 0.33 SD higher in Add Health; 0.20 SD higher in MIDUS; Table 2). However, their stress levels were comparable to those of participants with consistent disadvantage.
Depression
Depression outcomes followed the same pattern. In both samples, downward mobility was associated with higher rates of significant depression compared with consistent advantage (Add Health: 24% versus 16%; MIDUS: 21% versus 13%; Table 3) and with more severe symptoms (on average, 0.21 higher SD in Add Health and 0.31 higher SD in MIDUS; Table S2). However, downwardly mobile participants had similar rates of significant depression and depressive symptoms compared with individuals with consistent life‐course disadvantage.
Metabolic Syndrome
The MetS findings in MIDUS followed the same pattern as the psychosocial outcomes: downwardly mobile participants showed higher prevalence (21% versus 13%; Table 3) and more above‐threshold signs (on average, 0.26 more; Table S2) of MetS than participants with consistent advantage. Moreover, on both metabolic outcomes, these participants were comparable to those with consistent disadvantage. Add Health generally followed this pattern as well: downwardly mobile and consistently disadvantaged participants were similar on both metabolic outcomes. Nevertheless, downwardly mobile individuals had higher prevalence of MetS compared with those consistently advantaged (27% versus 24%), but these groups displayed similar numbers of signs on the continuous outcome.
Discussion
Despite the consistent health advantages associated with high SES,1, 2, 3, 4 recent studies of upwardly mobile youth indicate they experience a surprising mixture of outcomes in adulthood, characterized by lower psychological distress but worse cardiovascular health. In this study, we addressed 3 outstanding questions about this apparent tradeoff. The first question regarded generalizability: would the pattern continue to be evident when mobility was defined by income rather than education? In both of the multidecade prospective studies we considered, the answer was yes. Upwardly mobile participants reported substantially less psychological distress than consistently disadvantaged individuals. In fact, in most contrasts, their distress levels were comparable to consistently advantaged participants. However, this pattern was reversed for MetS, for which upwardly mobile participants fared worse than those with consistent advantage and closely resembled individuals with consistent disadvantage. These patterns were robust to alternative model specifications, where health outcomes were considered along a continuum of severity. Considered alongside previous research,5, 6, 7, 8, 9, 10 these results suggest that the apparent mobility–health tradeoff is a generalized phenomenon and not one restricted to instances in which mobility is achieved through education.
Research is starting to elucidate behavioral and biological pathways that could plausibly contribute to this tradeoff. The strongest candidate at present is self‐control and the tenacious pursuit of mobility‐related goals it enables. This persistent striving is a valuable psychological resource in many contexts,26, 27 but it seems to function as a double‐edged sword for disadvantaged youth. Indeed, prospective studies indicate that for disadvantaged youth, high self‐control forecasts success in school, avoidance of drugs, and better mental health, alongside higher stress hormone levels, faster cellular aging of leukocytes, and susceptibility to respiratory infection.6, 28, 29 Other processes that may contribute to the apparent mobility–health tradeoff include race‐ and class‐based discrimination, social isolation in school or the workplace, and internal conflicts about one's class identity.11, 12, 13 These candidates have received little empirical attention to date, so their roles in the patterns observed need to be considered in future research.
The study's second question also focused on generalizability, asking whether mobility's association with health might be cohort‐specific in ways that mirror broader generational trends in the prevalence of upward versus downward mobility. We found some evidence of cohort specificity in analyses of upward mobility and perceived stress. In Add Health, upward mobility was associated with more perceived stress relative to consistent advantage, but this relationship was not present in MIDUS. This discrepancy could reflect a generational shift, whereby upward mobility is a more stressful process for recent cohorts. Alternatively, it could represent a developmental phenomenon in which the stress associated with mobility dissipates with age. To discriminate between these interpretations, a longitudinal study with regular assessments of perceived stress is needed. Aside from perceived stress, we did not see evidence of cohort‐specific patterns; both types of mobility had the same relationship with depressive symptoms, MetS, and the tradeoff composite across cohorts. Consequently, we interpret the results as an indication that both upward and downward mobility have relatively consistent associations with health in adulthood, at least across cohorts born in the middle and later parts of the 20th century.
Our third question regarded how to interpret evidence of the mobility‐related health tradeoff. To clarify the meaning of previous findings, we considered whether this tradeoff was evident when the outcome was analyzed at the level of the person (rather than the group). It was. Across both studies, upwardly mobile individuals were more likely than other participants to have a profile marked by a lack of significant depression but, at the same time, the presence of MetS. Some readers may find it surprising that these outcomes tended to co‐occur because, in general, individuals with good mental health tend to have good physical health and vice versa.30, 31 It is also well established that depressive symptoms increase the risks of morbidity and mortality from cardiometabolic diseases.32 Despite these general patterns, recent evidence indicates that among members of disadvantaged groups, the same characteristics that promote well‐being and economic success might simultaneously exact a toll on physical health.13, 33, 34
The observations in the current study converge with earlier research in suggesting that upward mobility is associated with a health tradeoff.5, 6, 7, 8, 10 However, unlike some earlier reports in which the tradeoff appeared to be unique to individuals who self‐identified as black and/or Latinx,6, 10 we found signs of it across demographic categories. Because these earlier studies all focused on college, it could be that financial mobility worsens later cardiometabolic health through common stressors (eg, long hours at work, which undermine diet and sleep), whereas educational mobility presents challenges that are unique to and/or accentuated in youth of color (eg, stereotype threat, racial discrimination). Future research is needed to test these hypotheses explicitly. Statistical power could also be an explanation; with a relatively limited number of upwardly mobile participants of color, we may have been underpowered to detect mobility interactions with race and ethnicity.
The observations we describe must be considered in light of several limitations. First, our measure of life‐course socioeconomic conditions was coarse. It stratified participants into just 2 categories; captured a brief window in the adult life course; and, in the case of MIDUS, relied on retrospective reporting. Despite these weaknesses, the approach facilitated a harmonized analysis of 2 multidecade prospective studies that yielded consistent evidence of mobility–health associations. Still, future research could glean deeper and firmer insights into these processes with a more nuanced approach to characterizing SES trajectories. Second, neither of the studies measured health during childhood, so we cannot exclude the possibility of reverse causality, in which early disease or injury affected participants’ trajectories of SES. A scenario like this seems more likely to explain health outcomes related to downward versus upward mobility but nevertheless should be considered in future research where indicators of childhood health are available. Finally, it remains unclear how broad or narrow the apparent mobility–health tradeoff is. We focused on MetS to facilitate harmonized analysis, and the Add Health participants were too young to have developed most chronic diseases. However, future research needs to consider patterns of other more serious health outcomes in the same fashion (eg, myocardial infarction, premature mortality, stroke).
Despite these limitations, the current study advances knowledge regarding the health of individuals who experience socioeconomic mobility. In 2 multidecade prospective studies, we observed that upwardly mobile youth go on to experience less psychological distress in adulthood, as reflected by perceived stress and depressive symptoms, in tandem with higher MetS. In contrast, downwardly mobile youth go on to experience worse outcomes on all 3 dimensions of health. These findings converge with previous research on the same topic5, 6, 7, 8, 10 but extend our understanding of the phenomenon by showing that it generalizes across definitions of mobility and across cohorts of Americans. At a broader level, the patterns in this emerging literature suggest 2 somewhat counterintuitive conclusions for scientists and clinicians working on cardiovascular disease prevention. The first is that upward mobility is not always beneficial for cardiometabolic health, even if it improves economic standing and mental health. The second is that psychological well‐being and cardiometabolic health are not always aligned; in fact, the process of achieving upward mobility may cause them to diverge.
Sources of Funding
Preparation of this article was supported by grants from the National Institute of Child Health and Human Development (HD093718, HD091046); the National Heart, Lung, and Blood Institute (HL122328); and the National Institute on Drug Abuse (DA027827).
Disclosures
None.
Supporting information
Tables S1 and S2
Figure S1
(J Am Heart Assoc. 2020;9:e015698 DOI: 10.1161/JAHA.119.015698.)
For Sources of Funding and Disclosures, see page 10.
References
- 1. Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100(suppl 1):S186–S196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, Ricceri F, d'Errico A, Barros H, Bochud M, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta‐analysis of 1·7 million men and women. Lancet. 2017;389:1229–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen E, Miller GE. Socioeconomic status and health: mediating and moderating factors. Annu Rev Clin Psychol. 2013;9:723–749. [DOI] [PubMed] [Google Scholar]
- 4. Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. [DOI] [PubMed] [Google Scholar]
- 5. Courtin E, Nafilyan V, Avendano M, Meneton P, Berkman LF, Goldberg M, Zins M, Dowd JB. Longer schooling but not better off? A quasi‐experimental study of the effect of compulsory schooling on biomarkers in France. Soc Sci Med. 2019;220:379–386. [DOI] [PubMed] [Google Scholar]
- 6. Miller GE, Cohen S, Janicki‐Deverts D, Brody GH, Chen E. Viral challenge reveals further evidence of skin‐deep resilience in African Americans from disadvantaged backgrounds. Health Psychol. 2016;35:1225–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brody GH, Yu T, Miller GE, Chen E. Resilience in adolescence, health, and psychosocial outcomes. Pediatrics. 2016;138:e20161042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen E, Miller GE, Brody GH, Lei MK. Neighborhood poverty, college attendance, and diverging profiles of substance use and allostatic load in rural African‐American youth. Clin Psychol Sci. 2015;3:675–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sims J, Coley RL. Variations in links between educational success and health: implications for enduring health disparities. Cultur Divers Ethnic Minor Psychol. 2019;25:32–43. [DOI] [PubMed] [Google Scholar]
- 10. Gaydosh L, Schorpp KM, Chen E, Miller GE, Harris KM. College completion predicts lower depression but higher metabolic syndrome among disadvantaged minorities in young adulthood. Proc Natl Acad Sci USA. 2018;115:109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Johnson SE, Richeson JA, Finkel EJ. Middle class and marginal? Socioeconomic status, stigma, and self‐regulation at an elite university. J Pers Soc Psychol. 2011;100:838–852. [DOI] [PubMed] [Google Scholar]
- 12. Hardaway CR, McLoyd VC. Escaping poverty and securing middle class status: how race and socioeconomic status shape mobility prospects for African Americans during the transition to adulthood. J Youth Adolesc. 2009;38:242–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Destin M. Socioeconomic mobility, identity, and health: experiences that influence immunology and implications for intervention. Am Psychol. 2019;74:207–217. [DOI] [PubMed] [Google Scholar]
- 14. Hout M. Americans’ occupational status reflects the status of both of their parents. Proc Natl Acad Sci USA. 2018;115:9527–9532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chetty R, Grusky D, Hell M, Hendren N, Manduca R, Narang J. The fading american dream: trends in absolute income mobility since 1940. Science. 2017;356:398–406. [DOI] [PubMed] [Google Scholar]
- 16. Vespa J. The changing economics and demographics of young adulthood: 1975–2016. Current Population Reports. Washington DC: US Census Bureau; 2017;20–579. [Google Scholar]
- 17. Dienberg Love G, Seeman TE, Weinstein M, Ryff CD. Bioindicators in the MIDUS national study: protocol, measures, sample, and comparative context. J Aging Health. 2010;22:1059–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cohen S, Kamarck TW, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 19. Cohen S, Williamson GM. Perceived stress in a probability sample of the United States In: Spacapan S, Oskamp S, eds. The Social Psychology of Health. Newbury Park, CA: Sage; 1988:31–67. [Google Scholar]
- 20. Radloff LS. The CES‐D scale: a self‐report depression scale for research in the general population. J Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 21. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association ROR The Study of Obesity. Circulation. 2009;120:1640–1645. [DOI] [PubMed] [Google Scholar]
- 22. Bohr AD, Laurson K, McQueen MB. A novel cutoff for the waist‐to‐height ratio predicting metabolic syndrome in young American adults. BMC Public Health. 2016;16:295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ong KL, Tso AW, Lam KS, Cherny SS, Sham PC, Cheung BM. Using glycosylated hemoglobin to define the metabolic syndrome in United States adults. Diabetes Care. 2010;33:1856–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Goodman E. Metabolic syndrome and the mismeasure of risk. J Adolesc Health. 2008;42:538–540. [DOI] [PubMed] [Google Scholar]
- 25. Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA. 2015;313:1973–1974. [DOI] [PubMed] [Google Scholar]
- 26. Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, Houts R, Poulton R, Roberts BW, Ross S, et al. A gradient of childhood self‐control predicts health, wealth, and public safety. Proc Natl Acad Sci USA. 2011;108:2693–2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Casey BJ, Caudle K. The teenage brain: self control. Curr Dir Psychol Sci. 2013;22:82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Miller GE, Yu T, Chen E, Brody GH. Self‐control forecasts better psychosocial outcomes but faster epigenetic aging in low‐SES youth. Proc Natl Acad Sci USA. 2015;112:10325–10330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brody GH, Yu T, Chen E, Miller GE, Kogan SM, Beach SR. Is resilience only skin deep?: rural African Americans’ socioeconomic status‐related risk and competence in preadolescence and psychological adjustment and allostatic load at age 19. Psychol Sci. 2013;24:1285–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Evans DL, Charney DS, Lewis L, Golden RN, Gorman JM, Krishnan KR, Nemeroff CB, Bremner JD, Carney RM, Coyne JC, et al. Mood disorders in the medically Ill: scientific review and recommendations. Biol Psychiatry. 2005;58:175–189. [DOI] [PubMed] [Google Scholar]
- 31. Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychol Bull. 2005;131:260–300. [DOI] [PubMed] [Google Scholar]
- 32. Carney RM, Freedland KE. Depression and coronary heart disease. Nat Rev Cardiol. 2017;14:145–155. [DOI] [PubMed] [Google Scholar]
- 33. Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100:933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. James SA. John Henryism and the health of African‐Americans. Cult Med Psychiatry. 1994;18:163–182. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1 and S2
Figure S1


