Introduction
In 1998, Felitti and colleagues published a landmark study, titled “Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults.”1 Commonly referred to as the ACE (Adverse Childhood Experience) study, the authors reported, “We found a strong graded relationship between the breadth of exposure to abuse or household dysfunction during childhood and multiple risk factors for several of the leading causes of death in adults.”
See Article by Pierce et al.
In this issue of the Journal of the American Heart Association (JAHA), Pierce and colleagues2 report their analysis of the association between having experienced adversity and trauma in childhood with cardiovascular disease (CVD) outcomes. Using data from the CARDIA (Coronary Artery Risk Development in Young Adults) study, the authors measured the level of adversity experienced in childhood using the Childhood Family Environment (CFE) questionnaire, a survey instrument that was adapted from the original ACE study survey.
The CARDIA study is a longitudinal study of 3646 subjects who were first surveyed in 1985 to 1986 at an average age of 25 years. The authors administered the CFE questionnaire in 2000 to 2001 to assess the level of adversity experienced in childhood. On the basis of responses to 7 different questions, the level of CFE adversity is scored as low, moderate, or high. The authors were then able to track health outcomes through 2015 to 2016 to assess both the incidence of CVD and the all‐cause mortality rate. The authors concluded that, “Adverse CFE was associated with CVD incidence and all‐cause mortality later in life, even after controlling for CVD risk factors in young adulthood.”
To a large extent, Pierce et al2 have reproduced the outcomes of the original ACE study. They have done it using 30 years of longitudinal data in a population from a diverse geographical background selected to overrepresent blacks. The authors found that the association between childhood adversity and CVD incidence, “was no longer statistically significant in the fully‐adjusted analysis, indicating that demographic, socioeconomic, clinical, and psychological factors may collectively partially mediate this relationship.”
The authors identified an association between child adversity and CVD incidence and mortality “after controlling for CVD risk factors in young adulthood,” whereas that association was no longer statistically significant for CVD incidence after including “demographic, socioeconomic, clinical, and psychological factors.”
On the basis of the authors’ multivariate analysis, perhaps the strongest mediating factor in affecting CVD risk is participant education. There is a striking difference in the highest level of education attained among subjects having experienced different levels of childhood adversity. As shown in table 1 of the article, >45% of those in the highest level of adversity had either dropped out of high school or stopped with graduation from high school. By contrast, <30% of those in the lowest level of adversity had stopped at high school, with >70% having enrolled in college.
These findings are consistent with federal data from 1996, showing the association between the highest level of education attained and additional life expectancy at the age of 25 years, as shown in Figure 1. Recall that the average age of the subjects initially enrolled in the CARDIA study in 1985 to 1986 was 25.1 years. Comparing those who had not completed high school with those who had completed college, we see a 7.4‐year difference in life expectancy for men at this age and a 5.8‐year difference for women.
Figure 1. Additional life expectancy in the United States at the age of 25 years, by sex and highest level of education, 1996.
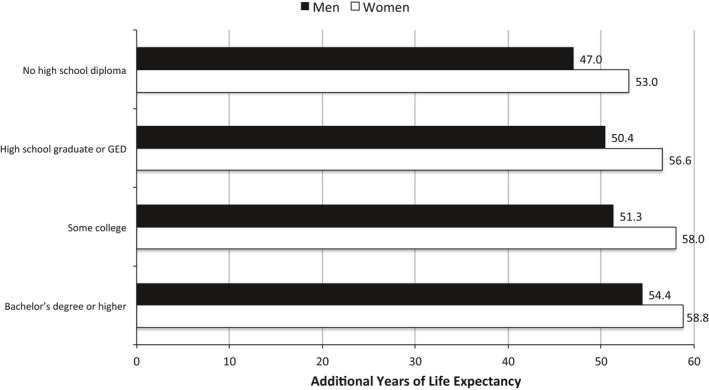
Data from US Centers for Disease Control and Prevention, 2011.3 GED indicates general equivalency diploma.
What might account for this life expectancy gap, given that these subjects were only a few years past adolescence? Figure 2 provides an answer. In the same way that life expectancy increases in lockstep with higher levels of education, rates of smoking decrease in lockstep with increasing education.
Figure 2. Percentage of people aged ≥18 years who were current smokers, 2011, by sex and highest level of education completed.
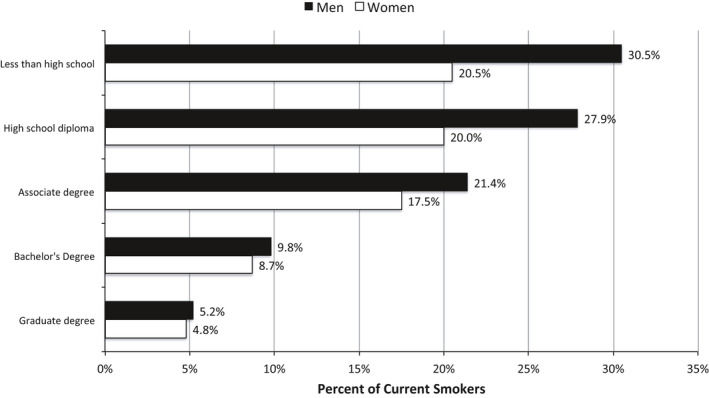
Data from US Centers for Disease Control and Prevention, 2012.4
It has long been established that smoking is associated with higher levels of CVD as well as cancer, leading to earlier deaths. Looking again at table 1 of the article by Pierce et al,2 we see a clear association between the level of childhood adversity experienced and subsequent rates of smoking. At the average age of 25 years, 34.9% of those having experienced high levels of adversity were current smokers, whereas 22.8% of those with low levels of adversity were smokers.
What is the link between education and smoking? Psychologists Philip Zimbardo and John N. Boyd have provided one clear answer: time perspective.5 Individuals growing up in different social backgrounds develop different perceptions of the concept of time. Those with a “future” perspective carefully consider the future consequences of present choices in the process of “planning for and achievement of future goals.” By contrast, those with a “present‐fatalistic” perspective come to believe “that the future is predestined and uninfluenced by individual actions, whereas the present must be borne with resignation because humans are at the whimsical mercy of ‘fate’.”
The authors described Zimbardo's own childhood experience of “Growing up in poverty [which] led Zimbardo to realize that his family and friends were prisoners of a fatalistic present. Education liberated him, and others, into a more future‐oriented realm of existence.” Children growing up in poverty and other forms of adversity are prone to adopting a “present‐fatalistic” perspective on the consequences of their action. “Since my life is predestined by fate,” a child may think, “why worry about the damage smoking may do to my health 30 years from now? Besides, it makes me feel so good.”
There is another way that these types of early childhood experiences can influence behaviors linked to future health status. Mead et al6 describe the way that the social networks one establishes can influence one's own behavior in things such as smoking. As children transition into adolescence, it is common to look to one's peers for guidance in attitudes and behaviors. Those adolescents who feel disconnected from the academic environment of school will seek out a network of friends who feel the same, and will tend to adopt behaviors that are common in this network of peers. As Mead et al6 point out, smoking is one of those behaviors that is often shared by such a social network, contributing to the association between low educational attainment and smoking.
In a study of >30 000 black and white adults aged ≥45 years, Kaplan et al7 concluded that, “Educational attainment is a significant predictor of longevity. Other factors including age, race, income, health behaviors, and cardiovascular risk factors only partially explain the relationship.”
Beyond associated health‐related behaviors and cardiovascular risk factors, Pierce et al2 have identified another important factor affecting CVD risk and longevity. As they describe, “Toxic stress, abuse, and neglect in childhood is thought to alter hypothalamic‐pituitary‐adrenal (HPA) axis…Individuals subsequently experience increases in the stress hormone cortisol and are predisposed to increased levels of inflammation and autonomic dysfunction.” This increase in hormonal response is often referred to as an increase in allostatic load. As described by Barr,8 “There is growing evidence that chronic elevation of allostatic load as a consequence of high levels of early childhood stress can trigger early atherosclerotic changes in children independently of behaviors.”
A common physiologic response to long‐term increases in allostatic load is increased intima‐media thickness and associated stiffness in the lining of the arterial circulation. Using ultrasonography, Thurston and Matthews9 were able to follow the intima‐media thickness of 81 black and 78 white adolescents with no evidence of CVD on preliminary analysis conducted at the age of 14 to 16 years. After controlling for blood pressure and body mass index, by the age of 19 years, those adolescents from families experiencing lower socioeconomic status were found to have increased carotid intima‐media thickness. The authors concluded that these disparities in CVD risk appear early in life among adolescents who have grown up under the stress of socioeconomic disadvantage.
There is a second outcome of dysregulation of allostatic load beginning early in childhood that can have profound impacts on educational attainment and associated CVD risk. As Pierce et al2 describe, early elevation of allostatic load caused by disruption of the hypothalamic‐pituitary‐adrenal axis can “cause an increase in the volume and activity of the amygdala, the center of the brain responsible for fear and emotional regulation.”
The amygdala is located in the central portion of the base of the brain. It is immediately adjacent to another important brain center, the hippocampus. Although the amygdala is largely responsible for emotional regulation, the hippocampus is responsible for the development of executive function (EF). As described by Zelazo et al in a report by the US Department of Education,10 EF involves “the attention‐regulation skills that make it possible to sustain attention, keep goals and information in mind, refrain from responding immediately, resist distraction, tolerate frustration, consider the consequences of different behaviors, reflect on past experiences, and plan for the future.”
As might be expected, strong EF is essential for a child entering kindergarten to adapt to the behavioral and learning expectations of the school environment. However, as reported by Barr,11 between the ages of 3 and 6 years, a child who is experiencing increased activity of the amygdala because of high levels of adversity and stress will also experience delayed development of EF. This delay in EF will often result in the child demonstrating disruptive behavior in kindergarten. Portilla et al12 studied 338 5‐year‐old children from diverse backgrounds as they first entered kindergarten. They reported that, “Low self‐regulation in kindergarten fall, as indexed by inattention and impulsive behaviors, predicted more conflict with teachers in kindergarten spring and this effect persisted into first grade. Conflict and low self‐regulation jointly predicted decreases in school engagement which in turn predicted first‐grade academic competence.”
By the end of kindergarten, children having experienced high levels of early adversity may be on their way to disconnecting from school. As they move into early adolescence, they may form close social networks with other children with comparable experiences. These networks may support unhealthy behaviors, such as smoking. Coupled with the cellular injury chronically elevated allostatic load triggers in the cardiovascular system, these behaviors increase the risk for CVD and premature mortality.
In their article, Pierce et al2 conclude that, “exposure to adversity and trauma during childhood—including child abuse, neglect, and household dysfunction—is associated with greater risk of incident cardiovascular disease, primarily coronary artery disease.” This conclusion is supported by the 30 years of longitudinal data the authors use to arrive at these conclusions. Pierce et al2 have confirmed that child adversity, as reflected in a stressful family environment, can lead to long‐term health consequences.
This is not to say, however, that a child experiencing early adversity is irreversibly destined to experience increased CVD and early mortality. As Wise13 has made abundantly clear, such a “highly deterministic view of early‐life interactions is not supported by the science…” Wise13 argues for “an expanded research and policy agenda that might be more capable of generating urgently needed strategies for reducing disparities in child health.” Rather than viewing the child as permanently damaged by the experience of adversity, we need to appreciate the child's capacity to respond to subsequent emotional and personal support in ways that can reverse the behavioral and physiologic impacts of adversity.
Disclosures
Dr Barr receives royalties from Johns Hopkins University Press for textbooks he has written. He is Professor of Pediatrics, and of Education (by Courtesy), at Stanford University.
(J Am Heart Assoc. 2020;9:e016162 DOI: 10.1161/JAHA.120.016162.)
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
For Disclosures, see page 4.
References
- 1. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults—the adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14:245–258. [DOI] [PubMed] [Google Scholar]
- 2. Pierce JB, Kershaw KN, Kiefe CI, Jacobs DR, Sidney S, Merkin SS, Feinglass J. Association of childhood psychosocial environment with 30‐year cardiovascular disease incidence and mortality in middle age. J Am Heart Assoc. 2020;9:e015326 DOI: 10.1161/JAHA.119.015326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. US Centers for Disease Control and Prevention . Health, United States, 2011: life expectancy at age 25, by sex and education level: United States, 1996 and 2006. http://www.cdc.gov/nchs/data/hus/2011/fig32.pdf. Accessed February 12, 2020.
- 4. US Centers for Disease Control and Prevention . Current cigarette smoking among adults—United States, 2011. Morb Mortal Wkly Rep. 2012;61:889–894. [PubMed] [Google Scholar]
- 5. Zimbardo PG, Boyd JN. Putting time in perspective: a valid, reliable individual‐differences metric. J Pers Soc Psychol. 1999;77:1271–1288. [Google Scholar]
- 6. Mead EL, Rimal RN, Ferrence R, Cohen JE. Understanding the sources of normative influence on behavior: the example of tobacco. Soc Sci Med. 2014;115:139–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kaplan RM, Howard VJ, Safford MM, Howard G. Educational attainment and longevity: results from the REGARDS U.S. national cohort study of blacks and whites. Ann Epidemiol. 2015;25:323–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barr DA. The childhood roots of cardiovascular disease disparities. Mayo Clin Proc. 2017;92:1415–1421. [DOI] [PubMed] [Google Scholar]
- 9. Thurston RC, Matthews KA. Racial and socioeconomic disparities in arterial stiffness and intima media thickness among adolescents. Soc Sci Med. 2009;68:807–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zelazo PD, Blair CB, Willoughby MT. Executive Function: Implications for Education. Washington, DC: US Department of Education, Institute of Education Sciences, National Center for Education Research ;2016. https://ies.ed.gov/ncer/pubs/20172000/pdf/20172000.pdf. Accessed February 13, 2020. [Google Scholar]
- 11. Barr DA. When trauma hinders learning. Phi Delta Kappan. 2018;99:39–44. [Google Scholar]
- 12. Portilla XA, Ballard PJ, Adler NE, Boyce WT, Obradovic J. An integrative view of school functioning: transactions between self‐regulation, school engagement, and teacher‐child relationship quality. Child Dev. 2014;85:1915–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wise PH. Confronting social disparities in child health: a critical appraisal of life‐course science and research. Pediatrics. 2009;124:S203–S211. [DOI] [PubMed] [Google Scholar]


