Abstract
Background
Temporal declines in cardiac stress tests results, coronary revascularization, and cardiovascular mortality have suggested a decline in the population burden of coronary disease until the 2000s. However, recent data indicate these favorable trends could be ending. We aimed to assess the evolution of the population burden of coronary disease in the community by examining trends in angiography and revascularization.
Methods and Results
We analyzed age‐ and sex‐adjusted trends from all coronary angiographic diagnostic procedures and revascularizations performed in Olmsted County, MN from 2000 to 2018. A total of 12 981 invasive angiograms were performed among 9049 individuals (64% men; 55% aged ≥65 years). Adjusted angiography rates decreased by 30% (95% CI, 25%–34%) between 2000 and 2009 and leveled off thereafter. Including computed tomography, angiography uncovered an increase in angiography use in recent years (risk ratio=1.15 [95% CI, 1.07–1.23] for 2018 versus 2014) and a decline in the prevalence of anatomic CAD from 2000 to 2018. CAD severity declined substantially from 2000 to 2009, followed by a plateau. Among 6570 revascularizations (72% men; 57% aged ≥65 years), 77% were percutaneous coronary interventions and 23% coronary artery bypass graft surgeries. The adjusted revascularization rates declined by 34% (95% CI, 27%–39%) from 2000 to 2009, followed by a plateau (risk ratio=1.10 [95% CI, 1.00–1.22]).
Conclusions
Between 2000 and 2018 in the community, coronary angiography use declined initially, leveled off, and then increased. Trends in CAD severity and revascularization use decreased then plateaued. The most recent trends are concerning as they suggest the burden of coronary disease is no longer declining. This warrants reinvigorated primary prevention and population surveillance.
Keywords: community surveillance, coronary angiography, coronary artery disease, coronary revascularization, epidemiology, secular trends
Subject Categories: Epidemiology, Coronary Artery Disease
Clinical Perspective
What Is New?
We studied the comprehensive experience of a community in the Upper Midwest between 2000 and 2018 and found that coronary angiography use declined initially, leveled off, and then increased.
Trends in coronary artery disease severity and revascularization use decreased then plateaued.
What Are the Clinical Implications?
These recent trends in diagnostic and revascularization coronary procedures are concerning as they suggest the burden of coronary disease is no longer declining.
This warrants reinvigorated primary prevention and population surveillance.
Introduction
During the past few decades, substantial declines in coronary heart disease (CHD) incidence1, 2, 3, 4 and mortality5, 6 rates were reported in the United States, and several longitudinal studies have reported a concomitant decline in severely abnormal cardiac stress tests.7, 8 Taken collectively, these data are consistent with a decline in the burden of CHD with approximately half of the reduction in CHD death rates between 1980 and 2000 attributed to improved clinical care of CHD, including secondary prevention and coronary revascularization.9
We previously reported an increase in revascularization in Olmsted County, MN, between 1990 and 2004, with a large increase in percutaneous coronary intervention (PCI) partially offset by a decrease in coronary artery bypass grafting (CABG) surgery.10 Other reports also revealed marked growth in the use of cardiac catheterization over that time period.11, 12 However, more recent reports13, 14, 15, 16, 17, 18 have described a decline in diagnostic coronary angiography and in all forms of coronary revascularization. These studies had inherent limitations including reliance on Medicare data, thereby excluding younger and privately insured patients, restriction to inpatient settings, and relatively short follow‐up. Further, they did not report the results of coronary angiograms which are essential to interpret trends in revascularization as the choice between CABG, PCI, or pharmacotherapy depends chiefly on the extent of anatomic coronary artery disease (CAD).19 Therefore, the community trends since 2000 in the use of angiography, prevalence and severity of CAD, and revascularization for CAD are unknown. To address these gaps in knowledge, we examined contemporary trends in use and results of coronary diagnostic (both invasive angiography and computed tomography [CT] angiography) and interventional procedures (both PCI and CABG) in a geographically defined community between 2000 and 2018.
Methods
Study Setting
Olmsted County, MN (2010 census population, 144 248), a mixed rural‐urban setting, is 75 miles southeast of Minneapolis and St Paul, with ≈70% of its population residing in Rochester, the centrally located county seat. In 2010, about 85% of all residents were white and 13% were aged ≥65 years. The Olmsted County population is largely middle class with 94% of adults having graduated from high school and only ≈4% uninsured. With the exception of a higher proportion being employed in the healthcare industry, the population of Olmsted County is representative of the state of Minnesota and the Upper Midwest region of the United States.20
Epidemiological research in Olmsted County is feasible because the county is relatively isolated from other urban centers, and nearly all medical care is delivered to local residents by a handful of providers. Mayo Clinic and Olmsted Medical Center provide comprehensive care for the region in every clinical discipline. The epidemiological potential of this situation is enhanced by the fact that each provider uses a unit medical record system whereby all data collected for an individual are assembled in one place. The unit records of each provider in the county are available for use. These medical records are easily retrievable because, since the early 1900s, Mayo Clinic has maintained extensive indexes based on clinical and histologic diagnoses and surgical and billable procedures. The Rochester Epidemiology Project21, 22 has developed a similar index for the records of other providers of medical care to local residents; it captures virtually all individuals who have resided in Olmsted County, MN, from 1966 to present, regardless of age, sex, ethnicity, disease status, socioeconomic status, or insurance status.23 The result is the linkage of medical records from essentially all sources of medical care available to and used by the Olmsted County population.
All Olmsted County residents aged ≥25 years who granted general research authorization to review their medical records were eligible to be included in this study. All aspects of the study were approved by the appropriate institutional review boards. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Coronary Procedures
All invasive coronary angiography procedures performed in Olmsted County from January 1, 2000 through December 31, 2018 were identified by International Classification of Diseases, Ninth Revision (ICD‐9) codes 88.50, 88.55, 88.56 and 88.57 and International Classification of Diseases, Tenth Revision (ICD‐10) codes B210010, B2100ZZ, B210110, B2101ZZ, B210Y10, B210YZZ, B211010, B2110ZZ, B211110, B2111ZZ, B211Y10, and B211YZZ along with Current Procedural Terminology, Fourth Edition codes 93454–93461, 93545, and 93563. The results of invasive angiographies were obtained from a registry maintained by Mayo Clinic that contains the invasive coronary angiography procedures, diagnostic and therapeutic, performed at Mayo Clinic since 1979, or were abstracted from the medical record by trained nurse abstractors when the angiography results were not available in the registry.
CT coronary angiography was introduced in 2010 and all procedures performed in Olmsted County from January 1, 2010 through December 31, 2018 were identified using Current Procedural Terminology, Fourth Edition code 75574. Results were abstracted from the medical record, and when only descriptive results for a vessel were available, “mild” was classified as <50% stenosis while “moderate” and “severe” were classified as ≥50% stenosis.
To avoid inclusion of repeat procedures that were part of a single clinical episode of care, any invasive angiogram procedure that occurred within 30 days of a prior invasive angiogram was excluded from the analysis. CT angiograms which occurred within 30 days of a previous CT angiogram or within 30 days of an invasive angiogram were also excluded.
Significant angiographic CAD was defined as 50% stenosis or greater of the left anterior descending, left circumflex, right coronary artery, or the left main coronary artery.24 Disease categories were created for analytical purposes: negative (no significant stenosis [as defined above]), 1‐vessel disease not involving the left main artery, 2‐vessel disease not involving the left main artery, 3‐vessel disease not involving the left main artery, and left main CAD.
Revascularization was defined as CABG or PCI, with or without stent placement. PCI was queried electronically from a registry that Mayo Clinic has maintained since 1979. CABG procedures were queried electronically using Current Procedural Terminology, Fourth Edition codes 33510–33514, 33516–33519, 33521–33523, 33533–33536, 00566, 00567, 33508, 35500, 35600, and 4110F.
Statistical Analysis
Age‐, sex‐, and year‐specific usage rates were calculated for each procedure: coronary angiography (invasive angiograms with and without CT angiograms), PCI, and CABG. PCI data were available through June 30, 2018, thus weighting was used to estimate the yearly rate for 2018. The denominators were determined by Olmsted County population census data for 2000 and 2010, with linear interpolation for the intercensal years and extrapolation after 2010.25 These rates were directly standardized to the age and sex distribution of the 2010 total US population using a lower cutoff age of 25 years. Poisson regression models were used to assess temporal trends in procedure use. Specific counts for each calendar year, age (integer years with those ≥85 years grouped together), and sex were used as the unit of observation. Model goodness‐of‐fit was assessed by examining the deviance statistic, which was found to be valid for all models examined.
Temporal trends in CAD were examined graphically by modeling year of the angiogram as a smoothing spline with 4 degrees of freedom while adjusting for age and sex. Logistic regression models were used to examine temporal trends in any CAD versus none, and, among those with CAD, 3‐vessel and/or left main disease versus 1‐ or 2‐vessel disease.
Models were fit using piecewise functions for 2000 to 2009 and 2010 to 2018 with connected segments and were adjusted for age, age2, and sex. Non‐linear temporal trends were tested by including year2 in the models. Analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC).
Results
Use of Coronary Angiography
Between 2000 and 2018, 13 565 invasive coronary angiograms were performed; 584 angiograms which occurred within 30 days of a previous angiogram were excluded, resulting in 12 981 invasive angiograms among 9049 individuals for analyses. Among the 9049 individuals, 6808 (75.2%) had 1 angiogram, 1439 (15.9%) had 2 angiograms >30 days apart, and 802 (8.9%) had ≥3 angiograms >30 days apart. The median (interquartile range) time between repeat angiograms was 2.00 (0.77–4.55) years. Among the invasive angiograms, 64% were performed on men and 55% of the subjects were aged ≥65 years at the time of the angiogram. The age‐ and sex‐standardized rates per 100 000 population were 948 (95% CI, 926–969) in 2000 to 2009 and 641 (95% CI, 624–658) in 2010 to 2018. The standardized rates of invasive angiography declined over time (P<0.001; Figure 1). Between 2000 and 2009, the rate of invasive coronary angiography declined by 30% (age‐ and sex‐adjusted risk ratio 0.70, 95% CI, 0.66–0.75 for 2009 compared with 2000) with a non‐linear trend (year2 P<0.001) indicating that the decline mostly occurred between 2005 and 2009 (Table S1). Between 2010 and 2018, no significant change was observed in the rate (P=0.079).
Figure 1.
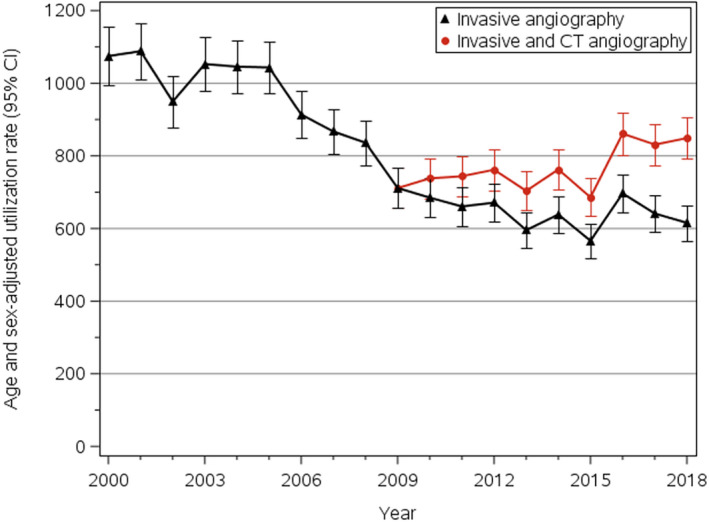
Trends in coronary angiography usage in Olmsted County, MN, 2000 to 2018. Yearly rates (95% CIs), per 100 000 people, have been standardized by the direct method to the age and sex distribution of the US 2010 total population. CT indicates computed tomography.
CT coronary angiograms were introduced in 2010, and 1426 of them were performed between 2010 and 2018. After exclusions (described under Methods), there were 1143 CT angiograms (17.2% of all angiograms performed during 2010–2018) among 1098 people; 48% were performed in men and 27% of the subjects were aged ≥65 years at the time of the test. The rate of CT angiograms increased during 2010 to 2018 (P<0.001), with CT angiograms comprising ≈25% of all angiograms performed in the most recent years (Table S2). After combining invasive and CT angiograms, a non‐linear increase was observed in angiography usage between 2010 and 2018 with no increase from 2010 to 2015 followed by a pronounced increase (Figure 1, Table S1). Inclusion of CT angiograms in the usage analyses for the entire study period only minimally offset the aforementioned decline in the usage of angiograms (standardized rate for 2010–2018: 772; 95% CI, 753–790), which remained markedly lower than the rate during 2000–2009 (P trend<0.001; Figure 1).
Prevalence and Severity of CAD
We first examined the trends in prevalence of any CAD from invasive and CT coronary angiograms combined, mindful of the fact that the recent increased use of CT angiograms would impact the trends in CAD prevalence. A linear decline was observed for prevalence of any CAD over the entire study period, adjusted for age and sex (Figure 2A; P linear trend<0.001). The odds ratios (OR) for any CAD versus none were 0.66 (95% CI, 0.58–0.76) for 2009 compared with 2000 and 0.70 (95% CI, 0.61–0.80) for 2018 compared with 2010 (Table).
Figure 2.
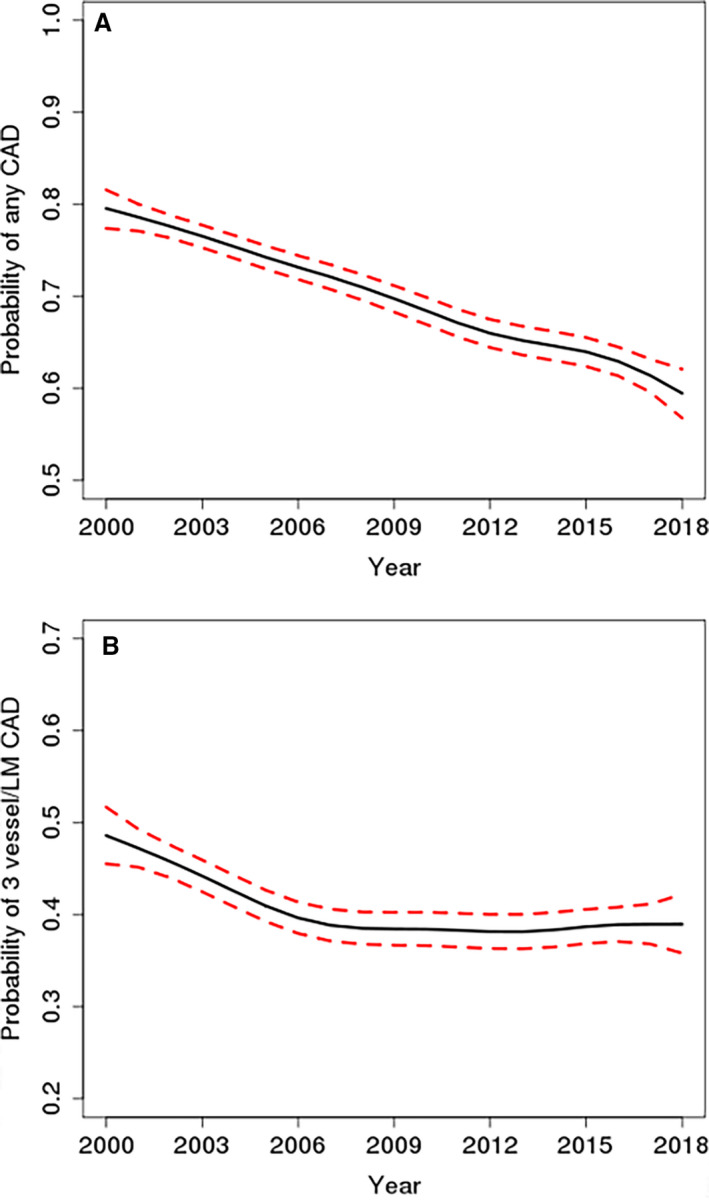
Spline curves of prevalence of coronary artery disease on invasive and computed tomography angiograms (A) and 3‐vessel and/or left main coronary artery disease among those with prevalent coronary artery disease identified from all invasive angiograms and computed tomography angiograms (B) in Olmsted County, MN, 2000 to 2018, adjusted for age and sex. CAD indicates coronary artery disease; LM, left main.
Table 1.
Temporal Trends in Prevalence of Coronary Artery Disease in Olmsted County, MN, 2000 to 2018
| CAD Prevalence | Type of Angiogram | Year Comparison | OR (95% CI)a |
|---|---|---|---|
| Any CAD vs none | Invasive | 2009 vs 2000 | 0.66 (0.58–0.76) |
| Invasive and CT | 2018 vs 2010 | 0.70 (0.61–0.80) | |
| 3‐vessel/left main vs 1‐ or 2‐vessel disease | Invasive |
2005 vs 2000 2009 vs 2005 |
0.70 (0.59–0.83) 0.91 (0.83–1.00) |
| Invasive and CT | 2018 vs 2010 | 1.02 (0.85–1.22) |
CAD indicates coronary artery disease; CT, computed tomography; OR, odds ratio.
Adjusted for age, age2, and sex.
We then focused on individuals with prevalent CAD to assess temporal trends in the severity of CAD (defined as 3‐vessel and/or left main disease versus 1‐ or 2‐vessel disease). Over the entire period, the prevalence of severe CAD followed a non‐linear trend (Figure 2B; P non‐linear trend<0.001). It declined between 2000 and 2005 (odds ratio=0.70, 95% CI, 0.59–0.83), leveled off between 2005 and 2009 (odds ratio=0.91, 95% CI, 0.38–1.00) with no further change between 2010 and 2018 (Table).
Trends in Coronary Revascularization
During the study period, 6570 revascularization procedures were performed, 72% among men and 57% in people aged ≥65 years. Most (77%) revascularizations were PCI with a minority (23%) of CABG. Among individuals undergoing PCI, 70% were men and 55% were aged ≥65 years. Of those undergoing CABG, 78% were men and 63% were aged ≥65 years.
The age‐ and sex‐standardized rates of having any revascularization procedure declined markedly during the earlier period and leveled off in most recent years (Figure 3). The standardized rates per 100 000 population were 460 (95% CI, 445–475) in 2000 to 2009 and 342 (95% CI, 330–355) in 2010 to 2018. Overall, age‐ and sex‐adjusted rates declined by 34% between 2000 and 2009 (risk ratio 0.66, 95% CI, 0.61–0.73 for 2009 compared with 2000). A non‐linear decline was observed (year2 P=0.002), illustrated by a 12% decrease between 2000 and 2005 and a 24% decrease between 2005 and 2009 (Table S1). The relative decline during 2000 to 2009 was more pronounced for CABG than PCI (P interaction<0.001); however, because PCIs occur more frequently, the absolute decline was greater for PCIs. The rates of revascularization stabilized in recent years (2010–2018).
Figure 3.
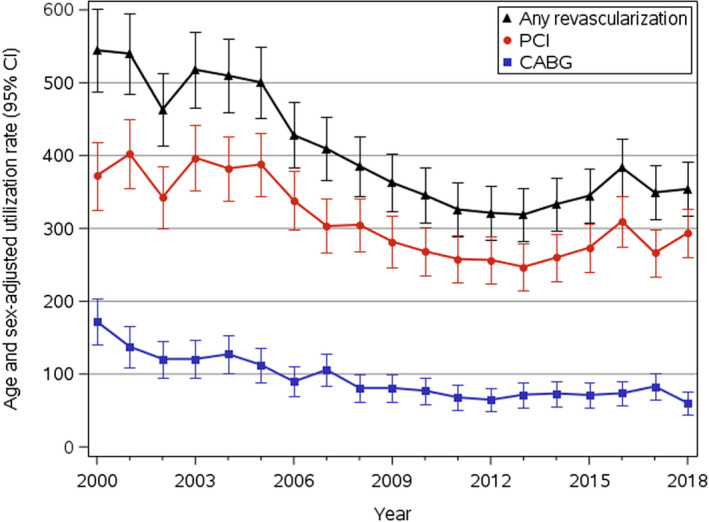
Trends in Coronary Revascularization in Olmsted County, MN, 2000 to 2018. Yearly rates (95% CIs), per 100 000 people, have been standardized by the direct method to the age and sex distribution of the US 2010 total population. CABG indicates coronary artery bypass grafting; PCI, percutaneous coronary interventions.
Discussion
Summary of Findings
These comprehensive analyses of a community in the Upper Midwest demonstrate profound changes in diagnostic and revascularization coronary procedures between 2000 and 2018. The use of invasive angiography declined, but the introduction of CT angiograms altered this trend resulting in an increase in the use of any diagnostic angiographic procedures and a resultant decrease in the prevalence of any angiographic CAD.
Importantly, the severity of angiographic CAD declined initially between 2000 and 2009 but leveled off between 2010 and 2018; the use of revascularization followed the same pattern.
Trends in the Use of Coronary Angiography
In the 1990s and the beginning of the 2000s, the use of coronary angiography increased in the community and nationally.10, 11, 12 Subsequent studies reported striking changes with a decline between 2004 and 2009.14, 16 Our data are congruent with these findings and demonstrate that the use of coronary angiography in the community continued to decline through 2009 but leveled off thereafter.
These trends likely reflect multiple factors. The previous increase in the use of cardiac diagnostic procedures received substantial attention from policymakers in the context of the Choosing Wisely campaign,26, 27 and appropriate use criteria were issued.28 Indeed, it was reported in a national sample of hospitals that performing a diagnostic coronary angiography in asymptomatic patients was associated with higher rates of inappropriate PCI and lower rates of appropriate PCI.29 Further, although our group reported a small increase in coronary angiography use from 1990 to 2004, there was an estimated 76% increase in “negative” angiography during that period.10 Thus, improved pre‐procedure risk stratification and higher thresholds for coronary angiography likely played an important role in the decline in use between 2000 and 2018.
In addition, the adoption of CT angiography and current appropriate use criteria for CT angiography, which include diagnosis and risk assessment in patients with low or intermediate pretest probability of CAD, changed clinical practice.30 The decline in coronary angiography likely reflects the adoption of CT angiography. Recently reported clinical data from Olmsted County by our group support this assumption,31 and the present report furthers this hypothesis since inclusion of CT angiography in our usage rates substantially offsets the declining use of invasive angiography in recent years.
Trends in the Prevalence of Angiographic CAD
Assessing trends in the prevalence and severity of anatomic CAD in the population is inherently challenging. While only angiography can provide such data in vivo, the use of angiography in the source population must be considered to draw inference from procedural data to the population. Over the present study period, the introduction of CT angiography provided clinicians with the opportunity to visualize the coronary anatomy directly and non‐invasively, thereby increasing the overall community use of angiography (invasive and non‐invasive combined). This, in turn, can be expected to lower the pre‐test probability of CAD among patients studied and consequently reduce the prevalence of any angiographic CAD. Importantly, however, the introduction of CT angiograms will not impact trends in the prevalence of severe CAD and of revascularization, which thus remain important bellwethers of the burden of significant CAD in the population. Our data support these concepts as most recently the prevalence of any CAD declined but the severity of CAD, which had previously declined, stabilized between 2010 and 2018.
Trends in CABG and PCI
A temporal decline in CABG surgery rates had been consistently documented.13, 14, 15, 16, 18 For PCI, the trends during the 2000s were mixed,13, 14, 15, 16, 17, 18 with evidence of a decline in usage outpaced by the decline in CABG surgery in the second decade of the 21st century. Over a similar period (2009–2014), Desai et al32 reported a decline in non‐acute PCIs within the NCDR (National Cardiovascular Data Registry)‐CathPCI Registry. However, these results are now several years old and cannot be compared with ours since the NCDR‐CathPCI Registry32 reports on data from a voluntary registry, subject to participation bias, while we relate the current comprehensive experience of a single community. The present data are important as they indicate that the decline in revascularization has now ceased, which is consistent with our aforementioned observation that the decline in the severity of CAD has also ended.
Limitations, Strengths, and Implications
Some limitations should be acknowledged to interpret our findings. The results emanate from a single community which may limit the generalizability to groups underrepresented in the population. However, the population of Olmsted County is representative of the state of Minnesota and the Upper Midwest region of the United States. Furthermore, age‐ and sex‐specific mortality rates are similar for Olmsted County, the state of Minnesota, and the entire United States, and broad disease trends in Olmsted County are commensurate with national trends which support the broad relevance of our data.20 Our data do not include referral indications; therefore inferences about changes in practice patterns over the study period cannot be directly drawn from these findings.
Conversely, our study has several important strengths. Examining the results of coronary angiography is seldom feasible in a defined population, and yet it constitutes the only possible approach to assess in vivo the prevalence of anatomic CAD. These data have important implications for understanding the evolution of coronary disease in the population. Taken collectively, our analyses of recent temporal trends in the use of coronary angiography, prevalence and severity of anatomic CAD, and revascularization practices indicate that the favorable trends noted in previous decades have vanished as we uncovered a leveling off in CAD severity and revascularization procedures in most recent years. These data must be interpreted in the context of trends in the incidence and mortality of clinical coronary disease. Over a period ending approximately in 2010, we reported a large reduction in the incidence of clinical coronary disease in Olmsted County.1, 2, 33 The temporal decline in the prevalence and severity of anatomic CAD on angiography during the first part of the period, as reported herein, is congruent with the evolution of clinical events and supports the effectiveness of primary prevention, including smoking cessation,34 treatment of hypertension,35 and dyslipidemia.36
However, most recently new mortality data raised considerable concern6, 37 as, since 2011, the number of deaths from all cardiovascular (CVD), heart disease, and stroke has been increasing, and the rates of decline of mortality slowed down. The increase in absolute number and age‐adjusted rates of deaths attributable to CVD are worrisome signals begging the question of whether we are losing ground in the fight against heart disease in the context of stagnating or increasing rates of obesity and diabetes mellitus.38 The present data, which show a leveling off in the decline in severity of angiographic CAD and in revascularization procedures, are congruent with these adverse mortality trends and should be interpreted as a wakeup call for public health and primary prevention, as well as strong rationale for the implementation of a robust CVD surveillance system.39
Conclusions
The comprehensive experience of a community in the Upper Midwest demonstrates profound changes in diagnostic and revascularization coronary procedures between 2000 and 2018. The use of angiography evolved after the introduction of CT angiograms, and the severity of angiographic CAD initially declined but leveled off most recently. A similar pattern was observed for the use of revascularization. The most recent trends are concerning as they suggest that the burden of coronary disease is no longer declining; this warrants reinvigorated public health, primary prevention, and population surveillance.
Sources of Funding
This study was supported by the National Institutes of Health, Bethesda, MD (R01 HL120957), and made possible by the Rochester Epidemiology Project, Rochester, MN (R01 AG034676) from the National Institute on Aging, Bethesda, MD. The funding sources played no role in the design, conduct, or reporting of this study.
Disclosures
None.
Supporting information
Table S1. Temporal Trends in Coronary Angiography and Coronary Revascularization in Olmsted County, MN, 2000 to 2018
Table S2. Angiography Usage Rates* in Olmsted County, MN, 2000 to 2018
Acknowledgments
We thank Susan Stotz, Ellen Koepsell, and Deborah Strain for their valuable support.
Author contributions: Dr Roger had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Substantial contributions to conception or design of the work, or the acquisition, analysis, or interpretation of data for the work: Gerber, PhD; Weston, MS; Manemann, MPH; Killian, BS; Roger, MD, MPH; Drafting of the work or revising it critically for important intellectual content: All authors; Final approval of the version to be published: All authors.
(J Am Heart Assoc. 2020;9:e015231 DOI: 10.1161/JAHA.119.015231.)
References
- 1. Gerber Y, Weston SA, Jiang R, Roger VL. The changing epidemiology of myocardial infarction in Olmsted County, Minnesota, 1995–2012. Am J Med. 2015;128:144–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 4. Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty‐two‐year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125:1848–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gerber Y, Jacobsen SJ, Frye RL, Weston SA, Killian JM, Roger VL. Secular trends in deaths from cardiovascular diseases: a 25‐year community study. Circulation. 2006;113:2285–2292. [DOI] [PubMed] [Google Scholar]
- 6. Sidney S, Quesenberry CP Jr, Jaffe MG, Sorel M, Nguyen‐Huynh MN, Kushi LH, Go AS, Rana JS. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 2016;1:594–599. [DOI] [PubMed] [Google Scholar]
- 7. Jouni H, Askew JW, Crusan DJ, Miller TD, Gibbons RJ. Temporal trends of single‐photon emission computed tomography myocardial perfusion imaging in patients with coronary artery disease: a 22‐year experience from a tertiary academic medical center. Circ Cardiovasc Imaging. 2017;10:e005628. [DOI] [PubMed] [Google Scholar]
- 8. Gibbons RJ. Is the search for enough moderate‐severe ischemia nearly over? JAMA Cardiol. 2019;4:203–205. [DOI] [PubMed] [Google Scholar]
- 9. Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. [DOI] [PubMed] [Google Scholar]
- 10. Gerber Y, Rihal CS, Sundt TM III, Killian JM, Weston SA, Therneau TM, Roger VL. Coronary revascularization in the community. A population‐based study, 1990 to 2004. J Am Coll Cardiol. 2007;50:1223–1229. [DOI] [PubMed] [Google Scholar]
- 11. Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hahn J, Lessard D, Yarzebski J, Goldberg J, Pruell S, Spencer FA, Gore JM, Goldberg RJ. A community‐wide perspective into changing trends in the utilization of diagnostic and interventional procedures in patients hospitalized with acute myocardial infarction. Am Heart J. 2007;153:594–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Culler SD, Kugelmass AD, Brown PP, Reynolds MR, Simon AW. Trends in coronary revascularization procedures among Medicare beneficiaries between 2008 and 2012. Circulation. 2015;131:362–370; discussion 370. [DOI] [PubMed] [Google Scholar]
- 14. Jones WS, Patel MR, Holleran SA, Harrison JK, O'Connor CM, Phillips HR III. Trends in the use of diagnostic coronary angiography, percutaneous coronary intervention, and coronary artery bypass graft surgery across North Carolina. Am Heart J. 2011;162:932–937. [DOI] [PubMed] [Google Scholar]
- 15. Yeh RW, Mauri L, Wolf RE, Romm IK, Lovett A, Shahian D, Normand SL. Population trends in rates of coronary revascularization. JAMA Intern Med. 2015;175:454–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Riley RF, Don CW, Powell W, Maynard C, Dean LS. Trends in coronary revascularization in the United States from 2001 to 2009: recent declines in percutaneous coronary intervention volumes. Circ Cardiovasc Qual Outcomes. 2011;4:193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bangalore S, Gupta N, Genereux P, Guo Y, Pancholy S, Feit F. Trend in percutaneous coronary intervention volume following the COURAGE and BARI‐2D trials: insight from over 8.1 million percutaneous coronary interventions. Int J Cardiol. 2015;183:6–10. [DOI] [PubMed] [Google Scholar]
- 18. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011;305:1769–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 appropriateness criteria for coronary revascularization: a report by the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2009;53:530–553. [DOI] [PubMed] [Google Scholar]
- 20. St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ III, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kurland LT, Elveback LR, Nobrega FT. Population studies in Rochester and Olmsted County, Minnesota, 1900–1968 In: Kessler IT, Levin ML, eds. The Community as an Epidemiologic Laboratory; A Casebook of Community Studies. Baltimore, MD: Johns Hopkins Press; 1970:47–70. [Google Scholar]
- 22. Melton LJ III. History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. [DOI] [PubMed] [Google Scholar]
- 23. St Sauver JL, Grossardt BR, Yawn BP, Melton LJ III, Pankratz JJ, Brue SM, Rocca WA. Data resource profile: the Rochester Epidemiology Project (REP) medical records‐linkage system. Int J Epidemiol. 2012;41:1614–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Neeland IJ, Patel RS, Eshtehardi P, Dhawan S, McDaniel MC, Rab ST, Vaccarino V, Zafari AM, Samady H, Quyyumi AA. Coronary angiographic scoring systems: an evaluation of their equivalence and validity. Am Heart J. 2012;164:547–552.e541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bergstrahl EJ, Offord KP, Chu C‐P, Beard CM, O'Fallon WM. Calculating incidence, prevalence, and mortality rates for Olmsted County, Minnesota residents: an update. Technical Report Series No. 49. Section of Biostatistics, Mayo Clinic, Rochester, MN, 1992. Available at: https://www.mayo.edu/research/documents/biostat-49pdf/doc-10027851. Accessed January 21, 2020. [Google Scholar]
- 26. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307:1801–1802. [DOI] [PubMed] [Google Scholar]
- 27. Berger J, Moller DE. The mechanisms of action of PPARs. Annu Rev Med. 2002;53:409–435. [DOI] [PubMed] [Google Scholar]
- 28. Patel MR, Bailey SR, Bonow RO, Chambers CE, Chan PS, Dehmer GJ, Kirtane AJ, Wann LS, Ward RP. ACCF/SCAI/AATS/AHA/ASE/ASNC/HFSA/HRS/SCCM/SCCT/SCMR/STS 2012 appropriate use criteria for diagnostic catheterization: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;59:1995–2027. [DOI] [PubMed] [Google Scholar]
- 29. Bradley SM, Spertus JA, Kennedy KF, Nallamothu BK, Chan PS, Patel MR, Bryson CL, Malenka DJ, Rumsfeld JS. Patient selection for diagnostic coronary angiography and hospital‐level percutaneous coronary intervention appropriateness: insights from the National Cardiovascular Data Registry. JAMA Intern Med. 2014;174:1630–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'Gara P, Rubin GD, Kramer CM, Berman D, Brown A, Chaudhry FA, Cury RC, Desai MY, Einstein AJ, Gomes AS, Harrington R, Hoffmann U, Khare R, Lesser J, McGann C, Rosenberg A, Schwartz R, Shelton M, Smetana GW, Smith SC Jr. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–1894. [DOI] [PubMed] [Google Scholar]
- 31. Gibbons RG, Carryer D, Hodge D, Miller TD, Roger VL, Wells AJ. Stress testing in the evaluation of stable chest pain in a community population. Mayo Clin Proc. 2019;pii:S0025‐6196(19)30724‐4 DOI: 10.1016/j.mayocp.2019.08.005. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 32. Desai NR, Bradley SM, Parzynski CS, Nallamothu BK, Chan PS, Spertus JA, Patel MR, Ader J, Soufer A, Krumholz HM, Curtis JP. Appropriate use criteria for coronary revascularization and trends in utilization, patient selection, and appropriateness of percutaneous coronary intervention. JAMA. 2015;314:2045–2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Manemann SM, Gerber Y, Chamberlain AM, Dunlay SM, Bell MR, Jaffe AS, Weston SA, Killian JM, Kors J, Roger VL. Acute coronary syndromes in the community. Mayo Clin Proc. 2015;90:597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cigarette smoking among adults and trends in smoking cessation—United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1227–1232. [PubMed] [Google Scholar]
- 35. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 36. Kuklina EV, Yoon PW, Keenan NL. Trends in high levels of low‐density lipoprotein cholesterol in the United States, 1999–2006. JAMA. 2009;302:2104–2110. [DOI] [PubMed] [Google Scholar]
- 37. Sidney S, Quesenberry CP Jr, Jaffe MG, Sorel M, Go AS, Rana JS. Heterogeneity in national U.S. mortality trends within heart disease subgroups, 2000–2015. BMC Cardiovasc Disord. 2017;17:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 39. Goff DC Jr, Brass L, Braun LT, Croft JB, Flesch JD, Fowkes FG, Hong Y, Howard V, Huston S, Jencks SF, Luepker R, Manolio T, O'Donnell C, Robertson RM, Rosamond W, Rumsfeld J, Sidney S, Zheng ZJ. Essential features of a surveillance system to support the prevention and management of heart disease and stroke: a scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Stroke, and Cardiovascular Nursing and the Interdisciplinary Working Groups on Quality of Care and Outcomes Research and Atherosclerotic Peripheral Vascular Disease. Circulation. 2007;115:127–155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Temporal Trends in Coronary Angiography and Coronary Revascularization in Olmsted County, MN, 2000 to 2018
Table S2. Angiography Usage Rates* in Olmsted County, MN, 2000 to 2018


