Abstract
This study investigates the possible association between social media usage and the mental health toll from the coronavirus at the peak of Wuhan's COVID-19 outbreak. Informed by the Crisis and Emergency Risk Communication Model and Health Belief Model, it proposes a conceptual model to study how people in Wuhan – the first epicenter of the global COVID-19 pandemic – used social media and its effects on users' mental health conditions and health behavior change. The results show that social media usage was related to both depression and secondary trauma, which also predicted health behavior change. But no relation was detected between health behavior change and mental health conditions. As the virus struck, social media usage was rewarding to Wuhan people who gained informational, emotional, and peer support from the health information shared on social media. An excessive use of social media, however, led to mental health issues. The results imply that taking a social media break may promote well-being during the pandemic, which is crucial to mitigating mental health harm inflicted by the pandemic.
Keywords: COVID-19, Wuhan, Social media, Mental health, Health behavior change, Coronavirus
Highlights
-
•
This study reveals mental health toll at the peak of Wuhan's COVID-19 outbreak.
-
•
Social media usage predicted both depression and secondary trauma in Wuhan residents.
-
•
Social media usage predicted health behavior change during the public health crisis.
-
•
Social media usage offered users vital informational, emotional, and peer support.
-
•
Social media are not the culprit for mental health issues detected in the pandemic.
1. Introduction
On December 31, 2019, Chinese health officials first reported to the Beijing office of the World Health Organization (WHO) that a cluster of pneumonia cases with unknown etiology emerged in Wuhan, the capital of Central China's Hubei Province (WHO, 2020). Those unusual pneumonia cases at Wuhan hospitals' intensive care units were soon diagnosed as being caused by a novel coronavirus. WHO formally named the virus as COVID-19, short for “coronavirus disease 2019,” on February 11, 2020 (Lin et al., 2020; Patel & Jernigan, 2020). Few expected the previously unknown virus could trigger a large-scale outbreak of novel pneumonia that put Wuhan on lockdown for 76 days. Even fewer anticipated that COVID-19 would spiral into a global health crisis, killing hundreds and thousands of people and infecting millions more around the world. The spread of the coronavirus was creating a new age of anxiety around the globe, in which the Wuhan people were the first suffering from the traumatic pandemic.
The scale of this pandemic was unprecedented in the history of public health crises, whose detrimental effects include inflicting long-lasting emotional trauma on people. A timely research is imperative for a better understanding of the evolving COVID-19 effects, especially the toll on mental health. This study analyzed how Wuhan residents (N = 320) processed health information on social media and investigated how their social media usage might reveal a toll on mental health at the peak of Wuhan's COVID-19 outbreak. The findings should contribute to understanding the possible links between social media usage and emotional trauma people underwent in a public health crisis. Hence, this study should generate insights for a better understanding of health information processing and the public response to pandemics.
2. Literature review
People in a public health crisis have difficulty to make life function like before as the stresses and uncertainty induced by health risks were sometimes too much to handle. To Wuhan residents, the initial signs of coronavirus-related stress became palpable after China's central government imposed a lockdown in the city on January 23, 2020. In February 2020, China used wartime control measures to put more cities on lockdown, affecting an estimated 760 million people (The Lancet, 2020). These militarized approaches confirmed uncertainty and increased stress and anxiety surrounding the deadly infectious disease among Wuhan residents, who experienced the first waves of emotional trauma during the global health crisis. Uncertainty in a health crisis is associated with fear due to heightened sense of threat (Avery, 2017). An elevated fear in a crisis for an extended period could take a toll on mental health. Hence, it is important to investigate how Wuhan residents coped with the possible mental health toll, if any, when they were thrown into disarray by the COVID-19 outbreak.
2.1. Social media use in health crises
As more people rely on social media to seek and share health information (de Calheiros Velozo & Stauder, 2018; Li et al., 2018), social media usage becomes a welcome relief from a health disaster like the COVID-19 pandemic. This study holds that analyzing social media usage in a pandemic context should help disclose mental health toll. Indeed, the easy access to health information on social media has empowered the public to be more active in evaluating health risks and managing health concerns (Roundtree, 2016; Tonsaker et al., 2014). Social media users produce and share timely and locally situated health information in response to public health crises. Meanwhile, governments and health officials have been actively adopting social media to contain harm caused by health crises, for instance, the 2001 anthrax attack in multiple U.S. cities (Reynolds & Seeger, 2005), the 2009 H1N1 flu crisis in Beijing (Hu & Zhang, 2014), and the 2015 measles outbreak in California (Meadows et al., 2019).
A great deal of work has been devoted to studying how people seek and share online health information in crisis situations (Avery, 2010, 2017; Hu & Zhang, 2014; Meadows et al., 2019; Park et al., 2019). Early studies in this stream had largely centered on audience channel selection and found that people were more likely to rely on traditional media for accessing health information in both crisis and routine contexts, who preferred newspapers or magazines over radio and television (Avery, 2010). Later, the public turned to use social media and mobile phones more than traditional media for accessing health information (Hu & Zhang, 2014). One of the great scientific challenges in analyzing the mental health toll caused by COVID-19 lies in making invisible emotional trauma visible, deciphering the key macroscale sociotechnical factors involved. The Crisis and Emergency Risk Communication (CERC) model (Jones et al., 2015) and Health Belief Model (HBM) (Rosenstock, 1974) have informed this study as appropriate theoretical frameworks in investigating Wuhan residents’ mental health conditions such as depression and secondary trauma.
2.2. The CERC model
The CERC model assumes that public crises, such as infectious disease outbreaks, natural disasters, or bioterrorism attacks, normally develop in five stages from 1) pre-crisis; 2) initial event; 3) maintenance; 4) resolution; to 5) evaluation (Reynolds & Seeger, 2005). The CERC model was originally proposed as an integrated framework for public health professionals to communicate with the public in a crisis situation (Meadows et al., 2019). This model can be applied to analyzing how Wuhan residents accessed and shared health information on social media in the COVID-19 outbreak as they experienced predictable patterns specified in the five-stage CERC model. Conceptualizing the public response to a health crisis in stages helps analyze their strategies in mitigating stress and threat of health risks.
In those initial weeks of the COVID-19 outbreak, Wuhan residents desperately sought information about the virus and its risks to themselves, family members, neighbors, and colleagues. When uncertainty in a crisis represents potential danger and harm, most people would actively engage in information seeking, trying to confirming or disconfirming the information they received (Brashers et al., 2000). Information seeking thus helps “reduce uncertainty by allowing for better discrimination between or among alternatives” (p. 63). The health information on social media played a crucial role for Wuhan residents to understand the crisis and mitigate risks. To them, the health information on WeChat, China's most popular social media mobile app, became a lifeline of information as local or national newspapers and television stations reported little about the epidemic due to censorship. Health crises tend to interrupt people's routine lives and cause confusion in them (Lachlan et al., 2016). Such crisis outcomes turned worse when COVID-19 hit a country with a tightly controlled media system. Meanwhile, information processing can be a double-edged sword in a public health crisis. While more health information helps relieve stress, information seeking itself could amplify uncertainty by increasing the number of alternatives, or by blurring the distinction between or among alternatives (Brashers et al., 2000). Information avoidance, as a passive type of information processing, can maintain uncertainty.
According to the CERC model, Wuhan residents might have to rely on social media to obtain information that is critical for them to make decisions in response to a series of tough questions, including, “Should I seek medical treatment?” “Do I need to wash my hands more often?” “Should I wear face masks?” (see CDC, 2018). Another factor that contributes to social media usage in Wuhan residents was that the news content was constantly censored by the government. In the first month of Wuhan's COVID-19 outbreak, the press, both local or national, rarely reported so-called “negative” news about the virus. The social media content was also censored, but it was not as easily or timely censored as the information in state-controlled media outlets (King et al., 2013). This study examines the possible association between social media use and mental health toll during Wuhan's COVID-19 outbreak regarding the first two stages of the CERC model.
2.3. Health information support
One of the major benefits people use social media for accessing health information is that the content provides social support to them, especially those with health concerns or medical conditions (Ouyang et al., 2016). Social support is defined as “the individual feeling valued and cared for by their social network as well as how well the person is embedded into a network of communication and social obligation” (Stephens & Petrie, 2015, p. 735). Social support involves as an exchange of resources among individuals who perceive it as intended to enhance the recipient's well-being (Tengku Mohd et al., 2019). The importance of social support-related factors on health has attracted scholarship from a broader array of scientists, researchers, and clinicians (Antonucci, 2001). Following previous research (Yang et al., 2018), this study examines the social support as a multidimensional concept in the forms of informational, emotional, and peer support Wuhan residents received when accessing health information related to COVID-19 on WeChat.
2.3.1. Informational support
People are motivated to seek health information on social media due to the benefits of social support that comes in the form of information to aid in health decision-making (Uchino et al., 2018). Informational support people obtain in using social media offer them higher self-esteem and increased perception of social capital (Selkie et al., 2020), including positive mental health outcomes (McConnell et al., 2015). Meanwhile, informational support decreases perceived threats and improves coping methods, which can be protective for mental health (McConnell et al., 2015). In the face of stressors in a health crisis, informational support could help decrease perceived threats, consequentially leading to more mental health support (Villagonzalo et al., 2019).
2.3.2. Emotional support
Researchers have offered various definitions of emotional support. Some have defined it to include the provision of care, empathy, love and trust (Langford et al., 1997), while others have emphasized expressions of encouragement, active listening, reflection, and reassurance (Dale et al., 2012). In this study, emotional support is defined as support in the form of caring, trust, and empathy the health information carries to social media users, which usually comes from other users in the same social media groups. Research has discovered that high emotional support mitigates the stress response and prevents the diverse stress effects on the course of depression and post-traumatic stress disorder (Mehnert et al., 2010). Emotional support is also characterized as reciprocal interactions of “mutual obligation,” but others have characterized it as solely a subjective perception of feeling accepted loved and respected (Langford et al., 1997). By and large, researchers tend to agree on the general benefits of emotional support to people's well-being and health outcomes.
2.3.3. Peer support
The peer support in this study refers to support from others who share their experiences by providing health information related to the pandemic on social media. The most effective peer support is the type of support matching the needs of social media users, who are eager to stay connected with others and share a sense of belonging to the same group (Brewer, 1991). Peer support people obtain on social media could increase self-esteem and self-efficacy, and reduce uncertainty about the self (McKenna & Bargh, 1998). Seeking support and social connection is a critical point in the lives of people with health concerns and medical conditions (Naslund et al., 2016). Overall, peer support complements communication needs for retaining social connection and reduces social isolation, which is necessary for managing mental health disorders like depression or secondary trauma.
2.4. Health behavior change
Facing the threat of COVID-19, people may use social media more for seeking health information and staying connected with others. Social media communication goes beyond the delivery of personal messages to seek the full scope of the epidemic impact, which helps develop a strong sense of disease prevention. All the life changes, in particular a stronger sense of disease prevention, could promote health behavior changes, for instance, wearing masks, using sanitizer, or washing hands. Among the health behavior theories, the Health Belief Model (Rosenstock, 1966) was developed to explain why people fail to adopt disease prevention measures or screening tests for the early detection of disease (Carpenter, 2010). The model helps understand the strategies of improving health behaviors like adherence to the treatment (Jones et al., 2014). According to HBM, people start to engage in a health-related behavior when they perceive susceptibility to a disease that has severe consequences and that the benefits to the health-related behavior outweigh the barriers (Castonguay et al., 2016).
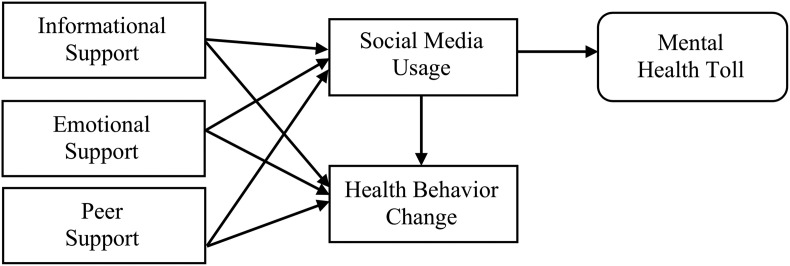
The initiation of health behavior changes can be motivated by cues to actions like perceived personal relevance of a health risk (Jones et al., 2015) or social and environmental cues like hospitals being overwhelmed by infected patients or a growing number of people sickened (Champion & Skinner, 2008). Informed by HBM, individual characteristics are also studied as modifying variables that influence perceptions and indirectly affect health behaviors (Carpenter, 2010; Jones et al., 2014). However, the role of social media content was not yet studied in the HBM literature as a cue to health behavior change. In the current health crisis, at least part of the behavior change in Wuhan residents might be attributed to social media usage. Informed by both the CREC model and HBM, we propose a conceptual model to explore mental health toll through analyzing social media usage (Fig. 1 ), which should contribute to understanding health information processing in a pandemic situation.
Fig. 1.
The conceptual model measuring mental health toll.
Based on our proposed model and literature reviewed, this study asks the following research questions:
RQ1
Did informational, emotional, and peer support people obtained from the health information on social media predict social media usage or health behavior change during Wuhan's COVID-19 outbreak?
RQ2
Did social media usage predict mental health toll like depression or secondary trauma during Wuhan's COVID-19 outbreak?
RQ3
Did social media usage predict the health behavior change among Wuhan residents?
RQ4
How did the demographic variables like age, gender, job status, and known death cases affect Wuhan residents' possible depression or secondary trauma?
3. Methods
3.1. Sampling
Using the purposive sampling method, this study recruited 558 participants who lived in all seven Wuhan urban districts, including Wuchang, Hongshan, and Jianghan districts, for an online survey that investigated how they accessed and shared health information with family members, friends and colleagues on social media. None of them reported having any depressive or traumatic disorders before the survey was conducted in early February 2020, two weeks after Wuhan was put on lockdown. The survey time represented the peak of local residents’ stress and uncertainty during the COVID-19 outbreak as no one knew what more could happened in Wuhan and when the lockdown would be lifted. A total of 238 participants were dropped out of the analyses for missing data on the main variables of interest. The final sample consisted of 320 Wuhan residents.
Specifically, typical case sampling was used, which is a common purposive sample technique, as this study focuses on the typicality or normality of Wuhan residents' response to the COVID-19 outbreak. The sampling technique requires prior knowledge of the sample and all the authors were either born or raised up in Wuhan who have known local residents well since childhood. When we recruited participants in Wuhan’ residential compounds and tower blocks, we considered the major attributes of the city population, such as age, gender, income, education background, lockdown and quarantine situations. Typical case sampling is thus appropriate for this study as it is an exploratory sampling strategy to identify the typical cases of Wuhan people's mental health. Using the latest census data published by the Wuhan government, the sample attributes largely matched with the proportion of the Wuhan population except gender. One major advantage of using the purposive sampling is that it is easier to generalize about this sample compared to a random sample of the Wuhan population, which was almost an impossible mission during the epidemic.
The respondents received no financial incentive for participating in this research, who answered questions about their demographics, social media usage, mental health conditions, and health information processing. After indicating an interest in the study, participants were sent a note via WeChat that contained the survey URL. After they completed the survey, participants were thanked and debriefed about the research design and purpose. The survey was first designed in English, which was then translated into Chinese by two bilingual researchers who are communication researchers. The final version was then reviewed by the third bilingual researcher to ensure the accurate translation of the survey, during which the cultural nuances were recognized without distortion or misinterpretation. The sample demographics are reported in Table 1 .
Table 1.
The sample demographics (N = 320).
| Demographics | n | % |
|---|---|---|
| Age (years) | ||
| 18-29 | 45 | 14.063 |
| 30-45 | 127 | 39.688 |
| 46-55 | 51 | 15.938 |
| 56-65 | 62 | 19.375 |
| 66 + | 30 | 9.375 |
| Missing | 5 | 1.563 |
| Gender | ||
| Male | 118 | 36.875 |
| Female | 202 | 63.125 |
| Education | ||
| Middle school or under | 18 | 5.625 |
| High school or equivalent | 45 | 14.063 |
| Some college | 87 | 27.188 |
| Bachelor's degree | 137 | 42.813 |
| Master's degree or higher | 33 | 10.313 |
| Job status | ||
| No job | 39 | 12.188 |
| Self-employed | 28 | 8.750 |
| Part-time work | 11 | 3.438 |
| Fulltime work | 242 | 75.625 |
| Perceived income level | ||
| Very low income | 27 | 8.438 |
| Low income | 62 | 19.375 |
| Medium income | 215 | 67.188 |
| High income | 14 | 4.375 |
| Very high income | 2 | 0.625 |
| Known death case | ||
| 0 | 234 | 73.125 |
| 1 | 50 | 15.625 |
| 2 | 23 | 7.188 |
| 3 | 10 | 3.125 |
| 4 or above | 3 | 0.938 |
3.2. Measures
This study examined social media usage and its impact on depression, secondary trauma, and health behavior change. All the scales were examined using a principal components exploratory factor analysis with varimax rotation, and a one-factor solution prevailed the analysis. Except the scale for measuring depression, the items in all other scales were assessed on a 5-point Likert-type scale ranging from 1 = strongly disagree to 5 = strongly agree.
3.2.1. Informational support
The scales of informational, emotional and peer support were adopted and revised from prior studies (Barrera et al., 2002; Oh & Lee, 2012). Four statements were used to measure informational support, which are 1) I use WeChat to gain information about how to manage the coronavirus epidemic; 2) If I have a question or need help related to the coronavirus epidemic, I can usually find the answers on WeChat; 3) I'd rather come to WeChat for information on how to manage the coronavirus epidemic than ask someone in person; and 4) On WeChat, I have learned things about managing the coronavirus epidemic I never knew anywhere else.” The scores on the four items were averaged to form the informational support index with a high level of internal consistency, M = 3.676, SD = 0.836: Cronbach's α = 0.853. A larger number indicates that the participants received more informational support.
3.2.2. Emotional support
The construct was measured by using four items, which are 1) I use the WeChat information to manage my stress caused by the coronavirus epidemic; 2) My stress levels go down while I'm engaging with others on WeChat; 3) While on WeChat, I feel I have fewer worries and concerns; 4) The health information on WeChat helps me alleviate feelings of loneliness. The scores on the four items were averaged to form the emotional support index with a high level of internal consistency, M = 3.377. SD = 0.926; Cronbach's α = 0.922. A larger number implies more emotional support.
3.2.3. Peer support
The construct was measured by using six items, which are 1) WeChat friends give me additional information about the coronavirus epidemic that I am not familiar with; 2) I use WeChat to read about other people's experience related to the coronavirus epidemic; 3) I use WeChat to share practical advice and suggestions about managing the coronavirus epidemic; 4) I would rather get advice on managing the coronavirus epidemic from WeChat friends rather than from official media; 5) I have used some of the information I learned from WeChat friends as part of my management strategies for coping with the coronavirus epidemic; and 6) It is better to get medical information from doctors, rather than someone on WeChat (Reversely coded). The scores on the six items were averaged to form the peer support index with a high internal consistency, M = 3.667, SD = 0.714, Cronbach's α = 0.867. A larger number indicates more peer support.
3.2.4. Health behavior change
The construct was self-created based on the COVID-19 situation in Wuhan, which has four items: 1) The health information on WeChat has changed many of my health behaviors, such as but not limited to wearing face masks, using sanitizer, or washing hands; 2) My changed health behaviors or habits for coping with the coronavirus epidemic are mainly due to the health information on WeChat; 3) The health information I have read on WeChat made me change my mind about the coronavirus epidemic (e.g., medicine, testing, diagnosis, and preventive actions); and 4) The moment I learn new knowledge about coronavirus on WeChat, I immediately apply it to my daily life, including health behavior change. The scores on the four items were averaged to form the index of health behavior change with a high internal consistency, M = 3.841, SD = 0.775, Cronbach's α = 0.900. A larger number indicates more change in health behavior during the outbreak.
3.2.5. Social media usage
The use of WeChat, China's dominate social media app, was measured by a 6-item instrument that was originally developed for measuring Facebook addiction (Andreassen et al., 2017). The wordings of the items were slightly revised to evaluate the WeChat use during Wuhan's COVID-19 outbreak. The participants were asked to rate how likely they agreed to the following statements: 1) You spend a lot of time thinking about the WeChat content on the epidemic or planning how to use it in preventing any disease; 2) You feel an urge to use WeChat more as you want to know more about the epidemic; 3) You keep reading/watching the WeChat content on the epidemic in order to forget about personal problems; 4) You have tried to cut down on the use of WeChat for knowing the epidemic without success; 5) You become restless or troubled if you are prohibited from using WeChat for health information on the epidemic; and 6) You use WeChat for the health information on the epidemic so much that it has had a negative impact on your life. The scores on the six items were averaged to form the index of social media usage with a high internal consistency, M = 3.081, SD = 0.834, Cronbach's α = 0.880. A larger number indicates a more excessive social media usage during the outbreak.
3.2.6. Depression
The seven out of the 21-item Depression Anxiety Stress Scale (DASS-21) (Lovibond & Lovibond, 1995) were used to measure possible depression in the sample. This is the only instrument using a 4-point Likert scale from 0 = “Do not apply to me at all” to 3 = “Applied to me very much, or most of the time.” The seven items include: “I couldn't seem to experience any positive feeling at all; ” “I found it difficult to work up the initiative to do things; ” and “I felt that life was meaningless.” DASS-21 has been translated into 40 languages, including Chinese, which has been one of the most widely used measures for discriminating between negative affective states like stress, anxiety, and depression. The scores on the seven items were averaged to form the depression index with a high internal consistency, M = 1.522, SD = 0.682, Cronbach's α = 0.939. A larger number indicates that a more depressive episode during the outbreak.
3.2.7. Secondary trauma
Considering many Wuhan residents in those initial weeks after the outbreak might not be directly infected by COVID-19 who were more likely to witness their neighbors, colleagues or family members suffering from the virus, we chose to measure whether local people showed signs of secondary trauma. Secondary trauma refers to “the natural, consequent behaviors and emotions resulting from knowledge about a traumatizing event experienced by a significant other. It is the stress resulting from helping or wanting to help a traumatized or suffering person” (Figley, 1999, p.10). This construct was measured by the Secondary Trauma Stress Scale (Bride et al., 2004). Among the 17-items instrument, three items measuring the stress in an office work environment were excluded in this study. Thus, the rest 14 items were used to measure the sample's secondary trauma with minimum wording changes, which include, “My heart started pounding when I thought about the coronavirus epidemic; ” “I had little interest in things I used to have an interest in; ” “I avoided people, places, or things that reminded me of the coronavirus epidemic; ” and “I had disturbing dreams about the coronavirus epidemic.” The scores on the 14 items were averaged to form the secondary trauma index, M = 2.331, SD = 0.800, Cronbach's α = 0.934. A larger number indicates a higher level of secondary trauma.
4. Findings
The final sample consists of 320 Wuhan residents, M age = 45.57, SD = 14.552. They were asked about gender, education background, job status (from 1 = no job to 4 = full time job), self-perceived income level in Wuhan from 1 = very low to 5 = very high as well as quarantine situations, such as residential area lockdown, limited access to public areas, known infection or death cases in their neighbors, colleagues, or family members involved. None of the variables concerning the quarantine situations were found to influence the data except known death cases, which might indicate that COVID-19 hit the whole city so badly that most people felt similar pain in those weeks. In early February, over a quarter of the Wuhan residents surveyed (26.875%) reported known death cases, in which 3.488% reported three or more deaths in their family members, colleagues, and neighbors. The sample demographics are reported in Table 1.
4.1. RQ1 – The impact of informational, emotional and peer support on social media usage or health behavior change
The data showed that the Wuhan residents obtained tremendous informational (M = 3.676, SD = 0.836) and peer (M = 3.724, SD = 0.714) support but slightly less emotional support (M = 3.377, SD = 0.926) when they accessed and shared health information about COVID-19 on WeChat. Regression analyses revealed a significant relationship between social media usage and the three types of support (Table 2 ). The three types of support explained a significant proportion of variance in the social media usage, R 2 = 0.478. This means that nearly half of the variance could be explained by the three independent variables. Thus, their social media usage could be predicted by how much informational, emotional, and peer support they received on WeChat.
Table 2.
The impact of three types of support on media exposure and health behavior change.
| Social Media Exposure (n = 299) |
Health Behavior Change (n = 321) |
|||||
|---|---|---|---|---|---|---|
| B | SEB | β | B | SEB | β | |
| Constant | −0.044 | 0.202 | 0.706 | 0.16 | ||
| Informational Support | 0.345 | 0.053 | 0.346∗∗∗ | 0.179 | 0.043 | 0.193∗∗∗ |
| Emotional Support | 0.15 | 0.054 | 0.165∗∗ | 0.166 | 0.044 | 0.199∗∗∗ |
| Peer Support | 0.356 | 0.072 | 0.297∗∗∗ | 90.515 | 0.058 | 0.475∗∗∗ |
| R2 | 0.478 | 0.58 | ||||
| Adjusted R2 | 0.473 | 0.576 | ||||
| F | 88.401∗∗∗ | 141.581∗∗∗ | ||||
Note: ∗∗p < .01, ∗∗∗p < .001.
Meanwhile, the participants also reported a series of health behavior changes, M = 3.841, SD = 0.775 after the virus spread. As shown in Table 2, there was another significant relationship between health behavior change and the informational, emotional and peer support Wuhan residents obtained on WeChat. The three types of support explained a significant proportion of variance in health behavior change, R 2 = 0.580, indicating that over half of the variance could be explained by the three independent variables. Thus, their health behavior change could be predicted by the informational, emotional and peer support they received on WeChat.
4.2. RQ2 – Social media usage predicts depression and secondary trauma
To answer RQ2, structural equation modeling (SEM) was performed to explore the relationship between social media usage and mental health toll like depression (Model 1) and secondary trauma (Model 2). We used the software SmartPLS to produce the partial least squares (PLS) path modeling, a variance-based SEM that allows estimating complex cause-effect relationship models with latent variables. This approach offers insights on several significant relationships between key variables holistically with the whole model fit being considered. Reliability tests were conducted for all the measurements in the SEM and all the scores of Average Variance Extracted (AVE) were higher than 0.5, indicating good convergent validity. Meanwhile, Cronbach's alpha values for all the measurements were higher than 0.7, indicating an overall satisfaction with reliability.
Internal consistency of the measurements was analyzed by calculating the composite reliability scores and the results showed that all the composite reliability scores were higher than 0.7, demonstrating a good reliability for both Model 1 and Model 2 (Nunnally, 1978). The discriminant validity was also evaluated by comparing the correlation coefficient with the square roots of the AVEs, the former was all bigger than the latter, which indicate good reliability of the scales used. The model fit evaluation requires the Standardized Root Mean Square Residual (SRMR) score to be less than 0.08, which is the benchmark for a good fit model (Hu & Bentler, 1998). For Model 1, SRMR = 0.057, and for Model 2, SRMR = 0.064. Both the SRMR scores are below 0.08, demonstrating a good model fit.
Factorial reliability of the scales in the two models were then evaluated by conducting factor analyses in SPSS, the result for Bartlett's Test of Sphericity is shown as Kaiser-Meyer-Olkin Measure of sampling adequacy (KMO) with Model 1, KMO score = 0.930, p < .001 and Model 2, KMO score = 0.934, p < .001, showing a good reliability for the two models (Pan, Lu, & Gupta, 2014). Finally, common-method bias was evaluated by Harman's single-factor test. In each of the two models, six factors were extracted in factor analysis. In Model 1, the first factor accounts for 39.400% of the variance and all the six factors 71.958%, while in Model 2, the first factor accounts for 36.132% of the variance and the six factors 65.860%. Thus, no common method bias was detected in this research (see Podsakoff et al., 2003).
A total of 280 participants reported their level of depression and 291 on secondary trauma in the survey, while the rest skipped the two measurements. Based on the DASS-21 (Lovibond & Lovibond, 1995), 159 participants, or 49.7%, reported having the normal level of depression, 60 or 18.8% suffered the mild level, 44 or 13.8% the moderate level, and 17 or 5.3% the severe level of depression. More than half of the respondents reported some level of depression with nearly 20% of them suffering moderate or severe depression. The measurement for secondary trauma did not provide similar benchmarks to this scale from normal to severe state. Among those reporting secondary trauma (n = 291), this study finds that most respondents (n = 232, 79.70%) reported the low level of secondary trauma, and 39, or 13.4%, reported the moderate level of secondary trauma and 20, or 6.9%, the high level of secondary trauma.
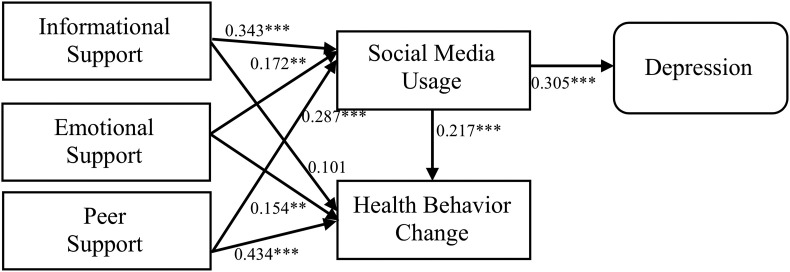
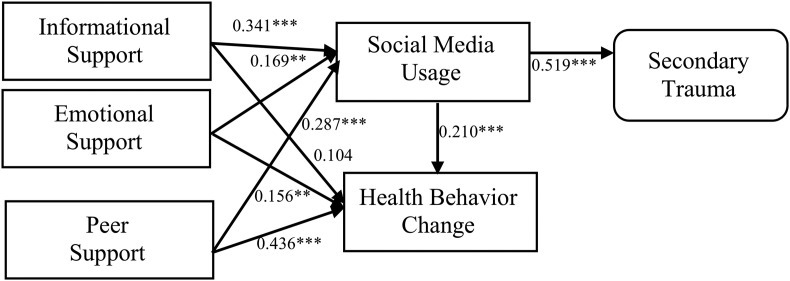
As shown in Fig. 2 , the SEM reveals that social media usage could significantly predict depression, indicating that an excessive social media usage contributed to more severe depression. Analyses also discovered that social media usage could significantly predict secondary trauma, suggesting that an excessive use of social media leaded to more severe secondary trauma (Fig. 3 ).
Fig. 2.
Model 1 measuring depression. Note: ∗∗p < .01, ∗∗∗p < .001. SRMR = 0.057.
Fig. 3.
Model 2 measuring secondary trauma. Note: ∗∗p < .01, ∗∗∗p < .001. SRMR = 0.064.
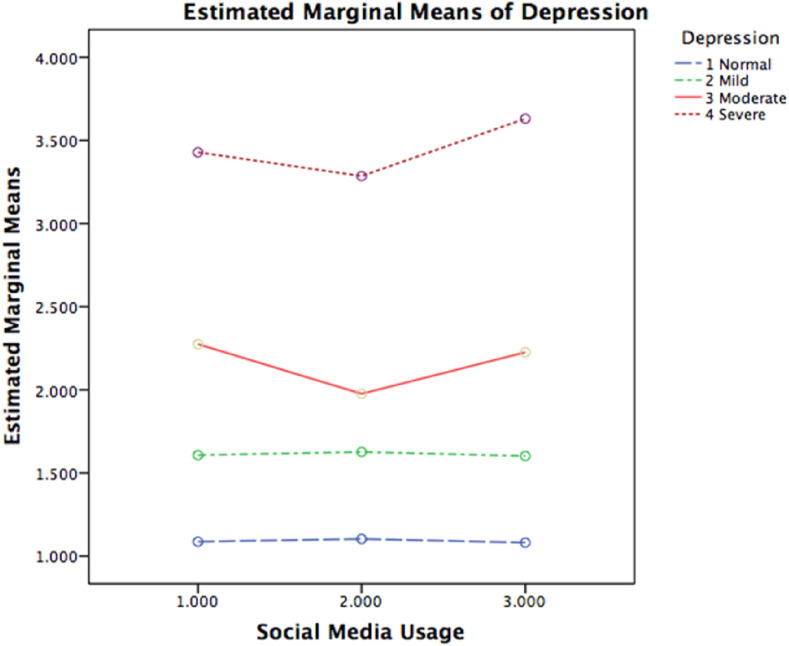
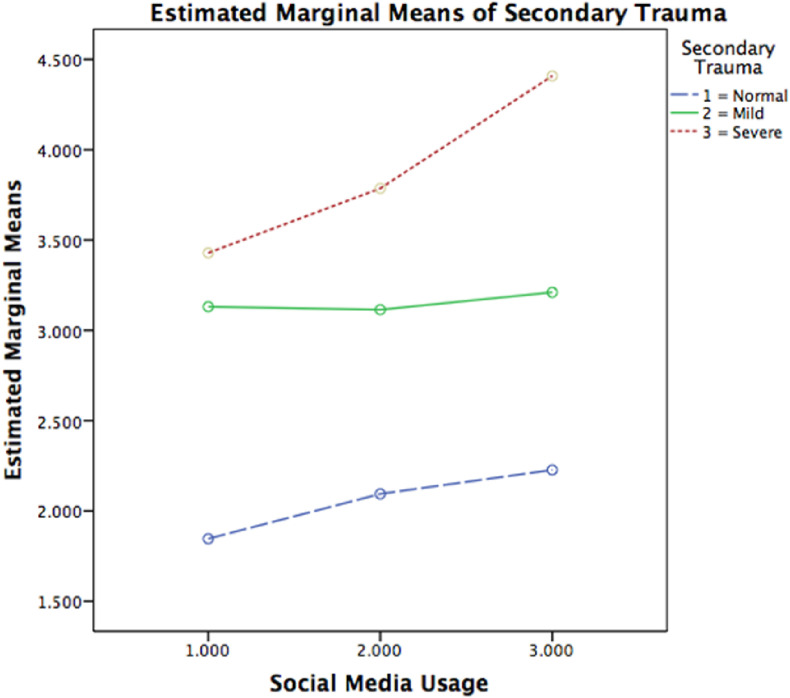
For a better understanding of the associations between social media usage and mental health toll at different levels, we recoded the social media usage into three categories (1 = light use, 2 = moderate use, and 3 = heavy use). Similarly, following Lovibond and Lovibond (1995), the depression was categorized into four levels from 1 = normal, 2 = mild, 3 = moderate to 4 = severe (Fig. 4 ) and the secondary trauma into three levels from 1 = normal, 2 = moderate to 3 = severe. Then a 4 (four levels of depression) x 3 (three levels of social media usage) between groups factorial ANOVA was also conducted with categorical depression and social media usage as between-groups factors and depression as the dependent variable. The main effect of depression is significant, F (3, 268) = 530.649, p < .000. So does the main effect of social media usage, F (2, 268) = 5.596, p < .01. A significant interaction between depression and social media usage was also observed, F (6, 268) = 3.644, p < .01.
Fig. 4.
The impact of social media usage on normal, mild and sever levels of depression.
Similarly, a 3 (three levels of secondary trauma) × 3 (three levels of social media usage) between groups factorial ANOVA was conducted with categorical constructs of secondary trauma and social media usage as between-groups factors and secondary trauma as the dependent variable. The main effect of secondary trauma is significant, F (2, 282) = 122.177, p < .000. So does the main effect of social media usage, F (2, 282) = 6.414, p < .01, but no interaction between secondary trauma and social media usage was detected, F (4, 282) = 1.696, p = .151. Hence, the two ANOVA analyses demonstrated a clear pattern that the group who reported the highest level of social media usage were afflicted the most by depression (Fig. 4) and secondary trauma (Fig. 5 ).
Fig. 5.
The social media usage impact on secondary trauma.
4.3. RQ3 – Social media usage and health behavior change
As shown in Fig. 2, Fig. 3, there is a significant relationship between social media usage and health behavior change in both Models 1 and 2. The participants’ health behavior changes were significantly influenced by social media usage. The more they used WeChat during the COVID-19 outbreak, the more likely they were to change health behaviors. It is worth noting that health behavior changes in Models 1 and 2 was not affected much by informational support but significantly influenced by both emotional and peer support of the health information on WeChat. This pattern remained the same in both Models 1 and 2 (see Fig. 2, Fig. 3).
4.4. RQ4 – The impact of demographics on depression and secondary trauma
Finally, we evaluated how the demographic variables might contribute to mental health toll. Regression analyses discover that some demographic variables could predict depression or secondary trauma. As shown in Table 3, known death cases could significantly predict depression but no other variables had the same effect. This means that the more death cases they knew among their neighbors, colleagues, or family members, the more depressive they felt during the epidemic. No other demographic variables were founded to influence depression. For secondary trauma, age, gender, job status, and known death cases could predict secondary trauma. This means that those who were older, female, knew more death cases, and had a more stable job were more likely to suffer from secondary trauma (see Table 3 ). The level of education was not found to be associated with either depression or secondary trauma, indicating that all respondents might suffer from depression or secondary trauma similarly regardless of their education backgrounds.
Table 3.
The impact of demographics on depression and secondary trauma.
| Depression (n = 280) |
Secondary Trauma (n = 291) |
|||||
|---|---|---|---|---|---|---|
| B | SEB | β | B | SEB | β | |
| Constant | 1.171 | 0.265 | 1.853 | 0.306 | ||
| Age | −0.005 | 0.003 | −0.109 | −0.009 | 0.004 | −0.163∗∗ |
| Gender | 0.125 | 0.084 | 0.089 | 0.21 | 0.096 | 0.126∗ |
| Education | −0.03 | 0.041 | −0.046 | −0.058 | 0.047 | −0.073 |
| Job | 0.07 | 0.045 | 0.106 | 0.124 | 0.051 | 0.156∗ |
| Death | 0.16 | 0.048 | 0.197∗∗∗ | 0.219 | 0.056 | 0.226∗∗∗ |
| R2 | 0.056 | 0.089 | ||||
| Adjusted R2 | 0.039 | 0.073 | ||||
| F | 3.205∗∗ | 3.308∗∗∗ | ||||
Note: ∗p < .05, ∗∗p < .01, ∗∗∗p < .001.
5. Discussion
A public health crisis almost always brings stern worries and anxiety to those under attack. The COVID-19 pandemic, however, has brought with it a whole new set of fears about the absence of a vaccine or medication, shortage of ventilators, imposing social distancing, wearing masks, escalating economic woes, and concerns about the well-being of loved ones. Such fears were quite evident among Wuhan residents as China was the first country afflicted by the COVID-19 pandemic and Wuhan became the first epicenter of the global health crisis. But it was quite a challenge to reveal certain invisible harm caused by the virus, including the toll on mental health like depression and secondary trauma.
The study uncovers the invisible harm such as depression and secondary trauma in Wuhan residents after the COVID-19 outbreak struck their city, implying how vulnerable people's mental health could be in such a crisis. The results disclose that when COVID-19 started to spread in Wuhan, it made nearly one in every five persons (19.2%) suffered from a moderate to severe level of depression and slightly more than one in every five persons (20.3%) showed from a moderate to severe level of secondary trauma. Those weeks were obviously a nerve-wracking period for Wuhan residents as they were the first group faced the initial waves of the deadly outbreak. Moreover, their mental health toll was found to be associated with social media usage and health behavior change.
To Wuhan residents, social media usage and health behavior change were found to help mitigate the threats of COVID-19 in the absence of testing kits or vaccines. They had obtained a significant amount of informational, emotional and peer support from the health information they accessed and shared on WeChat. The three types of support from health information were found to predict social media usage. In other words, the more support Wuhan residents obtained, the more they relied on WeChat for health information. It is also possible that more use of social media leads to higher levels of informational, emotional, and peer support, though no analysis was conducted to prove it. However, Wuhan people's health behavior changes like wearing face masks or washing hands can only be predicted by emotional and peer support but not by informational support. This implies that health information alone may not be able to change people's health behaviors, while an emotional touch or the influence of other community members embedded in the health information on social media showed a much stronger influence on behavior change.
Several unique characteristics of China's COVID-19 epidemic patterns and health policies, including delayed response from public health officials and censored information on the infectious disease in official news outlets, could prompt a heightened public mental health crisis. In those initial weeks after the outbreak, both online and offline health information about COVID-19 was constantly censored by officials, which drove people to social media for meeting health information needs in their friends' circle. China's tightly controlled media environment should be factored in understanding why Wuhan residents relied so much on social media (i.e., WeChat) for accessing health information. The content on Weibo, another popular social media app in China that functions like Twitter, was not included in the analyses as it was much less used for accessing health information related to COVID-19 because the Weibo content was more often and easily censored than that on WeChat. This may explain why Weibo was not used much by Wuhan residents in the current research.
It is evident that social media usage helped manage stressors and health risks, which can be predicted by the informational, emotional, and peer support they received from the shared health information. Meanwhile, this study finds that the overexposure to health information on social media could take a toll on mental health, i.e., developing depression or secondary trauma. It was possible those who consumed more health information on WeChat could attach excessive importance to the social media content, who, as this study discovers, also reported suffering more from depression or secondary trauma than those who used less. The findings serve as a timely reminder that people might need to take a social media break during a stressful health disaster like the COVID-19 pandemic.
However, this does not make social media the culprit for depression or secondary trauma. On the contrary, this study shows that Wuhan residents benefited from using social media, which was perceived as an important activity in those lockdown weeks. Indeed, in the face of fear caused by a public health crisis, we should never be overly confident that people would know how to balance social media usage and its impact on mental health. In other words, it would be hard for people to obtain ample informational, emotional, and peer support from the health information on social media but stop right before it might take a toll on their mental health. Without an easy access to health information might also cause stress or anxiety, which, in turn, could make those in Wuhan vulnerable to emotional toll.
5.1. Theoretical and practical implications
Informed by the CERC model and HBM, this research proposed a conceptual model exploring possible associations between social media usage and mental health toll or health behavior change. The proposed model makes contribution to the literature by applying the two theoretical frameworks, i.e., CERC model and HBM, to investigating an on-going public health crisis. This research treated social media usage as a cue to action concerning health behavior change, which, as we know, was not reported in the existing HBM literature. The COVID-19 pandemic is one of the most devastating catastrophes humans have experienced psychologically. Thus, we call for more scholarship equipped with new theoretical models to investigate the detrimental effects in public health crises. The current research represents part of the effort.
Practical implications can be drawn from this study for developing effective strategies to manage mental health during a public health crisis. This study provides evidence-based insights to offering metal healthcare to those who suffered psychologically during a pandemic, which emphasizes health policy and service development moving away from institutional care of mental health towards family- or community-based services. Knowing the underlying nature of mental health toll makes it possible to care mental health disorders at home or community, especially, when the hospitals and other medical resources were overwhelmed by patients sickened by infectious diseases during a pandemic. Historically, viruses have been the lethal foe of human beings. Our immune systems have evolved to protect our physical health in most cases but not nearly much concerning our psychologies. Public health officials should pay more attention to it in the health policy-making, who could help a lot even when they simply remind the public of taking a media break during a pandemic.
5.2. Limitations and future studies
Several limitations should be addressed when interpreting the results of this study. It was extremely difficult to collect data from Wuhan residents during the most traumatic time when facing risks and uncertainty after coronavirus hit their hometown. Many residents reported that they felt too sad to complete the survey, including recalling how many loved ones being infected or died. Anyone could stop at any time during the survey, which was the main reason that over 200 participants stopped soon after they began to answer questions. This should be factored into the interpretation of the results based on the purposive sample. The findings are also limited by using a non-probability sampling, and by the fact that the sample was skewed toward more female respondents. Hence, the results should be interpreted in consideration of possible gender-related biases.
This study was conducted in early February 2020 before we had a basic understanding of its global scope, which relied solely on self-reported data from the survey. No data were collected through interviews or participant observation, which would enable researchers to achieve a deeper understanding of the role of social media usage and how it might affect health behavior change and mental health. Future studies may calculate a mental health index, measures concerning the susceptibility of mental health states like stress, anxiety, depression, and traumatic disorders by analyzing how people seek and share health information on social media.
Other limitations include that this study was based on a one-time survey of Wuhan residents, in which some respondents might not feel comfortable providing answers disclosing their true mental stress. It was possible that some knew how to cope with the stress as the pandemic drags on, while others could develop post-traumatic stress disorder, which had no chance to test. Future longitudinal studies are needed to further test the causal relationships in the conceptual model proposed in this study.
Finally, the current research did not address developing possible intervention strategies and health policies that mitigate mental health toll during the COVID-19 crisis and beyond. Future studies may help work out some coping methods through identifying predictors for the susceptibility of mental health and health behavior change. These insights are critical in building a robust health ecosystem during a public health crisis.
6. Conclusion
This study adds empirical evidence to the devastating effect of COVID-19 pandemic on people's mental health. To public health officials, a patchwork response to the unprecedented COVID-19 pandemic could complicate the overall coping strategies. At an individual level, a panic response to the infectious disease with no cure in sight could be psychologically perilous to mental health. In the face of medical uncertainty, this study finds that people relied heavily on social media for accessing health information in their own social media groups. As the virus strikes, it makes evolutionary sense for people to develop a strong sense of sharing health information in the hope of surviving the outbreak. This research finds that an excessive use of social media content during a public health crisis could be rewarding in terms of obtaining informational, emotional and peer support, but at the same time, it might take a toll on mental health. There is no easy fix to people's stress disorders during a pandemic. Some may choose ordinary coping methods they used before to deal with new stressors, while others try to reinforce a strong sense of resilience. The findings imply that taking a social media break from time to time helps improve people's mental well-being during the COVID-19 pandemic.
CRediT authorship contribution statement
Bu Zhong: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing, Project administration, Supervision, Validation. Yakun Huang: Conceptualization, Investigation, Data curation. Qian Liu: Methodology, Data curation, Visualization, Formal analysis, Writing - original draft, Writing - review & editing, Validation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.chb.2020.106524.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- Andreassen C.S., Pallesen S., Griffiths M.D. The relationship between addictive use of social media, narcissism, and self-esteem: Findings from a large national survey. Addictive Behaviors. 2017;64:287–293. doi: 10.1016/j.addbeh.2016.03.006. [DOI] [PubMed] [Google Scholar]
- Antonucci T.C. Psychology of social support. In: Wright J.D., editor. International encyclopedia of the social and behavioral sciences. Elsevier; 2001. pp. 14465–14469. [Google Scholar]
- Avery E. Contextual and audience moderators of channel selection and message reception of public health information in routine and crisis situations. Journal of Public Relations Research. 2010;22(4):378–403. doi: 10.1080/10627261003801404. [DOI] [Google Scholar]
- Avery E. Public information officers' social media monitoring during the Zika virus crisis, a global health threat surrounded by public uncertainty. Public Relations Review. 2017;43(3):468–476. doi: 10.1016/j.pubrev.2017.02.018. [DOI] [Google Scholar]
- Barrera M., Jr., Glasgow R.E., McKay H.G., Boles S.M., Feil E.G. Do Internet-based support interventions change perceptions of social support?: An experimental trial of approaches for supporting diabetes self-management. American Journal of Community Psychology. 2002;30(3):637–654. doi: 10.1023/A:1016369114780. [DOI] [PubMed] [Google Scholar]
- Brashers D.E., Neidig J.L., Haas S.M., Dobbs L.K., Cardillo L.W., Russell J.A. Communication in the management of uncertainty: The case of persons living with HIV or AIDS. Communication Monographs. 2000;67(1):63–84. doi: 10.1080/03637750009376495. [DOI] [Google Scholar]
- Brewer M.B. The social self: On being the same and different at the same time. Personality and Social Psychology Bulletin. 1991;17(5):475–482. doi: 10.1177/0146167291175001. [DOI] [Google Scholar]
- Bride B.E., Robinson M.R., Yegidis B., Figley C.R. Development and validation of the secondary traumatic stress scale. Research on Social Work Practice. 2004;14(1):27–35. doi: 10.1177/1049731503254106. [DOI] [Google Scholar]
- de Calheiros Velozo J., Stauder J.E.A. Exploring social media use as a composite construct to understand itsrelation to mental health: A pilot study on adolescents. Children and Youth Services Review. 2018;91:398–402. [Google Scholar]
- Carpenter C.J. A meta-analysis of the effectiveness of Health Belief Model variables in pedicting behavior. Health Communication. 2010;25(8):661–669. doi: 10.1080/10410236.2010.521906. [DOI] [PubMed] [Google Scholar]
- Castonguay J., Filer C.R., Pittsb M.J. Seeking help for depression: Applying the health belief model to illness. Southern Communication Journal. 2016;81(5):289–303. doi: 10.1080/1041794X.2016.1165729. [DOI] [Google Scholar]
- CDC . 2018. Cerc: Crisis + emergency risk communication.https://emergency.cdc.gov/cerc/ppt/CERC_Introduction.pdf [Google Scholar]
- Champion V.L., Skinner C.S. The health belief model. In: Glanz K., Rimer B.K., Viswanath K., Orleans C.T., editors. Health behavior and health education theory, research, and practice. 4th ed. Jossey-Bass; 2008. pp. 45–66.http://ezaccess.libraries.psu.edu/login?url=http://ebookcentral.proquest.com/lib/pensu/detail.action?docID=353367 [Google Scholar]
- Dale J.R., Williams S.M., Bowyer V. What is the effect of peer support on diabetes outcomes in adults? A systematic review. Diabetic Medicine. 2012;29(11):1361–1377. doi: 10.1111/j.1464-5491.2012.03749.x. [DOI] [PubMed] [Google Scholar]
- Hu L., Bentler P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. doi: 10.1037/1082-989X.3.4.424. [DOI] [Google Scholar]
- Hu B., Zhang D. channel selection and knowledge acquisition during the 2009 beijing H1N1 flu crisis: A media system dependency theory perspective. Chinese Journal of Communication. 2014;7(3):299–318. doi: 10.1080/17544750.2014.926951. [DOI] [Google Scholar]
- Jones C.L., Jensen J.D., Scherr C.L., Brown N.R., Christy K., Weaver J. The Health Belief Model as an explanatory framework in communication research: Exploring parallel, serial, and moderated mediation. Health Communication. 2015;30(6):566–576. doi: 10.1080/10410236.2013.873363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C.J., Smith H., Llewellyn C. Evaluating the effectiveness of health belief model interventions in improving adherence: A systematic review. Health Psychology Review. 2014;8(3):253–269. doi: 10.1080/17437199.2013.802623. [DOI] [PubMed] [Google Scholar]
- King G., Pan J., Roberts M.E. How censorship in China allows government criticism but silences collective expression. American Political Science Review. 2013;107(2):326–343. doi: 10.1017/S00030554. [DOI] [Google Scholar]
- Lachlan K.A., Spence P.R., Lin X., Najarian K., Greco M.d. Social media and crisis management: CERC, search strategies, and twitter content. Computers in Human Behavior. 2016;54:647–652. doi: 10.1016/j.chb.2015.05.027. [DOI] [Google Scholar]
- Langford C.P.H., Bowsher J., Maloney J.P., Lillis P.P. Social support: A conceptual analysis. Journal of Advanced Nursing. 1997;25(1):95–100. doi: 10.1046/j.1365-2648.1997.1997025095.x. [DOI] [PubMed] [Google Scholar]
- Lin C., Ding Y., Xie B., Sun Z., Li X., Chen Z., Niu M. Asymptomatic novel coronavirus pneumonia patient outside Wuhan: Thevalue of CT images in the course of the disease. 2020;63:7–9. doi: 10.1016/j.clinimag.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang X., Lin X., Hajli M. Seeking and sharing health information on social media: A net valence model and cross-cultural comparison. Technological Forecasting and Social Change. 2018;126:28–40. doi: 10.1016/j.techfore.2016.07.021. [DOI] [Google Scholar]
- Lovibond S.H., Lovibond P.F. Psychology Foundation of Australia; 1995. Manual for the depression anxiety stress scales. [Google Scholar]
- McConnell E.A., Birkett M.A., Mustanski B. Typologies of social support and associations with mental health outcomes among LGBT youth. LGBT Health. 2015;2(1):55–61. doi: 10.1089/lgbt.2014.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna K.Y.A., Bargh J.A. Coming out in the age of the Internet: Identity "demarginalization" through virtual group participation. Journal of Personality and Social Psychology. 1998;75(3):681–694. doi: 10.1037/0022-3514.75.3.681. [DOI] [Google Scholar]
- Meadows C.W., Meadows C.Z., Tang L., Liu W. Unraveling public health crises across stages: Understanding Twitter emotions and message types during the California measles outbreak. Communication Studies. 2019;70(4):453–469. doi: 10.1080/10510974.2019.1582546. [DOI] [Google Scholar]
- Mehnert A., Lehmann C., Graefen M., Huland H., Koch U. Depression, anxiety, post-traumatic stress disorder and health-related quality of life and its association with social support in ambulatory prostate cancer patients. European Journal of Cancer Care. 2010;19(6):736–745. doi: 10.1111/j.1365-2354.2009.01117.x. [DOI] [PubMed] [Google Scholar]
- Naslund J.A., Aschbrenner K.A., Marsch L.A., Bartels S.J. The future of mental health care: Peer-to-peer support and social media. Epidemiology and Psychiatric Sciences. 2016;25(2):113–122. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally J.C. 2nd ed. McGraw-Hill; 1978. Psychometric theory. [Google Scholar]
- Oh H.J., Lee B. The effect of computer-mediated social support in online communities on patient empowerment and doctor patient communication. Health Communication. 2012;27(1):30–41. doi: 10.1080/10410236.2011.567449. [DOI] [PubMed] [Google Scholar]
- Ouyang A., Inverso N.A., Chow S.-M., Kumar A., Zhong B. Listening" to IBS patients in the 21st century: Offerings from an online self help and support group. Gastroenterology. 2016;150(4) doi: 10.1016/S0016-5085(16)32510-0. S739-S739. [DOI] [Google Scholar]
- Park S., Boatwright B., Avery E. Information channel preference in health crisis: Exploring the roles of perceived risk, preparedness, knowledge, and intent to follow directives. Public Relations Review. 2019;45(5):1–8. doi: 10.1016/j.pubrev.2019.05.015. [DOI] [Google Scholar]
- Patel A., Jernigan D.B. Novel coronavirus (2019-nCoV) situation report - 1. Morbidity and Mortality Weekly Report. 2020;69(5):140–146. doi: 10.15585/mmwr.mm6905e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff P.M., MacKenzie S.B., Lee J.-Y., Podsakoff N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Reynolds B., Seeger M.W. Crisis and emergency risk communication as an integrative model. Journal of Health Communication. 2005;10(1):43–55. doi: 10.1080/10810730590904571. [DOI] [PubMed] [Google Scholar]
- Rosenstock I.M. Why people use health services. Milbank Memorial Fund Quarterly. 1966;44(3):94–124. doi: 10.1111/j.1468-0009.2005.00425.x. 1966. [DOI] [PubMed] [Google Scholar]
- Rosenstock I.M. Historical origins of the health belief model. Health Education Monographs. 1974;2(4):328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Roundtree A.K. Social health content and activity on Facebook: A survey study. Journal of Technical Writing and Communication. 2016;47(3):300–329. doi: 10.1177/0047281616641925. [DOI] [Google Scholar]
- Selkie E., Adkins V., Masters E., Bajpai A., Shumer D. Transgender adolescents' uses of social media for social support. Journal of Adolescent Health. 2020;66(3):275–280. doi: 10.1016/j.jadohealth.2019.08.011. [DOI] [PubMed] [Google Scholar]
- Stephens M.H., Petrie K.J. Social support and recovery from disease and medical procedures. In: Wright J.D., editor. International encyclopedia of the social & behavioral sciences. Elsevier; 2015. pp. 735–740. [DOI] [Google Scholar]
- Tengku Mohd T.A.M., Yunus R.M., Hairi F., Hairi N.N., Choo W.Y. Social support and depression among community dwelling older adults in asia: A systematic review. BMJ Open. 2019;9(7):1–12. doi: 10.1136/bmjopen-2018-026667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet COVID-19: Fighting panic with information. The Lancet. 2020;395(10224):537. doi: 10.1016/S0140-6736(20)30379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonsaker T., Bartlett G., Trpkov C. Health information on the internet: Gold mine or minefield? Canadian Family Physician. 2014;60(5):407–408. [PMC free article] [PubMed] [Google Scholar]
- Uchino B.N., Bowen K., de Grey R.K., Mikel J., Fisher E.B. Social support and physical health: Models, mechanisms, and opportunities. In: Fisher E.B., Cameron L.D., Christensen A.J., Ehlert U., Guo Y., Oldenburg B., Snoek F.J., editors. Principles and concepts of behavioral medicine: A global handbook. Springer; 2018. pp. 341–372. [DOI] [Google Scholar]
- Villagonzalo K.-A., Arnold C., Farhall J., Rossell S.L., Foley F., Thomas N. Predictors of overall and mental health-related internet use in adults with psychosis. Psychiatry Research. 2019;278:12–18. doi: 10.1016/j.psychres.2019.05.034. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization: Coronavirus disease (COVID-2019) situation reports; 2020. Novel coronavirus (2019-nCoV) situation report -1.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf [Google Scholar]
- Yang F., Zhong B., Kumar A., Chow S.-M., Ouyang A. Exchanging social support online: A longitudinal social network analysis of irritable bowel syndrome patients' interactions on a health forum. Journalism & Mass Communication Quarterly. 2018;95(4):1033–1057. doi: 10.1177/1077699017729815. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.