Abstract
Background
Repeated assessment of cardiorespiratory fitness (CRF) improves mortality risk predictions in apparently healthy adults. Accordingly, the American Heart Association suggests routine clinical assessment of CRF using, at a minimum, nonexercise prediction equations. However, the accuracy of nonexercise prediction equations over time is unknown. Therefore, we compared the ability of nonexercise prediction equations to detect changes in directly measured CRF.
Methods and Results
The sample included 987 apparently healthy adults from the BALL ST (Ball State Adult Fitness Longitudinal Lifestyle Study) cohort (33% women; average age, 43.1±10.4 years) who completed 2 cardiopulmonary exercise tests ≥3 months apart (3.2±5.4 years of follow‐up). The change in estimated CRF (eCRF) from 27 distinct nonexercise prediction equations was compared with the change in directly measured CRF. Analysis included Pearson product moment correlations, SEE values, intraclass correlation coefficient values, Cohen's κ coefficients, γ coefficients, and the Benjamini‐Hochberg procedure to compare eCRF with directly measured CRF. The change in eCRF from 26 of 27 equations was significantly associated to the change in directly measured CRF (P<0.001), with intraclass correlation coefficient values ranging from 0.06 to 0.63. For 16 of the 27 equations, the change in eCRF was significantly different from the change in directly measured CRF. The median percentage of participants correctly classified as having increased, decreased, or no change in CRF was 56% (range, 39%–61%).
Conclusions
Variability was observed in the accuracy between nonexercise prediction equations and the ability of equations to detect changes in CRF. Considering the appreciable error that prediction equations had with detecting even directional changes in CRF, these results suggest eCRF may have limited clinical utility.
Keywords: cardiopulmonary exercise test, exercise test, fitness algorithm, maximum oxygen consumption, prognosis
Subject Categories: Risk Factors, Cardiovascular Disease, Exercise, Lifestyle, Statements and Guidelines
Nonstandard Abbreviations and Acronyms
- BALL ST
Ball State Adult Fitness Longitudinal Lifestyle Study
- CRF
cardiorespiratory fitness
- eCRF
estimated cardiorespiratory fitness
- ICC
intraclass correlation coefficient
- VO2max
maximal oxygen consumption
Clinical Perspective
What Is New?
We examined the accuracy of cardiorespiratory fitness (CRF) derived from 27 previously published nonexercise prediction equations for measuring longitudinal changes of CRF in a cohort of apparently healthy adults.
Although there was general agreement between CRF from the prediction equations and the gold standard cardiopulmonary exercise test, the prediction equations had a low degree of accuracy even when identifying the directional changes to CRF.
What Are the Clinical Implications?
As the importance of assessing CRF in routine clinical practice continues to be further established, it is important to note there is significant error associated with using nonexercise prediction equations to estimate CRF acutely or when assessing longitudinal changes to CRF.
These data suggest a limited prognostic utility of estimating CRF within a clinical setting.
Within apparently healthy adults, a single baseline measure of cardiorespiratory fitness (CRF) is inversely associated with mortality risk and incidence of many chronic diseases.1, 2, 3, 4 In addition, CRF is a stronger predictor of mortality compared with many other traditional risk factors.5 Accordingly, a Scientific Statement from the American Heart Association suggests CRF be considered a clinical vital sign that is regularly assessed alongside other established risk factors.4 Although the gold standard for measuring CRF is the cardiopulmonary exercise test, a vast majority of apparently healthy adults have never performed this test, making CRF the only major risk factor that is not regularly assessed in the primary care setting. To encourage the practice of CRF assessment in apparently healthy adults, it is recommended that all routine clinical visits should minimally include the determination of estimated CRF (eCRF) using a nonexercise prediction equation.4
Nonexercise prediction equations are based on the relationship between CRF and various characteristics, such as age and sex. In the research setting, epidemiologists have often used prediction equations to examine the relationship between CRF and health outcomes. This research has shown eCRF is inversely associated with all‐cause mortality6, 7, 8, 9, 10 and provided much of the impetus behind the recommendations for clinicians to minimally determine a patient's eCRF. Nonexercise prediction equations, however, have several inherent limitations. For example, prediction equations do not account for the well‐known genetic influence on CRF11 and social desirability biases can influence the self‐report aspects of some equations (eg, physical activity levels12). The resulting prediction error associated with equations is a significant limitation as a recent research study from our cohort found prediction equations were unable to accurately classify an individual's CRF level, thus reducing their potential clinical utility.13 Nonetheless, determining eCRF is recommended because of the ease of calculation and its previously demonstrated relationship with mortality.4
Although a single measure of CRF has merit, identifying changes over time allows for improved mortality risk determination. A convincing body of evidence indicates individuals who improve or maintain CRF long‐term have a reduced risk for early mortality.14, 15, 16, 17, 18, 19 Therefore, monitoring longitudinal changes to CRF is clinically relevant and is an important element within the recommendations to minimally include eCRF as a clinical vital sign. However, most nonexercise prediction equations were developed using cross‐sectional data, which could influence their ability to accurately assess longitudinal changes to CRF. One set of equations was developed using longitudinal data,20 although the accuracy of these equations over time has yet to be tested on a different cohort. Considering there is no universally accepted equation for assessing eCRF, the aim of the present study was to evaluate the ability of 27 different nonexercise CRF prediction equations to accurately detect changes in directly measured CRF using data from a single cohort of apparently healthy adults. We hypothesized that changes to eCRF would be correlated to directly measured CRF changes, yet misclassification would occur at the individual level.
Methods
Data from the BALL ST (Ball State Adult Fitness Longitudinal Lifestyle Study) cohort were used for this study. The sample included data from apparently healthy adults, aged 18 to 80 years old, who performed 2 comprehensive health and fitness assessments at least 3 months apart between April 1, 1968, and July 31, 2019. BALL ST participants were either self‐referred to a community‐based exercise program or were research participants in studies who provided written informed consent for their data to be used for research. Participants were defined as apparently healthy if they were free from known cardiovascular disease (eg, history of cardiac arrest, coronary artery disease, heart failure, myocardial infarction, stroke, and peripheral artery disease) and lung disease (eg, chronic obstructive pulmonary disease and emphysema). Participants were excluded if they were taking a β‐blocker medication or missing data for height or weight (a flowchart of inclusion/exclusion criteria is provided in Figure 1). The protocol for this study was reviewed by the Ball State University Institutional Review Board and determined to be exempt as only deidentified data were used. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Figure 1. Flowchart of inclusion/exclusion criteria for the study sample.
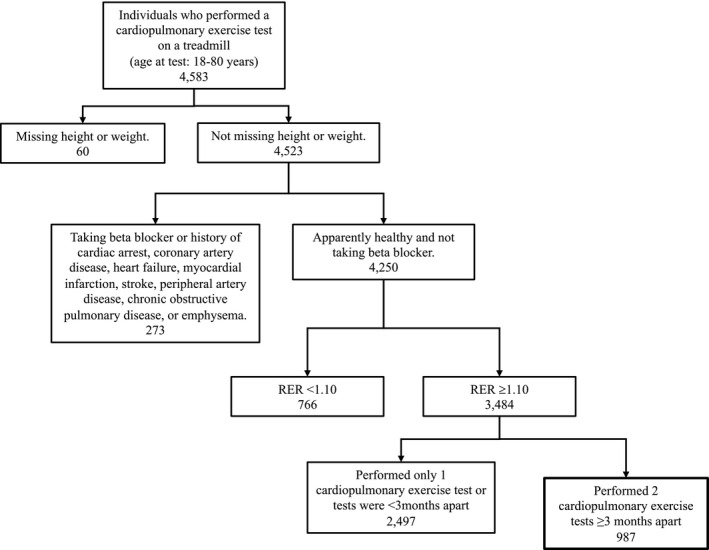
RER indicates respiratory exchange ratio.
Nonexercise Prediction Equations
A literature search was conducted using the PubMed electronic database and the following terms: “predicted VO2max,” “predicted VO2peak,” “estimated VO2max,” “estimated VO2peak,” “non‐exercise testing,” and “non‐exercise prediction” (to June 14, 2019). Additional equations were identified from within previous reviews,4, 21, 22, 23 and citations of these previous reviews were searched using Google Scholar. A total of 27 nonexercise prediction equations were included on the basis of the following criteria: (1) the equation predicted maximal oxygen consumption (VO2max) in both men and women; (2) walking or running was the exercise mode used to create the equation; (3) the equation was created from an apparently healthy adult cohort; (4) variables within the equation were available from the data collected on the BALL ST cohort (eg, excluded equations requiring variables such as thigh mass and perceived functional ability); and (5) a sample size of 100 could be produced from data within the BALL ST cohort.
The equations are provided in Table 1.20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 Although most equations estimated relative VO2max (mL·kg−1·min−1), 7 equations estimated maximal metabolic equivalents.20, 34 Estimated metabolic equivalents derived from these equations were multiplied by 3.5 to determine relative VO2max. 38 Variables within the equations included: sex, age, height, weight, body mass index, waist circumference, percentage body fat, smoking, resting heart rate, physical activity, dyslipidemia, hypertension, and diabetes mellitus (Table 2).20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 Trained technicians measured anthropometrics (height, weight, body mass index, and waist circumference) and determined percentage body fat using skin folds.39 Participants completed a health history questionnaire, which provided self‐reported smoking status, physical activity status, medication use, and medical history. Smoking status was recorded both on a 2‐level scale (“yes”/”no”) and an 8‐level scale that captured smoking habits.32 Self‐reported physical activity data were collected using the BALL ST scale, which captures both lifestyle and occupational physical activity.32 For the prediction equations that included measures of self‐reported physical activity, various questionnaires and scales were used (Table 1). For the equations that did not use the BALL ST scale, physical activity measures were converted from the BALL ST scale to the other scales (Table 3).20, 32, 40, 41 When a participant was missing data needed within a prediction equation, no eCRF was calculated for that participant for that equation.
Table 1.
Summary of Nonexercise CRF Prediction Equations for Estimating Relative VO2max (mL·kg−1·min−1)
| Authors | Equation | Reported R 2 | Reported SEE |
|---|---|---|---|
| No PA measure | |||
| Riddle et al 198024 †† | Men: (60−0.55 (age))·((4.13 (height [cm])/(2.54−135))/2.2 | ||
| Women: (48−0.37 (age))·((3.55 (height [cm])/(2.54−106))/2.2 | |||
| Wasserman et al 199425 | Men: PW=0.79 (height [cm])−60.7If PW=measured weight: [(50.72−0.372 (age))·(weight [kg])]·1.11If PW>measured weight: [(PW+(weight [kg])/2) (50.72−0.372 (age))]·1.11If PW<measured weight: [(50.72−0.372 (age)) (weight [kg])+6 ((weight [kg])−PW)] 1.11 | ||
| Women: PW=0.65 (height [cm])−42.8If PW=measured weight: [((weight [kg])+43)(22.78−0.17 (age)] 1.11If PW>measured weight: [((PW+(weight[kg])+86)/2)(22.78 −0.17 (age)] 1.11If PW<measured weight: [(PW+43)(22.78−0.17 (age))+6 (weight [kg])−PW)] 1.11 | |||
| Jang et al 2012 (model 1)26 | 50.543−0.069 (age)+13.525 (sex; men=1, women=0)−0.403 (BMI)−1.530 (CSS**) | 0.67 | 4.21 |
| Baynard et al 2016 (BMI)27 | 77.96−10.35 (sex; men=0, women=1)−0.92 (BMI)−0.32 (age) | 0.57 | 6.89 |
| Baynard et al 2016 (WC)27 | 88.35−14.79 (sex; men=0, women=1)−0.40 (WC)−0.27 (age) | 0.60 | 6.70 |
| Myers et al 201728 | 79.9−0.39 (age)−13.7 (sex; men=0, women=1)−0.127 (weight [lbs]) | 0.62 | 7.20 |
| de Souza et al 201829 | 45.2−0.35 (age)−10.9 (sex; men=1, women=2)−0.15 (weight [lbs])+0.68 (height [in])−0.46 | 0.62 | 6.60 |
| Includes measure of PA | |||
| Jackson et al 1990 (BMI)30 | 56.363+1.921 (PA*)−0.381 (age)−0.754 (BMI)+10.987 (sex; men=1, women=0) | 0.61 | 5.70 |
| Jackson et al 1990 (%fat)30 | 50.513+1.589 (PA*)−0.289 (age)−0.552 (%fat)+5.863 (sex; men=1, women=0) | 0.66 | 5.35 |
| Heil et al 199531 | 36.580−0.541 (%fat)+1.921 (PA*)+0.558 (age)−7.81E‐3 (age2)+3.706 (sex; men=1, women=0) | 0.74 | 4.90 |
| Whaley et al 1995 (BMI)32 | 64.62−0.339 (age)+9.006 (sex; men=1, women=0)+2.069 (PA†)−0.601 (BMI)−0.143 (RHR)−0.409 (CSS#) | 0.70 | 5.60 |
| Whaley et al 1995 (%fat)32 | 61.66−0.328 (age)+5.45 (sex; men=1, women=0)+1.832 (PA†)−0.436 (% fat)−0.143 (RHR)−0.446 (CSS#) | 0.73 | 5.38 |
| Matthews et al 199933 | 34.142+0.133 (age)−0.005 (age2)+11.403 (sex; men=1, women=0)+1.463 (PA*)+9.170 (height [m])−0.254 (weight [kg]) | 0.74 | 5.64 |
| Jurca et al 2005 (ACLS)34 ‡‡ | 18.81+2.49 (sex; men=1, women=0)−0.08 (age)−0.17 (BMI)−0.05 (RHR)+0.81 (PA1‡)+1.17 (PA2‡)+2.16 (PA3‡)+3.05 (PA4‡) | 0.60 | 5.25 |
| Jurca et al 2005 (ADNFS)34 ‡‡ | 21.41+2.78 (sex; men=1, women=0)−0.11 (age)−0.17 (BMI)−0.05 (RHR)+0.35 (PA1‡)+0.29 (PA2‡)+0.64 (PA3‡)+1.21 (PA4‡) | 0.58 | 6.90 |
| Jurca et al 2005 (NASA)34 ‡‡ | 18.07+2.77 (sex; men=1, women=0)−0.10 (age)−0.1 BMI)−0.03 (RHR)+0.32 (PA1‡)+1.06 (PA2‡)+1.76 (PA3‡)+3.03 (PA4‡) | 0.65 | 5.08 |
| Wier et al 2006 (BMI)35 | 57.402−0.372 (age)+8.596 (sex; men=1, women=0)+1.396 (PA§)−0.683 (BMI) | 0.62 | 4.95 |
| Wier et al 2006 (%fat)35 | 51.936−0.308 (age)+4.065 (sex; men=1, women=0)+1.217 (PA§)−0.483 (%fat) | 0.65 | 4.91 |
| Wier et al 2006 (WC)35 | 59.416−0.327 (age)+11.488 (sex; men=1, women=0)+1.297 (PA§)−0.266 (WC) | 0.64 | 4.90 |
| Nes et al 201136 | Men: 100.27−0.296 (age)+0.226 (PA¶)−0.369 (WC)−0.155 (RHR) | 0.61 | 5.70 |
| Women: 74.736−0.247 (age)+0.198 (PA¶)−0.259 (WC)−0.114 (RHR) | 0.56 | 5.14 | |
| Cáceres et al 2012 (9 levels)37 | Men: 47.189+0.394 (age)−0.282 (weight [kg])−4.289 (PA$)+0.231 (height [cm])−0.090 (RHR)−2.092 (dyslipidemia)−1.925 (hypertension) −2.901 (CSS**)−2.295 (diabetes mellitus) | 0.53 | 7.15 |
| Women: 37.844+0.250 (age)−0.208 (weight [kg])−3.428 (PA$)+0.139 (height [cm])−0.053 (RHR)−1.327 (dyslipidemia)−1.009 (hypertension)−1.508 (CSS**) | 0.44 | 5.74 | |
| Cáceres et al 2012 (5 levels)37 | Men: 39.390+0.409 (age)−0.307 (weight [kg])−4.437 (PA$)+0.254 (height [cm])−3.081 (CSS**) | 0.51 | 7.31 |
| Women: 31.733+0.244 (age)−0.219 (weight [kg])−3.598 (PA$)+0.151 (height [cm])−1.486 (CSS**) | 0.43 | 5.74 | |
| Jackson et al 2012 (BMI, 5 levels)20, ‡‡ | Men: 20.8013+0.1610 (age)−0.0022 (age2)−0.2240 (BMI)−0.0334 (WC)−0.0375 (RHR)+0.2163 (PA1‡)+0.3447 (PA2‡)+0.7877 (PA3‡)+1.1961 (PA4‡)−0.4306 (CSS**) | 5.81 | |
| Women: 14.5493+0.1136 (age)−0.0016 (age2)−0.1500 (BMI)−0.0088 (WC)−0.0359 (RHR)+0.2091 (PA1‡)+0.2275 (PA2‡)+0.7021 (PA3‡)+1.0070 (PA4‡)−0.3005 (CSS**) | 5.29 | ||
| Jackson et al 2012 (%fat, 5 levels)20, ‡‡ | Men: 17.7357+0.1620 (age)−0.0021 (age2)−0.1057 (%fat)−0.0422 (WC)−0.0363 (RHR)+0.2153 (PA1‡)+0.3655 (PA2‡)+0.8092 (PA3‡)+1.1989 (PA4‡)−0.4378 (CSS**) | 5.39 | |
| Women: 13.4967+0.1200 (age)−0.0017 (age2)−0.0817 (%fat)−0.0140 (WC)−0.0342 (RHR)+0.2402 (PA‡)+0.2735 (PA2‡)+0.7432 (PA3‡)+1.0346 (PA4‡)−0.3207 (CSS**) | 4.94 | ||
| Jackson et al 2012 (BMI, 2 levels)20, ‡‡ | Men: 21.2870+0.1654 (age)−0.0023 (age2)−0.2318 (BMI)−0.0337 (WC)−0.0390 (RHR)+0.6351 (PA$)−0.4263 (CSS**) | 5.92 | |
| Women: (14.7873+0.1159 (age)−0.0017 (age2)−0.1534 (BMI)−0.0088 (WC)−0.0364 (RHR)+0.5987 (PA$)−0.2994 (CSS**)) | 5.36 | ||
| Jackson et al 2012 (%fat, 2 levels)20, ‡‡ | Men: 18.1395+0.1662 (age)−0.0022 (age2)−0.1077 (%fat)−0.0431 (WC)−0.0380 (RHR)+0.6429 (PA$)−0.4339 (CSS**) | 5.46 | |
| Women: 13.7415+0.1223 (age)−0.0018 (age2)−0.0819 (%fat)−0.0141 (WC)−0.0349 (RHR)+0.6061 (PA$)−0.3188 (CSS**) | 5.01 | ||
| Jang et al 2012 (model 2)26 | 48.392−0.088 (age)+12.335 (sex; men=1, women=0)−0.386 (BMI)−0.621 (CSS**)+0.693 (PA§) | 0.73 | 3.82 |
%Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; CSS, current smoking status; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; PW, predicted weight; RHR, respiratory exchange ratio; VO2max, maximal oxygen consumption; WC, waist circumference (cm).
PA with *NASA Physical Activity Scale, †BALL ST (Ball State Adult Fitness Longitudinal Lifestyle Study) PA scale, ‡Physical Activity Index (5 levels), §NASA Physical Activity Status Scale, ¶Nord‐Trøndelag Health Study (HUNT) questionnaire, or $binary (no=0, yes=1); CSS with #8‐level code or **binary (no=0, yes=1). Dyslipidemia, hypertension, and diabetes mellitus were all coded no=0, yes=1.
Prediction equation calculates absolute VO2max but was converted to relative VO2max for the present study.
Prediction equation calculates metabolic equivalents but was converted to relative VO2max for the present study. In addition, the reported SEE from publication has been multiplied by 3.5 to convert to relative VO2max.
Table 2.
Summary of the Variables Used in the Prediction Equations
| Study | Sex | Age | Height | Weight | BMI | WC | %Fat | Smoking | RHR | PA | Dyslipidemia | Hypertension | Diabetes Mellitus |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Riddle et al 198024 | x | x | x | ||||||||||
| Wasserman et al 199425 | x | x | x | x | |||||||||
| Jang et al 2012 (model 1)26 | x | x | x | x | |||||||||
| Baynard et al 2016 (BMI)27 | x | x | x | ||||||||||
| Baynard et al 2016 (WC)27 | x | x | x | ||||||||||
| Myers et al 201728 | x | x | x | ||||||||||
| de Souza et al 201829 | x | x | x | x | |||||||||
| Jackson et al 1990 (BMI)30 | x | x | x | x | |||||||||
| Jackson et al 1990 (%fat)30 | x | x | x | x | |||||||||
| Heil et al 199531 | x | x | x | x | |||||||||
| Whaley et al 1995 (BMI)32 | x | x | x | x | x | x | |||||||
| Whaley et al 1995 (%fat)32 | x | x | x | x | x | x | |||||||
| Matthews et al 199933 | x | x | x | x | x | ||||||||
| Jurca et al 2005 (ACLS)34 | x | x | x | x | x | ||||||||
| Jurca et al 2005 (ADNFS)34 | x | x | x | x | x | ||||||||
| Jurca et al 2005 (NASA)34 | x | x | x | x | x | ||||||||
| Wier et al 2006 (BMI)35 | x | x | x | x | |||||||||
| Wier et al 2006 (%fat)35 | x | x | x | x | |||||||||
| Wier et al 2006 (WC)35 | x | x | x | x | |||||||||
| Nes et al 201136 | x | x | x | x | x | ||||||||
| Cáceres et al 2012 (9 levels)37 | x | x | x | x | x | x | x | x | x | x | |||
| Cáceres et al 2012 (5 levels)37 | x | x | x | x | x | x | |||||||
| Jackson et al 2012 (BMI, 5‐level PA)20 | x | x | x | x | x | x | x | ||||||
| Jackson et al 2012 (%fat, 5‐level PA)20 | x | x | x | x | x | x | x | ||||||
| Jackson et al 2012 (BMI, 2‐level PA)20 | x | x | x | x | x | x | x | ||||||
| Jackson et al 2012 (%fat, 2‐level PA)20 | x | x | x | x | x | x | x | ||||||
| Jang et al 2012 (model 2)26 | x | x | x | x | x |
%Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; RHR, resting heart rate; and WC, waist circumference.
Table 3.
Summary of the Conversions From the BALL ST Physical Activity Scale to the Other Physical Activity Scales Used in the Prediction Equations
| BALL ST Physical Activity Scale32 | 5‐Level Physical Activity Index20 | 2‐Level Physical Activity Index20 | NASA Physical Activity Scale40 | NASA Physical Activity Status Scale41 | Nord‐Trøndelag Health Study (HUNT) Questionnaire36 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Scale, 1–6) | (Scale, 0–4) | (Scale, 0–1) | (Scale, 0–7) | (Scale, 0–10) | (Scale, 0–45) | ||||||
| Whaley et al 1990 | Jurca et al 2005; Jackson et al 2012 | Jackson et al 2012; Cáceres et al 2012 | Jackson et al 1990; Heil et al 1995; Matthews et al 1999 | Wier et al 2006; Jang et al 2012 | Nes et al 2011 | ||||||
| 1 | Complete lack of exercise | 0 | No regular activity | 0 | Inactive | 0 | Avoid walking | 0 | Avoid walking | 0 | No exercise |
| 2 | Sedentary occupation and moderate recreational activity | 1 | Participated in some other regular physical activity, such as bicycling, swimming, racquet sports, and other strenuous sports, but not walking or jogging | 1.5 | 10–60 min·wk−1 of recreation or work that requires modest physical activity | 1.5 | 10–60 min·wk−1 of recreation or work that requires modest physical activity | 0 | Average of exercising once per week and 2–3 sessions·wk−1, do not break into a sweat, average of 16–30 min·session−1 and 30–60 min·session−1 | ||
| 3 | Moderate occupational and moderate recreational activity | 3 | >60 min·wk−1 of recreation or work that requires modest physical activity | 3 | >60 min·wk−1 of recreation or work that requires modest physical activity | 0 | Exercise 2–3 session·wk−1, do not break into a sweat, >60 min·session−1 | ||||
| 4 | Heavy occupational activity and moderate recreational activity | 2 | Walked or jogged <10 miles·wk−1 | 5 | Run 1–5 miles·wk−1 | 5 | Run 1–5 miles·wk−1 | 6 | Exercise 2–3 session·wk−1, break into a sweat, >60 min·session−1 | ||
| 5 | Participate regularly in an exercise program | 3 | Walked or jogged 10–20 miles·wk−1 | 1 | Active | 6 | Run 5–10 miles·wk−1 | 7.5 | “7” is run 11–15 miles·wk−1, “8” is run up to 20 miles·wk−1 | 18.75 | Average of exercising 2–3 session·wk−1 and every day, break into a sweat, >60 min·session−1 |
| 6 | Highly trained: run ≥20 miles·wk−1 | 4 | Walked or jogged >20 miles·wk−1 | 7 | Run >10 miles·wk−1 | 10 | Running >25 miles·wk−1 | 33.75 | Exercise almost every day, average of break into a sweat and go to exhaustion, >60 min·session−1 | ||
BALL ST indicates Ball State Adult Fitness Longitudinal Lifestyle Study; and NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center.
Direct Assessment of CRF
CRF was measured as VO2max determined from a cardiopulmonary exercise test on a treadmill using a standardized protocol (ie, Bruce,38 Ball State University Bruce Ramp,42 modified Balke‐Ware,38 and individualized protocols). The treadmill protocol was selected on the basis of self‐reported physical activity level with the goal of participants achieving maximal effort within 8 to 12 minutes. Ventilatory expired gas measurements were collected using commercially available computerized indirect calorimetry systems, as described previously.32 The indirect calorimetry systems were calibrated before exercise testing, according to the manufacturer's instructions. Respiratory data were averaged every 20 or 30 seconds, and VO2max was determined by averaging the highest 2 to 3 consecutively measured oxygen consumption values occurring in the last 2 minutes of the test. Participants were encouraged to exercise to volitional fatigue, and only tests in which participants achieved a respiratory exchange ratio of ≥1.10 were included in the analysis.
Statistical Analysis
Analyses were performed in R version 3.6.1 (R Core Team, Vienna, Austria). To assess the agreement between each prediction equation and directly measured CRF, intraclass correlation coefficient (ICC) estimates and their 95% CIs were calculated using the “irr” package in R based on a single‐score 1‐way model. Bland‐Altman plots were created to visualize the relationship between changes in the different prediction equations and directly measured CRF. The Benjamini‐Hochberg procedure was used to compare changes in eCRF with the changes in directly measured CRF and was used to compare differences between tests for continuous variables. Briefly, the Benjamini‐Hochberg procedure ranks and compares P values from t‐tests comparing directly measured CRF and eCRF with a critical value with a false discovery rate of 5%. This procedure accounts for multiple comparisons and reduces the risk of false positives.43 McNemar tests were used to compare the binary risk factors between tests. To allow for comparisons with previous research, Pearson product moment correlations and SEE values were calculated for the relationships between each prediction equation and directly measured CRF.
A change of ≥5% from the first test was used to classify participants as having increased (≥5%), decreased (≥5%), or no change (0%–4.9% change in either direction) in CRF.44 To compare the agreement in classifying directional changes when using eCRF versus directly measured CRF, concordant and discordant pairs were determined and used to calculate γ coefficients.45 In addition, Cohen's κ coefficients and their 95% CIs were determined. To examine the influence of follow‐up time on classifications, participants with a follow‐up test within 3 to 8 months were classified as having a “short” follow‐up, whereas those with ≥2 years were classified as having a “long” follow‐up. χ2 Tests were then performed for each prediction equation to examine the impact of follow‐up time on the percentage of participants correctly identified as having increased, decreased, or no change in CRF. Statistical significance was set at P<0.05, 2 tailed. Data are presented throughout the article as mean±SD, unless otherwise indicated.
Results
Descriptive characteristics of the sample at both tests are provided in Table 4.46 The sample included 987 participants (33% women; baseline age, 43.1±10.4 years) with an average follow‐up of 3.2±5.4 years (range, 3.0 months–38.0 years). Directly measured CRF (ie, VO2max) increased from test 1 (34.9±9.3 mL·kg−1·min−1) to test 2 (36.8±9.7 mL·kg−1·min−1) (P<0.05). Table 5, 20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 summarizes eCRF from the different equations for each test. At the baseline test, the ICC estimates were significant for 26 of 27 equations, with a range of 0.01 to 0.80 (“poor” to “good” associations based on the ICC interpretation proposed by Koo and Li47), the R 2 values had a range of 0.34 to 0.67, and the SEE values ranged from 4.1 to 6.1 mL·kg−1·min−1. For the second test, the ICC estimates were significant for all equations, with a range of 0.11 to 0.81 (“poor” to “good”), the R 2 values had a range of 0.31 to 0.71, and the SEE values ranged from 4.1 to 6.0 mL·kg−1·min−1. eCRF was statistically different from directly measured CRF for 23 of 27 equations at the baseline test and 26 of the equations for the second test.
Table 4.
Descriptive Characteristics of the Cohort
| Characteristic | Test 1 | Test 2 |
|---|---|---|
| Age, y | 43.1±10.4 | 46.3±11.0* |
| Height, m | 1.74±0.09 | 1.74±0.09 |
| Weight, kg | 80.2±17.4 | 79.8±16.9 |
| BMI, kg·m−2 | 26.3±4.8 | 26.2±4.8 |
| Waist circumference, cm | 89.0±14.0 | 88.9±13.6 |
| Body fat, % | 28.8±8.3 | 27.7±8.1* |
| Obesity, % | 24 | 23 |
| Hypertension, % | 22 | 21 |
| Dyslipidemia, % | 46 | 42* |
| Diabetes mellitus, % | 3 | 3 |
| Smoker, % | 12 | 9* |
| Inactive, % | 66 | 36* |
| Ethnicity, % | ||
| Asian or Pacific Islander | 0.2 | 0.2 |
| Black, not of Hispanic origin | 0.2 | 0.2 |
| Hispanic | 0 | 0 |
| White, not of Hispanic origin | 99.6 | 99.6 |
| Resting heart rate, beat·min−1 | 67.5±11.0 | 64.4±10.4* |
| VO2max, mL·kg−1·min−1 | 34.9±9.3 | 36.8±9.7* |
| FRIEND CRF percentile | 49±26 | 60±25* |
| Maximum heart rate, beat·min−1 | 179.8±13.5 | 175.7±13.5* |
| Maximum RER | 1.2±0.1 | 1.2±0.1 |
| Peak RPE | 18.3±1.7 | 18.4±1.8* |
Data are given as mean±SD. BMI indicates body mass index; FRIEND CRF percentile, VO2max percentile ranking from the Fitness Registry and the Importance of Exercise National Database46; RER, respiratory exchange ratio; RPE, rating of perceived exertion (6–20 Borg scale); and VO2max, maximal oxygen consumption.
Significantly different from test 1 (P<0.05).
Table 5.
Directly Measured CRF and eCRF at the First and Second Cardiopulmonary Exercise Test
| Variable | n | First Test | ICC (95% CI) | n | Second Test | ICC (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | R 2 | SEE | Mean±SD | R 2 | SEE | |||||
| Directly measured CRF | 34.9±9.3 | 36.8±9.7 | ||||||||
| No PA measure | ||||||||||
| Riddle et al 198024 | 987 | 29.6±6.9a | 0.46b | 5.1 | 0.49 (0.44–0.54)b | 987 | 28.3±7.1a, c | 0.55b | 4.7 | 0.37 (0.32–0.42)b |
| Wasserman et al 199425 | 987 | 33.9±7.0a | 0.54b | 4.7 | 0.70 (0.67–0.73)b | 987 | 32.8±7.1a, c | 0.62b | 4.3 | 0.66 (0.63–0.70)b |
| Jang et al 2012 (model 1)26 | 798 | 45.5±6.5a | 0.34b | 5.3 | 0.01 (−0.06 to 0.08) | 772 | 45.3±6.5a, c | 0.31b | 5.4 | 0.11 (0.04–0.18)b |
| Baynard et al 2016 (BMI)27 | 987 | 36.6±7.1a | 0.53b | 4.9 | 0.68 (0.65–0.71) b | 987 | 35.6±7.3a, c | 0.61b | 4.5 | 0.74 (0.71–0.77)b |
| Baynard et al 2016 (WC)27 | 813 | 35.6±7.4a | 0.57b | 4.9 | 0.73 (0.69–0.76)b | 845 | 35.0±7.4a, c | 0.62b | 4.6 | 0.76 (0.73–0.79)b |
| Myers et al 201728 | 987 | 36.2±7.3a | 0.53b | 5.0 | 0.70 (0.66–0.73)b | 987 | 35.1±7.5a, c | 0.62b | 4.7 | 0.74 (0.71–0.77)b |
| de Souza et al 201829 | 987 | 35.3±7.4 | 0.54b | 5.1 | 0.71 (0.68–0.74)b | 987 | 34.3±7.6a, c | 0.62b | 4.7 | 0.73 (0.70–0.76)b |
| Includes measure of PA | ||||||||||
| Jackson et al 1990 (BMI)30 | 811 | 32.6±9.7a | 0.61b | 6.1 | 0.76 (0.73–0.79)b | 799 | 34.2±9.8a, c | 0.62b | 6.0 | 0.77 (0.74–0.80)b |
| Jackson et al 1990 (%fat)30 | 456 | 28.2±9.1a | 0.60b | 5.8 | 0.70 (0.65–0.74)b | 490 | 30.3±8.6a, c | 0.53b | 5.8 | 0.68 (0.63–0.73)b |
| Heil et al 199531 | 456 | 34.3±7.5a | 0.55b | 5.0 | 0.70 (0.65–0.74)b | 490 | 36.4±7.2a, c | 0.51b | 5.1 | 0.64 (0.59–0.69)b |
| Whaley et al 1995 (BMI)32 | 878 | 34.7±8.3 | 0.62b | 5.2 | 0.78 (0.75–0.81)b | 861 | 36.1±8.4c | 0.59b | 5.3 | 0.76 (0.73–0.79)b |
| Whaley et al 1995 (%fat)32 | 490 | 30.6±8.4a | 0.62b | 5.2 | 0.78 (0.74–0.81)b | 529 | 32.2±7.8a, c | 0.55b | 5.3 | 0.73 (0.68–0.76)b |
| Matthews et al 199933 | 811 | 37.1±8.2a | 0.62b | 5.1 | 0.75 (0.72–0.78)b | 799 | 38.2±8.4a, c | 0.65b | 5.0 | 0.78 (0.75–0.80)b |
| Jurca et al 2005 (ACLS)34 | 808 | 35.5±8.0a | 0.65b | 4.7 | 0.79 (0.77–0.82)b | 793 | 37.0±8.1a, c | 0.67b | 4.6 | 0.80 (0.78–0.83)b |
| Jurca et al 2005 (ADNFS)34 | 808 | 38.4±7.6a | 0.63b | 4.6 | 0.70 (0.66–0.73)b | 793 | 38.0±7.8a | 0.70b | 4.3 | 0.79 (0.77–0.82)b |
| Jurca et al 2005 (NASA)34 | 808 | 34.4±8.1 | 0.66b | 4.7 | 0.80 (0.78–0.83)b | 793 | 35.2±8.2a, c | 0.69b | 4.6 | 0.81 (0.79–0.84)b |
| Wier et al 2006 (BMI)35 | 811 | 34.2±8.4a | 0.63b | 5.1 | 0.79 (0.76–0.81)b | 799 | 35.4±8.6a, c | 0.64b | 5.1 | 0.79 (0.76–0.82)b |
| Wier et al 2006 (%fat)35 | 456 | 30.1±8.0a | 0.63b | 4.9 | 0.77 (0.73–0.81)b | 490 | 31.7±7.5a, c | 0.56b | 5.0 | 0.73 (0.68–0.77)b |
| Wier et al 2006 (WC)35 | 676 | 33.1±8.1a | 0.64b | 4.9 | 0.79 (0.76–0.82)b | 698 | 34.5±8.1a, c | 0.64b | 4.9 | 0.79 (0.76–0.81)b |
| Nes et al 201136 | 676 | 40.9±7.5a | 0.67b | 4.4 | 0.53 (0.47–0.58)b | 697 | 41.6±7.7a, c | 0.71b | 4.2 | 0.61 (0.56–0.65)b |
| Cáceres et al 2012 (9 levels)37 | 666 | 34.1±6.8 | 0.42b | 5.1 | 0.63 (0.58–0.67)b | 642 | 31.7±6.6a, c | 0.52b | 4.6 | 0.61 (0.55–0.65)b |
| Cáceres et al 2012 (5 levels)37 | 666 | 35.2±7.0a | 0.42b | 5.4 | 0.62 (0.57–0.66)b | 643 | 32.5±6.8a, c | 0.48b | 4.9 | 0.62 (0.57–0.66)b |
| Jackson et al 2012 (BMI, 5‐level PA)20 | 595 | 38.3±7.0a | 0.57b | 4.6 | 0.58 (0.53–0.63)b | 592 | 38.8±7.2a, c | 0.65b | 4.3 | 0.68 (0.64–0.72)b |
| Jackson et al 2012 (%fat, 5‐level PA)20 | 383 | 36.5±6.4a | 0.60b | 4.1 | 0.58 (0.51–0.64)b | 412 | 37.6±6.3a, c | 0.59b | 4.1 | 0.58 (0.52–0.64)b |
| Jackson et al 2012 (BMI, 2‐level PA)20 | 595 | 38.2±7.1a | 0.56b | 4.7 | 0.59 (0.54–0.64)b | 592 | 38.6±7.3a, c | 0.65b | 4.4 | 0.70 (0.65–0.74)b |
| Jackson et al 2012 (%fat, 2‐level PA)20 | 383 | 36.4±6.4a | 0.59b | 4.1 | 0.59 (0.52–0.65)b | 412 | 37.4±6.4a, c | 0.59b | 4.1 | 0.60 (0.54–0.66)b |
| Jang et al 2012 (model 2)26 | 682 | 44.7±6.7a | 0.46b | 4.9 | 0.13 (0.05–0.20)b | 666 | 45.7±6.7a, c | 0.43b | 5.1 | 0.15 (0.07–0.22)b |
%Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; ICC, intraclass correlation coefficient; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Significantly different from directly measured CRF.
Significant correlation/association with directly measured CRF.
Significantly different from test 1 (P<0.05).
Table 6, 20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 summarizes the change in directly measured CRF and eCRF for each prediction equation for all follow‐up times, whereas Table 7, 20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 summarizes the change in directly measured CRF and eCRF for each prediction equation for follow‐up times ≤8 months and ≥2 years. For all follow‐up times, the ICC estimates were significant for 26 of 27 equations, with a range of 0.06 to 0.63 (“poor” to “moderate”), the R 2 values ranged from 0.06 to 0.43, and the SEE values had a range from 0.9 to 5.9 mL·kg−1·min−1. For 16 of the 27 equations, the change in eCRF was significantly different from the change in directly measured CRF. Bland‐Altman plots for the change in eCRF and change in directly measured CRF from each equation are provided in Figure 2.20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37
Table 6.
Changes in Directly Measured CRF and eCRF Between the First and Second Cardiopulmonary Exercise Tests for All Follow‐Up Times
| Variable | n | Mean±SD | R 2 | SEE | ICC (95% CI) |
|---|---|---|---|---|---|
| Directly measured CRF | 1.8±6.4 | ||||
| No PA measure | |||||
| Riddle et al 198024 | 987 | −1.3±3.8a | 0.35b | 3.0 | 0.40 (0.35–0.45)b |
| Wasserman et al 199425 | 987 | −1.1±3.1a | 0.37b | 2.5 | 0.36 (0.31–0.42)b |
| Jang et al 2012 (model 1)26 | 676 | −0.2±1.1a | 0.27b | 0.9 | 0.13 (0.06–0.21)b |
| Baynard et al 2016 (BMI)27 | 987 | −1.0±3.1a | 0.34b | 2.6 | 0.35 (0.30–0.41)b |
| Baynard et al 2016 (WC)27 | 770 | −0.7±3.5a | 0.36b | 2.8 | 0.43 (0.37–0.48)b |
| Myers et al 201728 | 987 | −1.1±3.1a | 0.38b | 2.4 | 0.37 (0.31–0.42)b |
| de Souza et al 201829 | 987 | −1.1±3.3a | 0.36b | 2.7 | 0.38 (0.33–0.43)b |
| Includes measure of PA | |||||
| Jackson et al 1990 (BMI)30 | 723 | 2.0±7.2 | 0.33b | 5.9 | 0.57 (0.52–0.61)b |
| Jackson et al 1990 (%fat)30 | 390 | 2.3±6.9a | 0.33b | 5.7 | 0.56 (0.49–0.63)b |
| Heil et al 199531 | 390 | 2.2±6.0a | 0.33b | 4.9 | 0.56 (0.49–0.63)b |
| Whaley et al 1995 (BMI)32 | 801 | 1.4±6.1 | 0.30b | 5.1 | 0.54 (0.49–0.59)b |
| Whaley et al 1995 (%fat)32 | 436 | 1.6±6.1 | 0.30b | 5.1 | 0.55 (0.48–0.61)b |
| Matthews et al 199933 | 723 | 1.4±5.8 | 0.37b | 4.6 | 0.60 (0.55–0.65)b |
| Jurca et al 2005 (ACLS)34 | 715 | 1.7±5.7 | 0.37b | 4.5 | 0.61 (0.56–0.65)b |
| Jurca et al 2005 (ADNFS)34 | 715 | −0.1±4.2a | 0.41b | 3.2 | 0.54 (0.49–0.59)b |
| Jurca et al 2005 (NASA)34 | 715 | 1.1±5.2a | 0.40b | 4.0 | 0.62 (0.57–0.66)b |
| Wier et al 2006 (BMI)35 | 723 | 1.6±6.4 | 0.35b | 5.2 | 0.59 (0.54–0.63)b |
| Wier et al 2006 (%fat)35 | 390 | 1.9±6.3 | 0.34b | 5.2 | 0.58 (0.51–0.64)b |
| Wier et al 2006 (WC)35 | 586 | 1.8±6.0 | 0.35b | 4.8 | 0.59 (0.54–0.64)b |
| Nes et al 201136 | 585 | 1.0±4.8a | 0.43b | 3.6 | 0.63 (0.58–0.68)b |
| Cáceres et al 2012 (9 levels)37 | 524 | −1.8±3.7a | 0.09b | 3.6 | 0.14 (0.06–0.23)b |
| Cáceres et al 2012 (5 levels)37 | 525 | −2.2±3.2a | 0.06b | 3.1 | 0.06 (−0.03 to 0.14) |
| Jackson et al 2012 (BMI, 5‐level PA)20 | 459 | 0.6±3.6a | 0.43b | 2.7 | 0.56 (0.50–0.62)b |
| Jackson et al 2012 (%fat, 5‐level PA)20 | 297 | 0.7±3.6 | 0.37b | 2.8 | 0.54 (0.45–0.62)b |
| Jackson et al 2012 (BMI, 2‐level PA)20 | 459 | 0.5±3.6a | 0.42b | 2.8 | 0.56 (0.49–0.62)b |
| Jackson et al 2012 (%fat, 2‐level PA)20 | 297 | 0.6±3.6 | 0.37b | 2.9 | 0.54 (0.45–0.62)b |
| Jang et al 2012 (model 2)26 | 547 | 1.1±2.9 | 0.32b | 2.4 | 0.43 (0.36–0.50)b |
%Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; ICC, intraclass correlation coefficient; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Significantly different from directly measured CRF.
Significant correlation/association with directly measured CRF.
Table 7.
Changes in Directly Measured CRF and eCRF Between the First and Second Cardiopulmonary Exercise Tests for Follow‐Up Times ≤8 Months and ≥2 Years
| Variable | n | ≤8 mo | ICC (95% CI) | n | ≥2 y | ICC (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | R 2 | SEE | Mean±SD | R 2 | SEE | |||||
| Directly measured CRF | 4.3±4.9 | −2.4±6.7 | ||||||||
| No PA measure | ||||||||||
| Riddle et al 198024 | 486 | 0.5±1.6a | 0.08b | 1.6 | −0.08 (−0.17 to 0.01) | 324 | −4.5±4.7a | 0.31b | 3.9 | 0.47 (0.38–0.55)b |
| Wasserman et al 199425 | 486 | 0.4±1.3a | 0.09b | 1.2 | −0.11 (−0.20 to −0.03) | 324 | −3.8±3.8a | 0.32b | 3.2 | 0.46 (0.37–0.54)b |
| Jang et al 2012 (model 1)26 | 336 | 0.2±0.7a | 0.06b | 0.7 | −0.18 (−0.28 to −0.08) | 224 | −0.9±1.2a | 0.20b | 1.1 | 0.13 (−0.00 to 0.25) |
| Baynard et al 2016 (BMI)27 | 486 | 0.4±1.5a | 0.05b | 1.5 | −0.12 (−0.20 to −0.03) | 324 | −3.6±3.8a | 0.30b | 3.1 | 0.45 (0.36–0.53)b |
| Baynard et al 2016 (WC)27 | 390 | 0.7±1.9a | 0.12b | 1.8 | 0.01 (−0.09 to 0.11) | 250 | −3.5±4.2a | 0.29b | 3.5 | 0.48 (0.37–0.57)b |
| Myers et al 201728 | 486 | 0.4±1.1a | 0.11b | 1.0 | −0.12 (−0.21 to −0.03) | 324 | −4.0±3.8a | 0.34b | 3.1 | 0.47 (0.38–0.55)b |
| de Souza et al 201829 | 486 | 0.5±1.5a | 0.07b | 1.4 | −0.10 (−0.19 to −0.01) | 324 | −3.9±4.0a | 0.32b | 3.3 | 0.47 (0.38–0.55)b |
| Includes measure of PA | ||||||||||
| Jackson et al 1990 (BMI)30 | 357 | 5.1±5.6a | 0.15b | 5.1 | 0.37 (0.27–0.45)b | 236 | −3.0±7.4 | 0.28b | 6.3 | 0.52 (0.43–0.61)b |
| Jackson et al 1990 (%fat)30 | 158 | 5.8±4.9a | 0.09b | 4.7 | 0.26 (0.11–0.40)b | 154 | −2.0±6.7 | 0.27b | 5.7 | 0.51 (0.39–0.62)b |
| Heil et al 199531 | 158 | 5.1±4.3 | 0.09b | 4.1 | 0.29 (0.14–0.43)b | 154 | −1.4±5.8a | 0.27b | 4.9 | 0.50 (0.38–0.61)b |
| Whaley et al 1995 (BMI)32 | 398 | 3.9±4.7 | 0.12b | 4.4 | 0.35 (0.26–0.43)b | 259 | −2.4±6.3 | 0.22b | 5.6 | 0.47 (0.37–0.56)b |
| Whaley et al 1995 (%fat)32 | 184 | 4.3±4.5 | 0.05b | 4.4 | 0.23 (0.09–0.36)b | 163 | −2.2±5.9 | 0.26b | 5.1 | 0.51 (0.38–0.61)b |
| Matthews et al 199933 | 357 | 4.0±4.3 | 0.16b | 3.9 | 0.40 (0.31–0.49)b | 236 | −2.8±6.0 | 0.33b | 4.9 | 0.57 (0.48–0.65)b |
| Jurca et al 2005 (ACLS)34 | 353 | 4.2±4.2 | 0.18b | 3.8 | 0.42 (0.33–0.51)b | 234 | −2.4±5.8 | 0.30b | 4.9 | 0.54 (0.44–0.63)b |
| Jurca et al 2005 (ADNFS)34 | 353 | 1.9±2.4a | 0.15b | 2.2 | 0.21 (0.11–0.31)b | 234 | −3.8±4.5a | 0.33b | 3.7 | 0.51 (0.41–0.60)b |
| Jurca et al 2005 (NASA)34 | 353 | 3.5±3.5a | 0.19b | 3.2 | 0.41 (0.32–0.49)b | 234 | −3.0±5.5 | 0.34b | 4.5 | 0.57 (0.48–0.65)b |
| Wier et al 2006 (BMI)35 | 357 | 4.3±4.7 | 0.16b | 4.4 | 0.40 (0.31–0.48)b | 236 | −3.0±6.6 | 0.29b | 5.6 | 0.54 (0.45–0.63)b |
| Wier et al 2006 (%fat)35 | 158 | 5.2±4.4 | 0.09b | 4.2 | 0.28 (0.13–0.42)b | 154 | −2.2±6.1 | 0.27b | 5.3 | 0.52 (0.39–0.62)b |
| Wier et al 2006 (WC)35 | 293 | 4.4±4.7 | 0.17b | 4.3 | 0.41 (0.31–0.50)b | 192 | −2.4±5.8 | 0.29b | 4.9 | 0.54 (0.43–0.63)b |
| Nes et al 201136 | 292 | 3.2±3.6a | 0.22b | 3.2 | 0.45 (0.35–0.53)b | 192 | −2.6±4.8 | 0.36b | 3.8 | 0.57 (0.47–0.66)b |
| Cáceres et al 2012 (9 levels)37 | 259 | −0.9±3.0a | 0.00 | 3.0 | −0.28 (−0.39 to −0.16) | 172 | −3.9±4.2a | 0.10b | 4.0 | 0.27 (0.13–0.41)b |
| Cáceres et al 2012 (5 levels)37 | 259 | −1.5±2.4a | 0.04b | 2.4 | −0.43 (−0.52 to −0.32) | 173 | −4.0±3.9a | 0.11b | 3.7 | 0.27 (0.13–0.41)b |
| Jackson et al 2012 (BMI, 5‐level PA)20 | 225 | 2.3±2.5a | 0.23b | 2.2 | 0.34 (0.22–0.45)b | 158 | −1.9±3.8 | 0.32b | 3.1 | 0.50 (0.37–0.60)b |
| Jackson et al 2012 (%fat, 5‐level PA)20 | 114 | 2.5±2.6a | 0.12b | 2.5 | 0.26 (0.08–0.42)b | 126 | −1.3±3.6a | 0.32b | 3.0 | 0.48 (0.33–0.60)b |
| Jackson et al 2012 (BMI, 2‐level PA)20 | 225 | 2.2±2.5a | 0.21b | 2.2 | 0.32 (0.20–0.44)b | 158 | −2.1±3.9 | 0.32b | 3.2 | 0.50 (0.38–0.61)b |
| Jackson et al 2012 (%fat, 2‐level PA)20 | 114 | 2.4±2.6a | 0.11b | 2.5 | 0.24 (0.06–0.41)b | 126 | −1.5±3.7a | 0.31b | 3.1 | 0.48 (0.33–0.60)b |
| Jang et al 2012 (model 2)26 | 272 | 2.1±2.3a | 0.20b | 2.1 | 0.30 (0.19–0.41)b | 182 | −0.6±2.9a | 0.22b | 2.6 | 0.30 (0.16–0.42)b |
%Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; ICC, intraclass correlation coefficient; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Significantly different from directly measured CRF.
Significant correlation/association with directly measured CRF.
Figure 2. Bland‐Altman plots for the changes in cardiorespiratory fitness between the first and second cardiopulmonary exercise tests for each equation.
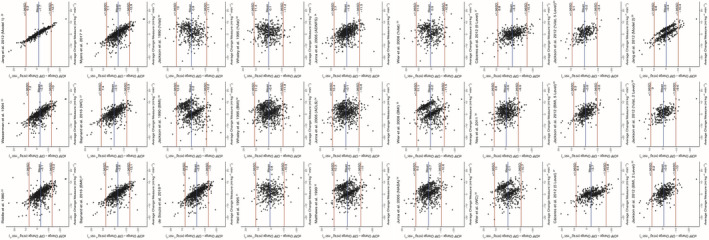
%Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Table 8, 20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 presents the percentage of participants correctly and incorrectly identified as having increased, decreased, or no change to CRF when using the prediction equations. The median correctly categorized as having increased CRF was 59% (range, 2%–75%), having decreased CRF was 60% (range, 15%–71%), and having no change in CRF was 57% (range, 28%–99%). The Cohen's κ coefficients were all significant, with a range 0.05 to 0.40 (“none” to “weak” levels of agreement based on the interpretations proposed by McHugh48). A significant interaction was observed between follow‐up time and the percentage of participants correctly classified by change in CRF (P<0.001). The percentage of participants correctly classified when the follow‐up time was ≤8 months is presented in Table 9.20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 The median correctly categorized as having increased CRF was 68% (range, 1%–86%), having decreased CRF was 7% (range, 0%–40%), and having no change in CRF was 65% (range, 26%–100%). Table 10, 20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 presents the percentage of participants correctly classified when the follow‐up time was ≥2 years. The median correctly categorized as having increased CRF was 34% (range, 3%–50%), having decreased CRF was 74% (range, 22%–92%), and having no change in CRF was 39% (range, 27%–95%). The γ coefficients for most of the prediction equations were significant for the different follow‐up times and are summarized in Table 11.20, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 When examining all follow‐up times, the median γ coefficient was 0.702, indicating a “strong” association,49 with a range of 0.005 to 0.801 (none to “strong” association).
Table 8.
Percentage of Participants Classified as Having Increased, Decreased, or No Change in CRF, According to Directly Measured CRF and eCRF
| Variable | Cohen's κ (95% CI) | Decrease in Directly Measured CRF | No Change in Directly Measured CRF | Increase in Directly Measured CRF | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | ||
| No PA measure | ||||||||||
| Riddle et al 198024 | 0.22 (0.19–0.26)* | 71 | 27 | 2 | 30 | 64 | 6 | 13 | 65 | 22 |
| Wasserman et al 199425 | 0.19 (0.16–0.23)* | 64 | 35 | 1 | 22 | 76 | 2 | 9 | 77 | 14 |
| Jang et al 2012 (model 1)26 | 0.05 (0.03–0.07)* | 15 | 85 | 0 | 1 | 99 | 0 | 1 | 97 | 2 |
| Baynard et al 2016 (BMI)27 | 0.19 (0.16–0.22)* | 62 | 36 | 2 | 22 | 76 | 2 | 8 | 77 | 15 |
| Baynard et al 2016 (WC)27 | 0.23 (0.19–0.27)* | 63 | 32 | 5 | 27 | 65 | 8 | 9 | 63 | 29 |
| Myers et al 201728 | 0.19 (0.15–0.22)* | 61 | 38 | 1 | 20 | 78 | 1 | 8 | 79 | 13 |
| de Souza et al 201829 | 0.20 (0.17–0.23)* | 63 | 35 | 2 | 25 | 73 | 3 | 10 | 72 | 18 |
| Includes measure of PA | ||||||||||
| Jackson et al 1990 (BMI)30 | 0.34 (0.29–0.39)* | 57 | 30 | 13 | 20 | 51 | 29 | 9 | 31 | 61 |
| Jackson et al 1990 (%fat)30 | 0.39 (0.32–0.47)* | 61 | 19 | 19 | 23 | 34 | 44 | 10 | 16 | 74 |
| Heil et al 199531 | 0.40 (0.32–0.47)* | 59 | 20 | 21 | 17 | 39 | 44 | 8 | 18 | 75 |
| Whaley et al 1995 (BMI)32 | 0.33 (0.27–0.38)* | 56 | 28 | 16 | 21 | 46 | 33 | 11 | 28 | 62 |
| Whaley et al 1995 (%fat)32 | 0.33 (0.26–0.40)* | 59 | 23 | 18 | 26 | 28 | 46 | 13 | 17 | 70 |
| Matthews et al 199933 | 0.36 (0.30–0.41)* | 57 | 33 | 10 | 17 | 56 | 26 | 6 | 34 | 60 |
| Jurca et al 2005 (ACLS)34 | 0.37 (0.31–0.42)* | 56 | 27 | 16 | 17 | 47 | 36 | 8 | 24 | 68 |
| Jurca et al 2005 (ADNFS)34 | 0.36 (0.31–0.41)* | 64 | 29 | 7 | 21 | 64 | 15 | 9 | 41 | 51 |
| Jurca et al 2005 (NASA)34 | 0.37 (0.31–0.42)* | 59 | 29 | 12 | 18 | 53 | 29 | 8 | 30 | 63 |
| Wier et al 2006 (BMI)35 | 0.37 (0.32–0.43)* | 60 | 28 | 12 | 16 | 57 | 27 | 9 | 31 | 60 |
| Wier et al 2006 (%fat)35 | 0.39 (0.31–0.46)* | 60 | 22 | 18 | 20 | 38 | 42 | 10 | 18 | 73 |
| Wier et al 2006 (WC)35 | 0.39 (0.33–0.45)* | 63 | 21 | 17 | 16 | 53 | 31 | 9 | 26 | 64 |
| Nes et al 201136 | 0.39 (0.33–0.45)* | 61 | 24 | 14 | 21 | 52 | 27 | 8 | 27 | 65 |
| Cáceres et al 2012 (9 levels)37 | 0.11 (0.06–0.16)* | 69 | 22 | 8 | 33 | 45 | 22 | 48 | 36 | 16 |
| Cáceres et al 2012 (5 levels)37 | 0.12 (0.07–0.17)* | 61 | 36 | 3 | 30 | 63 | 6 | 57 | 32 | 10 |
| Jackson et al 2012 (BMI, 5‐level PA)20 | 0.39 (0.33–0.46)* | 54 | 36 | 10 | 13 | 71 | 15 | 5 | 37 | 58 |
| Jackson et al 2012 (%fat, 5‐level PA)20 | 0.39 (0.31–0.47)* | 55 | 33 | 12 | 13 | 62 | 25 | 6 | 32 | 62 |
| Jackson et al 2012 (BMI, 2‐level PA)20 | 0.37 (0.30–0.43)* | 55 | 36 | 9 | 16 | 66 | 17 | 7 | 37 | 56 |
| Jackson et al 2012 (%fat, 2‐level PA)20 | 0.36 (0.28–0.44)* | 56 | 32 | 12 | 18 | 56 | 25 | 6 | 34 | 59 |
| Jang et al 2012 (model 2)26 | 0.32 (0.26–0.37)* | 31 | 59 | 10 | 6 | 77 | 17 | 3 | 41 | 56 |
A change of ≥5% from the first test was used to classify participants as having increased, decreased, or no change in CRF. %Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Significant agreement between eCRF and directly measured CRF.
Gray columns indicate correct predictions.
Table 9.
When Follow‐Up Testing Occurred ≤8 Months After the Baseline Test, Percentage of Participants Classified as Having Increased, Decreased, or No Change in CRF, According to Directly Measured CRF and eCRF
| Variable | Cohen's κ (95% CI) | Decrease in Directly Measured CRF | No Change in Directly Measured CRF | Increase in Directly Measured CRF | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | ||
| No PA measure | ||||||||||
| Riddle et al 198024 | 0.07 (0.03–0.11)* | 10 | 82 | 8 | 7 | 81 | 11 | 2 | 73 | 25 |
| Wasserman et al 199425 | 0.06 (0.03–0.08)* | 5 | 88 | 8 | 2 | 95 | 3 | 1 | 83 | 15 |
| Jang et al 2012 (model 1)26 | 0.01 (–0.00 to 0.01) | 0 | 100 | 0 | 0 | 100 | 0 | 1 | 98 | 1 |
| Baynard et al 2016 (BMI)27 | 0.05 (0.02–0.08)* | 8 | 85 | 8 | 4 | 91 | 5 | 1 | 83 | 16 |
| Baynard et al 2016 (WC)27 | 0.10 (0.05–0.15)* | 19 | 74 | 6 | 7 | 79 | 14 | 5 | 64 | 31 |
| Myers et al 201728 | 0.05 (0.02–0.08)* | 5 | 90 | 5 | 2 | 95 | 3 | 0 | 86 | 14 |
| de Souza et al 201829 | 0.06 (0.03–0.09)* | 8 | 85 | 8 | 5 | 89 | 6 | 2 | 79 | 19 |
| Includes measure of PA | ||||||||||
| Jackson et al 1990 (BMI)30 | 0.28 (0.20–0.36)* | 3 | 80 | 17 | 9 | 60 | 32 | 3 | 25 | 72 |
| Jackson et al 1990 (%fat)30 | 0.26 (0.13–0.39)* | 0 | 82 | 18 | 14 | 34 | 52 | 3 | 12 | 86 |
| Heil et al 199531 | 0.29 (0.16–0.42)* | 0 | 82 | 18 | 10 | 41 | 48 | 2 | 13 | 86 |
| Whaley et al 1995 (BMI)32 | 0.21 (0.13–0.29)* | 9 | 68 | 24 | 11 | 49 | 40 | 7 | 23 | 70 |
| Whaley et al 1995 (%fat)32 | 0.13 (0.02–0.23)* | 0 | 71 | 29 | 17 | 26 | 57 | 7 | 16 | 77 |
| Matthews et al 199933 | 0.30 (0.22–0.38)* | 3 | 90 | 7 | 6 | 65 | 29 | 2 | 27 | 71 |
| Jurca et al 2005 (ACLS)34 | 0.27 (0.19–0.36)* | 7 | 62 | 31 | 10 | 48 | 42 | 4 | 18 | 78 |
| Jurca et al 2005 (ADNFS)34 | 0.25 (0.17–0.33)* | 10 | 69 | 21 | 10 | 65 | 25 | 3 | 33 | 63 |
| Jurca et al 2005 (NASA)34 | 0.30 (0.21–0.38)* | 7 | 76 | 17 | 9 | 57 | 34 | 3 | 22 | 75 |
| Wier et al 2006 (BMI)35 | 0.32 (0.24–0.40)* | 7 | 80 | 13 | 5 | 67 | 28 | 3 | 26 | 71 |
| Wier et al 2006 (%fat)35 | 0.30 (0.16–0.43)* | 0 | 82 | 18 | 7 | 45 | 48 | 2 | 14 | 85 |
| Wier et al 2006 (WC)35 | 0.30 (0.21–0.39)* | 13 | 65 | 22 | 6 | 62 | 32 | 5 | 24 | 71 |
| Nes et al 201136 | 0.30 (0.20–0.40)* | 22 | 43 | 35 | 11 | 55 | 34 | 3 | 22 | 74 |
| Cáceres et al 2012 (9 levels)37 | 0.01 (−0.06 to 0.08) | 40 | 40 | 20 | 25 | 50 | 25 | 47 | 36 | 16 |
| Cáceres et al 2012 (5 levels)37 | 0.07 (0.02–0.12)* | 12 | 84 | 4 | 19 | 77 | 5 | 61 | 29 | 11 |
| Jackson et al 2012 (BMI, 5‐level PA)20 | 0.30 (0.20–0.40)* | 10 | 70 | 20 | 8 | 68 | 25 | 3 | 30 | 68 |
| Jackson et al 2012 (%fat, 5‐level PA)20 | 0.26 (0.12–0.40)* | 0 | 89 | 11 | 4 | 65 | 30 | 2 | 29 | 68 |
| Jackson et al 2012 (BMI, 2‐level PA)20 | 0.25 (0.15–0.35)* | 10 | 70 | 20 | 9 | 60 | 30 | 3 | 31 | 66 |
| Jackson et al 2012 (%fat, 2‐level PA)20 | 0.18 (0.04–0.32)* | 0 | 78 | 22 | 13 | 52 | 35 | 2 | 32 | 66 |
| Jang et al 2012 (model 2)26 | 0.35 (0.26–0.43)* | 0 | 96 | 4 | 2 | 82 | 17 | 2 | 32 | 66 |
A change of ≥5% from the first test was used to classify participants as having increased, decreased, or no change in CRF. %Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Significant agreement between eCRF and directly measured CRF.
Gray columns indicate correct predictions.
Table 10.
When Follow‐Up Testing Occurred ≥2 Years After the Baseline Test, Percentage of Participants Classified as Having Increased, Decreased, or No Change in CRF, According to Directly Measured CRF and eCRF
| Variable | Cohen's κ (95% CI) | Decrease in Directly Measured CRF | No Change in Directly Measured CRF | Increase in Directly Measured CRF | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | Estimated Decreased CRF | Estimated No Change CRF | Estimated Increased CRF | ||
| No PA measure | ||||||||||
| Riddle et al 198024 | 0.19 (0.12–0.26)* | 92 | 8 | 1 | 72 | 27 | 2 | 57 | 33 | 10 |
| Wasserman et al 199425 | 0.20 (0.13–0.27)* | 86 | 14 | 0 | 61 | 38 | 2 | 47 | 46 | 7 |
| Jang et al 2012 (model 1)26 | 0.09 (0.05–0.14)* | 22 | 78 | 0 | 5 | 95 | 0 | 2 | 95 | 3 |
| Baynard et al 2016 (BMI)27 | 0.24 (0.17–0.31)* | 84 | 15 | 1 | 53 | 47 | 0 | 38 | 54 | 8 |
| Baynard et al 2016 (WC)27 | 0.22 (0.14–0.31)* | 79 | 17 | 4 | 59 | 39 | 2 | 31 | 53 | 16 |
| Myers et al 201728 | 0.21 (0.14–0.29)* | 85 | 15 | 0 | 59 | 41 | 0 | 45 | 47 | 8 |
| de Souza et al 201829 | 0.22 (0.15–0.29)* | 86 | 14 | 1 | 61 | 39 | 0 | 45 | 45 | 10 |
| Includes measure of PA | ||||||||||
| Jackson et al 1990 (BMI)30 | 0.25 (0.16–0.35)* | 74 | 15 | 11 | 45 | 29 | 26 | 33 | 30 | 37 |
| Jackson et al 1990 (%fat)30 | 0.31 (0.19–0.43)* | 73 | 10 | 16 | 35 | 31 | 35 | 29 | 24 | 48 |
| Heil et al 199531 | 0.31 (0.20–0.43)* | 70 | 12 | 19 | 27 | 35 | 38 | 24 | 26 | 50 |
| Whaley et al 1995 (BMI)32 | 0.30 (0.21–0.39)* | 69 | 18 | 12 | 34 | 40 | 26 | 24 | 34 | 43 |
| Whaley et al 1995 (%fat)32 | 0.25 (0.13–0.36)* | 69 | 16 | 14 | 38 | 28 | 34 | 30 | 26 | 44 |
| Matthews et al 199933 | 0.30 (0.20–0.39)* | 74 | 17 | 9 | 43 | 33 | 24 | 21 | 39 | 40 |
| Jurca et al 2005 (ACLS)34 | 0.33 (0.23–0.42)* | 72 | 17 | 12 | 29 | 46 | 24 | 24 | 35 | 41 |
| Jurca et al 2005 (ADNFS)34 | 0.29 (0.20–0.37)* | 80 | 17 | 2 | 44 | 56 | 0 | 32 | 55 | 14 |
| Jurca et al 2005 (NASA)34 | 0.32 (0.23–0.42)* | 75 | 17 | 9 | 37 | 46 | 17 | 26 | 38 | 36 |
| Wier et al 2006 (BMI)35 | 0.31 (0.21–0.40)* | 77 | 12 | 11 | 38 | 38 | 24 | 33 | 30 | 37 |
| Wier et al 2006 (%fat)35 | 0.28 (0.16–0.40)* | 72 | 12 | 16 | 35 | 31 | 35 | 33 | 21 | 45 |
| Wier et al 2006 (WC)35 | 0.33 (0.22–0.43)* | 77 | 9 | 14 | 38 | 38 | 24 | 30 | 28 | 42 |
| Nes et al 201136 | 0.31 (0.20–0.41)* | 73 | 17 | 10 | 41 | 47 | 12 | 23 | 43 | 34 |
| Cáceres et al 2012 (9 levels)37 | 0.17 (0.06–0.27)* | 84 | 12 | 4 | 53 | 33 | 13 | 63 | 27 | 10 |
| Cáceres et al 2012 (5 levels)37 | 0.14 (0.04–0.25)* | 81 | 17 | 2 | 60 | 33 | 7 | 63 | 27 | 10 |
| Jackson et al 2012 (BMI, 5‐level PA)20 | 0.32 (0.22–0.42)* | 66 | 26 | 8 | 19 | 73 | 8 | 16 | 58 | 27 |
| Jackson et al 2012 (%fat, 5‐level PA)20 | 0.34 (0.22–0.47)* | 66 | 21 | 13 | 20 | 65 | 15 | 14 | 47 | 39 |
| Jackson et al 2012 (BMI, 2‐level PA)20 | 0.32 (0.21–0.42)* | 67 | 26 | 7 | 23 | 73 | 4 | 16 | 60 | 24 |
| Jackson et al 2012 (%fat, 2‐level PA)20 | 0.32 (0.21–0.44)* | 66 | 23 | 11 | 20 | 65 | 15 | 14 | 53 | 33 |
| Jang et al 2012 (model 2)26 | 0.22 (0.13–0.31)* | 43 | 45 | 12 | 13 | 68 | 19 | 4 | 61 | 35 |
A change of ≥5% from the first test was used to classify participants as having increased, decreased, or no change in CRF. %Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Significant agreement between eCRF and directly measured CRF.
Gray columns indicate correct predictions.
Table 11.
γ Coefficients From the Analysis Comparing CRF Directional Change Classifications When Using eCRF Versus Directly Measured CRF at ≤8 Months, ≥2 Years, and All Follow‐Up Time Points
| Variable | ≤8 mo | ≥2 y | All Follow‐Up Times |
|---|---|---|---|
| No PA measure | |||
| Riddle et al 198024 | 0.476a | 0.641a | 0.726a |
| Wasserman et al 199425 | 0.505a | 0.611a | 0.755a |
| Jang et al 2012 (model 1)26 | −0.200 | 0.802a | 0.801a |
| Baynard et al 2016 (BMI)27 | 0.479a | 0.658a | 0.745a |
| Baynard et al 2016 (WC)27 | 0.479a | 0.623a | 0.710a |
| Myers et al 201728 | 0.611a | 0.626a | 0.770a |
| de Souza et al 201829 | 0.493 a | 0.630 a | 0.731 a |
| Includes measure of PA | |||
| Jackson et al 1990 (BMI)30 | 0.659a | 0.530a | 0.656a |
| Jackson et al 1990 (%fat)30 | 0.720a | 0.560a | 0.695a |
| Heil et al 199531 | 0.750a | 0.562a | 0.696a |
| Whaley et al 1995 (BMI)32 | 0.505a | 0.571a | 0.622a |
| Whaley et al 1995 (%fat)32 | 0.470a | 0.515a | 0.636a |
| Matthews et al 199933 | 0.728a | 0.629a | 0.713a |
| Jurca et al 2005 (ACLS)34 | 0.611a | 0.591a | 0.668a |
| Jurca et al 2005 (ADNFS)34 | 0.612a | 0.666a | 0.727a |
| Jurca et al 2005 (NASA)34 | 0.675a | 0.617a | 0.693a |
| Wier et al 2006 (BMI)35 | 0.704a | 0.567a | 0.685a |
| Wier et al 2006 (%fat)35 | 0.741a | 0.516a | 0.688a |
| Wier et al 2006 (WC)35 | 0.614a | 0.570a | 0.662a |
| Nes et al 201136 | 0.616a | 0.608a | 0.702a |
| Cáceres et al 2012 (9 levels)37 | −0.237 | 0.391a | 0.176 |
| Cáceres et al 2012 (5 levels)37 | −0.532a | 0.352 | 0.005 |
| Jackson et al 2012 (BMI, 5‐level PA)20 | 0.670a | 0.649a | 0.745a |
| Jackson et al 2012 (%fat, 5‐level PA)20 | 0.673a | 0.631a | 0.725a |
| Jackson et al 2012 (BMI, 2‐level PA)20 | 0.617a | 0.665a | 0.723a |
| Jackson et al 2012 (%fat, 2‐level PA)20 | 0.564a | 0.630a | 0.701a |
| Jang et al 2012 (model 2)26 | 0.791a | 0.606a | 0.731a |
%Fat indicates percentage body fat; ACLS, equation based on data from the Aerobics Center Longitudinal Study; ADNFS, equation based on data from the Allied Dunbar National Fitness Survey; BMI, body mass index; CRF, cardiorespiratory fitness; eCRF, estimated CRF; NASA, equation based on data from National Aeronautics and Space Administration/Johnson Space Center; PA, physical activity; and WC, waist circumference.
Significant association between eCRF and directly measured CRF.
Discussion
Comparable to other established vital signs, routine assessment of CRF can improve mortality risk predictions.14, 15, 16, 17, 18, 19 As a result, an American Heart Association Scientific Statement suggests that clinicians regularly assess CRF alongside other risk factors by minimally determining a patient's eCRF using nonexercise prediction equations.4 To explore the value of routinely measuring eCRF within the same individual, the present study compared the ability of 27 different nonexercise prediction equations to accurately assess CRF over time. Similar to previous research that compared prediction equations with a single direct measure of CRF,13 the R 2 and SEE values at both testing time points are comparable to those reported in the original publications (Table 1). In the analysis, the median ICC value for test 1 was 0.70 (range, 0.01–0.80) and for test 2 was 0.73 (range, 0.11–0.81), indicating many of the equations had at least “moderate” accuracy for assessing CRF. When examining changes over time, however, the ICC values were generally lower (median, 0.54; range, 0.06–0.63). When assessing changes to CRF, although the median was still within the range of “moderate” accuracy,47 no equation had “good” accuracy (ICC ≥0.75). Furthermore, of the 27 equations examined, 16 determined changes in eCRF values that were significantly different from the change in directly measured CRF.
The difference in the mean change values between eCRF and directly measured CRF for many of the equations was <1.0 mL·kg−1·min−1, suggesting they can reasonably identify changes to group means. However, the principle reason for designating CRF as a clinical vital sign is that it can improve risk stratification for individual patients, particularly those with low CRF.4 As such, the main determinant of whether eCRF has clinical utility should be the ability to accurately assess changes to an individual's CRF, not the ability to accurately determine group means. To better understand the ability of prediction equations to detect longitudinal changes within individuals, the analysis included classifying participants on the basis of directional changes to CRF. The Cohen's κ coefficients between directly measured CRF and eCRF for classifying directional changes ranged from “none” to “weak,”48 and the median percentage of participants correctly classified when using eCRF was only 56% (range, 39%–61%). Differences between equations existed on their ability to correctly identify directional changes, although no equation correctly classified >61% of participants. Furthermore, the time between tests significantly influenced the correct classification of participants. The median percentage of individuals correctly classified as having a directional increase in CRF was greater when the time between tests was ≤8 months (68%) compared with ≥2 years (34%). In contrast, the percentage correctly classified as having a directional decrease in CRF was lower with tests ≤8 months apart (7%) compared with ≥2 years (74%). These errors associated with classifying directional changes, along with recent research that found inaccuracies when using eCRF to classify individuals into fitness tertiles,13 show that nonexercise prediction equations are unable to accurately stratify patients according to risk and therefore eCRF may not be appropriate to include as a clinical vital sign.
Several factors influence the ability to detect directional changes in CRF. For example, the percentage of participants correctly classified as having an increase in CRF was higher for equations that included physical activity as a variable (median of 62% correct) compared with equations that did not include physical activity (median of 15% correct). This finding is not surprising given that physical activity is the major modifiable contributor to changes in CRF.4 Of note, the equations that included physical activity also had a greater percentage of individuals misclassified as having a directional increase in CRF. Many of the individuals in the cohort were initially tested before starting a physical fitness program, meaning physical activity levels were typically higher at the time of the subsequent test. Nonetheless, directly measured CRF did not increase for all participants. The misclassification of these participants when using eCRF is concerning given that individuals who do not have an increase in CRF, despite increasing physical activity, are still at a greater risk for early mortality.15 Thus, the limited ability of prediction equations to correctly identify these individuals who did not experience an increase in CRF suggests a reduced clinical utility for nonexercise prediction equations.
The limitations associated with current prediction equations are unlikely to be overcome with future iterations. A source of error in many of the current prediction equations is the use of self‐report scales as opposed to objective measures to determine variables such as physical activity. Including objective measures within a prediction equation may still result in significant error, however, as the relationship between variables such as physical activity and CRF is not universal and individuals can respond differently to the same training stimulus.50 This inability to account for individual variability also impacts other common equation variables. Current prediction equations assume a lower CRF for older individuals on the basis of the well‐known inverse relationship between CRF and age.46 However, participation in a physical fitness program can improve CRF despite increasing age. Although many prediction equations include other variables to account for this error, the individual variability surrounding each variable will still lead to inaccuracies and limit the clinical utility of nonexercise prediction equations.
The strengths of the present study are that 27 distinct prediction equations were compared over time within a single cohort, which included a diverse range of ages, fitness levels, and time between tests. However, there were limitations. Many of the individuals in the cohort were initially tested before starting a physical fitness program. Accordingly, physical activity levels were generally increased for the second test but may not reflect typical free‐living changes. The study also compared only prediction equations developed from treadmill testing, yet cycling is another common mode of exercise that often results in a different CRF value.38 Future research should compare prediction equations using cycling. Also, data from some of the participants in the present cohort were part of the data sets used to create 6 of the prediction equations.27, 28, 29, 32 In addition, the conversion of physical activity scales and conversion from metabolic equivalents during analysis may have increased the error associated with certain equations. However, in the present study, the correlations to directly measured CRF at each test time point were similar to many of those reported in the original publications. Furthermore, different results were not observed with the Whaley et al equations,32 which used the original physical activity coding (54% of participants correctly categorized by directional change in CRF).
In conclusion, changes to eCRF, as determined using nonexercise prediction equations, were significantly associated with changes in directly measured CRF. However, changes in eCRF values from most of the prediction equations were significantly different from the changes in directly measured CRF. Furthermore, all of the prediction equations had a low degree of accuracy when identifying even the directional change of CRF. These findings highlight the errors associated with nonexercise prediction equations, especially related to monitoring longitudinal changes, and suggest limited prognostic utility of eCRF within a clinical setting.
Sources of Funding
Support for this project was provided, in part, from an American Heart Association Award AIREA33930023 (Dr Harber, principal investigator).
Disclosures
None.
Acknowledgments
The authors would like to acknowledge the work of Dr Leroy “Bud” Getchell, who established the Adult Physical Fitness Program at Ball State University and began the data collection for the BALL ST (Ball State Adult Fitness Longitudinal Lifestyle Study) cohort. In addition, the authors thank Dr Lynn Witty for her assistance in providing clinical insights on data interpretation.
(J Am Heart Assoc. 2020;9:e015117 DOI: 10.1161/JAHA.119.015117.)
For Sources of Funding and Disclosures, see page 21.
References
- 1. Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DL, Kaminsky LA. Cardiorespiratory fitness and mortality in healthy men and women. J Am Coll Cardiol. 2018;72:2283–2292. [DOI] [PubMed] [Google Scholar]
- 2. Blair SN, Kohl HW III, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all‐cause mortality: a prospective study of healthy men and women. JAMA. 1989;262:2395–2401. [DOI] [PubMed] [Google Scholar]
- 3. Laukkanen JA, Lakka TA, Rauramaa R, Kuhanen R, Venalainen JM, Salonen R, Salonen JT. Cardiovascular fitness as a predictor of mortality in men. Arch Intern Med. 2001;161:825–831. [DOI] [PubMed] [Google Scholar]
- 4. Ross R, Blair SN, Arena R, Church TS, Despres JP, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, et al Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653–e699. [DOI] [PubMed] [Google Scholar]
- 5. Blair SN. Physical inactivity: the biggest public health problem of the 21st century. Br J Sports Med. 2009;43:1–2. [PubMed] [Google Scholar]
- 6. Artero EG, Jackson AS, Sui X, Lee DC, O'Connor DP, Lavie CJ, Church TS, Blair SN. Longitudinal algorithms to estimate cardiorespiratory fitness: associations with nonfatal cardiovascular disease and disease‐specific mortality. J Am Coll Cardiol. 2014;63:2289–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nes BM, Vatten LJ, Nauman J, Janszky I, Wisloff U. A simple nonexercise model of cardiorespiratory fitness predicts long‐term mortality. Med Sci Sports Exerc. 2014;46:1159–1165. [DOI] [PubMed] [Google Scholar]
- 8. Shigdel R, Dalen H, Sui X, Lavie CJ, Wisloff U, Ernstsen L. Cardiorespiratory fitness and the risk of first acute myocardial infarction: the HUNT Study. J Am Heart Assoc. 2019;8:e010293 DOI: 10.1161/JAHA.118.010293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang Y, Chen S, Zhang J, Zhang Y, Ernstsen L, Lavie CJ, Hooker SP, Chen Y, Sui X. Nonexercise estimated cardiorespiratory fitness and all‐cancer mortality: the NHANES III Study. Mayo Clin Proc. 2018;93:848–856. [DOI] [PubMed] [Google Scholar]
- 10. Wang Y, Chen S, Lavie CJ, Zhang J, Sui X. An overview of non‐exercise estimated cardiorespiratory fitness: estimation equations, cross‐validation and application. J Sci Sport Exerc. 2019;1:38–53. [Google Scholar]
- 11. Bouchard C, Daw EW, Rice T, Perusse L, Gagnon J, Province MA, Leon AS, Rao DC, Skinner JS, Wilmore JH. Familial resemblance for VO2max in the sedentary state: the HERITAGE family study. Med Sci Sports Exerc. 1998;30:252–258. [DOI] [PubMed] [Google Scholar]
- 12. Sallis JF, Saelens BE. Assessment of physical activity by self‐report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(suppl 2):1–14. [DOI] [PubMed] [Google Scholar]
- 13. Peterman JE, Whaley MH, Harber MP, Fleenor BS, Imboden MT, Myers J, Arena R, Kaminsky LA. Comparison of non‐exercise cardiorespiratory fitness prediction equations in apparently healthy adults. Eur J Prev Cardiol. 2019. DOI: 10.1177/2047487319881242. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 14. Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DL, Fleenor BS, Kaminsky LA. The association between the change in directly measured cardiorespiratory fitness across time and mortality risk. Prog Cardiovasc Dis. 2019;62:157–162. [DOI] [PubMed] [Google Scholar]
- 15. Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DA, Fleenor BS, Kaminsky LA. The influence of change in cardiorespiratory fitness with short‐term exercise training on mortality risk from the Ball State Adult Fitness Longitudinal Lifestyle Study. Mayo Clin Proc. 2019;94:1406–1414. [DOI] [PubMed] [Google Scholar]
- 16. Kokkinos P, Myers J, Faselis C, Panagiotakos DB, Doumas M, Pittaras A, Manolis A, Kokkinos JP, Karasik P, Greenberg M, et al Exercise capacity and mortality in older men. Circulation. 2010;122:790–797. [DOI] [PubMed] [Google Scholar]
- 17. Laukkanen JA, Zaccardi F, Khan H, Kurl S, Jae SY, Rauramaa R. Long‐term change in cardiorespiratory fitness and all‐cause mortality: a population‐based follow‐up study. Mayo Clin Proc. 2016;91:1183–1188. [DOI] [PubMed] [Google Scholar]
- 18. Lee DC, Sui X, Artero EG, Lee IM, Church TS, McAuley PA, Stanford FC, Kohl HW III, Blair SN. Long‐term effects of changes in cardiorespiratory fitness and body mass index on all‐cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation. 2011;124:2483–2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang P, Sui X, Hand GA, Hebert JR, Blair SN. Association of changes in fitness and body composition with cancer mortality in men. Med Sci Sports Exerc. 2014;46:1366–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jackson AS, Sui X, O'Connor DP, Church TS, Lee DC, Artero EG, Blair SN. Longitudinal cardiorespiratory fitness algorithms for clinical settings. Am J Prev Med. 2012;43:512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Paap D, Takken T. Reference values for cardiopulmonary exercise testing in healthy adults: a systematic review. Expert Rev Cardiovasc Ther. 2014;12:1439–1453. [DOI] [PubMed] [Google Scholar]
- 22. Maranhão Neto GdA, Lourenço PMC, Farinatti PdTV. Equações de predição da aptidão cardiorrespiratória sem testes de exercício e sua aplicabilidade em estudos epidemiológicos: uma revisão sistemática. Cad Saude Publica. 2004;20:48–56. [DOI] [PubMed] [Google Scholar]
- 23. Maranhao Neto GA, Farinatti PTV. Non‐exercise models for prediction of aerobic fitness and applicability on epidemiological studies: descriptive review and analysis of the studies. Rev Bras Med Esporte. 2003;9:304–314. [Google Scholar]
- 24. Riddle W, Younes M, Remmers J, deGroot W. Graphical analysis of patient performance in the pulmonary function laboratory. Proc Annu Symp Comput Appl Med Care. 1980;1:283–290. [Google Scholar]
- 25. Wasserman K, Hansen JE, Sue DY, Whipp BJ, Casaburi R. Principles of Exercise Testing and Interpretation. 2nd ed Malvern, PA: Lea & Febiger; 1994. [Google Scholar]
- 26. Jang T‐W, Park S‐G, Kim H‐R, Kim J‐M, Hong Y‐S, Kim B‐G. Estimation of maximal oxygen uptake without exercise testing in Korean healthy adult workers. Tohoku J Exp Med. 2012;227:313–319. [DOI] [PubMed] [Google Scholar]
- 27. Baynard T, Arena RA, Myers J, Kaminsky LA. The role of body habitus in predicting cardiorespiratory fitness: the FRIEND registry. Int J Sports Med. 2016;37:863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Myers J, Kaminsky LA, Lima R, Christle JW, Ashley E, Arena R. A reference equation for normal standards for VO2 max: analysis from the Fitness Registry and the Importance of Exercise National Database (FRIEND Registry). Prog Cardiovasc Dis. 2017;60:21–29. [DOI] [PubMed] [Google Scholar]
- 29. de Souza ESCG, Kaminsky LA, Arena R, Christle JW, Araujo CGS, Lima RM, Ashley EA, Myers J. A reference equation for maximal aerobic power for treadmill and cycle ergometer exercise testing: analysis from the FRIEND registry. Eur J Prev Cardiol. 2018;25:742–750. [DOI] [PubMed] [Google Scholar]
- 30. Jackson AS, Blair SN, Mahar MT, Wier LT, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22:863–870. [DOI] [PubMed] [Google Scholar]
- 31. Heil DP, Freedson PS, Ahlquist LE, Price J, Rippe JM. Nonexercise regression models to estimate peak oxygen consumption. Med Sci Sports Exerc. 1995;27:599–606. [PubMed] [Google Scholar]
- 32. Whaley MH, Kaminsky LA, Dwyer GB, Getchell LH. Failure of predicted VO2peak to discriminate physical fitness in epidemiological studies. Med Sci Sports Exerc. 1995;27:85–91. [PubMed] [Google Scholar]
- 33. Matthews CE, Heil DP, Freedson PS, Pastides H. Classification of cardiorespiratory fitness without exercise testing. Med Sci Sports Exerc. 1999;31:486–493. [DOI] [PubMed] [Google Scholar]
- 34. Jurca R, Jackson AS, LaMonte MJ, Morrow JR Jr, Blair SN, Wareham NJ, Haskell WL, van Mechelen W, Church TS, Jakicic JM, et al Assessing cardiorespiratory fitness without performing exercise testing. Am J Prev Med. 2005;29:185–193. [DOI] [PubMed] [Google Scholar]
- 35. Wier LT, Jackson AS, Ayers GW, Arenare B. Nonexercise models for estimating VO2max with waist girth, percent fat, or BMI. Med Sci Sports Exerc. 2006;38:555–561. [DOI] [PubMed] [Google Scholar]
- 36. Nes BM, Janszky I, Vatten LJ, Nilsen TI, Aspenes ST, Wisloff U. Estimating V.O 2peak from a nonexercise prediction model: the HUNT Study, Norway. Med Sci Sports Exerc. 2011;43:2024–2030. [DOI] [PubMed] [Google Scholar]
- 37. Cáceres JM, Ulbrich AZ, Panigas TF, Benetti M. Equações de predição da aptidão cardiorrespiratória de adultos sem teste de exercícios físicos. Rev Bras Cineantropom Desempenho Hum. 2012;14:287–295. [Google Scholar]
- 38. Riebe D, Ehrman JK, Liguori G, Magal M. ACSM's Guidelines for Exercise Testing and Prescription. 10th ed Philadelphia, PA: Wolters Kluwer; 2018. [Google Scholar]
- 39. Siri WE. Body Composition From Fluid Spaces and Density: Analysis of Methods in Technologies for Measuring Body Composition. Washington, DC: National Academy of Science, National Research Council; 1961. [Google Scholar]
- 40. Ross RM, Jackson AS. Exercise Concepts, Calculations, and Computer Applications. Carmel, IN: Benchmark Press; 1990. [Google Scholar]
- 41. Wier LT, Ayers GW, Jackson AS, Rossum AC, Poston WS, Foreyt JP. Determining the amount of physical activity needed for long‐term weight control. Int J Obes Relat Metab Disord. 2001;25:613–621. [DOI] [PubMed] [Google Scholar]
- 42. Kaminsky LA, Whaley MH. Evaluation of a new standardized ramp protocol: the BSU/Bruce Ramp protocol. J Cardiopulm Rehabil. 1998;18:438–444. [DOI] [PubMed] [Google Scholar]
- 43. Benjamini Y, Hochberg Y. Controlling the false discovery rate—a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological). 1995;57:289–300. [Google Scholar]
- 44. Pandey A, Swift DL, McGuire DK, Ayers CR, Neeland IJ, Blair SN, Johannsen N, Earnest CP, Berry JD, Church TS. Metabolic effects of exercise training among fitness‐nonresponsive patients with type 2 diabetes: the HART‐D Study. Diabetes Care. 2015;38:1494–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Agresti A. Categorical Data Analysis. 3rd ed Hoboken, NJ: John Wiley & Sons Inc; 2013. [Google Scholar]
- 46. Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing: data from the Fitness Registry and the Importance of Exercise National Database. Mayo Clin Proc. 2015;90:1515–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276–282. [PMC free article] [PubMed] [Google Scholar]
- 49. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic; 1988. [Google Scholar]
- 50. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP; American College of Sports Medicine . American College of Sports Medicine position stand: quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. [DOI] [PubMed] [Google Scholar]


