Coagulopathy is a common feature of the coronavirus-2019 (COVID-19) and entails a worse prognosis. Studies have reported conflicting results regarding the effect of anticoagulation treatment on mortality in patients with COVID-19. In this meta-analysis study, we aim to examine the effect of anticoagulation use on mortality in patients with COVID-19. PubMed database was searched for relevant articles. Inclusion criteria were (1) Cohort studies, case series studies, or case reports. (2) The study population included patients with confirmed COVID-19 infection. (3) Use of anticoagulation, whether in therapeutic or prophylactic doses, was reported in the study. (4) Mortality among patients who received anticoagulation was reported in the study or could be calculated and compared with those who did not receive anticoagulation. Mortality rates were pooled using a random effect model. Risk ratio (RR) and its 95% confidence interval (CI) were calculated using the same model. Six studies with a total of 6,390 patients were included. The mortality rate in patients who were taking anticoagulation was 17.4%, whereas it was 20.9% in patients who were not taking anticoagulants (RR 1.17, 95% CI [0.87,1.57]). I2 index was 74%. There is no association between anticoagulation use and mortality in patients with COVID-19 infection.
The coronavirus-2019 (COVID-19) is a current pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A salient clinical feature of this illness is a marked increase in thrombotic and microvascular complications. Coagulopathy is considered a common feature of COVID-19 infection and is associated with poor prognosis.1 A recent report has identified heparan sulfate as a coreceptor for SARS-CoV-2 and suggested that exogenous heparin may provide therapeutic benefits for patients with COVID-19 infection.2 Studies to evaluate the effect of anticoagulation treatment on mortality in patients with COVID-19 are limited and have reported conflicting results. In this meta-analysis study, we examined the effect of anticoagulation use on mortality in patients with COVID-19.
PubMed database was searched for relevant articles using “COVID-19” and “characteristics” and “mortality,” “COVID-19” and “heparin,” COVID-19” and “warfarin,” and “COVID-19” and “coagulation” from inception until June 2, 2020. No language restricted was applied. Inclusion criteria were (1) Cohort studies, case series studies, or case reports. (2) The study population included patients with confirmed COVID-19 infection. (3) Use of anticoagulation, whether in therapeutic or prophylactic doses, was reported in the study. (4) Mortality among patients who received anticoagulation was reported in the study or could be calculated and compared with those who did not receive anticoagulation. All other studies were excluded. Review Manager 5.4 was used to perform a random effect model analysis to compare mortality between patients with COVID-19 infection who received anticoagulation and those who did not. RR with its 95% CI was calculated. Cohran's Q and I2 index were used for heterogeneity estimation. Sensitivity analysis was done by excluding one study at a time. Funnel plot was used to assess for potential publication bias.
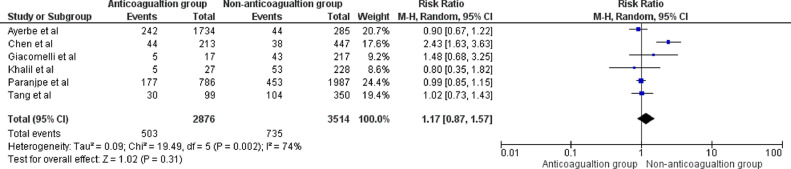
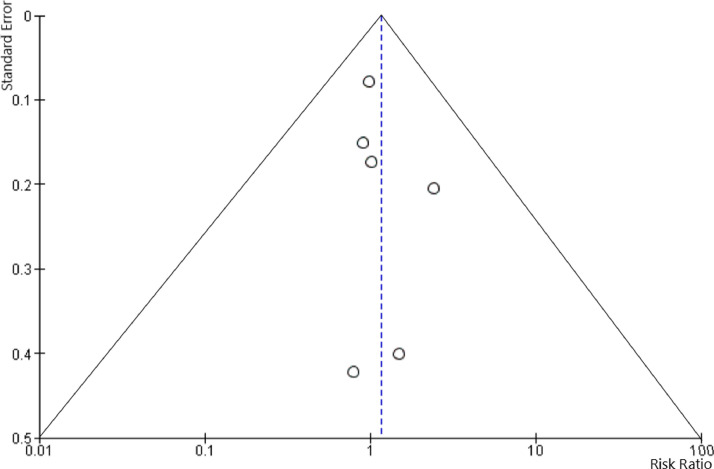
340 studies were initially identified. After careful assessment by applying our inclusion criteria, only 6 studies with a total of 6,390 patients were included. Of those, 2,876 were taking anticoagulants. Heparin was used in 3 studies,3, 4, 5 whereas the type of anticoagulant was not specified in the other 3 studies.6, 7, 8 In one study, heparin was used in prophylactic doses,4 whereas anticoagulation was used in therapeutic doses in 2 studies.6 , 7 The mortality rate in patients who were taking anticoagulation was 17.4%, whereas it was 20.9% in patients who were not taking anticoagulants (RR 1.17, 95% CI [0.87,1.57]). I2 index was 74%. Sensitivity analysis yielded consistent results (Figures 1 and 2 ).
Figure 1.
Forrest plot comparing mortality rates among patients with COVID-19 who received anticoagulation and those who did not.
Figure 2.
Funnel plot to assess for potential publication bias.
Coagulopathy in COVID-19-infected patients is multifactorial and can be explained by Virchow's triad (i.e., hypercoagulability, stasis of flow, and endothelial injury). (1) Hypercoagulability: Systemic infections typically initiate a systemic inflammatory response, which subsequently results in dysregulation of coagulation, platelet activation and leukocyte recruitment. This results in a hypercoagulable state, a concept often referred to as thromboinflammation.9 (2) Hyperviscosity: In acapillary viscometer study in 15 patients with COVID-19 infection, all patients had increased plasma viscosity.10 The hyperviscosity state can lead to endothelium injury and, thus, there is an increased risk for thrombosis in these patients. (3) Endothelial injury (endothelialitis): Endothelial injury is likely the starting point of Virchow's triad in COVID-19. A recent report showed accumulation of viral elements and inflammatory cells within endothelial cells with evidence of endothelial injury in patients with COVID-19 infection.11 This leads to activation of endothelial cells with subsequent expression of procoagulant factors.12
Based on these concepts, anticoagulation has been proposed in COVID-19 patients. However, anticoagulation use in patients with COVID-19 did not have a statistically significant effect on mortality in our analysis.
In an expert consensus statement,12 use of pharmacological prophylaxis with low molecular weight heparin was recommended in severe and critically ill COVID-19 patients at low or moderate risk of bleeding, in mild and moderate COVID-19 patients who have a high or moderate risk of venous thromboembolism based on PADUA or IMPROVE RAM risk scores, and in mild and moderate COVID-19 patients who have a high or moderate risk of venous thromboembolism.
Despite the inherent limitations of meta-analysis and differences in the studies included, analysis of closely matched studies shows no association between anticoagulation use and mortality in patients with COVID-19 infection. Decision to start anticoagulation in patients with COVID-19 should be individualized based on the risks and benefits.
Disclosures
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Bikdeli B, Madhavan MV, Jimenez D. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75 doi: 10.1016/j.jacc.2020.04.031. 2950 LP-2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clausen TM, Sandoval DR, Spliid CB. SARS-CoV-2 infection depends on cellular heparan sulfate and ACE2. Bio RxivPublished online January 1, 2020:2020.07.14.201616. doi:10.1101/2020.07.14.201616 [DOI] [PMC free article] [PubMed]
- 3.Chen F, Sun W, Sun S, Li Z, Wang Z, Yu L. Clinical characteristics and risk factors for mortality among inpatients with COVID-19 in Wuhan, China. Clin Translational Med. 2020 doi: 10.1002/ctm2.40. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ayerbe L, Risco C, Ayis S. The association between treatment with heparin and survival in patients with Covid-19. J Thromb Thrombolysis. 2020:1–4. doi: 10.1007/s11239-020-02162-z. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paranjpe I, Fuster V, Lala A. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76:122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khalil K, Agbontaen K, McNally D. Clinical characteristics and 28-day mortality of medical patients admitted with COVID-19 to a central London teaching hospital. J Infect. 2020 doi: 10.1016/j.jinf.2020.06.027. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giacomelli A, Ridolfo AL, Milazzo L. 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study. Pharmacol Res. 2020;158 doi: 10.1016/j.phrs.2020.104931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson SP, Darbousset R, Schoenwaelder SM. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133:906–918. doi: 10.1182/blood-2018-11-882993. [DOI] [PubMed] [Google Scholar]
- 10.Maier CL, Truong AD, Auld SC, Polly DM, Tanksley C-L, Duncan A. COVID-19-associated hyperviscosity: a link between inflammation and thrombophilia? Lancet (London, England) 2020;395:1758–1759. doi: 10.1016/S0140-6736(20)31209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varga Z, Flammer AJ, Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet (London, England) 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhai Z, Li C, Chen Y. Prevention and treatment of venous thromboembolism associated with coronavirus disease 2019 infection: a consensus statement before guidelines. Thromb Haemost. 2020;120:937–948. doi: 10.1055/s-0040-1710019. [DOI] [PMC free article] [PubMed] [Google Scholar]