Abstract
Background
Cardiovascular diseases (CVDs) and their risk factors need guideline‐oriented treatment to provide the best benefit for patients. These guidelines include recommendations for regular checkups, realized by general medical practitioners. In addition, individuals with CVD or CVD risk factors tend to use complementary methods for their condition. There is limited information on the association between complementary healthcare utilization and the adherence to recommended conventional health care.
Methods and Results
In this cross‐sectional analysis of the nationally representative 2017 National Health Interview Survey (n=26 742; response rate 80.7%) we examined the prevalence of conventional and complementary healthcare utilization within the past 12 months in individuals with CVD and/or CVD risk factors and the interactions between the two categories of health care. Of all participants, 38.1% reported risk factors for CVD and 11.4% a CVD diagnosis (groups show an overlap). Overall prevalence of visits to conventional and complementary medicine providers and the use of mind–body medicine was high within the population analyzed. Individuals with CVD and/or CVD risk factors using complementary health care were as likely or more likely to consult general practitioners (CVD: adjusted odds ratio [aOR], 1.17; 95% CI, 0.93–1.47; CVD risk: aOR, 1.21; 95% CI, 1.05–1.39) and medical specialists (CVD: aOR, 1.38; 95% CI, 1.17–1.64; CVD risk: aOR, 1.42; 95% CI, 1.28–1.58) than those not using complementary health care. Those using complementary health care were as likely to adhere to medical checkup as those not using complementary health care.
Conclusions
Complementary healthcare utilization use was not associated with a reduced adherence to conventional health care and recommended checkups. The potential positive association of complementary and conventional healthcare utilization needs to be confirmed in further studies.
Keywords: cardiovascular diseases, complementary therapies, health survey, mind–body therapies
Subject Categories: Cardiovascular Disease, Lifestyle, Risk Factors, Health Services
Nonstandard Abbreviations and Acronyms
- CVD
cardiovascular disease
- MBM
mind–body medicine
- NHIS
National Health Interview Survey
Clinical Perspective
What Is New?
Earlier research showed that complementary medicine utilization is common among patients with cardiovascular disease (CVD) or CVD risk factors, although exact numbers vary.
It has not been analyzed whether complementary medicine utilization affects the general health behavior on conventional medicine of patients with CVD or CVD risk factors.
In our analysis of the 2017 National Health Interview Survey individuals with CVD or CVD risk factors consulting complementary medicine practitioners and/or using mind–body medicine were also more likely to consult general medical practitioners.
What Are the Clinical Implications?
Due to a higher adherence to conventional medicine and recommended checkups, complementary medicine utilization can have a positive effect on conventional health behavior in patients with CVD or at risk of CVD.
The potential positive association of complementary and conventional healthcare utilization needs to be confirmed in further studies.
Introduction
Cardiovascular diseases (CVDs) comprise multiple disorders that affect the blood vessels and can lead to (sub)acute events such as stroke, ischemic heart disease, or congestive heart failure.1 Since 1990, CVD has been identified as the leading cause of death in both developed and nondeveloped countries. Within the past 3 decades, cardiovascular mortality has increased significantly2; in 2016, about every third death was caused by CVD, which amounts to an estimated 17.9 million people worldwide.1 Thus, direct and indirect economic costs caused by CVD and associated risk factors contribute to the high burden inflicted on healthcare systems.3
CVDs are mainly associated with certain predominantly modifiable risk factors. Most importantly, unhealthy eating habits leading to diabetes mellitus, obesity, hyperlipidemia, lack of physical exercise, smoking, alcohol consumption, arterial hypertension, etc, can increase the risk of developing an acute event.1, 4 Further factors associated with CVD include hereditary reasons,5 psychosocial stress, and depression.1 Also, low socioeconomic status, as defined by living environment, educational level, employment status, etc, increases cardiovascular risk.6 Although changes in lifestyle habits could positively affect up to 75% of the aforementioned CVD risk factors, disease prevalence has continued to increase1 according to the World Health Organization.7, 8
It is important to establish optimal treatment supported by international guideline recommendations.9 This would improve the patient outcomes by reducing mortality and hospitalization rates.10 The American College of Cardiology and American Heart Association regularly present updated international guidelines. Among others, these include therapeutic options, such as primary prevention via lifestyle changes and medical treatment options that offer patients the greatest benefit.8 Focusing on primary prevention, periodic control of blood sugar, cholesterol, arterial blood pressure, and anamnesis by medical practitioners is recommended.8 To maintain treatment goals, including medication and lifestyle changes, an enhanced cooperation between the various medical practitioners, patients themselves, and social surroundings can lead to the best results.11, 12
Data from the National Health Interview Survey (NHIS) show that almost 40% of United States citizens utilize complementary medicine approaches, and that medical conditions treated with such approaches include CVD risk factors such as high levels of cholesterol.13 Complementary medicine describes a combination of conventional health care and various therapies, such as yoga, mind–body medicine (MBM), traditional Chinese medicine, osteopathy, chiropractic, and many others.14 The idea of preventive and complementary medicine involves an overlap, especially with regard to lifestyle modification.15 Although use of complementary medicine approaches with conventional care appears beneficial in individuals with CVD or CVD risk factors,16, 17, 18, 19, 20, 21, 22, 23 relying solely on complementary approaches could result in poorer outcome. More specifically, complementary medicine use may be associated with lower adherence to necessary medical treatments or checkups.24
We used a large US representative data source to analyze the prevalence of conventional and complementary healthcare utilization in adults with CVD and/or CVD risk factors, and the associations between the 2 categories of health care. Specifically, we analyzed whether conventional healthcare utilization rates differ between individuals utilizing or not utilizing complementary medicine.
Methods
Study Design
We analyzed data from the 2017 NHIS. Data, methods used in the analysis, and materials used to conduct the research are available online to any researcher for purposes of reproducing the results or replicating the procedure (https://www.cdc.gov/nchs/nhis/index.htm). Conducted annually by the National Center for Health Statistics (NCHS), the NHIS is representative of the noninstitutionalized US population. In 2017, the survey included 32 617 households, and 26 742 adults provided data (response rate 80.7%). Using population‐based estimates, calculated using weights calibrated to the 2010 census population, the survey was representative for a weighted total of 246 657 271 US adults. More information on survey composition, sampling strategy, and administration of the NHIS is available from the US Centers for Disease Control and Prevention (http://www.cdc.gov/nchs/nhis/about_nhis.htm; ftp://ftp.cdc.gov/pub/health_statistics/nchs/dataset_documentation/nhis/2017/srvydesc.pdf).
The research ethics review board of the NCHS approved the NHIS data collection protocol on June 12, 2015 (Protocol #2015‐08). All participants provided informed consent.
In this analysis, we used data from the NHIS Family File, NHIS Person File, and NHIS Sample Adult File. Specifically, we extracted sociodemographic data and clinical data, including data on CVD diagnoses and CVD risk factors, as well as on conventional and complementary healthcare use.
For assessing CVD diagnoses, we analyzed self‐report data on earlier diagnoses of coronary heart disease, myocardial infarction, angina pectoris, and unspecified heart conditions. We classified participants who reported at least 1 of these diagnoses as CVD patients. Further, we analyzed self‐report data on cardiovascular risk factors, including hypertension, hypercholesterolemia, and diabetes mellitus or prediabetes mellitus. We classified participants who reported ≥1 of these risk factors as individuals with CVD risk factors; those who fell into this category but not into the CVD patient category were further classified as individuals with CVD risk factors but without a CVD diagnosis.
For healthcare utilization, we analyzed self‐reported consultations with physicians (general practitioners and/or medical specialists) and with complementary medicine practitioners (chiropractors, naturopaths, practitioners of chelation therapy, practitioners of traditional medicine, and/or homeopaths) in the past 12 months. We also analyzed the total number of consultations with any healthcare practitioners in the past 12 months and classified them as none, 1 to 3, and ≥4 office visits. We finally analyzed preventive cardiology care use, including blood pressure, cholesterol, and fasting glucose assessments, in the past 12 months, as well as MBM use, which included mantra meditation, mindfulness meditation, spiritual meditation, guided imagery, progressive relaxation, yoga, tai chi, and qi gong. We classified participants who had consulted at least 1 complementary medicine practitioner and/or utilized MBM in the past 12 months as complementary medicine users.
Statistical Analysis
We calculated the prevalence of consultations with conventional and complementary medicine practitioners as well as preventive cardiology care and MBM utilization in the past 12 months. Prevalence was calculated separately for the general population, CVD patients, and individuals with CVD risk factors but no diagnosis of a CVD, using absolute weights. Thereby, every survey participant was representative for a mean of 9223.59 individuals of the general population.
We further analyzed associations between conventional and complementary care by multiple logistic regression analyses. Because absolute weights would inflate sample size in inferential tests, the relative weights were calculated by dividing the participant's individual weight by the mean weight across the survey participants. Thus, we preserved the original sample size as well as the advantages of the NHIS complex sampling strategy. Specifically, we analyzed independent predictors of consultations with a general practitioner or medical specialist as well utilization of preventive cardiovascular care in the past 12 months. The main predictor of interest was use of complementary medicine in the past 12 months. For each conventional practitioner and preventive care type, we conducted a separate regression analysis controlling for the following potential sociodemographic and clinical confounders: age (categories 18–29, 30–39, 40–49, 50–64, and ≥65 years); ethnicity (non‐Hispanic white, Hispanic, African American, Asian, other); region (West, Northeast, Midwest, South); marital status (not in relationship, in relationship); education (less than college, some college or more); employment (employed, unemployed); health insurance coverage (coverage, no coverage); noncardiovascular comorbidities, including: (1) previous diagnoses of stroke, emphysema, chronic obstructive disease, asthma, ulcer, epilepsy, hay fever, sinusitis, bronchitis, kidney disease, liver disease, and arthritis; (2) neck, back, facial pain, or headache in the past 3 months; and (3) head or chest cold, stomach problems, diarrhea, or vomiting in the past 2 weeks, and the CVD risk factors hypertension, hypercholesterinemia, and diabetes mellitus/prediabetes mellitus (yes, no). Analyses of CVD patients also controlled for the specific type of CVD diagnoses, including coronary heart disease, myocardial infarction, angina pectoris, unspecified heart conditions, and stroke (previous diagnosis, no previous diagnosis). Only those potential confounders associated with the respective dependent variable with P≤0.10 on univariate analysis (chi‐square test) were included in the regression analyses. We computed adjusted odds ratio with 95% CI and considered P≤0.05 to be statistically significant in the regression analysis. All statistical analyses were performed using SPSS Statistics for Windows release 25.0 (IBM Corp, Armonk, NY).
Results
A weighted total of 93 943 190 (38.1%) participants reported risk factors for CVD and 28 214 424 participants (11.4%) had received a CVD diagnosis, with a large overlap between the 2 groups. A total of 74 449 360 (30.2%) participants reported CVD risk factors but no diagnosis of CVD. Demographics and clinical characteristics of patients with CVD and/or risk factors for CVD are reported in Table 1.
Table 1.
Demographic and Clinical Characteristics of Adults With CVD or CVD Risk Factors But No Manifest CVD
| Characteristics | CVD Patients (n=28 214 424) | Individuals With CVD Risk Factors (n=74 418 456) |
|---|---|---|
| Age, y | ||
| 18 to 29 | 4 655 577 (16.5%) | 11 868 557 (15.9%) |
| 30 to 39 | 4 673 002 (16.6%) | 11 285 140 (15.2%) |
| 40 to 49 | 4 016 159 (14.2%) | 11 286 622 (15.2%) |
| 50 to 64 | 7 162 018 (25.4%) | 19 723 779 (26.5%) |
| 65 | 7 707 668 (27.3%) | 20 254 358 (27.2%) |
| Sex | ||
| Male | 14 854 519 (52.6%) | 34 833 855 (46.8%) |
| Female | 13 359 905 (47.4%) | 39 584 601 (53.2%) |
| Ethnicity | ||
| Non‐Hispanic white | 20 349 434 (72.1%) | 52 311 462 (70.3%) |
| Hispanic | 3 145 412 (11.1%) | 9 125 269 (12.3%) |
| Black | 3 064 952 (10.9%) | 7 937 718 (10.7%) |
| Asian | 1 353 923 (4.8%) | 4 034 139 (5.4%) |
| Other | 300 703 (1.1%) | 1 009 868 (1.4%) |
| Region | ||
| West | 5 763 735 (20.4%) | 17 383 022 (23.4%) |
| Northeast | 5 114 419 (18.1%) | 13 406 517 (18.0%) |
| Midwest | 7 074 651 (25.1%) | 15 050 514 (20.2%) |
| South | 10 261 619 (36.4%) | 28 578 403 (38.4%) |
| Employment | ||
| Not employed | 18 088 329 (64.2%) | 34 110 618 (45.8%) |
| Employed | 10 106 002 (35.8%) | 40 305 268 (54.2%) |
| Education | ||
| Less than college | 14 854 519 (52.6%) | 34 833 855 (46.8%) |
| Some college or more | 13 359 905 (47.4%) | 39 584 601 (53.2%) |
| Marital status | ||
| Not in a relationship | 11 440 946 (40.6%) | 26 864 436 (36.2%) |
| In a relationship | 16 743 167 (59.4%) | 47 416 355 (63.8%) |
| Health insurance | ||
| Yes | 26 839 475 (95.1%) | 69 360 825 (93.2%) |
| No | 1 374 949 (4.9%) | 5 057 631 (6.8%) |
| CVDa | ||
| Coronary heart disease | 10 768 994 (38.2%) | … |
| Myocardial infarction | 7 583 582 (26.9%) | … |
| Angina pectoris | 4 402 727 (15.6%) | … |
| Heart condition, unspecified | 19 013 402 (67.4%) | … |
| CVD risk factora | ||
| Hypertension | 14 351 327 (50.9%) | 41 717 225 (56.1%) |
| Hypercholesterinemia | 11,107,136 (39.4%) | 37 082 840 (49.8%) |
| Diabetes mellitus/prediabetes mellitus | 9 589 248 (34.0%) | 32 221 417 (43.3%) |
Data expressed as weighted frequencies. CVD indicates cardiovascular disease.
Sums to >100% because multiple diagnoses were possible.
Adults with CVD risk factors but without CVD diagnosis had a higher prevalence of consultation with general practitioners and medical specialists than the general population, and CVD patients had higher prevalence of consultations than the general population and individuals with CVD risk factors but no manifest CVD (Figure 1). The same was true for consultations with complementary medicine practitioners except for consultations with chelation therapy practitioners and homeopaths (Figure 1). Among individuals with CVD risk factors but no manifest CVD, 92.5% had consulted healthcare practitioners at least once in the past 12 months, and 49.5% had ≥4 office visits. Among CVD patients, 92.6% had consulted healthcare practitioners at least once in the past 12 months, 60.4% had ≥4 office visits in the past 12 months. Prevalence of preventive cardiovascular care is shown in Figure 2.
Figure 1. Twelve‐month prevalence of consultations with conventional and complementary medicine practitioners in: (1) the general adult population; (2) adults with cardiovascular disease (CVD); or (3) adults with CVD risk factors but no manifest CVD.
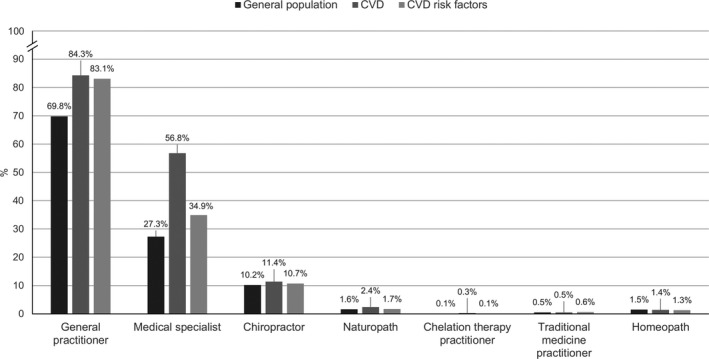
Weighted frequencies were used.
Figure 2. Twelve‐month prevalence of preventive cardiovascular care in: (1) the general adult population; (2) adults with cardiovascular disease (CVD); or (3) adults with CVD risk factors but no manifest CVD.
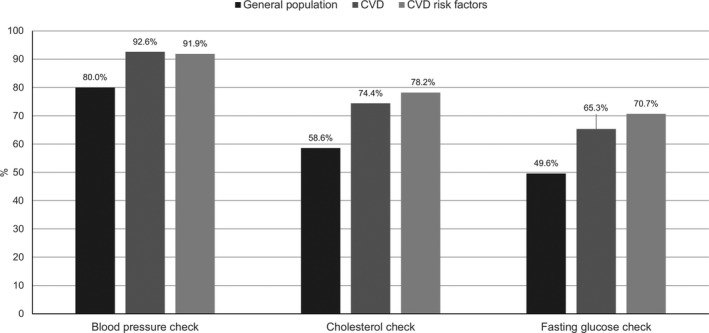
Weighted frequencies were used.
In addition, 23.6% of the general population, 22.8% of CVD patients, and 21.1% of individuals with CVD risk factors, but no manifest CVD used MBM, with yoga and spiritual meditation being the most commonly used mind–body modalities (Figure 3).
Figure 3. Twelve‐month prevalence of mind–body medicine use in: (1) the general adult population; (2) adults with cardiovascular disease (CVD); or (3) adults with CVD risk factors but no manifest CVD.
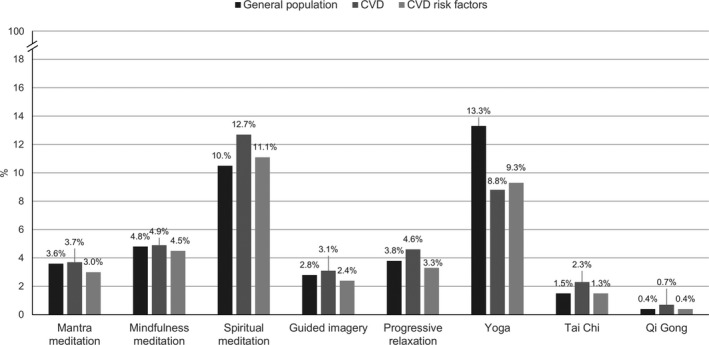
Weighted frequencies were used.
Altogether, 31.2% of the general population, 31.8% of CVD patients, and 29.7% of individuals with CVD risk factors, but no manifest CVD had used any form of complementary medicine.
Conventional and complementary medicine use were associated with each other among CVD patients and even more pronounced in individuals with CVD risk factors but no manifest CVD. In the latter group, individuals using complementary medicine significantly more often also consulted general practitioners and medical specialists compared with those not using complementary medicine. Patients with manifest CVD using complementary medicine also more often consulted medical specialists (but not general practitioners) than patients not using complementary medicine (Table 2). More individuals using complementary medicine also attended blood pressure and fasting glucose checkups in the previous 12 months than those not using complementary medicine, but these differences did not reach statistical significance (Table 2).
Table 2.
Associations of Consultations With CM Providers and Conventional Healthcare Utilization in Adults With CVD or CVD Risk Factors But No Manifest CVD
| CVD Patients Using CM | Individuals With CVD Risk Factors Using CM | |||||
|---|---|---|---|---|---|---|
| OR (95% CI) | Adjusted OR (95% CI) | P Value | OR (95% CI) | Adjusted OR (95% CI) | P Value | |
| Physician consultations past 12 months | ||||||
| General physician consultation | 1.09 (0.88–1.34) | 1.17 (0.93–1.47) | 0.18 | 1.28 (1.13–1.47) | 1.21 (1.05–1.39) | <0.01 |
| Medical specialist consultation | 1.25 (1.07–1.46) | 1.38 (1.17–1.64) | <0.01 | 1.50 (1.36–1.66) | 1.42 (1.28–1.58) | <0.01 |
| Preventive care past 12 months | ||||||
| Blood pressure check | 1.04 (0.78–1.40) | 1.13 (0.82–1.55) | 0.47 | 1.12 (0.94–1.34) | 1.10 (0.91–1.32) | 0.33 |
| Cholesterol check | 0.79 (0.67–0.94) | 0.98 (0.81–1.12) | 0.87 | 0.89 (0.80–1.00) | 0.96 (0.85–1.08) | 0.51 |
| Fasting glucose check | 1.00 (0.85–1.17) | 1.15 (0.96–1.37) | 0.13 | 1.10 (0.99–1.23) | 1.09 (0.97–1.22) | 0.14 |
Odds ratio >1 indicate higher utilization in individuals using CM; odds ratio <1 indicates higher utilization in individuals not using CM. Adjusted odds ratio and P‐values were derived from logistic regression analyses controlling for age, sex, education, employment, marital status, region of origin, race/ethnicity, health insurance coverage, noncardiovascular comorbidities, CVD risk factors, and CVD type (CVD patients only). Relative weights were used. CM indicates complementary medicine; CVD, cardiovascular disease; and OR, odds ratio.
Discussion
In this study we have reported on the association of complementary medicine use and use of general and complementary health care among US citizens with CVD and/or CVD risk factors. Individuals with CVD or CVD risk factors who utilized complementary medicine health care were as likely, or even more likely, to consult general medical practitioners and specialists, and to adhere to necessary checkups, compared with those who did not.
The general use of complementary health care in CVD as seen in our data is comparable with that seen in earlier studies. In 2012, a systematic review analyzed 27 studies—primarily data from the United States, Canada, and the United Kingdom. The results showed that use of complementary health care in CVD is common, although variable. The general prevalence of conventional medicine use ranged from 4% to 61%, respectively, and from 19% to 64% when only studies with comprehensive definitions of conventional and alternative medicine were included. Data among types of complementary healthcare utilization and reasons for it varied. Reasons mentioned included: belief of greater benefit vs. conventional therapy; treatment of adverse drug reactions to conventional medication; or treatment of a manifest CVD. In manifest heart failure, 7% to 82% of patients utilized complementary medicine to treat their condition.25 Furthermore, in 2007, the NHIS already showed that people with CVD or CVD risk factors were more likely to use complementary medicine than the general population.26
Although this is the first US nationally representative analysis to show a positive relationship between complementary and conventional healthcare utilization in individuals with CVD or CVD risk factors, our findings are in line with earlier work from other countries. In 2013, Canaway et al conducted a survey of 2766 Australian patients with diabetes mellitus and/or CVD. Participants were asked about their use of general health services and use of complementary medicine, defined as supplement use and consultations with complementary healthcare practitioners, within the past 12 months. Complementary healthcare users had a significantly higher number of general or specified medical practitioner consultations than nonusers.27 Analogous retrospective data among patients with diabetes mellitus treated in the Bastyr Center for Natural Health were analyzed and published in 2006. The analysis showed that naturopathic and conventional care were typically jointly used.28
Other studies also showed a general connection between the utilization of complementary and conventional healthcare utilization in other patient populations. According to Reid et al,29 complementary medicine users in Australia tend to use conventional medical care more often. Although there are many reasons for use of complementary medicine, chronic illnesses are a major reason according to data from Australia, Canada, and the United States.29, 30, 31 Chronic illnesses treated with complementary medicine include chronic pain, depression, and CVD,13 although only 10% of patients used complementary approaches for direct treatment of their CVD.32 Some data suggest that CVD patients utilizing complementary methods suffer from poorer health conditions33 and a lower quality of life29 when compared with nonusers. A poorer health condition may derive from a higher rate of chronic comorbidities such as anxiety, pain disorders, insomnia, or others,26, 27 and not the CVD itself. Predictive factors for complementary healthcare utilization in general and specifically in CVDs are female sex, middle‐age, higher educational level and income,13, 27, 34 and greater health literacy.35 Because health literacy is also associated with a higher utilization of conventional health care, it may be relevant for the positive association between conventional and complementary healthcare utilization.36, 37 Future studies could further target this association.
There are limitations to our findings. The NHIS survey is an annual cross‐sectional survey. Although our analysis showed a positive relationship between use of complementary and conventional health care, there is no evidence for a causal relationship between the 2 types of healthcare use. In addition, the survey contains self‐reported data from noninstitutionalized US citizens. As diagnoses and healthcare utilization could not be cross‐validated from medical records, respondents may tend to answer in a way that makes a good impression on the researcher. Respondents may also show misclassification or recall bias. Also, in the 2012 NHIS, there were no queries about reasons for consulting a specific practitioner. Thus, we could not assess the exact reason for healthcare utilization. In 2017, the NHIS only assessed a limited number of complementary therapies. Commonly used approaches, such as consultations with acupuncturists or use of supplements, were not assessed. Likewise, only a limited number of noncardiovascular comorbidities could be included in the analyses.
In individuals with CVD or CVD risk factors, complementary healthcare utilization is highly prevalent, as shown in our results. It also seems that individuals utilizing complementary health care also tend to consult more frequently with general medical practitioners. Referring to the American Heart Association guidelines, studies showed that team‐based treatment for patients improves the benefit and outcome of lifestyle change in patients with CVD. In addition to receiving support from the family, this also includes seeking care from different healthcare professions.8 Although the American Heart Association guideline addresses consultation with general clinical institutions, our data show that complementary care may be supportive as well. Further investigation will be needed.
Conclusions
Both conventional and complementary health care are used commonly among individuals with or at risk for CVD. Individuals with CVD or CVD risk factors consulting complementary medicine practitioners and/or using MBM more likely consult general medical practitioners as well. In manifest CVDs, significantly more patients tend to consult medical specialists when using complementary medicine than nonusers. More individuals using complementary medicine also tend to adhere to recommended checkups. Thus, our data are not compatible with a hypothesized negative association of complementary healthcare utilization and nonadherence to conventional therapy and diagnostics in individuals with or at risk for CVD. The potential positive association of complementary and conventional utilization of health care needs to be confirmed in further studies.
Sources of Funding
H.C. was supported by the Erich Ruthenfußer Stiftung.
Disclosures
None.
(J Am Heart Assoc. 2020;9:e014759 DOI: 10.1161/JAHA.119.014759.)
For Sources of Funding and Disclosures, see page 7.
References
- 1. World Health Organisation . Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and Region, 2000–2016. Geneva, Switzerland: WHO; 2018. [Google Scholar]
- 2. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. Executive summary: Heart Disease and Stroke Statistics—2013 Update: a Report from the American Heart Association. Circulation. 2013;127:143–152. [DOI] [PubMed] [Google Scholar]
- 3. Tarride JE, Lim M, DesMeules M, Luo W, Burke N, O'Reilly D, Bowen J, Goeree R. A review of the cost of cardiovascular disease. Can J Cardiol. 2009;25:e195–e202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gyárfás I, Keltai M, Salim Y. [Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries in a case‐control study based on the INTERHEART study]. Orv Hetil. 2006;147:675–686. [PubMed] [Google Scholar]
- 5. Lali R, Cui E, Ansarikaleibari A, Pigeyre M, Paré G. Genetics of early‐onset coronary artery disease: from discovery to clinical translation. Curr Opin Cardiol. 2019;34:706–713. [DOI] [PubMed] [Google Scholar]
- 6. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137:2166–2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren WM, Albus C, Benlian P, Boysen G, Cifkova R, et al. [European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts)]. G Ital Cardiol (Rome). 2013;14:328–392. [DOI] [PubMed] [Google Scholar]
- 8. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd‐Jones D, McEvoy JW, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:1376–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Komajda M, Cowie MR, Tavazzi L, Ponikowski P, Anker SD, Filippatos GS; QUALIFY Investigators . Physicians’ guideline adherence is associated with better prognosis in outpatients with heart failure with reduced ejection fraction: the QUALIFY international registry. Eur J Heart Fail. 2017;19:1414–1423. [DOI] [PubMed] [Google Scholar]
- 10. Shah BR, O'Brien EC, Roe MT, Chen AY, Peterson ED. The association of in‐hospital guideline adherence and longitudinal postdischarge mortality in older patients with non‐ST‐segment elevation myocardial infarction. Am Heart J. 2015;170:273–280.e1. [DOI] [PubMed] [Google Scholar]
- 11. Mitchell P, Wynia M, Golden R, McNellis B, Okun S, Webb CE, Rohrbach V, Von Johorn I. Core principles and values of effective team‐based health care. Discussion Paper. Washington, DC: Institute of Medicine; 2012. [Google Scholar]
- 12. Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, Owens DK, Goldstein MK. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–657. [DOI] [PubMed] [Google Scholar]
- 13. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 14. Jonas WB, Eisenberg D, Hufford D, Crawford C. The evolution of complementary and alternative medicine (CAM) in the USA over the last 20 years. Forsch Komplementmed. 2013;20:65–72. [DOI] [PubMed] [Google Scholar]
- 15. Ali A, Katz DL. Disease prevention and health promotion: how integrative medicine fits. Am J Prev Med. 2015;49:S230–S240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cramer H, Lauche R, Haller H, Dobos G, Michalsen A. A systematic review of yoga for heart disease. Eur J Prev Cardiol. 2015;22:284–295. [DOI] [PubMed] [Google Scholar]
- 17. Cramer H, Lauche R, Paul A, Langhorst J, Michalsen A, Dobos G. Mind‐body medicine in the secondary prevention of coronary heart disease. Dtsch Arztebl Int. 2015;112:759–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alenazi AM, Alshehri MM, Hoover JC, Yabroudi MA, Kachanathu SJ, Liu W. The effect of T'ai Chi exercise on lipid profiles: a systematic review and meta‐analysis of randomized clinical trials. J Altern Complement Med. 2018;24:220–230. [DOI] [PubMed] [Google Scholar]
- 19. Ursoniu S, Sahebkar A, Andrica F, Serban C, Banach M; Lipid and Blood Pressure Meta‐analysis Collaboration (LBPMC) Group . Effects of flaxseed supplements on blood pressure: a systematic review and meta‐analysis of controlled clinical trial. Clin Nutr. 2016;35:615–625. [DOI] [PubMed] [Google Scholar]
- 20. Serban C, Sahebkar A, Ursoniu S, Andrica F, Banach M. Effect of sour tea (Hibiscus sabdariffa L.) on arterial hypertension: a systematic review and meta‐analysis of randomized controlled trials. J Hypertens. 2015;33:1119–1127. [DOI] [PubMed] [Google Scholar]
- 21. Jayawardena R, Ranasinghe P, Chathuranga T, Atapattu PM, Misra A. The benefits of yoga practice compared to physical exercise in the management of type 2 diabetes mellitus: a systematic review and meta‐analysis. Diabetes Metab Syndr. 2018;12:795–805. [DOI] [PubMed] [Google Scholar]
- 22. Meng D, Chunyan W, Xiaosheng D, Xiangren Y. The effects of Qigong on type 2 diabetes mellitus: a systematic review and meta‐analysis. Evid Based Complement Alternat Med. 2018;2018:8182938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Michalsen A, Li C. Fasting therapy for treating and preventing disease—current state of evidence. Forsch Komplementmed. 2013;20:444–453. [DOI] [PubMed] [Google Scholar]
- 24. Dal Corso E, Bondiani AL, Zanolla L, Vassanelli C. Nurse educational activity on non‐prescription therapies in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2007;6:314–320. [DOI] [PubMed] [Google Scholar]
- 25. Grant SJ, Bin YS, Kiat H, Chang DH. The use of complementary and alternative medicine by people with cardiovascular disease: a systematic review. BMC Public Health. 2012;12:299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Anderson JG, Taylor AG. Use of complementary therapies by individuals with or at risk for cardiovascular disease: results of the 2007 National Health Interview Survey. J Cardiovasc Nurs. 2012;27:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Canaway R, Manderson L. Quality of life, perceptions of health and illness, and complementary therapy use among people with type 2 diabetes and cardiovascular disease. J Altern Complement Med. 2013;19:882–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bradley R, Oberg EB. Naturopathic medicine and type 2 diabetes: a retrospective analysis from an academic clinic. Altern Med Rev. 2006;11:30–39. [PMC free article] [PubMed] [Google Scholar]
- 29. Reid R, Steel A, Wardle J, Trubody A, Adams J. Complementary medicine use by the Australian population: a critical mixed studies systematic review of utilisation, perceptions and factors associated with use. BMC Complement Altern Med. 2016;16:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Metcalfe A, Williams J, McChesney J, Patten SB, Jetté N. Use of complementary and alternative medicine by those with a chronic disease and the general population―results of a national population based survey. BMC Complement Altern Med. 2010;10:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Saydah SH, Eberhardt MS. Use of complementary and alternative medicine among adults with chronic diseases: United States 2002. J Altern Complement Med. 2006;12:805–812. [DOI] [PubMed] [Google Scholar]
- 32. Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006;98:673–680. [DOI] [PubMed] [Google Scholar]
- 33. Rhee TG, Westberg SM, Harris IM. Complementary and alternative medicine in US adults with diabetes: reasons for use and perceived benefits. J Diabetes. 2018;10:310–319. [DOI] [PubMed] [Google Scholar]
- 34. Egede LE, Ye X, Zheng D, Silverstein MD. The prevalence and pattern of complementary and alternative medicine use in individuals with diabetes. Diabetes Care. 2002;25:324–329. [DOI] [PubMed] [Google Scholar]
- 35. Bains SS, Egede LE. Association of health literacy with complementary and alternative medicine use: a cross‐sectional study in adult primary care patients. BMC Complement Altern Med. 2011;11:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhang NJ, Terry A, McHorney CA. Impact of health literacy on medication adherence: a systematic review and meta‐analysis. Ann Pharmacother. 2014;48:741–751. [DOI] [PubMed] [Google Scholar]
- 37. Rolls CA, Obamiro KO, Chalmers L, Bereznicki LRE. The relationship between knowledge, health literacy, and adherence among patients taking oral anticoagulants for stroke thromboprophylaxis in atrial fibrillation. Cardiovasc Ther. 2017;35:e12304 DOI: 10.1111/1755-5922.12304. [DOI] [PubMed] [Google Scholar]


