Dear Editor,
Chow et al reported a marked decline in influenza incidence in Singapore during the first four months of 2020, likely attributable to public health measures aimed at controlling the coronavirus disease 2019 (COVID-19) pandemic (1). Measures, such as social distancing, mask-wearing, and limiting the size of group gatherings, might also have reduced the transmission of other respiratory infections. We report on the decreased incidence of pneumococcal disease in our institution during the first five months of the COVID-19 pandemic.
Singapore confirmed its first case of COVID-19 on 23 January 2020 (2), following which enhanced surveillance, contact tracing and infection control measures were implemented to contain the disease. When the DORSCON (Disease Outbreak Response System Condition) risk assessment level was raised to Orange on 7 February 2020, further measures including air travel restrictions, stay-home notices for newly returning travellers, and limiting large gatherings were introduced. These culminated in a partial lockdown period from 7 April 2020 (epidemiological week, e-week 15) to 1 June 2020 (e-week 23), termed the ‘Circuit Breaker’. During this period, closure of schools and non-essential workplaces, prohibition of dining in at eateries, and mandatory social distancing and mask-wearing were enacted. These resulted in a significant reduction in the community transmission of COVID-19, from a high of 58 reported community cases in a day at the start, to 0 community cases on the last day of the Circuit Breaker (3). Subsequently, phased reduction of restrictions was implemented, although mask-wearing, social distancing and limitations to group gathering sizes continued to be enforced. As of 19 July 2020 (e-week 30), the number of reported COVID-19 cases in Singapore was more than 47,000, with the majority (n=45,150) of cases being dormitory-based migrant workers on work permits (4).
Streptococcuspneumoniae is transmitted via respiratory droplets and contributes to significant morbidity and mortality in Singapore, especially at the extremes of age (5). Pneumococcal vaccination is recommended for adults aged 65 years and above or who have specific medical conditions; however, it is currently non-mandatory and vaccination rates have been low (6). Tan Tock Seng Hospital (TTSH) is a 1,600-bed adult tertiary care hospital, co-located with the National Centre of Infectious Diseases (NCID), a 330-bed purpose-built facility for centralised management of emerging infectious diseases. As part of routine infectious disease surveillance for these institutions, we reviewed the results of all urinary streptococcal antigen tests performed, as well as the number of notifications submitted to the Ministry of Health for invasive pneumococcal disease (IPD) (a notifiable disease for which reporting is mandatory for all clinicians and clinical laboratories), from the years 2010 to 2020.
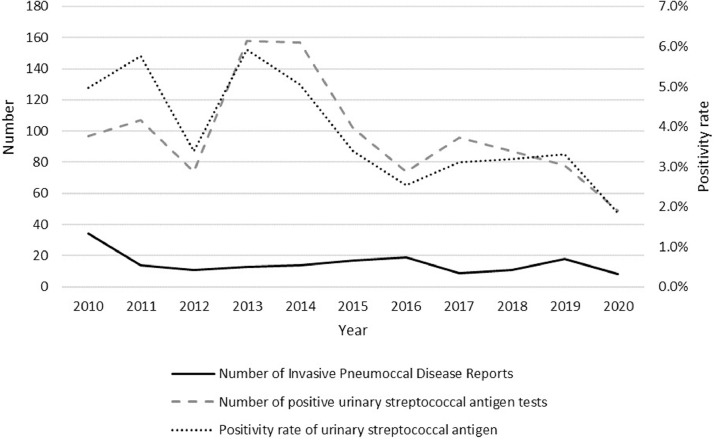
For e-weeks 1-27 of 2020, a total of 49 patients tested positive for urinary streptococcal antigen. For the same period each year for 2010-2019, a median of 96.5 (IQR 78-107) patients tested positive in our hospital (Fig. 1 ).
Fig. 1.
Trend of notification reports submitted to the Ministry of Health for invasive pneumococcal disease (IPD) (solid line), number of positive urinary streptococcal antigen tests (dashed line), and positivity rate of urinary streptococcal antigen tests (dotted line) from 2010 to 2020, e-weeks 1-27.
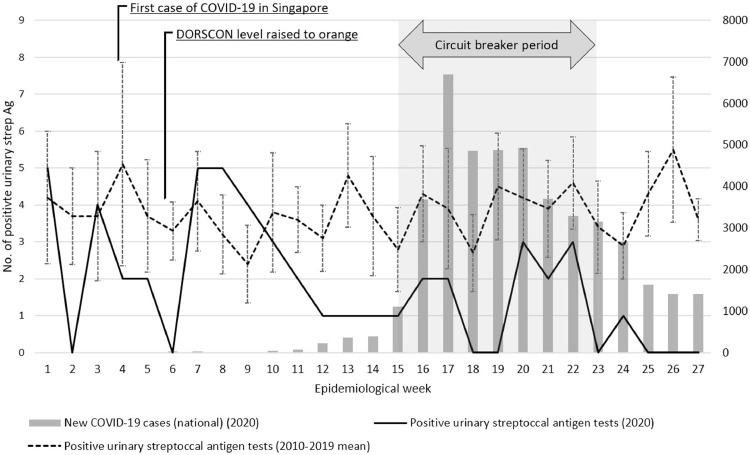
Contrasting 2020’s data against the preceding 10 years by e-week, the mean number of positive urinary streptococcal antigen results in 2020 fell to 1.81/week, from a mean of 3.81/week for the years 2010 to 2019 (standard deviation [SD] 2.38, P<0.0001), from e-weeks 1-27. The mean weekly positivity rate was 1.76% in 2020, a decrease from a mean rate of 4.07% (SD 2.44%, P<0.0001) over the previous 10 years (e-weeks 1-27). Examining the weekly trend, the number of positive urinary streptococcal antigen results started to fall in 2020 from e-week 9 onwards to 0-3 positive results per week, a decrease from the usual trend of 3-5 positive results per week from 2010-2019 (Fig. 2 ). This corresponded with the time period when public health measures to combat COVID-19 were implemented.
Fig. 2.
Number of new COVID-19 cases reported nationally (grey bars), as well as number of positive urinary streptococcal antigen tests from 2020 (solid line) versus the mean from 2010-2019 (dashed line), for e-weeks 1 to 27. Error bars represent the 95% confidence intervals for 2010-2019 data. Annotation of detection of first case of COVID-19, start of DORSCON level orange period, and duration of Circuit Breaker period in 2020.
Comparing the yearly trends from 2010 to 2020 (for e-weeks 1-27 inclusive), the positivity rate of urinary streptococcal antigen testing was 1.84% in 2020, compared to an overall positivity of 3.98% for years 2010 to 2019 (Fig. 1). In addition, the number of notifications to the Ministry of Health for IPD fell to its lowest point of 8 notifications during e-weeks 1 to 27 of 2020, compared to a median of 14 (IQR 11-18, P=0.18) over the previous 10 years during the same period. This is on a background of similar numbers of urinary streptococcus antigen tests carried out in e-weeks 1-27 of 2020 (2660 tests) compared to a median of 2702 tests (P=0.91) in 2010-2019 for the same period.
We postulate that the public health COVID-19 prevention measures introduced in Singapore resulted in an inadvertent decrease in pneumococcal disease transmission. A marked decline in influenza incidence in the first few months of the COVID-19 pandemic has been reported (1, 7). This was also observed in studies from China and other countries in East Asia (8, 9). Similarly, researchers in Taiwan reported record lows of incidence rates of severe complicated influenza and IPD (10). There has not been any widespread national campaigns over the past one year to increase pneumococcal vaccination in the population, no practice changes affecting the ordering of urinary streptococcal antigen tests, and no changes in reporting requirements for IPD, to account for our findings.
Historically, public health messaging for pneumococcal disease prevention has centred around vaccination. While this remains paramount, our study highlights the key role of behavioural and public health measures in reducing the transmission of S. pneumoniae. Accordingly, older adults and high-risk individuals should consider adopting more meticulous infection control practices such as frequent hand hygiene and mask-wearing during seasonal increases in respiratory illnesses, even during non-outbreak periods. At a national level, there is scope for sustained public health education and infection control policies beyond the COVID-19 period to reduce the burden of respiratory infections.
Our study has some limitations. There may have been some altered health-seeking behaviour due to the COVID-19 pandemic, which might have reduced overall presentation to medical facilities. Our data was limited to that from TTSH and NCID, of which the latter is the dedicated national centre for handling COVID-19 cases. Patients may have opted to present elsewhere due to this status. However, we believe this is less likely given that the number of urinary streptococcus antigen tests for e-weeks 1-27 of 2020 (ordered by clinicians based on clinical suspicion for pneumococcal disease) was similar to that for the same period from 2010 to 2019.
In conclusion, we observed a decreased incidence of pneumococcal disease at our institution that corresponded with the time period when public health measures were implemented to control COVID-19, suggesting that these measures had also had an inadvertent effect on the transmission of S. pneumoniae. Behavioural and infection control measures should be considered as part of long-term prevention efforts.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None.
Acknowledgement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Chow A, Hein AA, Kyaw WM. Unintended Consequence: Influenza plunges with public health response to COVID-19 in Singapore. J Infect. 2020;81(2):e68–e69. doi: 10.1016/j.jinf.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong JEL, Leo YS, Tan CC. COVID-19 in Singapore—Current Experience: Critical Global Issues That Require Attention and Action. JAMA. 2020;323(13):1243–1244. doi: 10.1001/jama.2020.2467. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health S. COVID-19 Situation Report 2020 [Available from: https://covidsitrep.moh.gov.sg/.
- 4.Ministry of Health S. 19 July 2020 Daily Report on COVID-19 2020 [Available from:https://www.moh.gov.sg/docs/librariesprovider5/local-situation-report/situation-report-19-jul-2020.pdf.
- 5.Low S, Chan FL, Cutter J, Ma S, Goh KT, Chew SK. A national study of the epidemiology of pneumococcal disease among hospitalised patients in Singapore: 1995 to 2004. Singapore Med J. 2007;48(9):824–829. [PubMed] [Google Scholar]
- 6.Ang LW, Cutter J, James L, Goh KT. Epidemiological characteristics associated with uptake of pneumococcal vaccine among older adults living in the community in Singapore: Results from the National Health Surveillance Survey 2013. Scand J Public Health. 2018;46(2):175–181. doi: 10.1177/1403494817720105. [DOI] [PubMed] [Google Scholar]
- 7.Soo RJJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased Influenza Incidence under COVID-19 Control Measures, Singapore. Emerg Infect Dis. 2020;26(8):1933–1935. doi: 10.3201/eid2608.201229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu D, Lu J, Liu Y, Zhang Z, Luo L. Positive effects of COVID-19 control measures on influenza prevention. International Journal of Infectious Diseases. 2020;95:345–346. doi: 10.1016/j.ijid.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Itaya T, Furuse Y, Jindai K. Does COVID-19 infection impact on the trend of seasonal influenza infection? 11 countries and regions, from 2014 to 2020. Int J Infect Dis. 2020;97:78–80. doi: 10.1016/j.ijid.2020.05.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galvin CJ, Li Y-CJ, Malwade S, Syed-Abdul S. COVID-19 preventive measures showing an unintended decline in infectious diseases in Taiwan. Int J Infect Dis. 2020;98:18–20. doi: 10.1016/j.ijid.2020.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]