Highlights
-
•
SARS-CoV-2 virus was present in the air in the ICU.
-
•
Virus may be discharged in aerosol for days after patients test negative.
-
•
The finding may be one of the reasons for patients` re-detectable positive.
-
•
The clinical guidelines for recovered COVID-19 patients need to be improved.
Abbreviations: COVID-19, coronavirus disease; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; MERS-CoV, Middle East respiratory syndrome coronavirus; RP, re-detectable positive patients; AURI, acute upper respiratory infection; QRT-PCR, quantitative real-time polymerase chain reaction; ORF1ab, open reading frame; NP, nucleocapsid protein; Ct, cycle threshold
Keywords: SARS-CoV-2, Indoor air environment, Aerosol, Ready-for-discharge patient, Re-detectable positive, ICU
Abstract
As coronavirus disease 2019 (COVID-19) is spreading worldwide, there have been arguments regarding the aerosol transmission of its causative agent, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Moreover, some re-detectable positive (RP) patients have been reported. However, little attention has been given to the follow-up of recovered patients, and there is no environmental evidence to determine whether these patients continue to shed the virus after they test negative. Therefore, with an objective to test the hypothesis of airborne transmission of SARS-CoV-2, it is necessary to 1) determine whether SARS-CoV-2 particles are present in the indoor air and 2) determine whether recovered patients are still shedding virus, thus providing much-needed environmental evidence for the management of COVID-19 patients during the recovery period. In this study, surface and air samples were collected from an intensive care unit (ICU) containing one ready-for-discharge patient. All surface samples tested negative, but the air samples tested positive for SARS-CoV-2. This implies that SARS-CoV-2 particles may be shed in aerosol form for days after patients test negative. This finding may be one of the reasons for the observation of RP patients; therefore, there is a need for improved clinical and disease management guidelines for recovered COVID-19 patients.
1. Introduction
Acute upper respiratory infection (AURI) is one of the most widespread infections among humans. Respiratory viruses are a common cause of AURI, which is responsible for approximately 200 million cases of pneumonia worldwide annually (He et al., 2017, Sande, Njunge, Ngoi, Mutunga, & Pollard, 2019). The common cold is the most widespread AURI caused by a virus (Ludwig et al., 2013); other viruses that cause AURI include influenza A, measles, rubella, etc. AURIs are a significant public health problem and a source of increased socioeconomic burden worldwide, as evident by the serious global public health crises caused by multiple AURI pandemics during the course of human history. One hundred two years ago, the first wave of the Spanish influenza (Spanish flu) pandemic occurred in the spring and summer of 1918. Thereafter, a serious epidemic occurred from September through December, spreading widely from France across the globe, thus causing the second pandemic wave. The following year, the Spanish flu spread from Eurasia to Oceania, New Zealand, and Australia, constituting the third wave (Crosby, 1989). During the Spanish flu pandemic, approximately 600 million people were infected (the total world population at the time was 2 billion people)(Lamb, 2001). The morbidity rate was 20% to 40 %; the death toll approximately 20–50 million; and the mortality rate was 2.5%–5%, far exceeding the number of deaths that occurred during the First World War (Taubenberger & Morens, 2006). Another AURI pandemic was severe acute respiratory syndrome (SARS), which occurred in Guangdong, China, in 2002. It first spread to Southeast Asia and then across the globe (China, 2003). The SARS pandemic was not eliminated until mid-2003. According to statistics released by the World Health Organization (WHO) in July 2003, there were 8098 cases of SARS worldwide, involving 32 countries and regions. The global death toll due to SARS was 774, with a case fatality rate of nearly 11 % (Department Of Communicable Disease, 2004). SARS also caused the collapse of patient care services in health care systems due to staff shortages. Since medical and nursing staff were infected with SARS, hospital intensive care units (ICUs) could not be run safely, forcing emergency departments to close down (Caulford,2004;Ahmad,2003;Parry,2003). This was followed by the Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak that occurred in Saudi Arabia in July 2012. According to statistics from the WHO, there were 2494 cases of MERS worldwide from September 2012 to November 2019, involving 24 countries and regions (WHO, 2019). The global death toll due to MERS was 858, with a case fatality rate of 34.4 %, which was even higher than that for SARS (WHO MERS-CoV Research Group, 2013; Assiri et al., 2013). Since AURIs are a serious threat to the health of the world's population and are a large significant obstacle to achieve the goal of building healthy cities via the WHO Healthy Cities Project (TSOUROS, 1995), strengthening preventive and control measures for AURI diseases is vital to reducing the global socioeconomic burden and improving human health globally, paving the way towards building healthy and smart cities.
2. Theory
The transmission of AURIs in humans is generally believed to occur in three ways: 1) inhalation of liquid droplets containing the virus; 2) close contact with infected persons; and 3) contact with surfaces contaminated with respiratory viruses. Moreover, aerosol transmission has been known to play an important role within enclosed spaces. Many traditional AURIs, such as influenza and tuberculosis, as well as many emerging infectious diseases are spread by the airborne route. A retrospective cohort study conducted in Hong Kong in 2003 suggested that aerosol transmission may have been an important transmission route during the SARS epidemic (Yu et al., 2004). Other studies reported that MERS-CoV infection may have been airborne (o, Zhang, Ma, & Zhou, 2020; Ergenekon, Mustafa, & Vedat, 2014). Since the coronavirus disease 2019 (COVID-19) pandemic has spread rapidly, aerosol transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has come into focus. WHO health officials stated that there is still insufficient evidence that SARS-CoV-2 is transmitted through the air, except in certain medical settings such as during intubation. To date, some studies have reported the presence of SARS-CoV-2 particles in the air in isolation rooms from hospitals treating COVID-19 patients (Guo, Wang, Zhang, Li, & Chen, 2020; Joshua L. Santarpia, 2020; Liu, 2020; Yuanfang J, 2020), but other similar studies in Singapore and Hong Kong have failed to detect SARS-CoV-2 particles in the air (Cheng et al., 2020a; Ong et al., 2020). Additional retrospective studies conducted as the SARS-CoV-2 epidemic progressed demonstrated that airborne transmission was one of the most likely mechanisms explaining the spatial pattern of infections. This contention has been highlighted in an open letter signed by 239 scientists from 32 countries that was featured in the Journal of Clinical Infectious Diseases on July 6. Three days later, the WHO published a scientific brief on the web and said that the transmission of SARS-CoV-2 by the aerosol route has not been demonstrated, and much more research is needed. Therefore, it is crucial to find more evidence to confirm whether SARS-CoV-2 is transmitted through the air.
Although all patients in the previous studies had tested positive for SARS-CoV-2 and had COVID-19, little attention has been paid to the follow-up of recovered patients. There have been some reported cases of patients who recovered from COVID-19 but tested positive again a few days later, even though they were quarantined after being discharge, and the re-detectable positive (RP) rate was 14.5 % (Lan, 2020). The reason for this observation remains unclear, and it is uncertain whether RP patients could cause new infections after being discharged. However, even though the pandemic has been largely controlled in several countries such as China and South Korea, RP patients may increase the risk of infection in cities because there are a growing number of patients who tested negative and were then discharged. In addition, there is no environmental evidence confirming whether recovered patients are still shedding SARS-CoV-2 particles; therefore, urgent investigations are needed because it could be one of the reasons for the observed RP patients. Therefore, our study aims to 1) determine whether SARS-CoV-2 particles are present in the indoor air, with an objective to test the hypothesis of airborne transmission of SARS-CoV-2, and 2) determine whether recovered patients are still shedding SARS-CoV-2 particles, thus providing much-needed environmental evidence for the management of COVID-19 patients during the recovery period.
3. Methods
3.1. Study design
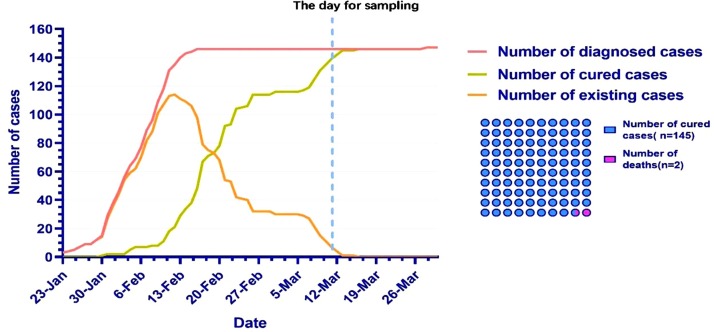
Guizhou Province is located in Southwest China. The first COVID-19 patient was reported on January 22, 2020, and the last patient was reported on March 16, 2020 (Fig. 1 ). Given the total of 147 reported cases, Guizhou is one of the five provinces with the lowest number of COVID-19 patients in China (the other four are Xizang, Qinghai, Ninxia, and Xinjiang) (China, 2020b; Province, 2020).
Fig. 1.
Reported COVID-19 by day in Guizhou province, China. * The data is from the web of health commission of Guizhou province (Province, 2020).
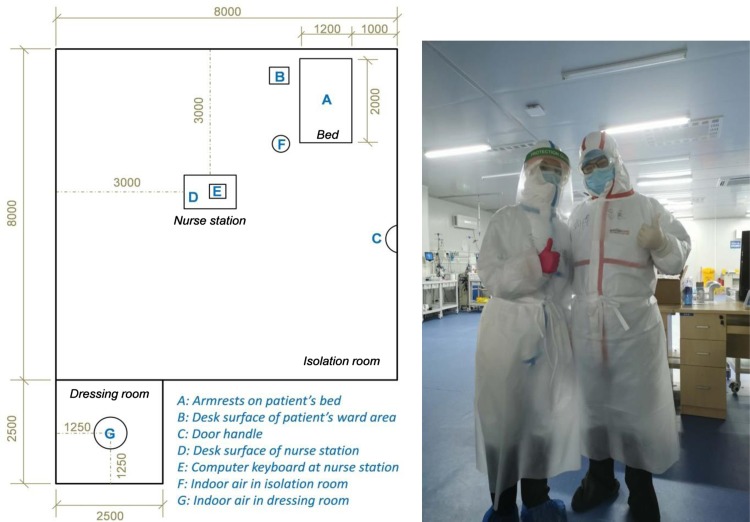
Jiangjunshan Hospital is the only designated hospital for COVID-19 treatment in Guizhou, with a cure rate of 98.64 % (145/147). There are two units in the ICU, including an isolation room and a staff personal protective equipment (PPE) dressing room. The infection prevention and control protocols for each unit include wearing PPE and changing gloves between units that are not removed before exiting the unit, limiting entry and exit into the ICU by staff, and outfitting all units with negative pressure equipment. The ICU was routinely cleaned three times daily at 7:00, 12:00, and 17:00. Routine cleaning included sweeping the floor, wiping the tables with 1000 mg/L chlorine-containing disinfectant, clearing rubbish, and sterilizing the indoor air for 30 min using an ozone disinfection machine. Additionally, the surfaces of all objects were wiped using 75 % medicinal alcohol when staff were free.
The sampling was performed on March 11, 2020 at 19:00, two hours after the completion of routine cleaning, when only one ready-for-discharge patient was isolated and under observation in the ICU at Jiangjunshan Hospital. Two types of samples were taken as shown in Fig. 2 : surface samples were taken from locations A, B, C, D, and E, and high-volume air samples were taken from locations F and G.
Fig. 2.
Schematic view of ICU room (mm).
3.1.1. Air samples
High-volume air samples were collected using a WA 400 Portable viral aerosol sampler (Dingblue Tech, Inc., http://www.dingbluetech.cn/) at 400 L/min for 15 min. (23 ± 1 °C, −15 Pa, RH 45 %), while the patient was present and was not wearing a mask. Air was pumped across an air collection tube and collected into a sterile tube containing 3 mL of viral transport media. Each air collection tube was collected independently to avoid cross-contamination. According to the code for indoor environmental pollution control of civil building engineering GB50325−2010 (2013 Edition) (China, 2013) published by the Ministry of Housing and Urban-Rural Development of the People's Republic of China and the number and density of patients in the ICU at Jiangjunshan Hospital, the two sampling points (F and G) were designed as 1) 0.5 m away from the patient’s bedside in the isolation room and 2) in the middle of the staff PPE dressing room. The sampling height for both locations was 1.5 m. Sampling points were chosen to avoid medical equipment, walls, doors, aisles, and air conditioning vents to prevent obstruction and interference.
3.1.2. Surface samples
To evaluate the efficacy of routine cleaning, we used sterile synthetic fibre swabs with plastic shafts to collect surface environmental samples. Swabs were premoistened with viral transport media and wiped over the surface of the object for a few seconds and then placed immediately into sterile tubes containing 3 mL of viral transport media. Each swab was collected independently to avoid cross-contamination.
3.1.3. Sample analysis
All samples were stored at 4 °C and shipped to the testing laboratory in ice packs within four hours of sampling to test for SARS-CoV-2. Test results were available on the same day. Quantitative analysis of the SARS-CoV-2 ribonucleic acid (RNA) genome was carried out by quantitative real-time polymerase chain reaction (qRT-PCR) according to the technical guidelines for laboratory detection of coronavirus infection (fifth edition) published by the National Health Commission of the People’s Republic of China (China, 2020a). Viral RNA was extracted using the LabServ® Prefilled Viral Total NA Kit-Flex and the Applied Biosystems 7500 System (Thermo Fisher Scientific Inc., Waltham, USA). qRT-PCR assays were performed on SARS-CoV-2 open reading frame 1ab (ORF1ab) and nucleocapsid protein (NP) gene fragments using China Food and Drug Administration (CFDA)-approved commercial Nucleic Acid Diagnostic Kits (PCR-Fluorescence Probing) (Daan Gene Inc., Guangzhou, China) and the Applied Biosystems 7500 System Real-Time PCR Detection System (Thermo Fisher Scientific Inc., Waltham, USA). Every assay consisted of a positive control and a negative control. Data from the samples were further analysed only when both controls produced the expected results; otherwise, the data were considered invalid, and the test was repeated. A sample was considered to have tested positive if either of the two targets (ORF1ab, NP) had an apparent logarithmic phase in the amplification curve, and the cycle threshold (Ct) value was < 40. Otherwise, the sample was considered to be negative if both targets had no apparent logarithmic phase or if the Ct value was ≥40 or indeterminate. In this study, an “intense positive” constituted a positive result from both the ORF1ab gene and the N gene of SARS-CoV-2. In addition, tests were repeated when a sample tested positive. The sample was confirmed to be positive when the second test was also positive.
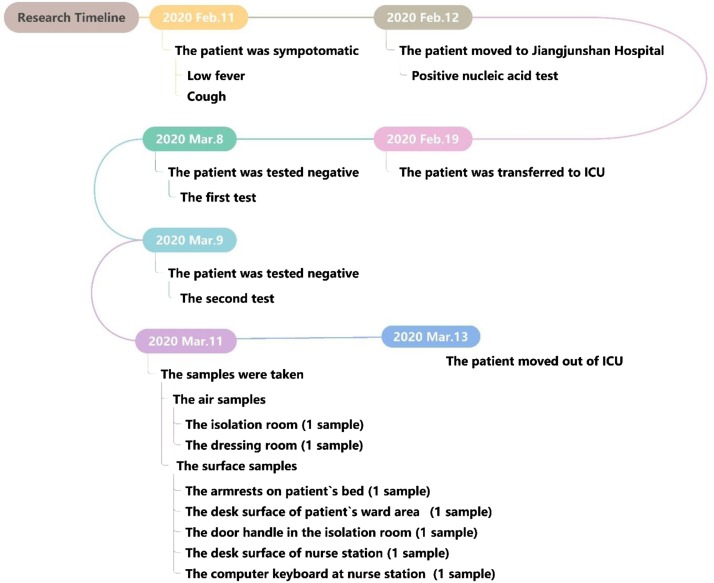
3.2. Patient details
Assessment of the patient epidemiological history revealed that the patient, a 64-year-old female, returned to Guizhou from Wuhan, China, on January 12, 2020, and developed symptoms, including low fewer and cough, on February 11, 2020. On February 12, 2020, she was hospitalized after SARS-CoV-2 infection was confirmed at Jiangjunshan Hospital. The first post-admission chest computed tomography (CT) imaging showed that the patient had 1) lobular patchy hyperdense shadows in both lungs, 2) emphysema, 3) cardiomegaly, and 4) aortic sclerosis. A routine blood test revealed the following counts: total white blood cells, 7. 4 × 109/L; neutrophils, 77.2 %; and lymphocytes, 13.4 %. On February 19, 2020, the patient was transferred to the ICU due to deterioration in her condition. After treatment, her condition improved, and she tested negative twice for SARS-CoV-2 on March 8 and 9, 2020. She then continued to be isolated and under observation for an additional 14 days (Fig. 3 ).
Fig. 3.
Patient Details.
4. Results
A total of seven samples were taken, and the positive test rate for SARS-CoV-2 was 14.29 % (1/7). In this study, all samples taken from surface and air environments from the staff PPE dressing room tested negative, but the air sample from the isolation room was intensely positive, as shown in Table 1 .
Table 1.
Samples from the air and surfaces of the ICU.
| Location | Sample collected points | Nucleic acid test results |
Result reporting | |
|---|---|---|---|---|
| The 1st test | The 2nd test | |||
| Isolation room | A: Armrests on the patient’s bed | – | \ | – |
| B: Desk surface of patient’s ward area | – | \ | – | |
| C: Door handles | – | \ | – | |
| D: Desk surface of the nurse's station | – | \ | – | |
| E: Computer keyboard at the nurse's station | – | \ | – | |
| F: Indoor air | + | + | + | |
| Dressing room | G: Indoor air | – | \ | – |
Note: Intensely positive indicated a positive result from both the ORF1ab gene and the N gene of SARS-CoV-2.
5. Discussion
In this study, we found that SARS-CoV-2 particles were present in the air of an isolation room in the ICU. The findings agreed with those reported by other studies that found that SARS-CoV-2 was present in indoor air (Guo et al., 2020; Joshua L. Santarpia, 2020; Liu, 2020; Yuanfang J, 2020). This result is an underlying piece of evidence supporting the hypothesis of airborne transmission of SARS-CoV-2. Moreover, our findings constituted the first piece of environmental evidence that patients who tested negative for SARS-CoV-2 may still be shedding the virus. Since reported median estimates of the half-life of SARS-CoV-2 in aerosols range from approximately 1.1–1.2 hours (95 % confidence intervals of 0.64–2.64) (van Doremalen et al., 2020), our samples were taken 48 h after the patient had tested negative for SARS-CoV-2 and two hours after the last disinfection operation at Jiangjunshan Hospital. It may be inferred that the aerial presence of SARS-CoV-2 in our study was not a result of retention. It is known that recovered patients who are still discharging the virus may have an increased risk of RP. Although the reason for RP remains unclear, potential major factors include virology, immunology, and sampling methodologies. A recent pathological research report found that SARS-CoV-2 could remain in the lung tissue of a ready-for-discharge patient (Yao et al., 2020), and we believe this study also supported the current virologic understanding of RP occurrence among COVID-19 patients, i.e., the false negatives caused by faulty sampling methodologies, viral residues in the patient’s body, intermittent viral release in the patient’s body (Xing Y-H, 2020), and viral distribution (Wölfel R, 2020, Xia, Tong, Liu, Shen, & Guo, 2020). Negative nasopharyngeal swab tests may result in disregarding the above factors. Another study reported that supplementing negative results with an anal swab test at discharge failed to reduce RP occurrence in COVID-19 patients (Liao, An, & Xuejiao, 2020). This study also analysed the differences in anti-SARS-CoV-2 IgG and IgM antibody levels in both RP and non-RP patients at the time of discharge but did not find any significant differences. According to the guidelines for the diagnosis and treatment of pneumonia caused by SARS-CoV-2 (sixth edition) published by the National Health Commission of the People’s Republic of China (China, 2020b), the discharge criteria for recovered patients included a return to normal temperature for more than three days, a significant improvement in respiratory symptoms, a significant absorption of pulmonary lesions on chest CT imaging, and at least two consecutive negative RNA test results conducted at least 24 h apart. As a result, some recovered patients discharged under the current standards are likely to retain SARS-CoV-2 in their lung tissue and may continue shedding it, which may cause new infections after patient discharge and increase the risk of infection transmission in cities. Therefore, our research contributes to the environmental evidence supporting the virologic hypothesis of RP occurrence in COVID-19 patients. We suggest considering the following measures to improve the current discharge standards and disease management of recovered COVID-19 patients. First, stricter protective measures should be taken for the medical staff and close contacts of recovered COVID-19 patients. Second, the clinical and disease management guidelines for discharged COVID-19 patients need to be improved, including extending the detection time prior to discharge. Pulmonary lesions on chest CT imaging, consecutive negative RNA results of nasopharyngeal and anal swab tests, serological testing, clinical features, and natural history of the infection should all be considered before discharging a patient. Continuous air monitoring around recovered COVID-19 patients should be combined with monitoring viral particles in patients' bodies to determine whether complete viral clearance has been achieved. Third, both the sensitivity and specificity of detection kits need to be improved to reduce false negatives.
Unlike other studies, SARS-CoV-2 was not detected on object surfaces in our study (Liu, 2020, Cheng et al., 2020b, Guo et al., 2020; Joshua L. Santarpia, 2020; Ong et al., 2020), which may be due to differences in routine cleaning operations that could lead to different levels of SARS-CoV-2 in the environment; for example, the frequency of disinfection at Jiangjunshan Hospital was higher than that reported in other locations (Guo et al., 2020; Liu, 2020; Ong et al., 2020). Additionally, the number and density of patients in the ICU at Jiangjunshan Hospital were much lower than those at other hospitals, indicating a markedly reduced risk of SARS-CoV-2 contamination in the environment. Moreover, many studies have shown that factors such as temperature and humidity can affect the spread of the virus in enclosed indoor environments (Feng, Bi, Zhang, Cai, & Huang, 2020; Zhang et al., 2019). Some studies reported that the rate in which SARS-CoV-2 spread was accelerated in cold and dry conditions (Casanova, Jeon, Rutal, Weber, & Sobsey, 2010; Chin, Chu, Perera, Hui, & Poon, 2020). Within an infected person, respiratory droplets with high humidity are produced under high humidity conditions by the atomization of human secretions containing the virus as they pass the air passage through out lung during coughing and sneezing. These droplets undergo size reduction due to the drying of water content if the surrounding air humidity and temperature are very low. In contrast, the size of the droplet is not reduced if the surrounding air humidity and temperature are high (Chen, Liu, Lin, & Chen, 2015; Liu, Wei, Li, & Ooi, 2017; Wu, Zhang, & Zhang, 2016). At the same time, the virus could become diluted with the surrounding water content in the air and become less active. Therefore, a humid environment may be beneficial for maintaining droplet size and reducing viral activity and may therefore play a larger role than the temperature of the indoor environment where a SARS-CoV-2-infected patient is located. In our study, the relative humidity in the ICU at Jiangjunshan Hospital was 45 %, which may imply that the droplets shed by the ready-for-discharge patient may undergo size reduction due to the surrounding air conditions being dry. As the expiratory droplet size of the SARS-CoV-2 distribution had a peak size between 0.25 and 1.0 μm (Liu, 2020), viruses with aerodynamic diameters smaller than 0.5 μm can remain suspended in the air instead of quickly settling onto the surfaces of objects, and exhaled droplet nuclei can be transmitted between occupants via the airborne route (Ai, Huang, & Melikov, 2019). Additionally, although our sampling was performed two hours after the last routine cleaning, the frequency of disinfection of object surfaces was higher than that of the air in the ICU at Jiangjunshan Hospital, which may have resulted in the air samples but not the object surfaces testing positive for SARS-CoV-2. To solve the problem of the long-term presence of SARS-CoV-2 viral aerosols in enclosed environments and reduce the risk of SARS-CoV-2 infection, we believe that it is necessary to increase the frequency of indoor air disinfection and to keep the relative humidity of the indoor environment at a high level to maintain droplet size, thereby reducing viral activity.
Our study has several limitations. First, viral cultures were not performed to demonstrate its viability. Second, the sample size was small due to the low incidence of COVID-19 in Guizhou Province. Moreover, due to the lack of consumables (air collection tubes), our research began during the late stage of the epidemic in Guizhou, and we were unable to continue performing air sample tests. The concentration of airborne SARS-CoV-2 was not quantified. The aerodynamic size distribution of SARS-CoV-2 aerosols was not evaluated. Additional studies are needed to confirm our observations.
6. Conclusions
Our findings revealed the presence of SARS-CoV-2 in the indoor air of the ICU and indicate that the virus may be shed via aerosol for days, even after a patient has tested negative. This finding may be one of the reasons for the observation of RP patients. This finding provides valuable empirical information and environmental evidence for the effective management of COVID-19 patients during the convalescent period. We suggest that it is necessary to extend the detection time for COVID-19 patients at the time of discharge and to continually monitor the air surrounding recovered COVID-19 patients for the presence of SARS-CoV-2. Additionally, the frequency of indoor air disinfection needs to be increased, and the indoor relative humidity should be kept at a high level. Our findings can be used to improve both routine cleaning during the outbreak and clinical and disease management guidelines for discharged COVID-19 patients.
Since ICUs are required to maintain negative pressure, close off the isolation ward, and isolate patients in the wards for days at a stretch, it is not possible to use traditional architectural design measures to reduce airborne virus concentrations such as adequate and effective ventilation and ultraviolet germicidal lamps. Additionally, it is difficult to limit the number and density of patients in ICUs and avoid overcrowding during emergency situations like the early stage of the epidemic in Wuhan. Therefore, to enhance the isolation and care facilities for infectious diseases, smart designs for health and quarantine facilities and ICUs are receiving more attention. Attention should be given to the physical elements and environments of buildings that had been designed to reduce the risk of infectious diseases such as Yersinia pestis, tuberculosis, typhoid, polio, and flu during historical epidemics prior to the development of medicines (Megahed & Ghoneim, 2020). In recent years, smarter health and quarantine facilities have been designed. In late 2014, a total of 56 hospitals in the United States of America were designated as specially designed, high-level isolation units (HLIUs) equipped with an advanced infrastructure, advanced laboratory capabilities, and well-trained staff by state governments and federal public health authorities to care for patients with highly hazardous communicable diseases (HHCDs) (Herstein et al., 2018). To improve the ability to prevent, treat, and manage viral respiratory infections and prevent future crises similar to COVID-19, we suggest that the following points be considered when designing smart buildings and hospitals in the future: 1) development of new air disinfection equipment with better disinfection efficiency and observable sustained effects; 2) strengthening of the cooperation and communication between scientists belonging to different fields such as environmental engineering, architecture, clinical medicine, and public health to design smarter and more effective ICUs that conform to health and isolation standards; 3) integration of information communication technology with hospital operations; and 4) implementation of the concept of the Internet of Things within smart hospitals in smart cities (Silva, Khan, & Han, 2018).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We would like to thank Prof. Maosheng Yao from Peiking University and Dingblue Tech, Inc. for their support in providing the sampling devices and technical support in this study.
References
- Ai Z.T., Huang T., Melikov A.K. Airborne transmission of exhaled droplet nuclei between occupants in a room with horizontal air distribution. Building and Environment. 2019;163 doi: 10.1016/j.buildenv.2019.106328. [DOI] [Google Scholar]
- Chen C., Liu W., Lin C.H., Chen Q. Comparing the Markov chain model with the eulerian and lagrangian models for indoor transient particle transport simulations. Aerosol Science and Technology. 2015;49(10):857–871. [Google Scholar]
- Cheng V.C.C., Wong S., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y.…Yuen K. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infection Control and Hospital Epidemiology. 2020;41(5):493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C.C., Wong S., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y.…Yuen K. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infection Control and Hospital Epidemiology. 2020;41(5):493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China T.M.O.H. 2013. The code for indoor environmental pollution control of civil building engineering GB50325-2013. (Reprinted.) [Google Scholar]
- China T.N.H.C. 2003. 2003-04-24). The outbreak of SARS in the global, 2020.http://www.nhc.gov.cn/wjw/zcjd/201304/999eecfa26134b9fbc28b2b648123d12.shtml from. [Google Scholar]
- China T.N.H.C. 2020. 2020-07-19). Reports of COVID-19, 2020.http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml from. [Google Scholar]
- China T.N.H.C. 2020. The guideline of the diagnosis and treatment for novel coronavirus pneumonia (the sixth edition). (Reprinted.) [Google Scholar]
- Crosby A.W. America’s forgotten pandemic, the influenza of 1918. New York New York/cambridge England Cambridge University Press. 1989;12(2) [Google Scholar]
- Department Of Communicable Disease W. 2004. WHO SARS risk assessment and preparedness framework (2020, pp.): WHO. (Reprinted.) [Google Scholar]
- Feng G., Bi Y., Zhang Y., Cai Y., Huang K. Study on the motion law of aerosols produced by human respiration under the action of thermal plume of different intensities. Sustainable Cities and Society. 2020;54 doi: 10.1016/j.scs.2019.101935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z., Wang Z., Zhang S., Li X., Chen W. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerging Infectious Diseases. 2020;26(7) doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He W., Chen C.J., Mullarkey C.E., Hamilton J.R., Wong C.K., Leon P.E.…Hoffman K.W. Alveolar macrophages are critical for broadly-reactive antibody-mediated protection against influenza A virus in mice. Nature Communications. 2017;8(1):846. doi: 10.1038/s41467-017-00928-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herstein J.J., Iwen P.C., Jelden K.C., Biddinger P.D., Gibbs S.G., Le A.B.…Lowe J.J. U.S. High-level isolation unit clinical laboratory capabilities update. Journal of Clinical Microbiology. 2018;56(2) doi: 10.1128/JCM.01608-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshua L. Santarpia D.N.R.V. 2020. Transmission potential of SARS-CoV-2 in viral shedding observed at the university of nebraska medical center: Preprint at medRxiv. (Reprinted) [Google Scholar]
- Lamb R.A. The viruses and their replication. Orthomyxoviridae Fields Virology. 2001;1 [Google Scholar]
- Lan L.X.D.Y. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323(15) doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao X., An J., Xuejiao L. 2020. ). Clinical characteristics of the recovered COVID-19 patients with re-detectable positive RNA test (257): NewsRX LLC. (reprinted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y.Z.N.Y. 2020. Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan Hospitals during COVID-19 outbreak: Preprint at medRxiv. (Reprinted.) [Google Scholar]
- Liu L., Wei J., Li Y., Ooi A. Evaporation and dispersion of respiratory droplets from coughing. Indoor Air. 2017;27(1):179–190. doi: 10.1111/ina.12297. [DOI] [PubMed] [Google Scholar]
- Ludwig M., Enzenhofer E., Schneider S., Rauch M., Bodenteich A., Neumann K.…Mueller C.A. Efficacy of a carrageenan nasal spray in patients with common cold: A randomized controlled trial. Respiratory Research. 2013;14(1):124. doi: 10.1186/1465-9921-14-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megahed N.A., Ghoneim E.M. Antivirus-built environment: Lessons learned from Covid-19 pandemic. Sustainable Cities and Society. 2020;61 doi: 10.1016/j.scs.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y.…Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. Journal of the American Medical Association. 2020;323 doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Province T.H.C.O. 2020. 2020-07-15). Reports of COVID-19 in Guizhou, 2020.http://www.gzhfpc.gov.cn/xwzx_500663/yqtb/ from. [Google Scholar]
- Sande C.J., Njunge J.M., Ngoi J.M., Mutunga M.N., Pollard A.J. Airway response to respiratory syncytial virus has incidental antibacterial effects. Nature Communications. 2019;10(1):1–11. doi: 10.1038/s41467-019-10222-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva B.N., Khan M., Han K. Towards sustainable smart cities: A review of trends, architectures, components, and open challenges in smart cities. Sustainable Cities and Society. 2018;38:697–713. doi: 10.1016/j.scs.2018.01.053. [DOI] [Google Scholar]
- TSOUROS A.D. The WHO Healthy Cities Project: State of the art and future plans. Health Promotion International. 1995;10(2):133–141. doi: 10.1093/heapro/10.2.133. [DOI] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N.…Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. The New England Journal of Medicine. 2020;382(16):1564–1567. doi: 10.1056/nejmc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2019. 2019-12-01). MERS monthly summary, November 2019, July, 2020.https://www.who.int/emergencies/mers-cov/en/ from. [Google Scholar]
- Wölfel R C.V.G.W. 2020. Virological assessment of hospitalized cases of coronavirus disease 2019 (2020, pp.): medRxiv. (Reprinted). [Google Scholar]
- Wu Y., Zhang X., Zhang X. Simplified analysis of heat and mass transfer model in droplet evaporation process. Applied Thermal Engineering. 2016;99:938–943. [Google Scholar]
- Xia J., Tong J., Liu M., Shen Y., Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS‐CoV‐2 infection. Journal of Medical Virology. 2020 doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao X., He Z., Li T., Zhang H., Wang Y., Mou H.…Bian X. Pathological evidence for residual SARS-CoV-2 in pulmonary tissues of a ready-for-discharge patient. Cell Research. 2020;30(6):541–543. doi: 10.1038/s41422-020-0318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu I.T.S., Li Y., Wong T.W., Tam W., Chan A.T., Lee J.H.W.…Ho T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. The New England Journal of Medicine. 2004;350(17):1731–1739. doi: 10.1056/nejmoa032867. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Feng G., Bi Y., Cai Y., Zhang Z.…Cao G. Distribution of droplet aerosols generated by mouth coughing and nose breathing in an air-conditioned room. Sustainable Cities and Society. 2019;51 doi: 10.1016/j.scs.2019.101721. [DOI] [Google Scholar]