Objective
During the coronavirus disease 2019 (COVID-19) pandemic, the entirety of clinical assistance in Italy has been reorganized to minimize the risk of infection. In addition, people have been forbidden to leave their homes except for strictly necessary reasons. These reasons, together with women’s perception of the high risk of COVID-19 in hospitals, led to a substantial drop in the number of patients presenting themselves to emergency department (ED) services. In Italy, emergency services and most healthcare services are free of charge for everyone. Therefore, we decided to evaluate the number of women self-referring to the obstetrics and gynecology (OB-GYN) ED triage and the percentage of admission before and during the COVID-19 pandemic.
Study Design
This was a retrospective study conducted at S.Orsola-Malpighi University Hospital of Bologna (a tertiary center with 2900 deliveries each year) during the following 2 periods: March 1 to 31, 2020, in the middle of the COVID-19 pandemic and after Italian authorities adopted restrictive measures, compared with a control period before the COVID-19 pandemic (March 1–31, 2019) (Figure ). Patients were divided into the following 3 groups: gynecologic patients, pregnant women up to 16 weeks, and pregnant women >16 weeks. The primary outcome was the number of hospitalized patients in the 2 study periods. Secondary outcomes were the reasons for and the proportion admitted of the total number of women seeking ED services. For each category, we identified different possible reasons for admission to OB-GYN ED, as reported in the Table . This was a clinical audit of fully anonymized data, and we judged it to fit the definition of a quality improvement study.1 Differences between 2020 and 2019 were assessed with z-tests. Exact Poisson confidence intervals were estimated by using the upper and lower bounds for Poisson-distributed counts.
Figure.
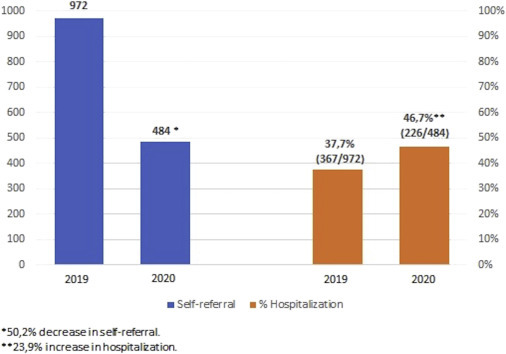
Number of patients admitted to ED and hospitalization rate in the 2 study periods
ED, emergency department.
Salsi. Obstetrics and gynecology emergencies during coronavirus disease 2019 pandemic. AJOG MFM 2020.
Table.
Numbers and details of patients self-referring to OB-GYN ED during March 2019 and March 2020, with hospitalization rates. After reporting the total number of self-referrals, further analysis were made dividing patients in three categories: gynecological patients, obstetrical patients <16 weeks and obstetrical patients >16 weeks
| Self-referral |
Hospitalization |
||||||
|---|---|---|---|---|---|---|---|
| March 2019 (N=972) | March 2020 (N=484) | Reduction (%) | P value | March 2019 hospitalization (%) | March 2020 hospitalization (%) | P value | |
| Total number of patients referring to OB-GYN ED | |||||||
| Gynecologic | 330 | 112 | 66.1 | <.001 | 88 (26.7) | 38 (33.9) | .141 |
| Obstetrical <16 wk | 242 | 118 | 51.2 | <.001 | 56 (23.1) | 24 (20.3) | .548 |
| Obstetrical ≥16 wk | 400 | 254 | 36.5 | <.001 | 223 (55.8) | 164 (64.6) | .025 |
| Total | 972 | 484 | 50.2 | <.001 | 367/972 (37.7) | 226/484 (46.7) | .001 |
| March 2019 N=330 (%) |
March 2020 N=112 (%)a |
Reduction (%)b | P value | March 2019 hospitalization N=88 (%) | March 2020 hospitalization N=38 (%)c | P value | |
|---|---|---|---|---|---|---|---|
| Gynecologic patients | |||||||
| Vaginal bleeding | 85 (25.8) | 26 (23.2) | 69.4 | <.001 | 17 (20) | 12 (46.2) | .008 |
| Lower abdominal pain | 70 (21.2) | 26 (23.2) | 62.9 | <.001 | 23 (32.9) | 7 (26.9) | .577 |
| Vulvar conditions | 41 (12.4) | 17 (15.2) | 58.5 | .004 | 5 (12.2) | 5 (29.4) | .114 |
| Postpartum complications | 33 (10) | 15 (13.4) | 54.5 | .013 | 10 (30.3) | 4 (26.7) | .797 |
| Vaginal bleeding and lower abdominal pain | 20 (6.1) | 14 (12.5) | 30 | .311 | 5 (25) | 4 (28.6) | .816 |
| Vaginal discharge | 27 (8.2) | 6 (5.4) | 77.8 | .001 | 0 | 0 | — |
| Other | 54 (16.4) | 8 (7.1) | 85.2 | <.001 | 28 (51.9) | 6 (75) | .220 |
| March 2019 N=242 (%) |
March 2020 N=118 (%)a |
Reduction (%)b | P value | March 2019 hospitalization N=56 (%) | March 2020 hospitalization N=24 (%)c | P value | |
|---|---|---|---|---|---|---|---|
| Obstetrical patients <16 wk | |||||||
| Vaginal bleeding | 108 (44.6) | 56 (47.5) | 48.1 | <.001 | 14 (13) | 7 (12.5) | .933 |
| Vaginal bleeding and lower abdominal pain | 45 (18.6) | 32 (27.1) | 28.9 | .140 | 17 (37.8) | 9 (28.1) | .377 |
| Lower abdominal pain | 39 (16.1) | 17 (14.4) | 56.4 | .017 | 6 (15.4) | 3 (17.6) | .832 |
| Hyperemesis | 13 (5.4) | 2 (1.7) | 84.6 | .014 | 7 (53.8) | 0 | .155 |
| Other | 37 (15.3) | 11 (9.3) | 70.3 | <.001 | 12 (32.4) | 5 (45.5) | .428 |
| March 2019 N=400 (%) |
March 2020 N=254 (%)a |
Reduction (%)b | P value | March 2019 hospitalization N=223 (%) | March 2020 hospitalization N=164 (%)c | P value | |
|---|---|---|---|---|---|---|---|
| Obstetrical patients >16 wk | |||||||
| Painful uterine contraction or labor | 118 (29.5) | 79 (31.1) | 33 | .010 | 96 (81.4) | 56 (70.9) | .086 |
| Leaking amniotic fluid (PROM or suspected PROM) | 77 (19.3) | 53 (20.9) | 31.2 | .050 | 57 (74) | 49 (92.5) | .008 |
| Lower abdominal pain (not classified as labor) (<36 wk) | 50 (12.5) | 31 (12.2) | 38 | .037 | 9 (18) | 6 (19.4) | .879 |
| High blood pressure | 15 (3.8) | 22 (8.7) | 46.6 | .275 | 12 (80) | 20 (90.9) | .341 |
| Vaginal bleeding | 24 (6) | 18 (7.1) | 25 | .361 | 8 (33.3) | 1 (5.6) | .030 |
| Reduced fetal movements | 18 (4.5) | 10 (3.9) | 44.4 | .153 | 5 (27.8) | 6 (60) | .094 |
| Other | 98 (24.5) | 41 (16.1) | 58.2 | <.001 | 62 (63.4) | 15 (36.6) | .004 |
ED, emergency department; OB-GYN, obstetrics and gynecology; PROM, premature rupture of membranes.
Salsi. Obstetrics and gynecology emergencies during coronavirus disease 2019 pandemic. AJOG MFM 2020.
Total number of patients for each category in 2020 with percentage calculated over the total number of gynecologic patients for that month
reduction in percentage when compared with those in the same period in 2019
percentage of patients in this category admitted to hospital over the number of access for that reason during March 2020.
Results
A total of 972 women self-referred to our OB-GYN ED during March 2019. During March 2020, the total number of OB-GYN self-referrals was 484, indicating a 50.2% reduction (P<.001), likely because of the COVID-19 pandemic. Overall, the number of patients admitted to the hospital was lower in 2020, but analyzing the proportion of women being hospitalized over the number of accesses, the hospitalization rate was significantly higher during the COVID-19 pandemic (226/484, 46.7% vs 367/972, 37.7% in 2019; P<.001), suggesting that during the COVID-19 pandemic, women are going to hospital for more serious problems than in previous years.
When the 3 groups were compared separately, the proportion of inpatient admissions was significantly lower in 2019 than in 2020 only in the category of pregnant women >16 weeks (64.6% vs 55.8% in 2019; P=.025). Conversely, no significant difference was observed in the other 2 groups. Results are reported in the Table.
Conclusion
The significant reduction in OB-GYN ED accesses observed during the COVID-19 pandemic represents the indirect evidence of the probably inappropriate use of emergency services under normal circumstances by women, going to ED just to obtain a clinical evaluation or an ultrasound quickly, with consequent higher healthcare costs. However, we want to stress the possibility that people’s fear of COVID-19 might lead to critical situations owing to important delays in seeking medical care, even if apparently this was not the case in our population. The main strength of this study is that this is the only type of ED in which it is possible to conduct this kind of analysis, because it is not affected by the higher number of patients with COVID-19 infection seeking emergency services. We noted that the only cause of OB-GYN ED referral that increased in March 2020 compared with 2019 is high blood pressure in pregnancy; this might be an indirect sign of higher stress rates among pregnant women.
Footnotes
This paper is part of a supplement that represents a collection of COVID-related articles selected for publication by the editors of AJOG MFM without additional financial support.
The authors report no conflict of interest.
Reference
- 1.Casarett D., Karlawish J.H., Sugarman J. Determining when quality improvement initiatives should be considered research: proposed criteria and potential implications. JAMA. 2000;283:2275–2280. doi: 10.1001/jama.283.17.2275. [DOI] [PubMed] [Google Scholar]


