Abstract
Background
Previous reports have described a leveling off of mortality from premature coronary artery disease (CAD). In recent years, the prevalence of cardiovascular risk factors has increased in rural communities and young adults.
Methods and Results
We extracted CAD mortality rates from the Centers for Disease Control and Prevention Wide‐Ranging Online Data for Epidemiologic Research (CDC WONDER) database from 1999 to 2017, focusing on mortality from premature CAD (defined as <65 years of age in women) and urban–rural differences. Variations in mortality rates over time, assessed with Joinpoint regression modeling, are expressed as estimated annual percentage change (95% CI) and stratified by urbanization, sex, age, and race. Age‐adjusted mortality rates decreased for women and men. Stratification by urbanization revealed that premature CAD mortality is stagnating among women in rural areas. However, this stagnation conceals a statistically significant increase in CAD mortality rates since 2009 in women aged 55 to 64 years (estimated annual percentage change: +1.4%; 95% CI, +0.3% to +2.5%) and since 1999 in women aged 45 to 54 years (estimated annual percentage change: +0.6%; 95% CI, +0.2% to 1.0%). Since 1999, mortality has been stagnating in the youngest group (aged 35–44 years; estimated annual percentage change: +0.2%; 95% CI, −0.4% to +0.8%). Stratification by race indicated an increase in mortality rates among white rural women. Premature CAD mortality remains consistently higher in the rural versus urban United States, regardless of sex, race, and age group.
Conclusions
Premature CAD mortality rates have declined over time. However, stratification by sex and urbanization reveals disparities that would otherwise remain concealed: CAD mortality rates have increased among women from rural areas since at least 2009.
Keywords: epidemiology, gender, mortality, premature coronary artery disease, race, rural
Subject Categories: Cardiovascular Disease, Epidemiology, Women, Coronary Artery Disease
Clinical Perspective
What Is New?
We analyzed trends in mortality rates from premature coronary artery disease (CAD) in the United States from 1999 to 2017.
After stratification by sex and urbanization, an increase in CAD mortality was found among women residing in the rural United States.
Women in urban areas and men (in urban and rural areas) showed opposite trends.
What Are the Clinical Implications?
These findings call for an intensification of public health efforts regarding cardiovascular risk factor awareness, assessment, and control, especially for young women in rural communities.
Because premature CAD is a result of exposure to cardiovascular risk factors during adolescence and early adulthood, one wonders if efforts for primary and secondary prevention are enough or if a focus on primordial prevention is necessary.
Nonstandard Abbreviations and Acronyms
- CAD
coronary artery disease
- CDC
Center of Disease Control and Prevention
- EAPC
estimated annual percent shange
Introduction
Coronary artery disease (CAD) remains the leading cause of death in the United States despite considerable reductions in mortality over the past several decades. These trends have been attributed to improved primary and secondary prevention efforts and advances in diagnosis and treatment of CAD. However, recent reports have suggested a leveling off of CAD mortality rates, especially in young individuals, including women.1, 2 People residing in rural US communities appear to be disproportionately affected by these trends.3 The population count in rural communities is roughly 60 million (about 20% of the US population).4 This segment of the population is experiencing increasing disparity in prevalence of cardiovascular risk factors compared with urban counterparts.5, 6 The burden of cardiovascular risk factors among young adults is growing.7 Furthermore, rising hospitalization rates for myocardial infarction (MI) in young women have been reported recently.8
Taken together, these recent reports raise the suspicion that CAD mortality rates in young individuals, especially young women, and in residents of rural communities may have been negatively affected even further in recent years. Limited data are available about recent trends in CAD mortality in these populations. Recognizing urban–rural differences has important implications for optimization and allocation of healthcare resources and prevention programs.
We sought to analyze the most recent mortality rates from premature CAD, defined by the American College of Cardiologists and the American Heart Association as <65 years of age in women and <55 years in men,9 stratified by urbanization, age, sex, and race.
Methods
Anonymized data and materials are available at Centers for Disease Control and Prevention Wide‐Ranging Online Data for Epidemiologic Research (CDC WONDER) and can be accessed at (https://wonder.cdc.gov/). The statistical program Joinpoint is also freely available from the National Institutes of Health (https://surveillance.cancer.gov/joinpoint/download).
We extracted CAD mortality rates from the multiple‐cause‐of‐death files of CDC WONDER from 1999 to 2017. This publicly accessible database provides mortality data on the US population collected by state registries and entered into the National Vital Statistics System. Demographic data and underlying cause of death are indicated on death certificates. Institutional review board approval was waived because all data are deidentified and publicly available.
CAD was defined as International Classification of Diseases, Tenth Revision (ICD‐10) codes I20–I25. We focused on mortality from premature CAD (defined as <65 years of age in women9) and in three 10‐year age strata (35–44, 45–54, and 55–64 years). Premature CAD in men is defined as <55 years of age; the stratum of men aged 55 to 64 years is reported for comparison purposes.9
Age‐adjusted mortality rates were calculated with the 2000 US Census as the default population. We further stratified mortality by sex and urbanization (metropolitan, medium‐small towns, rural). This represents a condensed version of the 2013 National Center for Health Statistics (NCHS) Urban–Rural Classification Scheme used by the CDC10: “metro” (large central metro plus large fringe metro), “med‐small” (medium metro plus small metro), “rural” (micropolitan plus noncore). We stratified by race according to the categories provided by CDC WONDER: “black or African American” and “white.” The category “Hispanic origin” was not analyzed to avoid bias, as Hispanic ethnicity is likely to be misclassified on death certificates.11 The analysis was confined to the 1999–2017 period because urbanization data are not available before 1999 and 2017 represents the latest available data.
The Joinpoint software (v4.5.0.1; National Cancer Institute) was used to assess variations in the estimated annual percentage change (EAPC). EAPC represents the change in mortality occurring during a certain time period, expressed as a percentage and averaged over the specified time period; for example, if mortality increases by 7% during a 10‐year period, the EAPC for that period is +0.7%. Joinpoint uses a Monte Carlo permutation test to identify time points (“joinpoints”) where the trend, or magnitude of the trend, changes significantly from the preceding one (using a t test), then fitting the simplest model by applying the smallest number of trend segments, referred to as “period” in this article. An EAPC and 95% CI are calculated for each period.
We assumed a Poisson distribution (events occur randomly and independently), and a maximum of 3 joinpoints were prespecified (fewer joinpoints might conceal a change in trend, whereas >3 were unnecessary because they did not reveal additional inflection points in exploratory analyses). This method is commonly used to minimize bias when assessing trends in incidence or mortality rates.1, 2, 12 A P value <0.05 was considered statistically significant.
Results
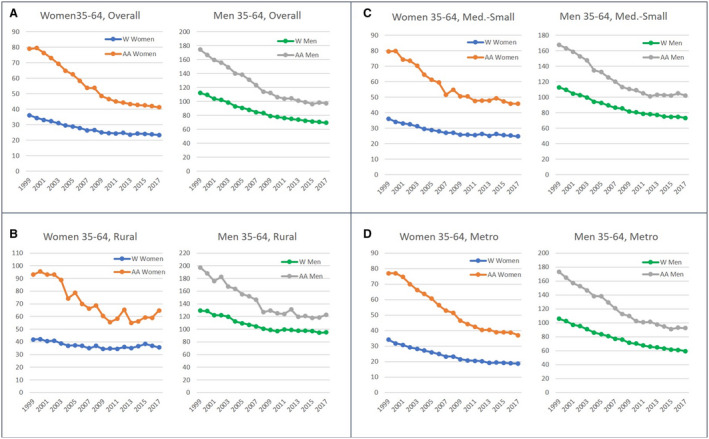
Age‐adjusted mortality from premature CAD has been decreasing at similar rates for men and women, slowing down after 2010. This decrease is more pronounced in women (EAPC: −0.8%; 95% CI, −1.3% to −0.3%) versus men (EAPC: −1.5%; 95% CI, −1.8% to −1.2%), highlighted in Figure 1 and Table 1. When stratified by urbanization, stagnation is evident among women in the rural and medium‐small town groups (since 1999 and 2009, respectively). Further stratification by age shows that stagnation in mortality rates for rural women conceals an increase in CAD mortality rates in 55‐ to 64‐year‐olds (EAPC: +1.4%; 95% CI, +0.2% to +2.5%) since 2010 and in the 45‐ to 54‐year‐old group, uninterrupted since 1999 (EAPC: +0.6%; 95% CI, +0.2% to +1.0%). The youngest group (aged 35–44 years) of rural women experienced a stagnation in mortality rate for the entire period (EAPC: +0.2%; 95% CI, −0.4% to +0.8%), as displayed in Table 2 and Figure 2. The stagnation in age‐adjusted mortality rates seen in medium‐small towns is driven since 2008 by stagnation in the group aged 55 to 64 years (EAPC: −0.5%; 95% CI, −0.9% to 0.0%; Figure 2 and Table 2.
Figure 1.
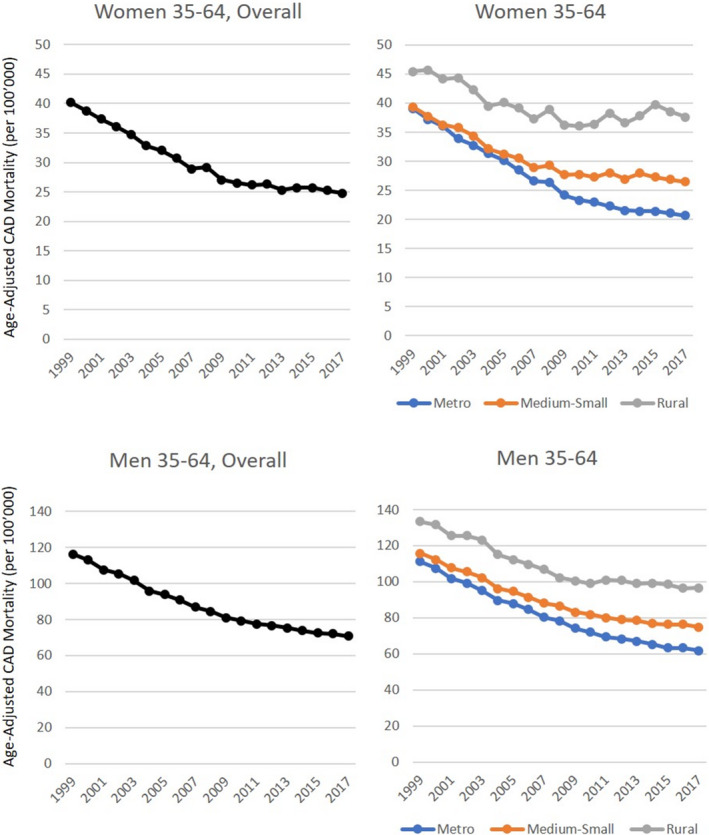
Age‐adjusted mortality from premature CAD in 35‐ to 64 year‐olds by sex and urbanization.
Detailed data are presented in Table 1. CAD indicates coronary artery disease.
Table 1.
Age‐Adjusted Mortality From Premature CAD in People Aged 35 to 64 Years, Stratified by Sex and Urbanization
| Urbanization Area | Period, y | EAPC | 95% CI | Note | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Women | |||||
| All regions | 1999–2010 | −3.8a | −4.0 | −3.5 | … |
| 2010–2017 | −0.8a | −1.3 | −0.3 | … | |
| Metro | 1999–2011 | −4.5a | −4.7 | −4.3 | … |
| 2011–2017 | −1.4a | −2.1 | −0.8 | … | |
| Medium‐Small | 1999–2009 | −3.4a | −3.8 | −3.0 | … |
| 2009–2017 | −0.3b | −0.9b | 0.2b | Stagnationb | |
| Rural | 1999–2009 | −2.4a | −3.0 | −1.8 | … |
| 2009–2017 | 0.8b | −0.1b | 1.7b | Stagnationb | |
| Men | |||||
| All regions | 1999–2010 | −3.5a | −3.6 | −3.4 | … |
| 2010–2017 | −1.5a | −1.8 | −1.2 | … | |
| Metro | 1999–2011 | −3.9a | −4.0 | −3.7 | … |
| 2011–2017 | −1.9a | −2.3 | −1.5 | … | |
| Medium‐Small | 1999–2009 | −3.3a | −3.5 | −3.1 | … |
| 2009–2017 | −1.3a | −1.5 | −1.0 | … | |
| Rural | 1999–2008 | −2.9a | −3.2 | −2.6 | … |
| 2008–2017 | −0.4b | −0.9b | 0.0b | Stagnationb | |
Results from statistical analysis (Joinpoint software). CAD indicates coronary artery disease; and EAPC, estimated annual percentage change.
P<0.05.
EAPCs relevant for the discussion.
Table 2.
Age‐Specific Mortality From Premature CAD by Sex, Age Group, and Urbanization
| Urbanization Area | Period, y | EAPC | 95% CI | Note | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Women | |||||
| 35–44 y | |||||
| Metro | 1999–2004 | 0.9 | −0.8 | 2.6 | … |
| 2004–2007 | −9.3 | −16.4 | −1.5 | … | |
| 2007–2017 | −1.5a | −2.2 | −0.8 | … | |
| Medium‐Small | 1999–2002 | 4.3 | −2.9 | 12.0 | … |
| 2002–2017 | −2.1a | −2.7 | −1.4 | … | |
| Rural | 1999–2017 | 0.2b | −0.4b | 0.8b | Stagnationb |
| 45–54 y | |||||
| Metro | 1999–2006 | −2.3a | −2.9 | −1.7 | … |
| 2006–2010 | −4.6a | −6.8 | −2.4 | … | |
| 2010–2017 | −2.0a | −2.7 | −1.4 | … | |
| Medium‐Small | 1999–2017 | −0.7a | −1.0 | −0.5 | … |
| Rural | 1999–2017 | 0.6a , b | 0.2b | 1.0b | Significant increaseb |
| 55–64 y | |||||
| Metro | 1999–2010 | −5.5a | −5.8 | −5.1 | … |
| 2010–2017 | −1.6a | −2.3 | −0.8 | … | |
| Medium‐Small | 1999–2008 | −5.3a | −5.8 | −4.9 | … |
| 2008–2017 | −0.5b | −0.9b | 0.0b | Stagnationb | |
| Rural | 1999–2010 | −4.1a | −4.7 | −3.5 | … |
| 2010–2017 | 1.4a , b | 0.3b | 2.5b | Significant increaseb | |
| Men | |||||
| 35–44 y | |||||
| Metro | 1999–2017 | −3.2a | −3.4 | −2.9 | … |
| Medium‐Small | 1999–2003 | 0.1 | −2.1 | 2.3 | … |
| 2003–2017 | −3.0a | −3.3 | −2.6 | … | |
| Rural | 1999–2003 | 3.1a | 1.1 | 5.1 | … |
| 2003–2009 | −4.7a | −6.1 | −3.4 | … | |
| 2009–2012 | 2.3 | −4.8 | 9.9 | … | |
| 2012–2017 | −3.3a | −4.9 | −1.6 | … | |
| 45–54 y | |||||
| Metro | 1999–2006 | −2.9a | −3.3 | −2.5 | … |
| 2006–2009 | −4.5a | −7.6 | −1.3 | … | |
| 2009–2017 | −2.8a | −3.2 | −2.5 | … | |
| Medium‐Small | 1999–2017 | −2.2a | −2.3 | −2.0 | … |
| Rural | 1999–2017 | −1.4a | −1.5 | −1.2 | … |
| 55–64 y | |||||
| Metro | 1999–2004 | −5.0a | −5.6 | −4.3 | … |
| 2004–2011 | −3.8a | −4.3 | −3.3 | … | |
| 2011–2017 | −1.4a | −1.9 | −0.9 | … | |
| Medium‐Small | 1999–2006 | −4.7a | −5.0 | −4.4 | … |
| 2006–2011 | −2.4a | −3.1 | −1.7 | … | |
| 2011–2017 | −0.3b | −0.7b | 0.1b | Stagnationb | |
| Rural | 1999–2008 | −4.2a | −4.6 | −3.9 | … |
| 2008–2017 | 0.0b | −0.4b | 0.3b | Stagnationb | |
Results from statistical analysis (Joinpoint software). CAD indicates coronary artery disease; and EAPC, estimated annual percentage change.
P<0.05.
EAPCs relevant for the discussion results from the statistical analysis.
Figure 2.
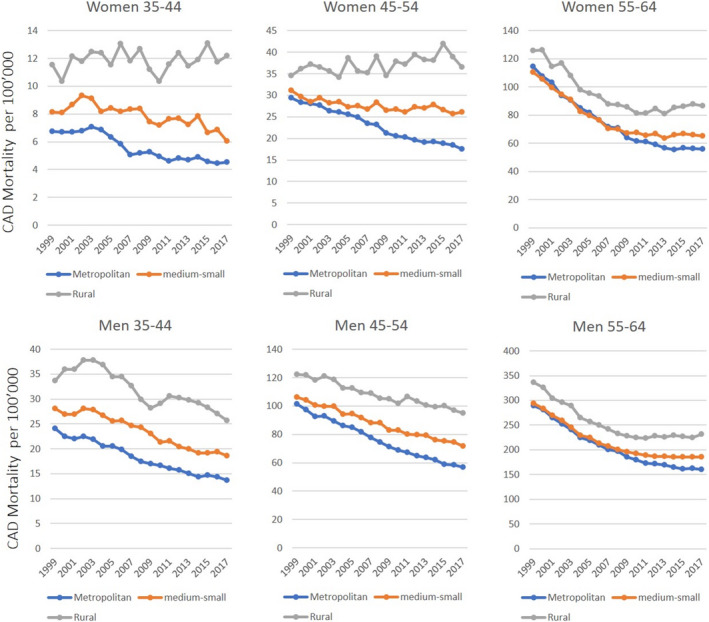
Age‐specific mortality from premature CAD according to age groups, sex, and urbanization.
Detailed data are presented in Table 2. CAD indicates coronary artery disease.
In men, the age‐adjusted mortality rates revealed stagnation in rural areas from 2008 onward (EAPC: −0.4%; 95% CI, −0.9% to 0.0%: Figure 1 and Table 1. This finding was driven by stagnation among the 55‐ to 64‐year‐olds since 2008 (EAPC: 0.0%; 95% CI, −0.4 to +0.3%). In addition, this same age group witnessed stagnation of mortality rates in medium‐small towns from 2011 (EAPC: −0.3%; 95% CI, −0.7 to +0.1%; Figure 2 and Table 2. Although the age cutoff for the premature CAD definition in men is <55 years, the group aged 55 to 64 years is reported for comparison.
When the analysis was not limited to the premature CAD age range but included ages ≥35 years, the disparities and the increase in CAD mortality rate remained concealed (Figure 3 and Table 3). This was related to the relatively high number of deaths from CAD in the group aged >65 years. Mortality rates with a uniform scale are shown in Figure 4 for comparison.
Figure 3.
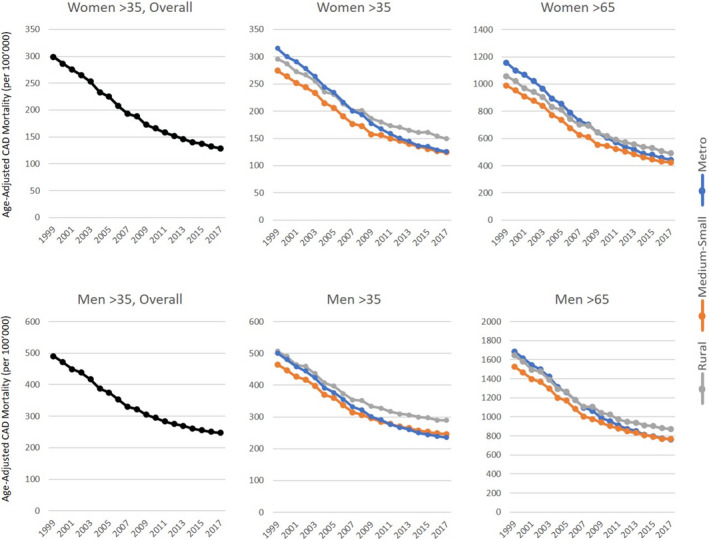
Age‐adjusted mortality from CAD in people aged ≥35 years, stratified by urbanization.
Detailed data are presented in Table 3. CAD indicates coronary artery disease.
Table 3.
Age‐Adjusted Mortality From CAD in People Aged ≥35 Years, Stratified by Urbanization and Sex
| Urbanization Area | Period, y | EAPCa | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Aged ≥35 y | ||||
| Overall | ||||
| Women | 1999–2002 | −5.2 | −2.3 | −5.6 |
| 2002–2010 | −5.9 | −6.3 | −5.4 | |
| 2010–2017 | −3.5 | −4 | −3 | |
| Men | 1999–2002 | −3.6 | −4.9 | −2.4 |
| 2002–2007 | −5.4 | −6.2 | −4.5 | |
| 2007–2012 | −3.8 | −4.7 | −2.9 | |
| 2012–2017 | −2.1 | −2.7 | −1.5 | |
| Metro | ||||
| Women | 1999–2002 | −3.9 | −5.3 | −2.5 |
| 2002–2012 | −6.1 | −6.4 | −5.8 | |
| 2012–2017 | −3.4 | −4.3 | −2.6 | |
| Men | 1999–2002 | −3.9 | −5.3 | −2.5 |
| 2002–2009 | −5.4 | −5.9 | −4.9 | |
| 2009–2014 | −3.7 | −4.6 | −2.7 | |
| 2014–2017 | −2.0 | −3.5 | −0.4 | |
| Medium‐Small | ||||
| Women | 1999–2003 | −4.2 | −5 | −3.3 |
| 2003–2009 | −6.1 | −6.8 | −5.4 | |
| 2009–2017 | −3.1 | −3.5 | −2.7 | |
| Men | 1999–2003 | −3.8 | −4.6 | −3 |
| 2003–2007 | −5.6 | −6.9 | −4.3 | |
| 2007–2012 | −3.3 | −4.1 | −2.4 | |
| 2012–2017 | −1.8 | −2.4 | −1.2 | |
| Rural | ||||
| Women | 1999–2010 | −4.6 | −4.9 | −4.3 |
| 2010–2017 | −2.5 | −3.2 | −1.7 | |
| Men | 1999–2009 | −4.3 | −4.6 | −4 |
| 2009–2017 | −1.8 | −2.3 | −1.4 | |
| Aged >65 y | ||||
| Metro | ||||
| Women | 1999–2002 | −3.8 | −5.2 | −2.4 |
| 2002–2012 | −6.3 | −6.6 | −6 | |
| 2012–2017 | −3.8 | −4.6 | −2.9 | |
| Men | 1999–2002 | −3.9 | −5.4 | −2.5 |
| 2002–2009 | −5.7 | −6.2 | −5.2 | |
| 2009–2014 | −3.9 | −5 | −2.8 | |
| 2014–2017 | −2.1 | −3.8 | −0.4 | |
| Medium‐Small | ||||
| Women | 1999–2003 | −4.2 | −5.2 | −3.3 |
| 2003–2009 | −6.5 | −7.2 | −5.7 | |
| 2009–2017 | −3.6 | −4.0 | −3.2 | |
| Men | 1999–2003 | −3.9 | −4.8 | −3 |
| 2003–2007 | −6.1 | −7.6 | −4.5 | |
| 2007–2012 | −3.6 | −4.6 | −2.5 | |
| 2012–2017 | −2.1 | −2.8 | −1.4 | |
| Rural | ||||
| Women | 1999–2011 | −4.9 | −5.2 | −4.6 |
| 2011–2017 | −2.9 | −3.9 | −2 | |
| Men | 1999–2010 | −4.5 | −4.8 | −4.2 |
| 2010–2017 | −2.0 | −2.6 | −1.4 | |
Results from statistical analysis (Joinpoint software). CAD indicates coronary artery disease; and EAPC, estimated annual percentage change.
All EAPCs, P<0.05.
Figure 4.
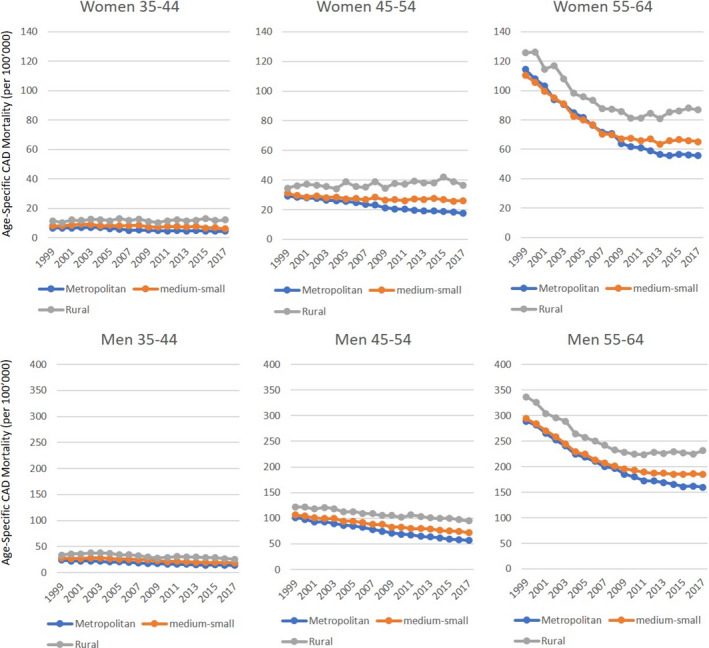
Age‐specific mortality rates according to age groups, sex, and urbanization. These are the same data reported in Figure 2 and Table 2, but presented with the same scale for comparison purposes.
Stratification by race shows higher CAD mortality rates for black patients throughout the entire period. The increase in mortality rates in rural areas was driven by a mortality increase in white women beginning in 2009 (EAPC: +0.9%; 95% CI, 0.0 to +1.8%), whereas black women experienced a numerical increase in mortality rates that was not statistically significant (EAPC: +0.5%; 95% CI, −2.0 to +0.4%). CAD mortality rates have been stagnating for both black and white men in rural areas (since 2010 and 2009, respectively). In addition, black men in medium‐small towns had a more recent onset of stagnation beginning in 2012 (Figure 5 and Table 4). To provide a better geographical overview, a map of the NCHS Urban–Rural Classification Scheme used by the CDC is provided in Figure 6.
Figure 5.
Age‐adjusted mortality from premature CAD in 35‐ to 64‐year‐olds by race and urbanization.
A, “Overall” denotes all urbanization categories. Mortality rates for women and men residing in rural areas (B), in medium‐small towns (C), and in metropolitan areas (D). Detailed data are presented in Table 4. B indicates black; CAD, coronary artery disease; and W, white.
Table 4.
Age‐Adjusted Mortality From Premature CAD in People Aged 35 to 64 Years, Stratified by Urbanization, Race, and Sex
| Race/Sex | Period, y | EAPC | 95% CI | Note | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Overall | |||||
| White women | 1999–2009 | −3.5a | −3.8 | −3.2 | … |
| 2000–2007 | −0.7a | −1.2 | −0.3 | … | |
| Black women | 1999–2001 | −1.7 | −5.2 | 2.5 | … |
| 2001–2011 | −5.3a | −5.7 | −5.0 | … | |
| 2011–2017 | −1.2a | −1.9 | −0.4 | … | |
| White men | 2009–2009 | −3.4a | −3.6 | −3.3 | … |
| 2009–2017 | −1.7a | −1.9 | −1.4 | … | |
| Black men | 1999–2011 | −4.3a | −4.6 | −4.0 | … |
| 2011–2017 | −1.1a | −2.0 | −0.2 | … | |
| Metro | |||||
| White women | 1999–2010 | −4.3a | −4.6 | −4.0 | … |
| 2010–2017 | −1.5a | −2.1 | −0.9 | … | |
| Black women | 1999–2001 | −1.7 | −6.0 | 2.7 | … |
| 2001–2012 | −5.5a | −5.8 | −5.1 | … | |
| 2012–2017 | −1.3a | −2.4 | −0.2 | … | |
| White men | 1999–2011 | −3.7a | −3.9 | −3.6 | … |
| 2011–2017 | −2.0a | −2.4 | −1.5 | … | |
| Black men | 1999–2005 | −3.8a | −4.6 | −3.0 | … |
| 2005–2010 | −5.4a | −6.9 | −3.9 | … | |
| 2010–2017 | −1.7a | −2.4 | −1.1 | … | |
| Medium‐Small | |||||
| White women | 1999–2007 | −3.6a | −4.1 | −3.1 | … |
| 2007–2017 | −0.7a | −1.1 | −0.3 | … | |
| Black women | 1999–2009 | −4.8a | −5.5 | −4.1 | … |
| 2009–2017 | −1.2a | −2.2 | −0.1 | … | |
| White men | 1999–2009 | −3.2a | −3.4 | −3.0 | … |
| 2009–2017 | −1.4a | −1.6 | −1.1 | … | |
| Black men | 1999–2002 | −3.1a | −5.3 | −0.8 | … |
| 2002–2008 | −4.8a | −5.8 | −3.8 | … | |
| 2008–2012 | −2.6a | −4.8 | −0.3 | … | |
| 2012–2017 | 0.2b | −0.8b | 2.5b | Stagnationb | |
| Rural | |||||
| White women | 1999–2009 | −2.0a | −2.6 | −1.4 | … |
| 2009–2017 | 0.9a , b | 0.0b | 1.8b | Significant increaseb | |
| Black women | 1999–2010 | −4.9a | −6.0 | −3.7 | … |
| 2010–2017 | 0.5b | −2.0b | 0.4b | Stagnationb | |
| White men | 1999–2009 | −2.8a | −3.1 | −2.5 | … |
| 2009–2017 | 0.4b | −0.8b | 0.1b | Stagnationb | |
| Black men | 1999–2010 | −4.1a | −4.7 | −3.4 | … |
| 2010–2017 | −0.7b | −2.1b | 0.7b | Stagnationb | |
Results from statistical analysis (Joinpoint software). CAD indicates coronary artery disease; and EAPC, estimated annual percentage change.
P<0.05.
EAPCs relevant for the discussion results from the statistical analysis.
Figure 6.
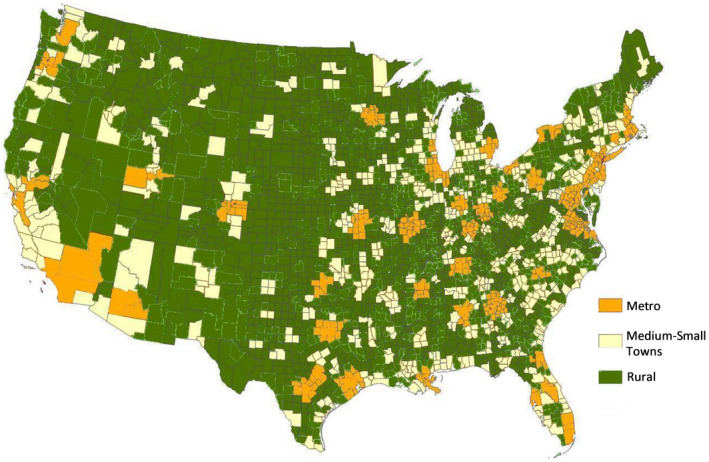
Urbanization, as defined by the Centers for Disease Control and Prevention ( https://www.cdc.gov/nchs/data_access/urban_rural.htm ).
CAD mortality rates have been consistently higher in rural than urban areas since 1999. The gap between urban and rural mortality rates has widened over time, especially in women. In 1999, the mortality rate for men aged 35 to 64 years in rural areas was 133.4 per 100 000 (95% CI, 131.0–135.7) and 111.2 per 100 000 (95% CI, 110.0–112.5) in metropolitan areas (absolute urban–rural difference of 22.2 per 100 000, 16.6% relative difference). In 2017, mortality for rural men was 96.7 per 100 000 (95% CI, 94.7–98.6) and 61.9 per 100 000 (95% CI, 61.1–62.3) for metropolitan men (absolute urban–rural difference of 34.8 per 100 000, 36.0% relative difference). In women aged 35 to 64, in 1999, the mortality rate in rural areas was 45.4 per 100 000 (95% CI, 44.1–46.8) and 39.0 per 100 000 (95% CI, 38.3–39.8) in metropolitan areas (urban–rural absolute difference 6.4 per 100 000, relative difference 16.9%). By 2017, the mortality rate for rural women was 37.6 per 100 000 (95% CI, 36.4–38.8) and for metropolitan women was 20.7 per 100 000 (95% CI, 20.2–21.1), amounting to an urban–rural absolute difference of 16.9 per 100 000 and a relative difference of 45.5%. These diverging trends in urban–rural mortality rates are even more pronounced in the younger age groups (35–44 and 45–54 years; Figures 1 and 2).
Discussion
In the United States, overall trends in premature death from CAD conceal considerable urban–rural disparities that become apparent when mortality is stratified by urbanization. When further stratified by sex, these trends reveal a disturbing aspect: women living in the rural United States have, for the first time, experienced an increase in premature CAD mortality. This result is in stark contrast to their metropolitan counterparts, who have experienced a virtually uninterrupted reduction in premature CAD mortality.
Increases in mortality rates often accompany increases in incidence and/or case fatality rates.13 Because there is no systematic recording of the incidence of MI and ischemic heart disease, hospitalization rates are often used as a proxy, with their own limitations. Nevertheless, recent data from representative cohorts showed an increase in the incidence of MI hospitalizations in young patients, especially young women.5, 6, 14, 15, 16 The increase in obesity prevalence has affected women more than men.7 Studies also suggested that middle‐aged women with diabetes mellitus or metabolic syndrome have up to a 5‐fold increase in the risk of CAD or acute MI compared with nondiabetic women and men.17, 18 In addition, nontraditional cardiovascular risk factors such as depression and perceived stress are also more common in young individuals, especially young women.19, 20, 21 Recent attention has been focused on neurobiological pathways as the basis for the increase in cardiovascular risk and will hopefully lead to improved awareness and treatment.22, 23
These latest trends are mirrored in the cardiovascular risk profiles of young patients hospitalized for MI, especially women.8, 24 Overall, the burden of cardiovascular risk factors in young patients with MI is increasing.8, 24, 25 The recognition of these differences in MI presentation in young women26 is offset by differences in treatment27 and general underrepresentation in trials studying risk factors, outcomes, and treatments.28, 29
Contrary to common perceptions, young patients (aged 35–54 years) comprise about a third of the hospitalizations for acute MI (33% in men and 31% in women in the 2010–2014 period; in women, this proportion was 21% in the 1995–1999 time period) according to a recent study.8 This result is in contrast to the Medicare population's hospitalization rate, which declined >20% in the 2001–2010 period.30 Of note, these adverse trends have occurred despite considerable improvements in both acute and chronic care of patients with CAD.
Our analyses also highlighted important racial disparities showing higher CAD mortality rates in black patients compared with white patients and stagnation of CAD mortality rates among young black people living in rural areas. This result points toward a similar direction as previous studies.31
Our study has some limitations that need to be addressed. It is possible that misclassification bias is present given inaccuracy on death certificates.32, 33, 34 Studies addressing misclassification bias have reported a tendency toward overestimation in mortality from CAD by as much as 20%,34 but a study addressing misclassification in out‐of‐hospital deaths showed a high degree of agreement between physician review and death certificate diagnosis.35 Another study found that misclassification affected mostly older (aged >85 years) decedents, older women in particular.32 We also cannot exclude that part of the effect on mortality is caused by cohort effect, which has implications for future studies: The increase in mortality reported in this study might lead to reduced CAD mortality in older age groups in the future, because high‐risk individuals are already deceased. Another potential bias that we cannot account for is competing risk. Nevertheless, it seems unlikely that competing risk inflated the adverse trends in premature CAD mortality, especially in the most recent years, which have seen a rise in death rates due to drug overdose and suicide: a recent report from the CDC showed a 2.6‐fold increase in drug‐overdose deaths in women aged 30 to 64 years during the 1999–2017 period.36 Finally, the data presented do not allow inferences regarding causality or other contributing factors because no information about risk factors, socioeconomic factors, healthcare access, and other items linked to the death certificate are available.
It is important to consider that these findings derive from publicly available data stemming from the CDC. Therefore, these data are not from a population sample that is assumed to be generalizable to the whole US population but rather from a census of all premature CAD deaths in the United States; this aspect confers high external validity. Moreover, the consistent coding with ICD‐10 for the entire period avoids potential misclassification due to overlap with ICD‐9 time periods. Another strength of our study is the nonbiased estimation of EAPC by Joinpoint regression analysis. Finally, to the best of our knowledge, this study is the first to show an increase in mortality rates from premature CAD in a segment of the US population.
Because death from premature CAD is the result of the exposure to cardiovascular risk factors accrued during childhood, adolescence, and young adulthood, these findings call for an intensification of public health efforts targeting prevention and cardiovascular risk factor control in young Americans, especially young women and residents of rural areas. Furthermore, one wonders if a focus on primary prevention is enough or if an additional, equally (if not more) intense focus on primordial prevention is necessary.37, 38
Conclusions
Disparities in the mortality rates from premature CAD are considerable across sex, urbanization, and race. Women living in the rural United States who are aged 45 to 54 and 55 to 64 years have experienced an increase in CAD mortality since 1999 and 2009, respectively, whereas the youngest group (35‐ to 44‐year‐olds) have experienced stagnating CAD mortality rates since 1999. Stagnation of CAD mortality rates was found among men aged 55 to 64 years in rural areas and medium‐small towns. These alarming trends warrant an intensification of public health efforts aimed at improving primary prevention and cardiovascular risk factor control in young women, especially those residing in rural areas.
Disclosures
None.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
(J Am Heart Assoc. 2020;9:e015334 DOI: 10.1161/JAHA.119.015334.)
For Disclosures, see page 12.
References
- 1. Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–2132. [DOI] [PubMed] [Google Scholar]
- 2. Wilmot KA, O'Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation. 2015;132:997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kulshreshtha A, Goyal A, Dabhadkar K, Veledar E, Vaccarino V. Urban‐rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep. 2014;129:19–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bureau of the Census . New census data show differences between urban and rural populations. American Community Survey, 2011–15 2016.
- 5. Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008). J Rural Health. 2012;28:392–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patterson PD, Moore CG, Probst JC, Shinogle JA. Obesity and physical inactivity in rural America. J Rural Health. 2004;20:151–159. [DOI] [PubMed] [Google Scholar]
- 7. Peters SAE, Muntner P, Woodward M. Sex differences in the prevalence of, and trends in, cardiovascular risk factors, treatment, and control in the United States, 2001 to 2016. Circulation. 2019;139:1025–1035. [DOI] [PubMed] [Google Scholar]
- 8. Arora S, Stouffer GA, Kucharska‐Newton AM, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd‐Jones D, McEvoy JW, Michos ED, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ingram DD, Franco SJ. 2013 NCHS urban–rural classification scheme for counties. National Center for Health Statistics. Vital Health Stat. 2014;2:166. [PubMed] [Google Scholar]
- 11. Smith DP, Bradshaw BS. Rethinking the Hispanic paradox: death rates and life expectancy for US non‐Hispanic White and Hispanic populations. Am J Public Health. 2006;96:1686–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Geiss LS, Wang J, Cheng YJ, Thompson TJ, Barker L, Li Y, Albright AL, Gregg EW. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312:1218–1226. [DOI] [PubMed] [Google Scholar]
- 13. Tunstall‐Pedoe H, Kuulasmaa K, Mahonen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary‐event rates to changes in coronary heart disease mortality: 10‐year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353:1547–1557. [DOI] [PubMed] [Google Scholar]
- 14. Lundeen EA, Park S, Pan L, O'Toole T, Matthews K, Blanck HM. Obesity prevalence among adults living in metropolitan and nonmetropolitan counties—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67:653–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Martin SL, Kirkner GJ, Mayo K, Matthews CE, Durstine JL, Hebert JR. Urban, rural, and regional variations in physical activity. J Rural Health. 2005;21:239–244. [DOI] [PubMed] [Google Scholar]
- 16. Cossman JS, James WL, Cosby AG, Cossman RE. Underlying causes of the emerging nonmetropolitan mortality penalty. Am J Public Health. 2010;100:1417–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kalyani RR, Lazo M, Ouyang P, Turkbey E, Chevalier K, Brancati F, Becker D, Vaidya D. Sex differences in diabetes and risk of incident coronary artery disease in healthy young and middle‐aged adults. Diabetes Care. 2014;37:830–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mente A, Yusuf S, Islam S, McQueen MJ, Tanomsup S, Onen CL, Rangarajan S, Gerstein HC, Anand SS, Investigators I. Metabolic syndrome and risk of acute myocardial infarction a case‐control study of 26,903 subjects from 52 countries. J Am Coll Cardiol. 2010;55:2390–2398. [DOI] [PubMed] [Google Scholar]
- 19. Shah AJ, Veledar E, Hong Y, Bremner JD, Vaccarino V. Depression and history of attempted suicide as risk factors for heart disease mortality in young individuals. Arch Gen Psychiatry. 2011;68:1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xu X, Bao H, Strait K, Spertus JA, Lichtman JH, D'Onofrio G, Spatz E, Bucholz EM, Geda M, Lorenze NP, et al. Sex differences in perceived stress and early recovery in young and middle‐aged patients with acute myocardial infarction. Circulation. 2015;131:614–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Xu X, Bao H, Strait KM, Edmondson DE, Davidson KW, Beltrame JF, Bueno H, Lin H, Dreyer RP, Brush JE, et al. Perceived stress after acute myocardial infarction: a comparison between young and middle‐aged women versus men. Psychosom Med. 2017;79:50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tawakol A, Osborne MT, Wang Y, Hammed B, Tung B, Patrich T, Oberfeld B, Ishai A, Shin LM, Nahrendorf M, et al. Stress‐associated neurobiological pathway linking socioeconomic disparities to cardiovascular disease. J Am Coll Cardiol. 2019;73:3243–3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dar T, Radfar A, Abohashem S, Pitman RK, Tawakol A, Osborne MT. Psychosocial stress and cardiovascular disease. Curr Treat Options Cardiovasc Med. 2019;21:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leifheit‐Limson EC, D'Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, Krumholz HM, Lichtman JH. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO study. J Am Coll Cardiol. 2015;66:1949–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lichtman JH, Leifheit EC, Safdar B, Bao H, Krumholz HM, Lorenze NP, Daneshvar M, Spertus JA, D'Onofrio G. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: evidence from the VIRGO Study (Variation in Recovery: role of Gender on Outcomes of Young AMI Patients). Circulation. 2018;137:781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gupta A, Barrabes JA, Strait K, Bueno H, Porta‐Sanchez A, Acosta‐Velez JG, Lidon RM, Spatz E, Geda M, Dreyer RP, et al. Sex differences in timeliness of reperfusion in young patients with ST‐segment‐elevation myocardial infarction by initial electrocardiographic characteristics. J Am Heart Assoc. 2018;7:e007021 DOI: 10.1161/JAHA.117.007021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Scott PE, Unger EF, Jenkins MR, Southworth MR, McDowell TY, Geller RJ, Elahi M, Temple RJ, Woodcock J. Participation of women in clinical trials supporting FDA approval of cardiovascular drugs. J Am Coll Cardiol. 2018;71:1960–1969. [DOI] [PubMed] [Google Scholar]
- 29. Kim ES, Carrigan TP, Menon V. Enrollment of women in National Heart, Lung, and Blood Institute‐funded cardiovascular randomized controlled trials fails to meet current federal mandates for inclusion. J Am Coll Cardiol. 2008;52:672–673. [DOI] [PubMed] [Google Scholar]
- 30. Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee‐for‐service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. [DOI] [PubMed] [Google Scholar]
- 31. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr, Willis M, et al; American Heart Association Council on E, Prevention, Council on Cardiovascular Disease in the Y, Council on C, Stroke N, Council on Clinical C, Council on Functional G, Translational B and Stroke C . Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. [DOI] [PubMed] [Google Scholar]
- 32. Lloyd‐Jones DM, Martin DO, Larson MG, Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020–1026. [DOI] [PubMed] [Google Scholar]
- 33. Smith CJ, Scott SM, Wagner BM. The necessary role of the autopsy in cardiovascular epidemiology. Hum Pathol. 1998;29:1469–1479. [DOI] [PubMed] [Google Scholar]
- 34. Coady SA, Sorlie PD, Cooper LS, Folsom AR, Rosamond WD, Conwill DE. Validation of death certificate diagnosis for coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. J Clin Epidemiol. 2001;54:40–50. [DOI] [PubMed] [Google Scholar]
- 35. Folsom AR, Gomez‐Marin O, Gillum RF, Kottke TE, Lohman W, Jacobs DR Jr. Out‐of‐hospital coronary death in an urban population—validation of death certificate diagnosis. The Minnesota Heart Survey. Am J Epidemiol. 1987;125:1012–1018. [DOI] [PubMed] [Google Scholar]
- 36. VanHouten JP, Rudd RA, Ballesteros MF, Mack KA. Drug overdose deaths among women aged 30‐64 years—United States, 1999–2017. MMWR Morb Mortal Wkly Rep. 2019;68:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chomistek AK, Chiuve SE, Eliassen AH, Mukamal KJ, Willett WC, Rimm EB. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol. 2015;65:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fernandez‐Jimenez R, Jaslow R, Bansilal S, Santana M, Diaz‐Munoz R, Latina J, Soto AV, Vedanthan R, Al‐Kazaz M, Giannarelli C, et al. Child health promotion in underserved communities: the FAMILIA Trial. J Am Coll Cardiol. 2019;73:2011–2021. [DOI] [PubMed] [Google Scholar]


