Abstract
Background
In late 2019, the world saw a viral outbreak of unprecedented scale that sent a significant fraction of humankind into either quarantine or lockdown. Coronavirus disease 2019 (COVID-19) is a respiratory tract infection caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which was first recognized in Wuhan, China, in December 2019.
Methods
We created and administered a 17-item questionnaire for health care professionals (HCPs) to assess their level of knowledge towards this ongoing and evolving pandemic. It was disseminated through Web- and mobile-based social networks. The questions were sourced and created from various standard national and international guidelines available at the time of writing.
Results
A total of 827 medical personnel participated in the study. Among them, 65.5% scored between 60% and 79%, indicating a moderate level of knowledge. There was no statistically significant difference in the scores of doctors, nursing officers and dental surgeons (p = 0.200). Participants had good knowledge regarding clinical symptoms, mode of transmission and preventive measures. But the study identified some gaps in knowledge in the implementation of management protocols, handling of dead bodies and biomedical waste management of COVID-19 cases.
Conclusion
With this understanding, regular training, drills and knowledge dissemination along with skill development through learning correct practices focusing on HCP at all levels are the current needs.
Keywords: Coronavirus, COVID-19, Adult respiratory distress syndrome, Health care professionals
Introduction
Coronavirus has become a major pathogen causing an outbreak affecting humankind. The last two decades have seen several such epidemics and pandemics of international concern. In 2002–03, the world saw the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV), followed by the H1N1 influenza in 2009 and the Middle East respiratory syndrome–coronavirus (MERS-CoV) that was first identified in Saudi Arabia in 2012. In 2019, a similar disease was identified from the Wuhan province, in China; the genetic sequence revealed that it was a beta-coronavirus closely linked to the SARS virus.1
The respiratory disease caused by the novel coronavirus, designated COVID-19 (an acronym for Coronavirus disease 2019), was declared as a Public Health Emergency of International Concern on 30 January 2020.1 As on date, that is, 3 July 2020, the total number of cases worldwide stands at 10,533,779 cases with more than 5,12,842 deaths,2 and India has 2,27,439 cases with 18,213 deaths.3 Most people (about 80%) have recovered from the disease without the need for any special treatment. Around 1 of every 6 individual affected by COVID-19 becomes seriously ill.1
The steps to mitigate the pandemic encompasses measures starting at a global level, zooming all the way on to the patient level. Health care workers are required to function at various echelons from screening, triage, contact tracing and treating COVID-19 patients. The scientific knowledge with respect to SARS-CoV-2 and COVID-19 is evolving each day. Health care professionals (HCPs) have to remain constantly updated of changing testing and treatment modalities and guidelines. Studies have found that there is a high prevalence of misinformation among HCPs in the context of COVID-19, especially from social media.4,5 To facilitate the outbreak management of COVID-19 in India, there is an urgent need to understand the awareness of COVID-19 at this critical juncture. To do this, it was thought prudent to assess the level of existing knowledge of HCPs, hence this study was undertaken.
Materials and methods
A cross-sectional survey was conducted from 6th April to 8th April 2020, the second week after the nationwide lockdown. As it was not feasible to do a community-based national sampling survey during this special period, we collected the data online, thereby keeping in line with the social distancing and lockdown protocols. A self-administered questionnaire of 17 items was developed and duly validated. The questions were sourced and derived from various standard National and International guidelines existing at the time of the study, for example, World Health Organization (WHO), Centers for Disease Control and Prevention and Indian Council of Medical research, and so on. The questionnaire was first pilot tested in 30 respondents, their responses were analyzed, and changes were made based on the feedback received from the participants.
The data were collected through Google Forms by sharing the link, electronically. 12 questions were multiple-choice type and 5 questions were in yes/no format. Doctors, dental surgeons and nurses working in various tertiary care and secondary care hospitals in which care to suspected/confirmed COVID-19 patients was being provided across India were included in the study.
Informed consent was taken from the participants while taking on the online questionnaire. Participants had to answer a yes–no question to confirm their willingness to participate voluntarily.
Statistical analysis
The data were analyzed using SPSS version 26.0. Each correct answer on the questionnaire was given one point. The total score varied between 0 (with no correct answer) and 17 (for all correct answers). Quantitative data were expressed as mean and standard deviation. Qualitative data variables were expressed using frequency and percentage. One-way analysis of variance test was used to compare the mean scores of participants, and post-hoc Tukey's test was used for pairwise comparison of scores. A P value <0.05 is considered to be statistically significant.
To classify the knowledge levels, the original Bloom's cut-off points, 80.0%–100.0%, 60.0%–79.0% and ≤59.0%, were adapted to categorize into high, moderate and low-level of knowledge, respectively.6,7
Results
A total of 827 HCPs responded to the questionnaire that consisted a mix of 529 doctors, 269 nurses and 29 dental surgeons. Of 529 doctors, 201 were medical officers, 217 were specialists and 111 were subspecialists.
The overall mean score was 9.30 ± 1.82 (54.70%). Among 827 HCPs, 65.5% (n = 542) scored between 60% and 79%, indicating a moderate level of knowledge, as per Bloom's cut-off point; 33.7% (n = 279) had a low level of knowledge, scoring less than 60%; and only 0.73% (n = 6) scored ≥80%.
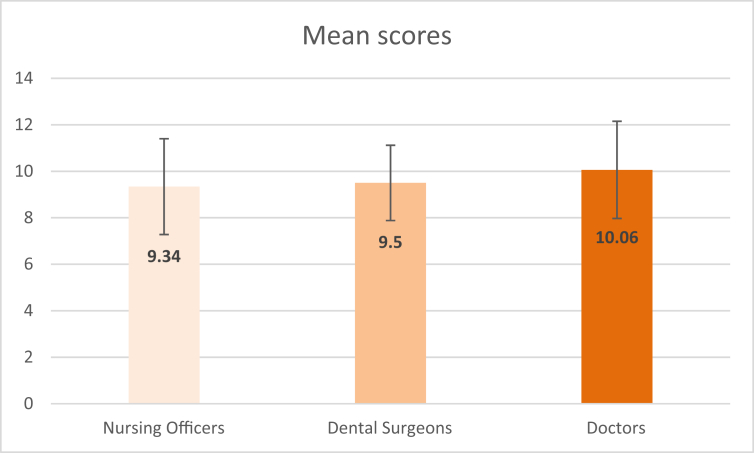
The mean scores of the participants as per their qualifications are shown in Fig. 1. Doctors showed higher mean scores (10.06 ± 2.09) when compared to nursing officers (9.34 ± 2.06) and dental surgeons (9.50 ± 1.62). However, there was no statistically significant difference in the mean scores of doctors, nursing officers and dental surgeons (p = 0.200).
Fig. 1.
Mean scores of HCPs as per qualification (columns indicate the mean scores; error bars indicate standard deviation).
The study showed that 89% participants (n = 736) responded correctly about the duration of quarantine for COVID-19, which as per the WHO and national guidelines should be 14 days.1 Also, 95% (n = 786) were aware that a confirmed case of COVID-19 is a person with a positive laboratory test result irrespective of signs and symptoms, reflecting the knowledge on the confirmed case was high.8
On the question of ascertaining the understanding of the definition of a contact case, which as per the WHO is the person who provided direct care to a COVID-19 patient without personal protective equipment (PPE) or who had face-to-face contact within 1 m and for more than 15 min, with a probable or confirmed case 2 days before and 14 days after symptom onset,8 28.9% participants (n = 239) attempted the question correctly, reflecting that the understanding of defining a contact case needs to be developed further.
Bleaching powder preparation as a disinfectant was correctly answered by 78.7% (n = 651). This is an important area of awareness as the COVID wards need to be disinfected by a team of HCPs, hence lack of knowledge of effective preparation will result in the increasing spread of the virus as COVID-19 can survive on the surface for hours to days.9
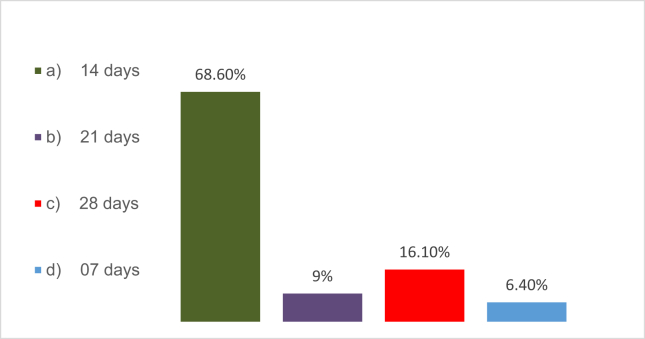
There was a substantial variation in the understanding of the duration of follow-up of contact from the time of last contact with the confirmed case as shown in Fig. 2. 16.1% (n = 133) answered it correctly as 28 days, indicating the insufficiency of knowledge on this concept.
Fig. 2.
Responses to question on the duration of follow-up of a contact from the time of last contact with COVID-19. Correct answers are marked in red in the figure.
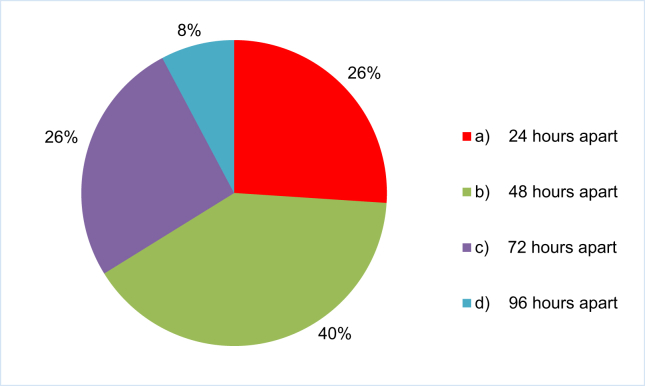
Only 26% (n = 215) were aware that two laboratory tests should be negative in a clinically recovered COVID-19 patient collected 24 h apart for discharging the patient.10 As depicted in Fig. 3, there appears to be a wide variation in the knowledge and understanding of the discharge protocol based on reverse transcriptase polymerase chain reaction (RT-PCR) results.
Fig. 3.
Responses to question on the discharge protocol for two laboratory tests to be negative in the recovered patient. Correct answers are marked in red in the figure.
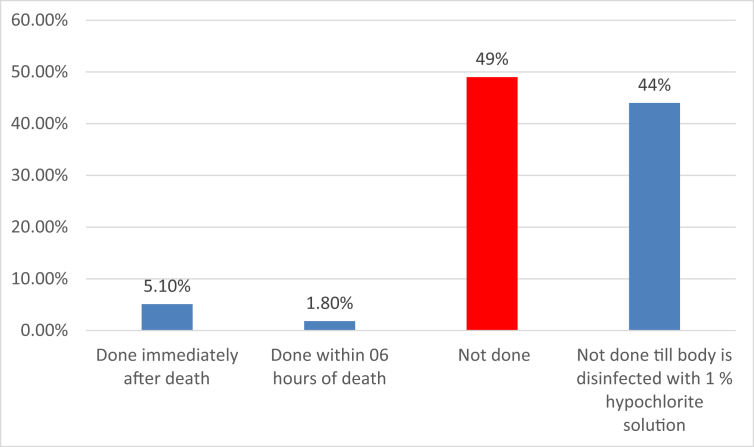
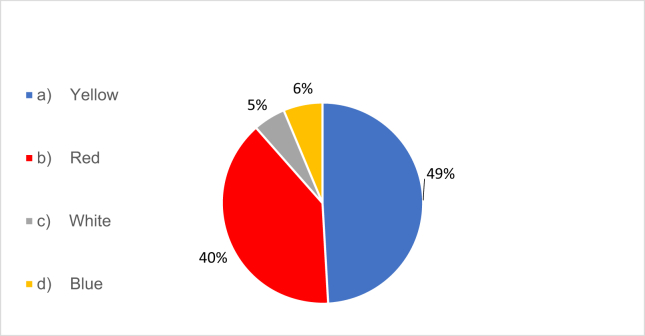
Handling of the dead is an important area of concern, and embalming is not performed for COVID-19 deaths.11 Only 49% (n = 405) had a clear understanding of this concept. The responses are depicted in Fig. 4.
Fig. 4.
Responses to question on the embalming of COVID-19 patients. Correct answers are marked in red in the figure.
40% participants (n = 330) responded correctly that eye goggles in doffed off PPE while treating COVID-19 patients should be in the red category of waste disposal (Fig. 5). The point to be understood is that all doffed off PPEs will be disposed in the yellow category except eye goggles, which will be in the red category.12
Fig. 5.
Responses to question on the disposal of eye goggles after doffing. Correct answers are marked in red in the figure.
As an HCP, while managing a COVID-19 case, 89.5% (n = 740) were aware that the N95 mask to be used and not a surgical mask.
35.3% participants (n = 292) were aware that when an asymptomatic HCP has treated COVID-19–positive case without PPE, he/she should be given chemoprophylaxis and to be placed in a quarantine centre. An HCP will be placed in isolation only when he becomes symptomatic. The Indian Council of Medical Research recommends hydroxychloroquine prophylaxis to all asymptomatic health care workers involved in COVID-related activities.12
49.7% participants (n = 411) were aware that testing between 5th and 14th day for an asymptomatic contact of a confirmed case is to be performed.13
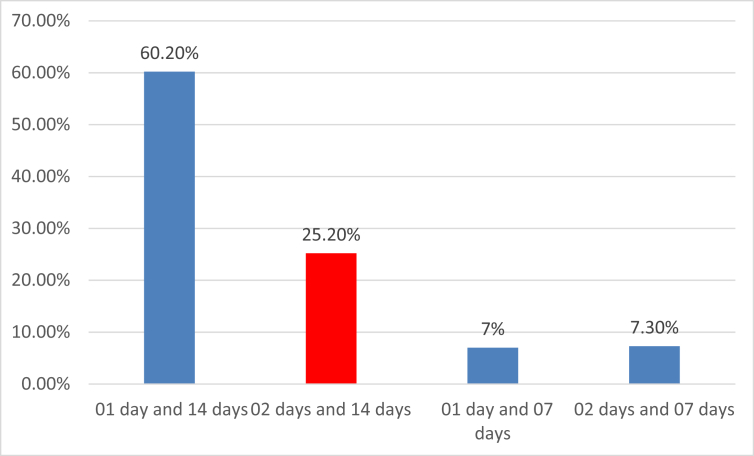
For quarantine, a ‘contact’ is a person involved from 2 days before and up to 14 days after the contact with the COVID-19–positive patient.8 25.2% participants (n = 209) answered this question correctly, as shown in Fig. 6.
Fig. 6.
Responses to question on the criteria of contact for the purpose of quarantine—a ‘contact’ is a person involved _ days before and _ days after the contact with the COVID-19–positive patient. Correct answers are marked in red in the figure.
87.9% participants (n = 727) knew that older people and those with underlying comorbidities are more likely to develop serious illness.1
17.7% participants (n = 146) felt that eating or contact with wild animals would result in COVID-19 infection. As of now, there is no evidence that companion animals, including pets, can spread or be the source of COVID-19 infection.9
96.8% participants (n = 800) knew that patients with COVID-19 may be asymptomatic throughout or while in the incubation period, but still are infective to others.1 95.9% participants (n = 793) were aware that it is equally important to take measures to prevent children and young adults from getting infected.9
The global containment strategy includes the rapid identification of confirmed cases with isolation and early management. 97.5% participants (n = 806) answered correctly that isolation and effective treatment of people who are infected with the COVID-19 virus are ways to reduce the spread of the virus.1
Discussion
This study showed that 65.5% had a moderate and another 33.7% had a low level of knowledge. The overall score was 54.7%. This contrasts with similar studies performed in China. Maheshwari et al.14 and Giao et al.15 showed that 86.7% and 81.4% of HCPs had sufficient knowledge about COVID-19 in their respective studies. The difference can be possible because, in those studies, the questions were in yes/no format as compared to multiple-choice type in this study. Health care workers are not only at the forefront of the ongoing battle against COVID-19, but also at higher risk of acquiring the disease than the general population.16 It is therefore of paramount importance that HCPs have adequate knowledge about all aspects of the disease ranging from symptomatology and diagnosis to treatment and prevention strategies. These results highlight the need for greater efforts to raise general awareness among HCPs about COVID-19.
The difference in mean scores in various subgroups of HCPs based on their qualification was not statistically significant. These results are comparable to previous studies.7,17 These findings suggest that the training modules should focus equally on all HCPs, as this is a novel disease and knowledge on the subject is continuously evolving.
The participants showed a high level of knowledge regarding the duration of quarantine and definition of the confirmed case. These results are comparable to previous studies.7,14
The study showed that the participants had good knowledge regarding clinical symptoms, mode of transmission and preventive measures. These results are comparable to the study by Giao et al.15 and to another study published by Asaad et al.,17 which assessed awareness towards MERS-CoV among HCPs in south-western Saudi Arabia.
Less than one-third participants were aware of the definition of close contact in this study. Modi et al.18 also showed that the participants had poor knowledge about understanding of close contact in their study.
However, we found some knowledge gaps with regard to the management of these cases. The protocols of chemoprophylaxis, laboratory investigations, discharge, handling of dead bodies of COVID-19–positive patients and disposal of PPE are poorly understood. These results are somewhat similar to the studies published by Khan et al.19 and Bener et al.,20 which also showed that the HCPs had insufficient knowledge about the management aspects of MERS and SARS patients, respectively. Tice et al.21 also showed that less than one-third respondents were aware of the management protocol for SARS in their workplace.
Strength of study
The strength of the study is in a large sample size of HCPs collected in a short duration of 72 h, wherein 827 doctors and nurses responded despite being in a state of the COVID-19 outbreak.
Limitations of study
As this is a questionnaire-based online survey with voluntary participation and those who did not participate may be systematically different from those who participated, and thus the possibility of respondent bias cannot be ruled out. Secondly, amongst the HCPs to whom the questionnaire was made available online, the maximum respondents were doctors. This may have contributed to participant bias, thus limiting generalizability to all HCPs. Despite these limitations, the study provides valuable information about the knowledge of HCPs during a critical period of the pandemic.
Recommendations
The need of the hour is to bridge the awareness gap by enhancing the knowledge and practices with special emphasis on screening and contact tracing, skill development for procedures like donning and doffing of PPE, treatment protocols, focused group training on clinical and administrative procedures, standardization of operating protocols and consolidated training in areas like biomedical waste management. Prospective studies on this subject assessing the change in the level of knowledge amongst HCPs with progression of the pandemic can be conducted in the future. The knowledge before and after training modules. These measures will enhance the knowledge, attitude and practices among HCPs towards this rapidly emerging life challenging global pandemic with a high case fatality rate.
Conclusion
The HCPs had a moderate level of knowledge about COVID-19. The qualification and work experience did not significantly affect the knowledge levels. The main knowledge gaps were in understanding of the definition of close contact and practical aspects of handling cases like laboratory investigations, treatment and discharge protocols, biomedical waste management and handling of dead bodies. As the disease is progressing at a fast pace, the HCPs should be aware of all the nuances of the disease to combat the pandemic effectively.
Disclosure of competing interest
The authors have none to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mjafi.2020.07.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.WHO EMRO . 2020. Questions and Answers | COVID-19 | Health Topics.http://www.emro.who.int/health-topics/corona-virus/questions-and-answers.html [Internet]. Emro.who.int. [cited 15 April 2020]. Available from: [Google Scholar]
- 2.COVID-19 Situation Reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ [Internet]. Who.int. [cited 03 July 2020]. Available from: [Google Scholar]
- 3.MoHFW . 2020. Home.https://www.mohfw.gov.in/ [Internet]. Mohfw.gov.in. [cited 03 July 2020]. Available from: [Google Scholar]
- 4.Datta R., Yadav A.K., Singh A., Datta K., Bansal A. The infodemics of COVID-19 amongst healthcare professionals in India. Med J Armed Forces India. 2020 May 29 doi: 10.1016/j.mjafi.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kouzy R., Abi Jaoude J., Kraitem A. Coronavirus goes viral: quantifying the COVID-19 misinformation epidemic on Twitter. Cureus. 2020 Mar;12(3) doi: 10.7759/cureus.7255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed N., Taneepanichskul S. Knowledge, attitude and practice of dengue fever prevention among the people in male, Maldives. J Health Res. 2008;22(suppl l):33–37. [Google Scholar]
- 7.Olum R., Chekwech G., Wekha G., Nassozi D.R., Bongomin F. Coronavirus disease-2019: knowledge, attitude, and practices of health care workers at makerere university teaching Hospitals, Uganda. Front Publ Health. 2020 Apr 30;8:181. doi: 10.3389/fpubh.2020.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . World Health Organization; Geneva: 2020. Global Surveillance for COVID-19 Caused by Human Infection with COVID-19 Virus: Interim Guidance, 20 March 2020. [Google Scholar]
- 9.Coronavirus Disease 2019 (COVID-19) Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/faq.html [Internet] [cited 15 April 2020]. Available from: [Google Scholar]
- 10.COVID-19 Situation Reports. 2020. [Internet]. Who.int. cited 15 April 2020]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation reports/ [Google Scholar]
- 11.World Health Organization . World Health Organization; Geneva: 2020. Infection Prevention and Control for the Safe Management of a Dead Body in the Context of COVID-19: Interim Guidance, 24 March 2020. [Google Scholar]
- 12.Indian Council of Medical Research . 2020. Revised Advisory on the Use of Hydroxychloroquine (HCQ) as Prophylaxis for SARS-CoV-2 Infection (In Supersession of Previous Advisory Dated 23rd March, 2020) pp. 1–4. [Google Scholar]
- 13.Revised Strategy of COVID19 Testing in India (Version 3, Dated 20/03/2020) Indian Council of Medical Research; 2020. [Google Scholar]
- 14.Maheshwari S., Gupta P.K., Sinha R., Rawat P. Knowledge, attitude, and practice towards coronavirus disease 2019 (COVID-19) among medical students: a cross-sectional study. J Acute Dis. 2020 May 1;9(3):100. [Google Scholar]
- 15.Giao H., Han N.T., Van Khanh T., Ngan V.K., Van Tam V., Le An P. Knowledge and attitude toward COVID-19 among healthcare workers at district 2 Hospital, Ho Chi Minh city. Asian Pac J Trop Med. 2020;13 [Google Scholar]
- 16.Nguyen L.H., Drew D.A., Joshi A.D. Risk of COVID-19 among frontline healthcare workers. medRxiv. 2020 Jan 1 [Google Scholar]
- 17.Asaad A.M., El-Sokkary R.H., Alzamanan M.A., El-Shafei M. Knowledge and attitudes towards Middle East respiratory syndrome-coronavirus (MERS-CoV) among health care workers in south-western Saudi Arabia. East Mediterr Health J. 2019;25 doi: 10.26719/emhj.19.079. [DOI] [PubMed] [Google Scholar]
- 18.Modi P.D., Nair G., Uppe A. COVID-19 awareness among healthcare students and professionals in Mumbai metropolitan region: a questionnaire-based survey. Cureus. 2020 Apr;12(4) doi: 10.7759/cureus.7514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan M.U., Shah S., Ahmad A., Fatokun O. Knowledge and attitude of healthcare workers about middle east respiratory syndrome in multispecialty hospitals of Qassim, Saudi Arabia. BMC Publ Health. 2014 Dec;14(1):1281. doi: 10.1186/1471-2458-14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bener A., Al-Khal A. Knowledge, attitude and practice towards SARS. J Roy Soc Promot Health. 2004 Jul;124(4):167–170. doi: 10.1177/146642400412400408. [DOI] [PubMed] [Google Scholar]
- 21.Tice A.D., Kishimoto M., Dinh C.H., Lam G.T., Marineau M. Knowledge of severe acute respiratory syndrome among community physicians, nurses, and emergency medical responders. Prehospital Disaster Med. 2006 Jun;21(3):183–189. doi: 10.1017/s1049023x00003654. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.