Abstract
Rationale and Objectives
While affiliated imaging centers play an important role in healthcare systems, little is known of how their operations are impacted by the COVID-19 pandemic. Our goal was to investigate imaging volume trends during the pandemic at our large academic hospital compared to the affiliated imaging centers.
Materials and Methods
This was a descriptive retrospective study of imaging volume from an academic hospital (main hospital campus) and its affiliated imaging centers from January 1 through May 21, 2020. Imaging volume assessment was separated into prestate of emergency (SOE) period (before SOE in Massachusetts on March 10, 2020), “post-SOE” period (time after “nonessential” services closure on March 24, 2020), and “transition” period (between pre-SOE and post-SOE).
Results
Imaging volume began to decrease on March 11, 2020, after hospital policy to delay nonessential studies. The average weekly imaging volume during the post-SOE period declined by 54% at the main hospital campus and 64% at the affiliated imaging centers. The rate of imaging volume recovery was slower for affiliated imaging centers (slope = 6.95 for weekdays) compared to main hospital campus (slope = 7.18 for weekdays). CT, radiography, and ultrasound exhibited the lowest volume loss, with weekly volume decrease of 41%, 49%, and 53%, respectively, at the main hospital campus, and 43%, 61%, and 60%, respectively, at affiliated imaging centers. Mammography had the greatest volume loss of 92% at both the main hospital campus and affiliated imaging centers.
Conclusion
Affiliated imaging center volume decreased to a greater degree than the main hospital campus and showed a slower rate of recovery. Furthermore, the trend in imaging volume and recovery were temporally related to public health announcements and COVID-19 cases.
Key words: COVID-19, Pandemic, Radiology operation, Imaging volume, Service locations
Introduction
On December 31, 2019, China reported a cluster of 41 cases of an unusual pneumonia in Wuhan (1). Since then, the SARS-CoV-2 virus, manifesting as coronavirus disease 2019 (COVID-19), has become a global pandemic, infecting more than 9 million people worldwide by June 20, 2020 (2,3). By late March, the United States led the world in the number of confirmed COVID-19 cases (4). By the end of May, the death toll related to COVID-19 had surpassed 100,000 in the United States with daily new cases still exceeding 10,000 (5). The first case of COVID-19 in Massachusetts was reported on January 29, 2020, followed by the first case in Boston on February 1, 2020. Massachusetts’ governor, Charlie Baker, declared a “state of emergency” on March 10, 2020. In the ensuing weeks, Massachusetts implemented measures to mitigate the spread of COVID-19 by creating policies that limited public gatherings, prohibited on-premises food and drink consumption in restaurants, and enforced closure of nonessential services (6).
The COVID-19 pandemic has devastated the global economy and has had sweeping effects on the health care sector (7, 8, 9). In addition to policies and announcements of the federal government and Centers for Disease Control and Prevention (CDC), local and state governmental policies have played pivotal roles in influencing healthcare operations, such as encouraging rescheduling of elective clinical visits and surgeries in order to slow the transmission of COVID-19 and to conserve healthcare resources (10). During this time, radiology departments have experienced a corresponding drastic decline in imaging volume (11).
Naidich et al. recently reported a decrease in imaging volume by as much as 88% at Northwell Health (11). In addition, outpatient imaging volume was shown to be disproportionately affected compared to inpatient volume due to postponement of elective patient visits and surgeries (12). Although affiliated imaging centers play an important role in the operation of numerous healthcare systems, little is known of how their operations are impacted by the COVID-19 pandemic. Towards the end of March, imaging volumes in certain regions of Europe have shown a slight increase since the nadir earlier in the month (13). Such rebound has not been extensively investigated in the United States (14).
The purpose of our study is to investigate the impact of the COVID-19 pandemic on overall radiology imaging volume at a large academic hospital campus compared to its affiliated imaging centers.
Materials and methods
Study Setting
This was a single-institution, retrospective collection of aggregate data that was compliant with the health insurance portability and accountability act (HIPAA) and approved with exemption by our Institutional Review Board (IRB). This was a retrospective study including all diagnostic imaging studies performed at our large urban academic hospital (main hospital campus) and its affiliated imaging centers (including urgent care centers) from January 1, 2020 to May 21, 2020. Our institution is a 1011 bed quaternary care urban academic medical center in Boston, MA, and yearly sees approximately 50,000 inpatients, 110,000 ED patients, and 1.5 million outpatients. Twenty-six affiliated imaging centers were included in this study. Our institution employs approximately 126 part or full-time radiologists at main campus, a portion of which generally staff affiliated centers, either on-site or remotely. On-site radiologists at affiliated sites may range from zero to approximately ten at any given time, although the number on-site is recently decreased in the setting of COVID and remote workflow being implemented. The data was extracted from the hospital enterprise medical imaging data warehouse as daily volumes.
Imaging Modality
All diagnostic imaging studies were classified according to patient service location (main hospital campus or affiliated imaging center) and modality type (mammography, magnetic resonance imaging [MRI], nuclear medicine, ultrasound, computed tomography [CT], and radiography). Imaging studies at the main hospital campus included inpatient, outpatient, and emergency room exams, and studies at the affiliated imaging centers included mainly of outpatient and lower acuity urgent care exams.
Local and National Health Announcements
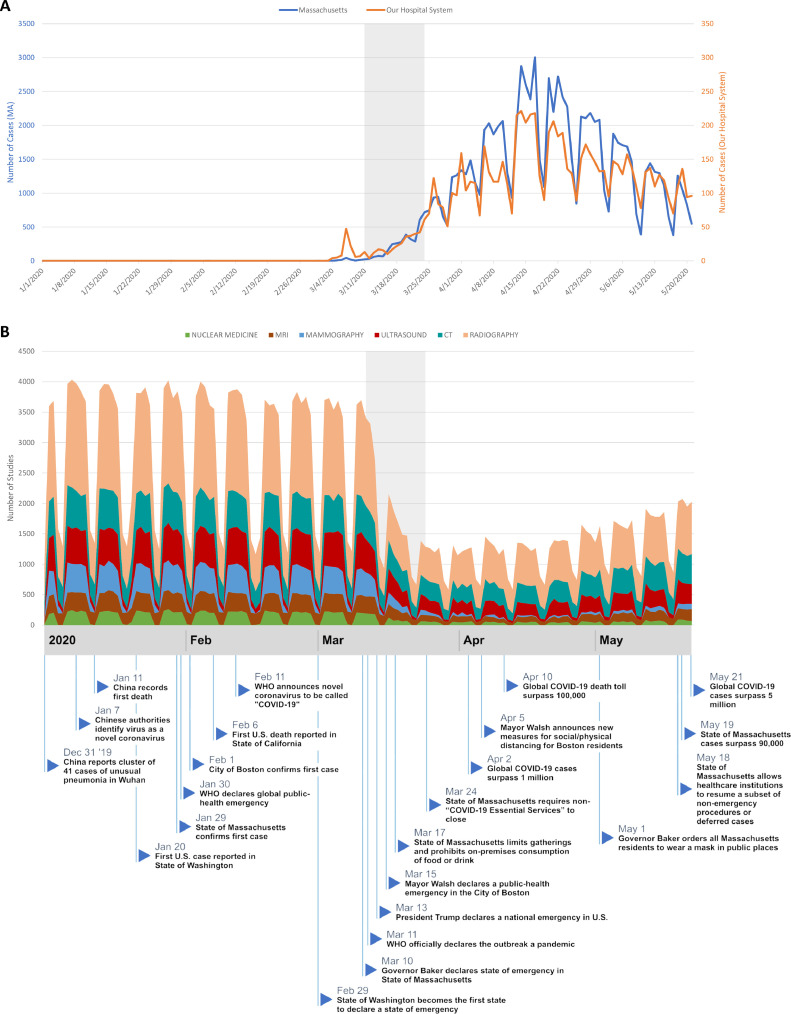
Major local and national public health information was obtained through the official CDC, World Health Organization, and Business Insider webpages (15, 16, 17). Publicly available data of COVID-19 cases in Massachusetts as well as Massachusetts public health announcements were obtained using the Massachusetts and Boston COVID-19 Response Reporting websites (mass.gov and boston.gov) (6,18). Major events were plotted on a timeline in relationship to imaging volume change (Fig 1 ).
Fig. 1.
(a) Daily new COVID-19 cases in state of Massachusetts and across our healthcare system from January 1, 2020 through May 21, 2020. (b) Timeline of imaging volume during the COVID-19 pandemic. Daily imaging volume by modality type at the main hospital campus and affiliated imaging centers and new COVID-19 cases in Massachusetts from January 1, 2020 to May 21, 2020. The blue flags mark notable local, state, and national COVID-19 events. The periodic pattern in imaging volume and COVID-19 census comes from the weekly pattern, with lower numbers corresponding to weekends. (Color version of figure is available online.)
Statistical Analysis
For descriptive analysis of change in imaging volume over time, three time periods were designated: “pre-SOE (state of emergency)” (time before the declaration of SOE in Massachusetts on March 10, 2020), “post-SOE” (time after the requirement of closure of “nonessential” services on March 24, 2020), and “transition” (time between pre-SOE and post-SOE periods).
For averaged weekly imaging volume assessment, data from January 5, 2020 to May 16, 2020 was used to ensure that the weeks were defined as Sunday to Saturday. For comparison of weekly imaging volume, weeks 1 through 9 (January 5, 2020 through March 7th, 2020) were considered to represent the “pre-SOE” period and weeks 12 through 19 (March 22, 2020 through May 16, 2020) were considered to represent the “post-SOE” period. Weeks 10 through 11 were considered to represent the “transition” period and were not included in this portion of the analysis, as imaging volume sharply decreased during this period before reaching a new relatively stable post-SOE equilibrium.
Descriptive statistics of imaging volume trends were further assessed via interrupted time series analysis using the total daily volume for each location based on the three designated time periods as described. Weekdays and weekends/public holidays were analyzed independently using interrupted time series to mitigate the weekly cyclical variance in volume.
Data was presented as mean with 95% confidence interval (CI). Statistical analysis was performed using Prism (GraphPad, San Diego, CA) and RStudio (RStudio, Boston, MA).
Results
Trend in imaging volume in relationship to state of emergency declaration in Massachusetts
After state of emergency was declared in Massachusetts, our hospital and its affiliated imaging centers responded on March 11th, 2020 by postponing nonessential imaging studies and deferring nonessential in-person activities. This resulted in a drastic decrease in imaging volume from a total of 189,166 imaging studies performed between weeks 1 and 9 to 69,900 imaging studies performed between weeks 12 and 19 (Table 1 ). The average weekly imaging volume decreased by 58% from weeks 1–9 (21,018 studies) to weeks 12–19 (8737 studies; Table 2 ; p < 0.001). Specifically, the weekly average at the main hospital campus declined from 10,855 studies (weeks 1–9; 100%, baseline) to 5028 studies (weeks 12–19; 46% of baseline; p < 0.001), with the lowest weekly volume reaching 4460 studies (41% of baseline; week 15) (Table 2). In comparison, the weekly average at the affiliated imaging centers dropped from 10,163 (weeks 1–9; 100%, baseline) to 3709 (weeks 12–19; 36% of baseline; p < 0.001), with the lowest weekly volume reaching 3024 studies (30% of baseline; week 13) (Table 2).
Table 1.
Study Volume by Image Modality Type at Main Hospital Campus and Affiliated Imaging Centers During Weeks 1–9 (Pre-SOE Period) and Weeks 12–19 (Post-SOE Period)
| Weeks 1–9 |
Weeks 12–19 |
% Decrease: Pre-SOE Vs Post-SOE |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Main | Affiliated | Total | Main | Affiliated | Total | Main | Affiliated | Total | |
| Total Volume | 97,698 | 91,468 | 189,166 | 40,226 | 29,674 | 69,900 | 58.8% | 67.6% | 63.0% |
| Image modality | |||||||||
| Radiography | 47,728 | 33,861 | 81,589 | 21,515 | 11,800 | 33,315 | 54.9% | 65.2% | 59.2% |
| CT | 18,423 | 14,587 | 33,010 | 9,668 | 7,366 | 17,034 | 47.5% | 49.5% | 48.4% |
| Ultrasound | 10,781 | 16,344 | 27,125 | 4,528 | 5,844 | 10,372 | 58.0% | 64.2% | 61.8% |
| Mammography | 7,334 | 13,243 | 20,577 | 549 | 943 | 1,492 | 92.5% | 92.9% | 92.7% |
| MRI | 7,746 | 9,480 | 17,226 | 2,781 | 2,818 | 5,599 | 64.1% | 70.3% | 67.5% |
| Nuclear medicine | 5,686 | 3,953 | 9,639 | 1,185 | 903 | 2,088 | 79.2% | 77.2% | 78.3% |
Table 2.
Mean Study Volumes in Weeks 1–9 (Pre-SOE Period) and Weeks 12–19 (Post-SOE Period) and Lowest Weekly Volume Through Weeks 12–19 at the Main Hospital Campus and the Affiliated Imaging Centers
| Weeks 1–9 |
Weeks 12–19 |
Weeks 12–19 |
Pre-SOE Vs Post-SOE |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Main |
Affiliated |
Main |
Affiliated |
Main | Affiliated | Main | Affiliated | |||||
| Mean (% of Baseline) | 95% CI* | Mean (% of Baseline) | 95% CI | Mean (% of Baseline) | 95% CI | Mean (% of Baseline) | 95% CI | Lowest Weekly Volume (% of Baseline) | p Value | |||
| Total volume | 10,855 (100%) | 10,472–11,239 | 10,163 (100%) | 9778–10,549 | 5028 (46%) | 4551–5506 | 3709 (36%) | 3294–4125 | 4460 (Week 15) (41%) | 3024 (Week 13) (30%) | < 0.001 | < 0.001 |
| Image modality | ||||||||||||
| Radiography | 5303 (100%) | 5069–5537 | 3762 (100%) | 3603–3922 | 2689 (51%) | 2551–2828 | 1475 (39%) | 1289–1661 | 2529 (Week 12) (48%) | 1050 (Week 12) (28%) | < 0.001 | < 0.001 |
| CT | 2047 (100%) | 1994–2100 | 1621 (100%) | 1570–1672 | 1209 (59%) | 1044–1373 | 921 (57%) | 808–1034 | 931 (Week 13) (45%) | 763 (Week 13) (47%) | < 0.001 | < 0.001 |
| Ultrasound | 1198 (100%) | 1148–1248 | 1816 (100%) | 1742–1891 | 566 (47%) | 497–635 | 731 (40%) | 652–809 | 459 (Week 15) (38%) | 626 (Week 15) (34%) | < 0.001 | < 0.001 |
| Mammography | 815 (100%) | 764–866 | 1471 (100%) | 1390–1553 | 69 (8%) | 51–86 | 118 (8%) | 74–162 | 38 (Week 15) (5%) | 58 (Week 15) (4%) | < 0.001 | < 0.001 |
| MRI | 861 (100%) | 834–887 | 1053 (100%) | 1032–1075 | 348 (40%) | 269–426 | 352 (33%) | 293–411 | 231 (Week 14) (27%) | 276 (week 13) (26%) | < 0.001 | < 0.001 |
| Nuclear Medicine | 632 (100%) | 599–665 | 439 (100%) | 417–462 | 148 (23%) | 125–171 | 113 (26%) | 103–123 | 112 (Week 16) (18%) | 90 (Week 18) (20%) | < 0.001 | < 0.001 |
*CI, confidence interval. Average weekly imaging volume of weeks 1–9 was considered the volume baseline.Cl, column title.
Trend in imaging volume in relationship to daily new COVID-19 cases in Massachusetts
The daily new number of COVID-19 cases in Massachusetts increased throughout March and peaked on April 17, 2020 with a reported 3005 new cases (Fig 1A, blue line). This was subsequently followed by a steady decline in the daily new COVID-19 cases in the month of May. The trend in daily new COVID-19 positive cases across our hospital system was similar, reaching a peak of 221 positive new cases on April 14, 2020, followed by a steady gradual decline. The overall imaging volume within our hospital system slowly increased (slope = 22.6 studies per day) as the daily new COVID-19 cases in Massachusetts began to decline from April 18th, 2020 onward (slope −43.1 studies per day). Total imaging volume continued to increase throughout May as healthcare institutions in Massachusetts resumed a subset of nonemergency procedures and deferred elective cases starting on May 18th, 2020 (19). By May 21, the total daily imaging volume was 68% of pre-SOE daily average imaging volume (Fig 2 ).
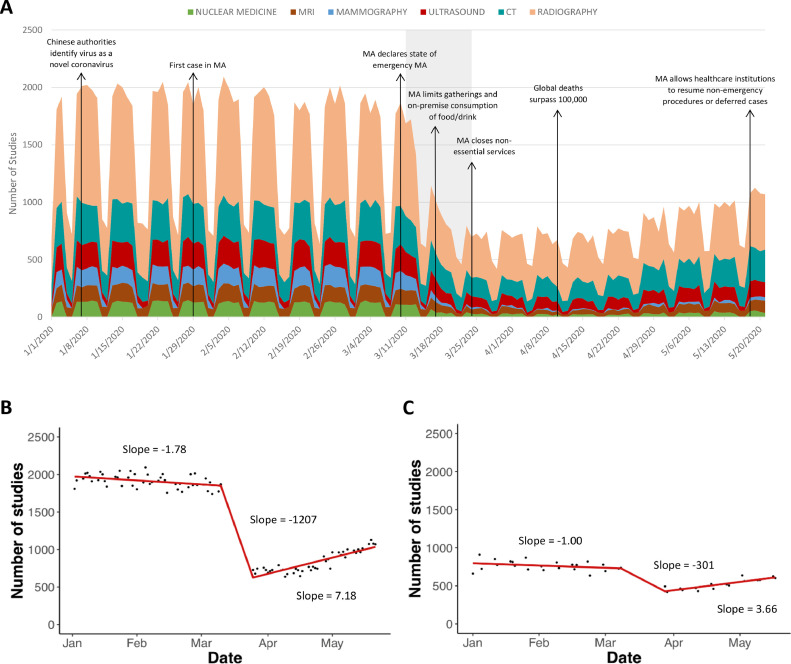
Fig. 2.
Daily volume at the main hospital. (a) Daily imaging volume by modality type at the main hospital campus from January 2020 to May 2020. Gray zone marks the significant decline in daily imaging volume during the transition period, the time between the pre-SOE and post-SOE periods. (b) Trend of the total study volume at the main hospital campus during the pre-SOE, transition, and post-SOE during weekdays. (c) Trend of the total study volume at the main hospital campus during the pre-SOE, transition, and post-SOE during weekends.
Comparison of imaging volume between the main hospital campus and affiliated imaging centers during the COVID-19 pandemic
The trends in daily imaging volume at the main hospital campus and affiliated imaging centers were similar, both demonstrating a sharp decline after March 10th, 2020 when Massachusetts Governor Baker declared a state of emergency (Fig 3 ). During the pre-SOE period, there was a slight gradual decrease in imaging volume at both the main hospital campus (slope = −1.78 for weekdays; slope = −1.00 for weekends) and at the affiliated imaging centers (slope = −2.07 for weekdays; slope = −0.58 for weekends). During the transition period, there was greater volume drop at the affiliated imaging centers (slope = −1270 for weekdays; slope = −399 for weekends) than at the main hospital campus (slope = −1207 for weekdays; slope = −301 for weekends). Following the transition period, imaging volume increased at a greater rate at the main hospital campus (slope = 7.18 for weekdays; slope = 3.66 for weekends) than at affiliated imaging centers ((slope = 6.95 for weekdays; slope = 2.72 for weekends) (Fig 3).
Fig. 3.
Daily volume at the affiliated outpatient imaging centers. (a) Daily imaging volume by modality type at the affiliated imaging centers from January 2020 to May 2020. Gray zone marks the significant decline in daily imaging volume during the transition period, the time between the pre-SOE and post-SOE periods. (b) Trend of the total study volume at the affiliated imaging centers during the pre-SOE, transition, and post-SOE during weekdays. (c) Trend of the total study volume at the affiliated imaging centers during the pre-SOE, transition, and post-SOE during weekends.
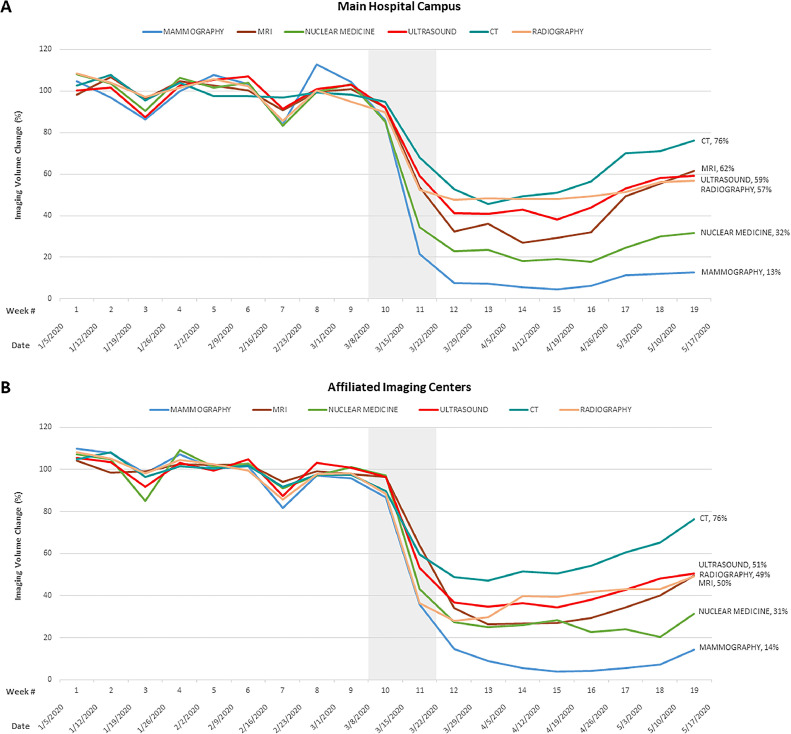
Comparison of imaging volume across modalities
There was a decline in volume for all imaging modalities from weeks 1–9 to weeks 12–19. CT, radiography, and ultrasound exhibited the lowest decrease in volume, with a weekly volume decrease of 41%, 49%, and 53%, respectively, at the main hospital campus, and 43%, 61%, and 60%, respectively, at the affiliated imaging centers (Table 2; Fig 4 ). Mammography exhibited the greatest average weekly volume decrease of 92% at both the main hospital campus and the affiliated imaging centers (Table 2). Nuclear medicine studies exhibited the second largest volume decrease of 77% at the main hospital campus and 74% at affiliated imaging centers. Of note, aside from mammography and nuclear medicine studies, all other imaging modalities exhibited greater volume decrease at the affiliated imaging centers than at the main hospital campus (Table 2). By week 19, CT imaging recovered to 76% of baseline volume at both the main hospital campus and the affiliated imaging centers (Fig 4). Mammography volume remained low at both the main hospital campus (13% of baseline volume) and the affiliated imaging centers (14% of baseline volume; Fig 4) at week 19.
Fig. 4.
Percent change of weekly imaging volume by modality type at (a) main hospital campus and (b) affiliated imaging centers, from January 2020 through May 2020. Gray zone marks the significant decline in weekly imaging volume during the transition period, the time between the pre-SOE and post-SOE periods. Average weekly imaging volume of weeks 1–9 (pre-SOE period) was used as reference and considered 100%. The percentage listed beside each imaging modality represent the percent of baseline volume recovery at week 19.
Discussion
The COVID-19 pandemic has had sweeping effects on the US healthcare system (8,9). In our study, we observed a close temporal relationship between imaging volume trend and recovery and important public health announcements. Furthermore, we noticed that imaging volume decreased to a greater extent at nonhospital-based affiliated imaging centers along with a slower rate of volume recovery, and that mammography and nuclear medicine volume exhibited the greatest volume decrease during the COVID-19 pandemic.
The response to the COVID-19 pandemic has been led by national public health authorities in coordination with local government and hospitals. Imaging volume at our institution began decreasing sharply starting on March 11th, following a state of emergency being declared in Massachusetts. Similarly, previous studies have shown that imaging volume decreased elsewhere in the country as well, including at institutions in the state of New York and in Santa Clara County, California, all within a week of the observed decrease at our institution (11,14). It was during this time that the WHO declared the COVID-19 outbreak a pandemic; together with subsequent CDC and American College of Radiology recommendations, this led to changes in not only our hospital system policies, but all health care systems across the United States to delay nonessential imaging studies as part of the widespread effort to slow the rate of new infections (10,16,17,20). The change in our hospital's and referring providers imaging orders, decision to suspend screening programs and nonurgent elective procedures, and patients’ decisions to delay imaging, resulted in a 58% drop in weekly volume, which is comparable to the 20% to 60% decrease reported at other institutions (9,11,20,21). As daily new cases of COVID-19 began to decrease by April 17th, 2020, and as Massachusetts began easing restrictions in May, we observed a steady recovery of volume; by May 21st, the daily imaging volume recovered to 68% of pre-SOE daily volume averages—70% at the main hospital campus, and 66% at affiliated imaging centers (19). Our results demonstrate the close relationship between local hospital policy changes and imaging volume fluctuations with national and state public health announcements. As the pandemic moves forward, there is further need for close coordination of efforts from governmental agencies and local healthcare systems to ensure a safe and effective recovery, especially for locations with rising COVID-19 cases.
Hospital-owned or affiliated imaging centers generate a substantial amount of revenue and capture a large proportion of the outpatient radiology volume (22,23). The success of nonhospital based imaging centers may be partly due to the ability to provide expedited and more convenient outpatient access (22). During the current pandemic, our affiliated imaging centers showed a greater decrease in average weekly imaging volume (64%) compared to the main hospital campus (54%). This is not unexpected, as hospital-based facilities perform both emergent, inpatient and outpatient studies, whereas affiliated imaging centers perform mostly outpatient and low acuity urgent care studies. Patients with specialized needs or emergent needs, including the rising number of symptomatic patients with COVID-19, still may require hospital-based care during this pandemic and likely partly account for the lower decrease in volume at the main hospital campus. Similar to Los Angeles County + USC Medical Center's approach, we did not make an attempt to reduce inpatient and emergency department imaging, but prioritization of exams was emphasized (20). This is also consistent with previous research demonstrating that inpatient volumes were not affected to the same extent as outpatient studies (11).
Interestingly, we noticed that not only was the extent of imaging volume decrease greater at affiliated imaging centers than at the main hospital campus, the rate of volume recovery was also slower at the affiliated imaging centers. Possible explanations for this observation include patients and referring providers postponing elective imaging appointments due to ongoing concerns about the pandemic, referring providers delaying scheduling of elective outpatient studies, or slower reopening of affiliated imaging centers compared to large urban hospitals per state mandate. In addition, high acuity visits to the main hospital campus may have increased due to postponement of medical care or delayed presentation of patients with subacute or chronic symptoms; for example, several reports have raised concerns of patients delaying stroke and heart failure treatment amid COVID-19 concerns which may have resulted in high clinical severity at time of presentation (24, 25, 26, 27). With the affiliated imaging centers contributing substantially to revenue, there are significant economic ramifications on health care systems and radiology groups from loss of imaging volume at these locations, including possible delay of expansion plans, delay of equipment maintenance and upgrade, hiring delays, staff furloughs, and even staff layoffs. Our hospital system implemented temporary pay and benefit reductions, as well as wage freezes to offset the financial loss (28). The best method to address the financial impact, however, will vary across different radiology practices, depending on size, location, operational budget, staffing needs, and financial reserve. Short-term and long-term changes, therefore, need to be carefully implemented to weather the current economic climate.
Various modalities were differentially affected during the COVID-19 pandemic. Previous studies in New York and Santa Clara demonstrated that mammography and nuclear medicine exhibited the greatest degree of volume reduction (11,14). Similarly, mammography and nuclear medicine also exhibited the greatest level of decrease in our study. Screening exams make up a substantial portion of mammography studies and other imaging studies including lung cancer screening and CT colonography, which were suspended by hospital and radiology policies in compliance with local and national policies. The impact, both in terms of patient care and healthcare costs, will require further research. The relatively attenuated CT and radiography volume reduction, both at the main hospital campus and at affiliated imaging centers, is not unexpected given COVID-19 is often primarily a pulmonary disease, for which chest radiograph or CT may be indicated per the American College of Radiology Appropriateness criteria (29). Furthermore, the relatively smaller decrease in ultrasound studies may be related to the increasing knowledge of coagulopathy in patients with COVID-19 (30, 31, 32, 33). Consideration should be taken for temporary reallocation of resources and personnel, including radiologists and technologists, from mammography and nuclear medicine to other busier radiology divisions.
There are several limitations to our study. The first is the retrospective nature of the study. The second is that our aggregated data lacks the information to allow breakdown of studies by body part and study indication, thus limiting detailed analysis of how different radiology subspecialties and disease sites are impacted by the COVID-19 pandemic. Furthermore, we did not subdivide imaging studies based on status of the patient as the composition was different at the main hospital campus, which comprised of inpatient, outpatient, and emergency room studies, whereas the affiliated imaging centers comprised mainly of outpatient studies. However, the goal of our study was to compare all-patient imaging volume at the main hospital campus to that of the affiliated imaging centers. Revenue data was also not available through our hospital enterprise medical imaging data warehouse. Finally, our hospital system is a large quaternary care academic center located in a state with relatively high COVID-19 cases, which may potentially limit the generalizability of our results.
In conclusion, imaging volume at our large quaternary care academic medical center was closely associated with public health announcements at the local, state, national, and international level, and was inversely associated with daily new COVID-19 cases in the state of Massachusetts. Nonhospital-based affiliated imaging centers showed a greater decrease in overall imaging volume and demonstrated a slower rate of volume recovery than the main academic hospital. Outpatient-centric imaging modalities such as mammography and nuclear medicine exhibited the greatest extent of volume decrease during the COVID-19 pandemic. Future studies should incorporate the various imaging data published across different healthcare systems. Generalizable prediction and economic recovery models may help institutions prepare for potential future pandemics by informing budgeting decisions and resource allocation.
Conflicts of interest
Dr. Little is a textbook author and editor for Elsevier and receives royalties for his prior work. Dr. Succi reports personal fees and nonfinancial support from 2 Minute Medicine, Inc., and royalties from Frequency Therapeutics for work not related to this manuscript. Dr. Flores reports grant funding from the American College of Radiology Innovation Fund and the National Cancer Institute Research Diversity Supplement for work not related to this manuscript.
Financial and Grant Support
None.
References
- 1.Pneumonia of unknown cause – China. World Health Organization. Accessed June 1, 2020, Available at: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/.)
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVID-19 CORONAVIRUS PANDEMIC. Worldmeter. (Accessed June 1, 2020. Available at: https://www.worldometers.info/coronavirus/)
- 4.Jr. DGM . The New York Times; 2020. The U.S. now leads the world in confirmed coronavirus cases. 2020 March 26. [Google Scholar]
- 5.Centers for Disease Control and Prevention; 2020. United States coronavirus (COVID-19) death toll surpasses 100,000.https://www.cdc.gov/media/releases/2020/s0528-coronavirus-death-toll.html Accessed June 1, 2020, Available at: [Google Scholar]
- 6.COVID-19 State of Emergency. 2020. Accessed June 14, 2020, Available at: https://www.mass.gov/info-details/covid-19-state-of-emergency.)
- 7.Sharma P, Leung TY, Kingshott RPJ. Managing uncertainty during a global pandemic: an international business perspective. J Bus Res. 2020;116:188–192. doi: 10.1016/j.jbusres.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khullar D, Bond AM, Schpero WL. COVID-19 and the Financial Health of US Hospitals. JAMA. 2020;21:2127–2128. doi: 10.1001/jama.2020.6269. [DOI] [PubMed] [Google Scholar]
- 9.Cavallo JJ, Forman HP. The economic impact of the COVID-19 pandemic on radiology practices. Radiology. 2020;296:E141–E144. doi: 10.1148/radiol.2020201495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ACRCOVID-19 clinical resources for radiologists. Available at: https://www.acr.org/Clinical-Resources/COVID-19-Radiology-Resources.)
- 11.Naidich JJ, Boltyenkov A, Wang JJ. Impact of the COVID-19 pandemic on imaging case volumes. J Am Coll Radiol. 2020;17:865–872. doi: 10.1016/j.jacr.2020.05.004. Accessed May 31, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parikh KD, Ramaiya NH, Kikano EG. COVID-19 pandemic impact on decreased imaging utilization: a single institutional experience. Acad Radiol. 2020 doi: 10.1016/j.acra.2020.06.024. S1076-6332(20)30399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.COVID-19 Impact on CT Imaging VoluME. 2020. (Accessed May 31, 2020, Available at: https://www.aidoc.com/blog/ct-imaging-volumes-covid19/.)
- 14.Madhuripan N, Cheung HM, Cheong LHA. Variables influencing radiology volume recovery during the next phase of the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Radiol. 2020;17:855–864. doi: 10.1016/j.jacr.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.A comprehensive timeline of the new coronavirus pandemic, from China's first case to the present. Business Insider, 2020. (Accessed June 2, 2020, Available at: https://www.businessinsider.com/coronavirus-pandemic-timeline-history-major-events-2020-3#december-31-2019-chinese-health-officials-informed-the-world-health-organization-about-a-cluster-of-41-patients-with-a-mysterious-pneumonia-most-were-connected-to-the-huanan-seafood-wholesale-market-a-wet-market-in-the-city-of-wuhan-1.)
- 16.Coronavirus (COVID-19). 2020. (Accessed June 3, 2020, Available at:https://www.cdc.gov/coronavirus/2019-ncov/index.html.)
- 17.Coronavirus disease (COVID-19) pandemic. 2020. (Accessed June 3, 2020, Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019.)
- 18.CORONAVIRUS DISEASE (COVID-19) IN BOSTON. 2020. (Accessed June 2, 2020, Available at:https://www.boston.gov/news/coronavirus-disease-covid-19-boston.)
- 19.Reopening Health and Human Services in Massachusetts Phase 1. Mass.gov, 2020. (Accessed June 3, 2020, Available at:https://www.mass.gov/lists/reopening-health-and-human-services-in-massachusetts-phase-1.)
- 20.Shin H, Abdelhalim A, Chau S. Responding to coronavirus disease 2019: LA County hospital experience. Emerg Radiol. 2020 doi: 10.1007/s10140-020-01818-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips CD, Shatzkes DR, Moonis G. From the eye of the storm: multi-institutional practical perspectives on neuroradiology from the COVID-19 outbreak in New York City. AJNR Am J Neuroradiol. 2020;41:960–965. doi: 10.3174/ajnr.A6565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boland GW. Diagnostic imaging centers for hospitals: a different business proposition for outpatient radiology. J Am Coll Radiol. 2007;4:581–583. doi: 10.1016/j.jacr.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 23.Shields J. Outpatient imaging center ventures: a third-party, for-profit perspective. J Am Coll Radiol. 2004;1:876–881. doi: 10.1016/j.jacr.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 24.Schirmer CM, Ringer AJ, Arthur AS. Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J Neurointerv Surg. 2020;12:639–642. doi: 10.1136/neurintsurg-2020-016299. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg RJ, Goldberg JH, Pruell S. Delays in seeking medical care in hospitalized patients with decompensated heart failure. Am J Med. 2008;121:212–218. doi: 10.1016/j.amjmed.2007.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oxley TJ, Mocco J, Majidi S. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Romero J, Valencia S, Guerrero A. Acute appendicitis during coronavirus disease 2019 (COVID-19): changes in clinical presentation and CT findings. J Am Coll Radiol. 2020;17:1011–1013. doi: 10.1016/j.jacr.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mass General Brigham Imposes Pay Cuts, Freezes wages and benefits as pandemic losses mount. 2020. (Accessed July 31, 2020, Available at:https://www.wbur.org/commonhealth/2020/06/17/mass-general-brigham-salary-cuts-furloughs.)
- 29.ACRAppropriateness Criteria®. (Accessed June 13, 2020, Available at:https://acsearch.acr.org/list.)
- 30.Levi M, Thachil J, Iba T. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438–ee40. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang N, Li D, Wang X. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klok FA, Kruip M, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ackermann M, Verleden SE, Kuehnel M. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]