Abstract
OBJECTIVE
Daily self-monitoring of blood glucose (SMBG) is essential for type 1 diabetes management yet is challenging during adolescence. Ecological momentary assessment (EMA) is the repeated sampling of behaviors and experiences in real time in the natural environment. The purpose of this study was to evaluate 1) the validity of self-reported SMBG values via text message–delivered EMA surveys compared with objective SMBG values via glucose meters and 2) in-the-moment motivators and barriers to performing SMBG in a pediatric type 1 diabetes population.
Methods
Youth (n = 62, aged 11–21 years) with type 1 diabetes received three text messages daily for 10 days containing surveys inquiring about SMBG engagement. Objective SMBG values were downloaded from glucose meters.
Results
On average, participants reported performing SMBG 4 times/day. Of the self-reported SMBG values, 39.6% were accurate. Inaccurate values included additions (i.e., self-reported value with no objective value), omissions (i.e., objective value with no self-reported value), and alterations (difference between self-report and objective SMBG values ≥10 mg/dL). Of the matched pairs of self-reported and objective SMBG values, 41.3% were altered. Bland–Altman plots determined that the mean difference between self-reported and objective glucose data were −5.43 mg/dL. Participants reported being motivated to check their blood glucose because it was important for their health, and reported barriers included wanting to ignore the task, forgetting, and not having devices.
Conclusion
Youth’s self-reported SMBG values may not align with objective readings. The results of this study can facilitate future research to determine individual factors related to SMBG and accuracy of self-reporting.
Type 1 diabetes is one of the most common pediatric chronic conditions. It affects ∼1.93/1,000 youth in the United States, and the incidence is rapidly increasing around the world (1). If not properly managed, type 1 diabetes can lead to serious health complications and mortality (2). Unfortunately, glycemic stability is especially difficult to achieve in adolescence and young adulthood, leaving youth with type 1 diabetes at high risk for more immediate complications such as diabetic ketoacidosis and severe hypoglycemia (3,4). The T1D Exchange clinic network studied the glycemic control of >16,000 Americans with type 1 diabetes; average A1C levels increased starting around the age of 10 years, peaked at around the age of 18 years, and slowly decreased toward recommended targets throughout adulthood (3). These findings suggest that youth and emerging adults may have difficulty regulating their fluctuating blood glucose levels. Because there is currently no cure for or way to prevent type 1 diabetes, it is crucial to better understand factors that contribute to engagement in diabetes care (5).
One step in achieving improved outcomes in this population is daily self-monitoring of blood glucose (SMBG). Two commonly used products for determining glucose levels are glucose meters and continuous glucose monitoring (CGM) systems (2). At the time this study was in development, CGM devices were not indicated for making treatment decisions; therefore, the focus of this project was on the performance of manual SMBG with a meter. People with type 1 diabetes are advised to perform SMBG at least 4 times/day to assist in maintaining glycemic stability and in-range recommendations (2,6).
Not only is it important for people with type 1 diabetes to perform SMBG, but the accuracy of their SMBG is also crucial. Previous research with self-report methodology indicates that the accuracy of youth’s SMBG values varies greatly (50–74% inaccurate values), with reduced accuracy rates when youth believe health care providers cannot see objective values (7–9). On the other hand, Gonder-Frederick et al. (7) noted that altering test values (e.g., changing a value from 400 to 200 mg/dL) was extremely rare. With objective SMBG data now more readily available to providers and patients, an updated evaluation of the validity of patients’ self-reported SMBG values is warranted. Evaluation of the accuracy of self-reports can provide recommendations on the necessity of reviewing objective device summaries at clinic visits.
Adolescence is associated with a number of complicating factors that contribute to difficulties with glycemic stability. Youth with type 1 diabetes begin to transition to autonomous care during adolescence, a process that has been known to be complicated (5,10). Additionally, pubertal growth can contribute to the decline of glycemic stability, which may be frustrating for patients who adhere to behavioral recommendations (5). Diabetes burnout and distress are highly related to glycemic variability, as are fear of hyperglycemia and hypoglycemia (11,12). Although the literature speaks to the aforementioned broad factors that negatively affect SMBG in the adolescent and emerging adult age-group, to our knowledge, there is limited research on the immediate (e.g., in-the-moment) motivators for and barriers to performing SMBG in this population. Using a method that looks at individual, immediate antecedents to SMBG has the potential to inform future interventions (13).
One technique well suited for evaluating in-the-moment antecedents is ecological momentary assessment (EMA). EMA is the repeated sampling of behaviors and experiences in real time, in the natural environment, and reduces biases that occur when using one-time retrospective self-report methods (e.g., recall bias) (14,15). As opposed to traditional longitudinal studies, EMA offers exponentially more assessment points over time, thus allowing for the study of behaviors, emotions, and experiences in greater detail at the individual level (16,17).
EMA has been validated in many clinical populations and has been used to assess variables such as mood, location, quality of life, self-esteem, and pain (15–19). To date, however, there has been only one study using EMA to assess SMBG behaviors in youth with type 1 diabetes. Mulvaney et al. (20) asked participants to complete brief surveys regarding SMBG behaviors twice daily over the phone for 10 consecutive days. Participants completed 58.9% of the phone surveys; 14% of adolescents reported not engaging in SMBG. Noticing the less-than-optimal response rate to the survey, these authors suggested using text messages instead of phone calls because adolescents typically communicate via text more frequently than via phone (20,21). Approximately 95% of teens and 96% of young adults in the United States have access to or own a smartphone; thus, texting may be a viable option for EMA survey prompts (22,23).
The purposes of this study were to assess 1) the accuracy of EMA self-reported SMBG values relative to actual SMBG meter data and 2) self-reported in-the-moment motivators for and barriers to performing SMBG in a pediatric population with type 1 diabetes. Based on previous literature (7), we hypothesized that youth would report accurate SMBG values ∼50% of the time. Furthermore, we hypothesized that common motivators for checking blood glucose would be more internally driven (i.e., motivated by personal drive), whereas barriers to SMBG would be externally driven (i.e., environmental or social consequences).
Research Design and Methods
Participants
Participants were recruited during their routine diabetes appointments at the pediatric endocrinology clinic affiliated with the authors’ institution between May and December 2016. Patients were recruited if they were between the ages of 11 and 21 years, had been diagnosed with type 1 diabetes a minimum of 6 months before their appointment, did not report having any severe cognitive or learning disorders that might impede their ability to participate in research study questionnaires, had daily access to a personal smartphone for at least 2 weeks, and were either able to download their SMBG device data remotely (i.e., via Diasend software) or return to the clinic within the following 2 months to have their devices downloaded. The enrollment target of 80 was informed by previous EMA studies (20,24).
Procedures
The University of Florida institutional review board approved all study procedures. Patients who met eligibility criteria via clinic medical record review were approached by research staff at routine diabetes appointments. All interested and eligible patients (n = 74) completed an informed consent/assent, a demographics survey, and a text message preference survey at enrollment. At this time, participants also provided their usual mealtimes and were able to report separately for weekends and weekdays.
Participants received three text messages per day for 10 consecutive days, individually programmed to be sent at around their reported typical mealtimes (i.e., texts were sent 30 minutes after their reported typical breakfast, lunch, and dinner times to provide a 30-minute variability window). Text messages were sent to each participant beginning the Monday after they gave consent. Mealtimes were chosen because this is a consistent daily time when people with type 1 diabetes are advised to perform SMBG to determine the correct amount of insulin to administer for the upcoming meal (2). Although national guidelines recommend that people with type 1 diabetes perform SMBG at least 4 times/day, we chose to send EMA surveys at mealtimes because we assumed that most youth would likely eat at least 3 times/day. We intentionally did not include other recommended SMBG times (i.e., just after waking or before going to bed) because these times had the potential to cause participants to feel burden or annoyance (e.g., if they received a text after already going to bed or before waking up).
Each text contained a link to a Research Electronic Data Capture (REDCap) survey inquiring about SMBG around their meal. REDCap is a secure, Web-based application designed to support data capture for research studies hosted at the authors’ institution (25). Participants were encouraged to answer the surveys immediately.
After 10 days of receiving texts, participants were asked to submit their SMBG data by either downloading data remotely via Diasend software or by returning to the clinic so study staff could download the data. After completing all study procedures, participants received $10 each.
Measures
SMBG Adherence Survey via REDCap
Participants were queried 3 times/day via texts containing REDCap survey links. A medical appointment reminders company, ClientTell Services, sent the texts. Survey questions were developed after reviewing common motivators and barriers described in the literature, speaking with patients, and discussing the survey project with endocrinology clinic team members. Each survey asked the same set of questions:
Did you check your blood glucose the last time you ate?
If so, what time did you check?
What was your blood glucose the last time you checked?
Why did/didn’t you check?
Possible responses to the question about SMBG timing included morning (6:00–11:00 a.m.), afternoon (11:30 a.m. to 3:00 p.m.), late afternoon (3:30–5:00 p.m.), evening (5:30–8:00 p.m.), and late evening (8:30 p.m. to bedtime). We chose to ask broadly whether participants checked “around mealtimes” as opposed to the recommended 20 minutes before meals because we wanted to account for those youth who may check mid- or postmeal. This decision allowed us to focus on our aims of assessing SMBG value accuracy and motivators/barriers to SMBG instead of other questions about adherence behaviors.
Possible responses regarding why they performed SMBG included:
I didn’t want to upset my parents.
It’s important for my health.
I don’t want to upset my doctor(s).
I have a medical appointment coming up soon.
I’m afraid of highs/lows.
I didn’t check yet.
The responses explaining why a participant did not check blood glucose included:
I forgot.
I’m ignoring that right now.
I didn’t want to check in front of other people.
I didn’t have my meter with me.
I didn’t need to check yet today.
For both questions, participants could select as many of the responses that applied to that moment.
Glucose Meter Data
SMBG data were obtained for the 10 days in which participants completed the EMA portion of the study at diabetes clinic appointments or via transmission to the clinic with Diasend software on personal computers. Participants were asked to submit all meter data captured during the 10-day period of receiving texts; therefore, some participants provided data from multiple meters. If a participant was not able to directly download SMBG data, paper records were obtained; in those instances, participants were asked to have a parent or legal guardian fill out paper diaries based on the information in the glucose meter, which serves as an adequate substitute for SMBG glucose meter data (26). Glucose meter data reports included both timestamps of when each blood glucose check was conducted and the corresponding glucose value. The data from these reports were then manually compared with the self-reported SMBG data (via EMA surveys) by matching timestamps from the objective data to self-reported times checked (i.e., answers to question 2 of the survey).
Statistical Analyses
Descriptive analyses determined the percentage of reported motivators for and barriers to SMBG. To evaluate the accuracy of the self-reports sent via REDCap surveys compared with the objective glucose meter data, all SMBG values were categorized into one of four classifications based on previous research: 1) accurate, 2) addition, 3) alteration, or 4) omission (8). Additions represented when there were self-reported SMBG values that were not contained in the objective readings. Omissions represented when there were objective SMBG values that were not reported in the self-reported SMBG values. Values were considered accurate if the absolute value of the difference between self-reported and objective SMBG readings was ≤10 mg/dL (7). Finally, alterations represented any instance in which the absolute value of the difference between self-reported and objective SMBG readings was >10 mg/dL.
Data management and analyses were conducted using SAS v. 9.4 statistical software. Initial descriptive analyses were conducted on the group of participants with any collected SMBG data, including additions, omissions, alterations, and accurate values. Additional analyses were conducted among participants who had matched pairs of self-reported SMBG values and objective values. Two sets of matched pairs were created: 1) all instances in which participants completed a REDCap survey indicating that they performed SMBG and there was an associated objective meter value recorded on the same date, closest to and before the time indicated on the REDCap survey timestamps, and 2) matched pairs within a valid time window, defined as instances in which objective meter timestamps were verified to have been within the self-reported SMBG time window (i.e., the time window during which participants self-reported having performed SMBG). Among matched self-report and objective data, descriptive analyses were conducted to determine the rate of alterations and accuracies. The level of agreement between self-reported and objective SMBG data and patterns of under- and over-reporting of self-reported blood glucose levels were examined via Bland–Altman plots.
Results
Demographics
Clinic staff approached 191 individuals and asked whether they were interested in participating in the study (Figure 1). Seventy-four individuals consented to participate in the study. Of those who declined to participate, 46 were not interested, 35 had no way to upload their meter data or could not return to the clinic, 28 did not have access to a smartphone, 2 had issues with their meters, 1 did not come with a caregiver to the appointment, and 5 had another reason they could not participate. Of the 74 who consented, two asked to withdraw from the study before any text messages were sent to them. Ten did not answer any texts and were lost to follow-up; the researchers could not be certain these participants received the text messages (e.g., they could have given the wrong phone number or blocked the number sending texts). Thus, the sample consisted of 62 youth, most of whom were male (56.5%) and Caucasian (75.8%). Of these 62 participants, 11 began receiving texts and then asked to stop receiving texts messages and be dropped from the study; their data before withdrawal were included in analyses.
FIGURE 1.
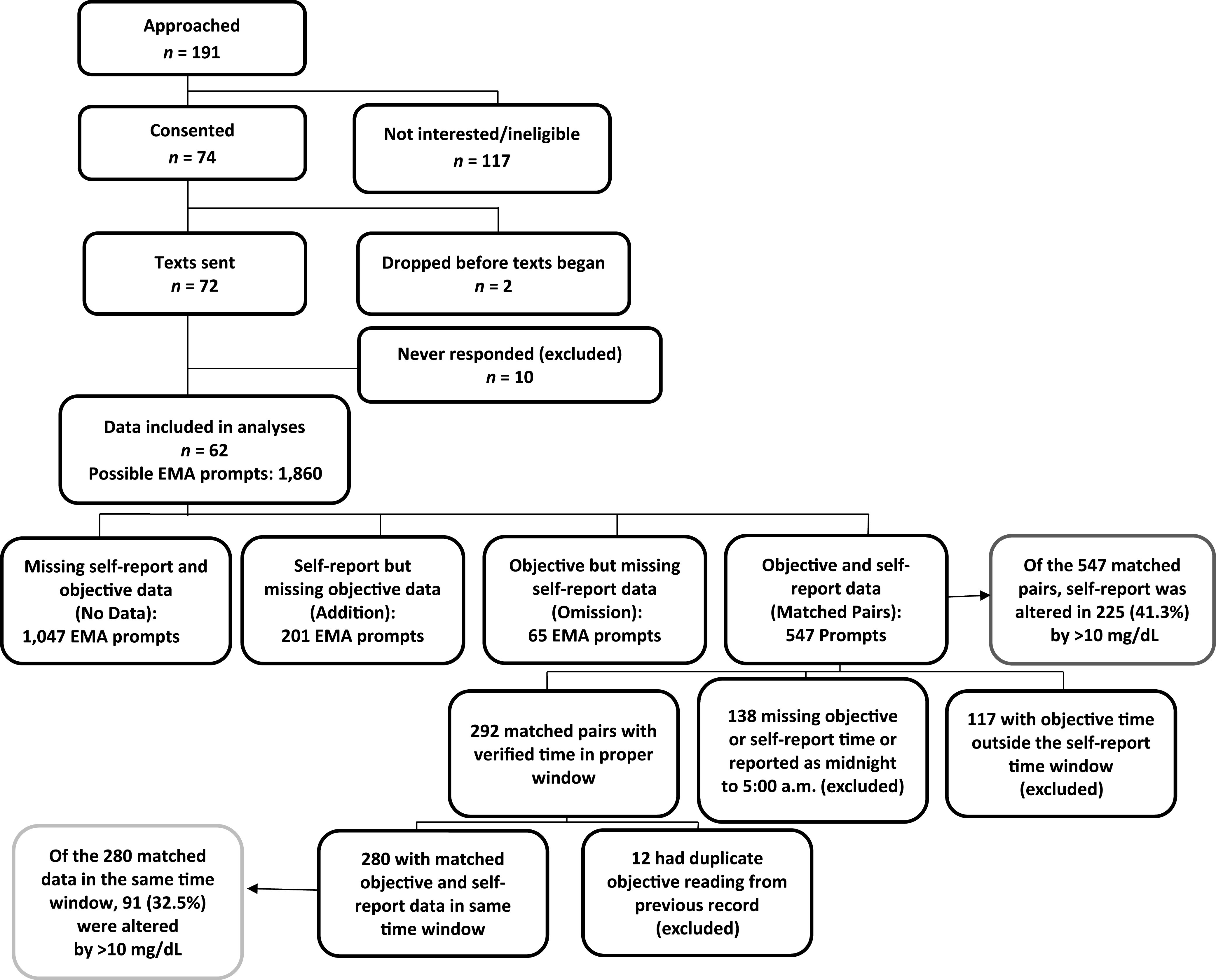
Consort diagram.
On average, the participants in this study had been diagnosed with type 1 diabetes for 7.1 ± 4.3 years and were 16.4 ± 3 years of age (range 11–21 years). Although we did not collect information regarding participants’ insurance coverage, more than half of the patients seen at the clinic from which the sample was drawn are publicly insured. On average, participants self-reported performing SMBG 4.4 ± 1.8 times/day; there was no difference in self-reported SMBG frequency between participants with insulin pumps and those on a multiple daily injection (MDI) regimen. Nearly half (49.2%) of the sample reported using a CGM system, although usage varied from 4 times/year to every day.
Two-tailed independent t tests and χ2 tests (α = 0.05) revealed that participants who either dropped from the study before texts began or were lost to follow-up (combined n = 12) did not differ significantly from those who were included in the final analysis (n = 62) with regard to sex, age, total family income, or phone type. However, there was a significant difference with regard to race [χ2 (3) = 8.232, P = 0.041] such that 6 of 57 Caucasian, 4 of 7 African American, 1 of 6 Hispanic or Latino, and 0 of 2 Asian-American individuals dropped out of the study. Table 1 provides demographic data.
TABLE 1.
Demographics of Overall Study Participants and Those Included in Subgroup Analyses
| Overall (n = 62) | Participants With Valid EMA Surveys and Matched Objective Data (n = 38) | |
|---|---|---|
| Male | 35 (56.5) | 21 (55.3) |
| Race/ethnicity | ||
| Non-Hispanic white | 47 (75.8) | 31 (81.6) |
| Non-Hispanic black | 3 4.8) | 2 (5.3) |
| Non-Hispanic Asian/Pacific Islander | 2 (3.2) | 1 (2.6) |
| Hispanic | 9 14.5) | 4 (10.5) |
| Did not report | 1 (1.6) | — |
| Age, years | 16.4 ± 3.0 (11.0, 21.0) | 16.2 ± 3.1 (11.0, 21.0) |
| Family income | ||
| <$20,000 | 3 (4.8) | 2 (5.3) |
| $20,000–39,999 | 12 (19.4) | 8 (21.1) |
| $40,000–59,999 | 6 (9.7) | 4 (10.5) |
| $60,000–79,999 | 6 (9.7) | 2 (5.3) |
| $80,000–99,999 | 3 (4.8) | 2 (5.3) |
| ≥$100,000 | 22 (35.5) | 16 (42.1) |
| Did not report | 10 (16.1) | 4 (10.5) |
| Diabetes duration, years | 7.1 ± 4.3 (1.0, 17.0) | 7.0 ± 4.1 (1.0, 16.0) |
| Mean SMBG frequency, times/day | 4.4 ± 1.8 (2.0, 9.0)* | 4.7 ± 2.0 (2.0, 9.0)† |
| Insulin delivery: insulin pump | 36 (58.1) | 25 (65.8) |
| Insulin delivery: MDI regimen | 26 (41.9) | 13 (34.2) |
| Uses CGM system | 30 (49.2)† | 21 (55.3) |
Data are n (%) or mean ± SD (minimum, maximum).
n missing = 2.
n missing = 1.
EMA Prompt Responses
A total of 1,860 surveys were sent to participants via text message (30 texts per participant). Of these 1,860 messages sent, 816 surveys (43.8%) were answered. Participants ranged from answering 0 of 30 to 30 of 30 surveys received. A univariate ANOVA indicated significant differences in the number of surveys answered on specific days (early versus late in the 10-day survey period) [Welch’s F (9,5.19) = 2.355, P = 0.012]. Post hoc Games-Howell tests revealed that significantly more surveys were answered on days 2–3 than on day 9 (P <0.05) and on days 2–5 than on day 10 (P <0.05). In general, fewer surveys were answered as days in the study increased. A univariate ANOVA revealed a significant main effect of the time of day surveys were answered [Welch’s F (2,1.806) = 3.676, P = 0.026]. Post hoc Games-Howell tests revealed a significant difference between the first and third surveys sent each day (P = 0.035), such that more surveys were answered earlier in the day compared with later (48.2% in the morning vs. 41.2% in the evening).
In the answered surveys, participants indicated 73.2% of the time that they had checked their glucose the last time they ate, 9.3% reported not checking, and 17.5% responded that they had not eaten yet (i.e., did not need to check). The majority of participants (93.7%) reported that they had checked because they recognized it was important for their health. The second most common response (27%) was being afraid of highs and lows, followed by not wanting to upset their doctors (18.5%), not wanting to upset their parents (15.4%), and having a medical appointment coming up (0.33%). The most common response regarding why participants did not check was forgetting (48.7%), followed by choosing to ignore their diabetes (27.6%), not having a meter with them (26.3%), not needing to yet (17.1%), and not wanting to check in front of others (7.9%).
Comparison of Self-Report Data to Glucose Meter Device Data
A total of 813 data points existed among those who provided any self-reported or objective SMBG value recorded at any single record point. Of all the data collected, 24.7% were additions (i.e., self-reported SMBG value reported, but missing objective SMBG value), and 8% were omitted (i.e., objective SMBG present, but no self-reported SMBG value given). In the second analysis including only times when there were matched pairs of self-reported and objective data regardless of time window verification (i.e., whether the timing of self-reported SMBG via survey responses matched the timestamp of the objective reading; n = 547), 41.3% (n = 225) of self-reported values were altered by >10 mg/dL compared with their matching objective value. To put in perspective the difference between reported and objective SMBG values, a Pearson’s correlation between these altered matched pairs only was conducted. Results indicated that self-reported and objective SMBG data only correlated at 0.3 (P <0.01), indicating a high degree of discrepancy. In a third analysis conducted only for matched pairs that were within a valid time window (e.g., participant reported checking between 6:00 and 11:00 a.m. and there was a meter value timestamped during that same window of time; n = 280), 32.5% (n = 91) of self-reported SMBG values were altered >10 mg/dL, and 67.5% of matched values were accurate. No significant differences existed between sexes or age-groups (11–15 vs. 16–21 years) with regard to number of additions, omissions, alterations, or accurate SMBG values.
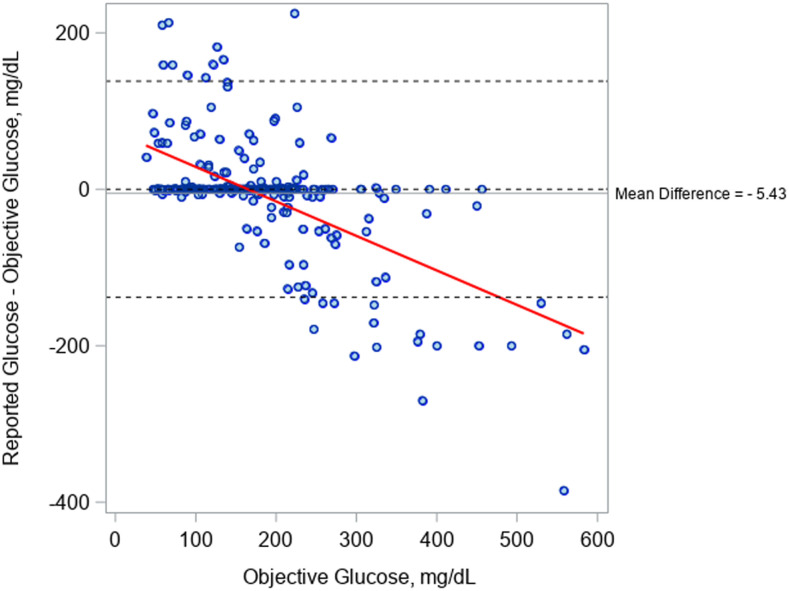
Figure 2 shows the agreement between self-reported and objective SMBG values; a difference of 0 indicates perfect agreement. The Bland–Altman plot mean difference between self-reported and objective glucose data were −5.43 mg/dL, indicating that self-reported SMBG data on average were lower than corresponding objective SMBG data. As objectively measured SMBG increased, there were more instances of underreporting SMBG and less agreement overall. Alternatively, at lower levels of objectively measured SMBG, there were more instances of self-reporting higher values of SMBG.
FIGURE 2.
Bland–Altman plot showing agreement between self-reported and objective SMBG values relative to objective SMBG values.
Discussion
SMBG remains an essential component of glycemic monitoring in people with type 1 diabetes. Unfortunately, youth face many barriers to performing SMBG in general and to reporting their SMBG data accurately (e.g., poor family communication, executive functioning deficits, and psychosocial factors). Ours is one of the first studies to use a text message–delivered EMA design to assess the validity of self-reported SMBG values and self-reported antecedent motivators for and barriers to performing SMBG in a pediatric population with type 1 diabetes. This information is crucial to develop future treatments to assist youth in improving their SMBG behaviors.
Major findings from this study were that youth often self-reported inaccurate SMBG readings, even when they were aware that their self-reports would be compared with objective readings. Furthermore, approximately one-third of the time youth reported not performing SMBG when they should have because they wanted to ignore their diabetes. This choice may be a sign of diabetes burnout or a poor adolescent coping strategy (i.e., not wanting to confront a problem by ignoring it).
EMA Survey Responses
Morning surveys were answered more often than those sent in the afternoon or evening, and this finding directly contradicts the findings of Mulvaney et al. (20). It is likely that text messages are easier for youth to answer compared with phone calls.
Regarding the trajectory of surveys answered over the 10 days, the number of surveys answered decreased over time, with significantly lower response rates during the second week compared with the first week. This finding also contradicts the study by Mulvaney et al. (20), which had a stable response rate over time. One possible explanation is that participants perceived that they would be held more accountable by phone calls than by texts. The depersonalization that likely resulted from the automated text message format (i.e., messages only contained a survey link) may have negatively affected survey response adherence.
Validity of Self-Reported SMBG Values
Our findings indicate that only 39.6% of self-reported SMBG values (via EMA) matched the objective meter values. The rest of the self-reported values (60.4%) were inaccurate (i.e., added, omitted, or altered). These findings differ from those of Gonder-Frederick et al. (7), who used the same categorical labels to assess the validity of self-reported SMBG compared with glucose meter data. That study reported that participants had significantly more omissions than additions, whereas our results are opposite (i.e., many more additions than omissions). These findings might be the result of CGM usage. Those who reported using CGM while participating in the study self-reported using their CGM systems anywhere from rarely to every day; thus, it was difficult to determine how often participants were checking with their CGM device as opposed to manually with a meter. CGM was not approved for nonadjunctive use at the time of this study.
Another difference between our findings and those of Gonder-Frederick et al. (7) was that we found approximately one-third of reported SMBG values to have been altered compared with matched objective data, whereas the previous study indicated that approximately 20% of diaries had altered values. Also, the participants in our study self-reported performing SMBG an average of 4.4 ± 1.8 times/day, whereas participants in the previous study reportedly checked, on average, 2.19 ± 1.09 times/day (7). Since the previous study’s publication, the recommendation in national guidelines for how often to perform SMBG has increased to 4 times/day for people with type 1 diabetes. This recommendation is often discussed with patients at our clinic. It is possible that adolescents in our study were more likely to add SMBG values when they had not actually checked to have a more favorable clinical profile.
Analyzing the frequency of SMBG using objective measures can be complicated because of differences in devices and combinations of devices used. Although further analyzing demographic differences between self-reported and objective SMBG data were outside the scope of this study, our team has proposed methods for such analysis elsewhere (27).
Approximately one-third of our participants altered their self-reported SMBG values based on comparison with their objective values. It is difficult to determine why this occurred without making assumptions. It is possible that participants may have changed some of the values to appear as if they were in more favorable glycemic ranges; however, not all alterations were changed to a more clinically favorable number (i.e., closer to the recommended blood glucose range of 70–180 mg/dL). Some may have reported SMBG values based on an educated guess without verifying with their meters. Others may have reported previous values from earlier in the day that did not reflect current values. Still others may have been using their CGM device to monitor their blood glucose. Either way, our findings differ significantly from those of Gonder-Frederick et al. (7), who concluded that alterations were extremely rare. Future research is recommended to examine the potential for, reasons for, and predictors of these discrepancies.
Antecedent Motivators for and Barriers to Performing SMBG
EMA responses regarding immediate motivators for performing SMBG showed that most youth reported being motivated by the knowledge that SMBG is important for their health. It is well supported in the literature that youth typically are less motivated to make behavioral changes that align with a healthy lifestyle (e.g., quitting or refraining from smoking or following a healthy eating plan) because of future long-term health goals and rather are motivated by immediate consequences such as feeling good and their appearance. The response option “It’s important for my health” in our survey was too broad to determine whether youth understood this response as a long-term or immediate health consequence. Because nonengagement with diabetes treatment recommendations causes immediate health consequences, one can assume that this statement potentially relates to more immediate health effects. It is also possible that youth selected this response because they thought it was what their doctors or the researchers would want to hear (i.e., response bias).
Additionally, 27% of the time, youth reported that they performed SMBG because of fear of having too high/low blood glucose levels. This finding is consistent with the literature (11,12). Although this anxiety propels youth to adhere to treatment recommendations, it also underscores the need for an additional area of intervention—namely, providing coping skills for diagnosis-related anxiety. Numerous studies have shown that youth with higher general anxiety have lower SMBG frequency and higher blood glucose values (11,12,28). Although some level of anxiety may be useful for motivation, long-term and increased anxiety can lead to poor engagement with diabetes-related treatments and medical complications (e.g., somatic symptoms).
Participants who reported not checking their blood glucose at mealtimes most commonly reported that they had forgotten to check (48.7%) or did not have their glucose meters with them (26.3%). This finding is supported by literature regarding executive function development in youth; it is more difficult for youth to plan and follow through with self-management tasks (10,29). These results provide evidence that poor planning and difficulty following through on diabetes care is still a challenge in this population. On the other hand, although CGM systems were not approved for treatment decisions during data collection for this study, it is possible that some of the youth were using their CGM device rather than their glucose meter to check their glucose. There was no response in the survey to capture this then off-label behavior.
Notably, 27.3% of the time, youth did not perform SMBG and selected “I’m ignoring that right now” as the barrier. Diabetes burnout is an understudied aspect of diabetes treatment engagement; it has been described as a time when patients with type 1 diabetes realize that adhering to treatment is important for their health but lack the motivation to do so (30). The literature suggests that diabetes-related emotional distress (i.e., anxiety, depressive symptoms, and fear) may inhibit youth with type 1 diabetes from participating in their treatment regimens (31,32). Peyrot and Rubin (31) suggest that clinicians should identify patients who are suffering from diabetes-related distress, apply effective treatments to relieve the distress, and refer patients for mental health services when appropriate.
EMA data collection may be a way to identify patients at-risk for diabetes burnout. Furthermore, future studies should aim to better understanding the factors behind participants reporting that they ignore diabetes self-care behaviors. Such data were not collected in this study, but there may have been many reasons for participants to ignore SMBG, including not wanting to check in front of other people, not being able to check at a given time, being afraid of the results, avoiding an injection, or not wanting to put forth the effort needed to engage in the task. Future research using more detailed qualitative data collection methods may parse this issue further.
Limitations
Several limitations should be considered when interpreting these results. The sample was limited to those who had access to a smartphone. Many in the sample (42.3%) reported total family income >$100,000. Both of these factors limit generalizability. Moreover, the survey prompts were not time-sensitive to account for participants who may not have had data plans (i.e., those who could only answer the prompts when they had WiFi access later in the day). As a result, some of the responses may have been delayed, reducing the “in-the-moment” advantage of EMA. Also, study staff were unable to check for accuracy of meter timestamps, particularly for participants who submitted their data via Diasend software from personal computers. Thus, it is possible that some discrepancies were the result of faulty meter timestamps. Finally, we dropped participants from the study who did not answer any of the texts because we could not be certain whether they had received the messages in the first place. A selection bias may have existed toward youth who were more likely to perform diabetes care tasks.
Replication of this study design is encouraged, particularly replication involving complete objective data, CGM, and more control over the technology (e.g., sending texts and using an independent app). Future interventionists may consider the results from our study to design just-in-time adaptive interventions using mobile technologies that could have the ability to notify patients in the moment when they need to adhere to treatment (13).
Future studies also should be designed to accommodate advances in diabetes technology, particularly the growing prevalence of CGM and automated insulin delivery systems. For the foreseeable future, these new technologies will still require diabetes self-care behaviors to be performed by adolescents and emerging adults. By way of example, interventions could focus on psychosocial treatment prompts such as reminders about coping skills to reduce diabetes-related burnout and anxiety or to increase SMBG diabetes care behaviors such as delivering insulin before meals.
Conclusion and Implications for Clinical Care
This study was the first to use a text message–delivered EMA design and the first to use EMA to validate self-reported SMBG values in this population. Our results indicate that youth with type 1 diabetes are likely to self-report inaccurate blood glucose values; therefore, clinical adjustments of insulin doses should rely on valid measures of glucose as opposed to self-reported SMBG values.
This study also highlights the need for further research into individual diabetes-specific treatment adherence barriers and motivators to expand on responses about motivators such as “It’s important for my health” and barriers such as “I’m ignoring that right now.” Clinical trials that study similar patient populations should consider incorporating measures that use objective SMBG values given the potential discrepancies between self-reported and objective values. Clinicians and interventionists would benefit from considering how youth’s tendency to want to ignore their diabetes may affect their treatment adherence.
Clinicians who treat youth with type 1 diabetes should consider that self-reported data may not be accurate, and therefore it is crucial to evaluate and make recommendations based on objective data. To improve access to objective data for medical decision-making, clinicians should facilitate the use of CGM and continue to advocate for improved access to CGM for all patients. Clinicians should also be aware that misreporting data provides insights into behavioral barriers to self-care. For example, a teen may be choosing to ignore diabetes, but this may be only the first indication of a more formidable barrier such as diabetes burnout, stigma, or bullying. Clinicians may be able to determine the root of each patient’s barriers by using motivational interviewing techniques and asking questions using an open and nonjudgmental approach to evoke discussion with their patients. It is possible that addressing such issues may be a more important clinical intervention than narrowly focusing on SMBG adherence and insulin dosing to improve patients’ glycemic stability.
Article Information
Acknowledgments
The authors acknowledge the patients and families who participated in this study, as well as the clinic staff who assisted in downloading meter data. The authors also acknowledge the research assistants and volunteers who recruited participants for the study and diligently input data.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
J.L.W. researched data and wrote the manuscript. S.C.W. researched data. A.A.-O., S.L.F., D.M.J., and M.J.H. reviewed/edited the manuscript. D.S. contributed to discussion and reviewed/edited the manuscript. D.M.J. is the guarantor of this work, and as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Dabelea D, Mayer-Davis EJ, Saydah S, et al.; SEARCH for Diabetes in Youth Study . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Diabetes Association 7. Diabetes technology: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S77–S88 [DOI] [PubMed] [Google Scholar]
- 3.Miller KM, Foster NC, Beck RW, et al.; T1D Exchange Clinic Network . Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care 2015;38:971–978 [DOI] [PubMed] [Google Scholar]
- 4.Rewers A, Chase HP, Mackenzie T, et al. Predictors of acute complications in children with type 1 diabetes. JAMA 2002;287:2511–2518 [DOI] [PubMed] [Google Scholar]
- 5.Chiang JL, Maahs DM, Garvey KC, et al. Type 1 diabetes in children and adolescents: a position statement by the American Diabetes Association. Diabetes Care 2018;41:2026–2044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Driscoll KA, Johnson SB, Hogan J, Gill E, Wright N, Deeb LC. Insulin bolusing software: the potential to optimize health outcomes in type 1 diabetes mellitus. J Diabetes Sci Technol 2013;7:646–652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonder-Frederick LA, Julian DM, Cox DJ, Clarke WL, Carter WR. Self-measurement of blood glucose: accuracy of self-reported data and adherence to recommended regimen. Diabetes Care 1988;11:579–585 [DOI] [PubMed] [Google Scholar]
- 8.Mazze RS, Shamoon H, Pasmantier R, et al. Reliability of blood glucose monitoring by patients with diabetes mellitus. Am J Med 1984;77:211–217 [DOI] [PubMed] [Google Scholar]
- 9.Wilson DP, Endres RK. Compliance with blood glucose monitoring in children with type 1 diabetes mellitus. J Pediatr 1986;108:1022–1024 [DOI] [PubMed] [Google Scholar]
- 10.McNally K, Rohan J, Pendley JS, Delamater A, Drotar D. Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care 2010;33:1159–1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonder-Frederick L, Nyer M, Shepard JA, Vajda K, Clarke W. Assessing fear of hypoglycemia in children with type 1 diabetes and their parents. Diabetes Manag (Lond) 2011;1:627–639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Majidi S, Driscoll KA, Raymond JK. Anxiety in children and adolescents with type 1 diabetes. Curr Diab Rep 2015;15:47. [DOI] [PubMed] [Google Scholar]
- 13.Nahum-Shani I, Hekler EB, Spruijt-Metz D. Building health behavior models to guide the development of just-in-time adaptive interventions: a pragmatic framework. Health Psychol 2015;34S:1209–1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stone A, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Ann Behav Med 1994;16:199–202 [Google Scholar]
- 15.Stone AA, Schwartz JE, Neale JM, et al. A comparison of coping assessed by ecological momentary assessment and retrospective recall. J Pers Soc Psychol 1998;74:1670–1680 [DOI] [PubMed] [Google Scholar]
- 16.Hedeker D, Mermelstein RJ, Berbaum ML, Campbell RT. Modeling mood variation associated with smoking: an application of a heterogeneous mixed-effects model for analysis of ecological momentary assessment (EMA) data. Addiction 2009;104:297–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol 2008;4:1–32 [DOI] [PubMed] [Google Scholar]
- 18.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol 2010;15:1–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stein KF, Corte CM. Ecologic momentary assessment of eating-disordered behaviors. Int J Eat Disord 2003;34:349–360 [DOI] [PubMed] [Google Scholar]
- 20.Mulvaney SA, Rothman RL, Dietrich MS, et al. Using mobile phones to measure adolescent diabetes adherence. Health Psychol 2012;31:43–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lenhart A. Teens, smartphones & texting. Available from https://www.fitsnews.com/wp-content/uploads/2012/03/PIP_Teens_Smartphones_and_Texting.pdf. Accessed 28 September 2019
- 22.Pew Research Center Mobile fact sheet. Available from https://www.pewinternet.org/fact-sheet/mobile. Accessed 18 June 2019
- 23.Anderson M, Jiang J. Teens, social media & technology 2018. Available from https://www.pewinternet.org/2018/05/31/teens-social-media-technology-2018. Accessed 18 June 2019
- 24.Mulvaney SA, Ho YX, Cala CM, et al. Assessing adolescent asthma symptoms and adherence using mobile phones. J Med Internet Res 2013;15:e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guilfoyle SM, Crimmins NA, Hood KK. Blood glucose monitoring and glycemic control in adolescents with type 1 diabetes: meter downloads versus self-report. Pediatr Diabetes 2011;12:560–566 [DOI] [PubMed] [Google Scholar]
- 27.Westen SC, Warnick JL, Albanese-O’Neill A, et al. Objectively measured adherence in adolescents with type 1 diabetes on multiple daily injections and insulin pump therapy. J Pediatr Psychol 2019;44:21–31 [DOI] [PubMed] [Google Scholar]
- 28.Herzer M, Hood KK. Anxiety symptoms in adolescents with type 1 diabetes: association with blood glucose monitoring and glycemic control. J Pediatr Psychol 2010;35:415–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bagner DM, Williams LB, Geffken GR, Silverstein JH, Storch EA. Type 1 diabetes in youth: the relationship between adherence and executive functioning. Child Health Care 2007;36:169–179 [Google Scholar]
- 30.Polonsky W. Diabetes Burnout: What to Do When You Can’t Take It Anymore. Alexandria, VA, American Diabetes Association, 1999 [Google Scholar]
- 31.Peyrot M, Rubin RR. Behavioral and psychosocial interventions in diabetes: a conceptual review. Diabetes Care 2007;30:2433–2440 [DOI] [PubMed] [Google Scholar]
- 32.Weissberg-Benchell J, Antisdel-Lomaglio J. Diabetes-specific emotional distress among adolescents: feasibility, reliability, and validity of the problem areas in diabetes-teen version. Pediatr Diabetes 2011;12:341–344 [DOI] [PubMed] [Google Scholar]