Abstract
Background
Should all out‐of‐hospital cardiac arrest (OHCA) patients be directly transported to cardiac arrest centers (CACs) remains under debate. Our study evaluated the impacts of different transport time and destination hospital on the outcomes of OHCA patients.
Methods and Results
Data were collected from 6655 OHCA patients recorded in the regional prospective OHCA registry database of Taoyuan City, Taiwan, between January 2012 and December 2016. Patients were matched on propensity score, which left 5156 patients, 2578 each in the CAC and non‐CAC groups. Transport time was dichotomized into <8 and ≥8 minutes. The relations between the transport time to CACs and good neurological outcome at discharge and survival to discharge were investigated. Of the 5156 patients, 4215 (81.7%) presented with nonshockable rhythms and 941 (18.3%) presented with shockable rhythms. Regardless of transport time, transportation to a CAC increased the likelihoods of survival to discharge (<8 minutes: adjusted odds ratio [aOR], 1.95; 95% CI, 1.11–3.41; ≥8 minutes: aOR, 1.92; 95% CI, 1.25–2.94) and good neurological outcome at discharge (<8 minutes: aOR, 2.70; 95% CI, 1.40–5.22; ≥8 minutes: aOR, 2.20; 95% CI, 1.29–3.75) in OHCA patients with shockable rhythms but not in patients with nonshockable rhythms.
Conclusions
OHCA patients with shockable rhythms transported to CACs demonstrated higher probabilities of survival to discharge and a good neurological outcome at discharge. Direct ambulance delivery to CACs should thus be considered, particularly when OHCA patients present with shockable rhythms.
Keywords: cardiac arrest center, initial rhythm, neurological outcome, out‐of‐hospital cardiac arrest, transport time
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care
Nonstandard Abbreviations and Acronyms
- ALS
advanced life support
- aOR
adjusted odds ratio
- BLS
basic life support
- CAC
cardiac arrest center
- CPC
Cerebral Performance Category
- CPR
cardiopulmonary resuscitation
- DNR
do not resuscitate
- EMS
emergency medical service
- EMT
emergency medical technician
- GAM
generalized additive model
- IQR
interquartile range
- OHCA
out‐of‐hospital cardiac arrest
- OR
odds ratio
- PSM
propensity score matching
- ROSC
return of spontaneous circulation
- SMD
standardized mean difference
Clinical Perspective
What Is New?
To our knowledge, this is the first study to evaluate the impact of transport time to treatment center and type of treatment center on the prognosis of out‐of‐hospital cardiac arrest patients with shockable and nonshockable rhythms using a large database.
Not all out‐of‐hospital cardiac arrest patients would benefit from better prognosis when transported to a cardiac arrest center.
Transportation to a cardiac arrest center significantly increased the likelihood of survival to discharge and a good neurological outcome at discharge in out‐of‐hospital cardiac arrest patients with shockable rhythms but not in those with nonshockable rhythms.
What Are the Clinical Implications?
These findings may serve as a reference for emergency medical service in deciding whether to bypass the closest hospital to a cardiac arrest center to increase the probability of a better outcome in out‐of‐hospital cardiac arrest patients.
Out‐of‐hospital cardiac arrest (OHCA) remains a major public health problem with a low survival rate. The overall survival rate varies greatly worldwide and ranges from 2% in Asia to 9% in Europe.1 Moreover, the survival rate of OHCA patients differs between those with shockable and nonshockable initial rhythms, with the former having a higher survival rate.2
Post–cardiac arrest care is the fifth link of the Chain of Survival to encourage the preservation of the brain and heart functions of cardiac arrest survivors.3 The implementation of post–cardiac arrest care treatment protocol, including percutaneous coronary intervention and targeted temperature management, markedly improved rates of survival to discharge with good neurological recovery in OHCA patients4, 5 and was accordingly included in later post–cardiac arrest care guidelines.6
Because of the wide variation among hospitals in the resources for optimum post–cardiac arrest care, it has been suggested that OHCA patients be transported to a cardiac arrest center (CAC) for post–cardiac arrest care7, 8 for a higher likelihood of survival to discharge and good neurological outcomes (Cerebral Performance Category [CPC] of 1 or 2).9, 10 Furthermore, transport time was not found to be associated with survival to discharge or good neurological outcome, affirming that it is safe to bypass the nearest hospitals to directly transport OHCA patients to CACs.11 Even when transporting patients directly to CACs increased the bypass time by >20 minutes, the odds of survival to discharge and good neurological outcome were still higher than those transported to non‐CACs in a shorter time.12
However, 2 important questions remain: Is there an ideal transport time for OHCA patients? Moreover, should all OHCA patients be transported to CACs? A previous study has suggested triaging patients according to the initial cardiac rhythm because of major differences in prognosis; however, a limited number of patients were included.13 The objective of this study was to evaluate the relationship between transport time to CACs and the survival and neurological outcomes by shockable rhythms in a large series of patients.
Methods
Study Design and Setting
The data that support the findings of this study are available from the first author on reasonable request (E‐mail: rainccy217@gmail.com). This was a retrospective cohort study using data from the OHCA database in Taoyuan City, Taiwan, between January 2012 and December 2016. The OHCA database in Taoyuan City is a regional prospective registry database to which all emergency departments within the city must report.14
Taoyuan City is the fourth‐largest metropolitan area, made up of cities and rural areas in Taiwan. There are 13 responsibility hospitals of first aid in Taoyuan. In the emergency medical service (EMS) system of Taoyuan City, the duty emergency medical technicians (EMTs) are either of an intermediate or a paramedic level. An EMT‐paramedic can perform intubation and the administration of epinephrine and amiodarone intravenous injection or intraosseous infusion, whereas an EMT‐intermediate can perform laryngeal mask airway insertion and intravenous injection or intraosseous infusion. Mechanical cardiopulmonary resuscitation (CPR) is provided to the patient continually until arriving at the closest hospital. In Taoyuan City, all EMS followed the same rescue service principle of transporting patients to the hospital in the vicinity of the location of arrest.
Selection of Participants
Patients with OHCA >18 years of age and transported by EMS were included in this study. Patients were excluded if they had a do not resuscitate order, were pronounced dead at the scene, experienced cardiac arrest attributable to an obvious noncardiac cause (ie, trauma, intoxication, and drowning), were pregnant, had missing data on transport time or outcomes, or transport time increased because of a medical problem (ie, cardiac arrest during ambulance transport).
Data Collection
Data collection was based on the Utstein template.15 Data were collected from the EMS running sheet and by review of hospital medical records. Information obtained included age, sex, location of arrest, witness status (witnessed arrest or not), provision of bystander CPR (yes or no), prehospital return of spontaneous circulation, number of EMTs dispatched, level of EMT certification, type of life support provided, EMS parameters (response time, scene time interval, and transport time), neurological outcome by CPC Scale, destination hospital's capability (CAC or not), and initial rhythm (shockable or not).
For EMS parameters, the response time was the time from an emergency call to EMS arrival on the scene. The scene time interval was the time EMS remained at the scene. The transport time was the interval between EMS leaving the scene and arrival at a hospital.
To be defined as a CAC in our study, a hospital had to meet all of the following criteria: (a) certification by the World Health Organization–Health Promoting Hospital network between January 2012 and December 2016, (b) high case volume of >100 OHCA patients admitted per year,16 (c) had a cardiovascular system emergency consulting team, (d) the capacity to perform 24/7 percutaneous coronary intervention, (e) a targeted temperature management protocol used in both the emergency department and intensive care unit,9 and (f) had the capability to perform extracorporeal membrane oxygenation in the intensive care unit.17 A hospital was only considered a CAC during and after the year it received its Health Promoting Hospital certification. All CACs included in the study had preestablished cardiac arrest management protocols for percutaneous coronary intervention, extracorporeal membrane oxygenation, and targeted temperature management developed in accordance with American Heart Association guidelines.18, 19
To limit potential information and selection bias, data were collected from the same database using the same template and patients were matched on propensity score. Definitions for CAC and good neurological outcome were clearly defined. Also, all EMS followed the same rescue service principle of transporting patients to the medical care institution in the vicinity of the location of arrest regardless of the patient's characteristics; this reduced the possible bias in patient selection.
Outcome Measures
The primary outcome was good neurological outcome at hospital discharge, defined by a CPC grade of 1 (good cerebral performance and mild or no neurological disability) or 2 (moderate cerebral disability and conscious and able to function independently). The secondary outcome was survival to hospital discharge.
Statistical Analysis
Categorical variables (eg, sex, arrest location, and witness status) were presented as numbers and percentages and were compared using a χ2 test. Continuous variables (eg, age and EMS parameters) were presented as mean and SD or median and interquartile range, as appropriate. The Student t test and Mann‐Whitney U test were used for normally and nonnormally distributed continuous variables, respectively.
To reduce selection bias and approximate a randomized scenario, the propensity score matching analysis was used to adjust the potential confounding factors, where it was trying to make equal probability of transporting to CAC and non‐CAC. We selected the covariates according to the confounders and related outcomes.20, 21 Covariates that were related to the outcome, including age, sex, location of arrest, witnessed arrest, bystander CPR, number of EMTs, EMT certification level, prehospital return of spontaneous circulation, initial rhythms, and type of life support given, were put into the model to calculate the propensity score. A 1:1 matching without replacement was conducted. The algorithm used was 8 to 1 digit match, proceeding sequentially to the lowest digit match on propensity score. After 1:1 propensity score matching, logistic regression models were built up to show the relationship between EMS time and survival to discharge or good neurological outcome at discharge. The odds ratio (OR) and adjusted OR (aOR) were reported with 95% CI.
Meanwhile, we tried to find an optimal cutoff for transport time by means of generalized additive model. The transport time value for which there was an average probability of an OHCA patient having a good CPC was taken as the cut point, which in our study was 7.5 minutes (Figure 1). Consequently, the transport time was dichotomized into <8 or ≥8 minutes for subsequent analysis. This cutoff and transporting to CAC and non‐CAC would be a combination factor in the logistic regression model. The restricted cubic spline smooth function with 3 knots was used to visualize the relationship between the probability of a good neurological outcome and transport time to CAC. The data were analyzed using SPSS software (IBM SPSS Statistics for Windows, version 20.0; IBM Corp, NY) and Stata software for the restricted cubic spline function (version 13.0; StataCorp, College Station, TX), R with generalized additive model package, and SAS 9.4 for propensity score matching. P<0.05 was considered to be statistically significant.
Figure 1. Generalized additive model (GAM) plots showing the relationship between probability of having good Cerebral Performance Category (CPC) score and transport time in all out‐of‐hospital cardiac arrest patients.
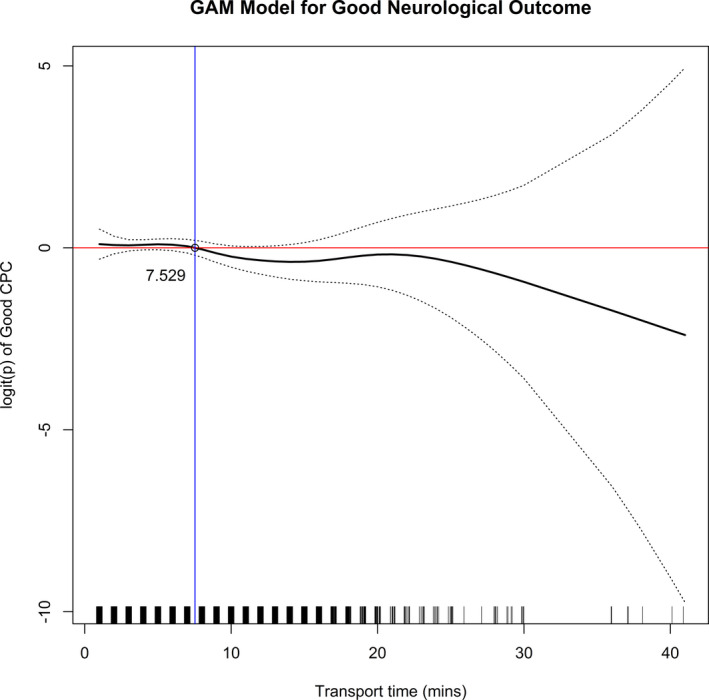
The cut point obtained for the transport time was based on the relationship between transport time and probability of having a good CPC. The transport time for which there was an average probability of having a good CPC was 7.5 minutes.
Ethical Approval
This study was reviewed and approved by the Institutional Review Board of Linkou Chang Gung Memorial Hospital (201701755B0) with a waiver of informed consent.
Results
Characteristics of Study Subjects
Among the 11 080 OHCA patients, 6655 who met the eligibility criteria were included in the present study (Figure 2). Baseline characteristics according to destination hospital's capability before and after propensity score matching are presented in Table 1. Among the 6655 cases, 2616 (39.3%) and 4039 (60.7%) were transported to non‐CACs and CACs, respectively. The non‐CAC and CAC groups differed significantly in age (69.0 versus 67.4 years old; P<0.001), rate of witnessed arrest (41.7% versus 44.5%; P=0.03), rate of bystander CPR (28.7% versus 32.2%; P=0.003), percentage of achieving prehospital return of spontaneous circulation (4.3% versus 5.5%; P=0.02), and percentage of patient with shockable rhythms (21.4% versus 25.8%; P <0.001). After propensity score 1:1 matching, 5156 patients were left, with 2578 patients each in the non‐CAC and CAC groups. Of the 5156 patients, 4215 (81.7%) presented with nonshockable rhythms and 941 (18.3%) presented with shockable rhythms. No statistically significant baseline characteristics between the non‐CAC and CAC groups were found.
Figure 2. Flow diagram of patient enrollment.
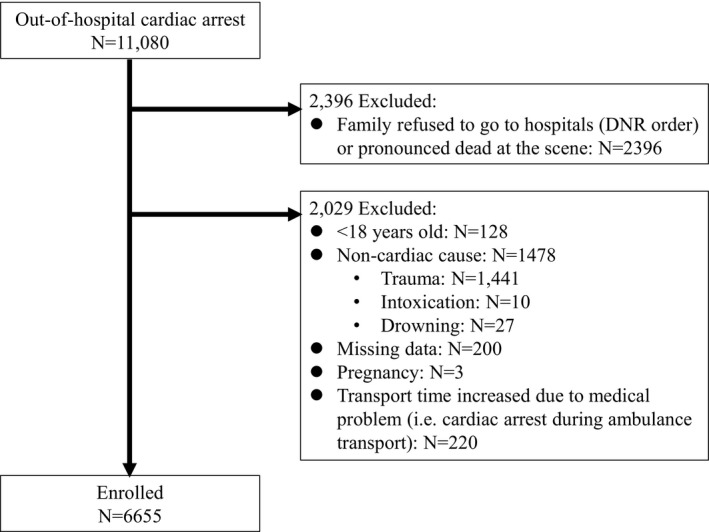
DNR indicates do not resuscitate.
Table 1.
Baseline Characteristics of the Study Population Before and After PSM Analysis
| Characteristics | Before PSM (N=6655) | After PSM (N=5156) | |||||
|---|---|---|---|---|---|---|---|
| Non‐CAC (N=2616) | CAC (N=4039) | P Value | Non‐CAC (N=2578) | CAC (N=2578) | P Value | SMDa | |
| Age, mean (SD), yb | 69.0 (17.1) | 67.4 (17.3) | <0.001c | 69.3 (17.0) | 69.4 (16.9) | 0.83 | −0.006 |
| <40 | 150 (5.7) | 255 (6.3) | 0.008 | 142 (5.5) | 130 (5.0) | 0.74 | 0.02 |
| 40–49 | 228 (8.7) | 423 (10.5) | 211 (8.2) | 221 (8.6) | −0.01 | ||
| 50–59 | 364 (13.9) | 629 (15.6) | 356 (13.8) | 375 (14.5) | −0.02 | ||
| 60–69 | 454 (17.4) | 723 (17.9) | 449 (17.4) | 436 (16.9) | 0.01 | ||
| 70–79 | 509 (19.5) | 730 (18.1) | 507 (19.7) | 477 (18.5) | 0.03 | ||
| ≥80 | 911 (34.8) | 1279 (31.7) | 913 (35.4) | 939 (36.4) | −0.02 | ||
| Sexb | |||||||
| Women | 819 (31.3) | 1195 (29.6) | 0.14 | 821 (31.8) | 796 (30.9) | 0.45 | 0.02 |
| Men | 1797 (68.7) | 2844 (70.4) | 1757 (68.2) | 1782 (69.1) | −0.02 | ||
| Location of arrestb | |||||||
| Public | 492 (18.8) | 775 (19.2) | 0.70 | 491 (19.0) | 465 (18.0) | 0.35 | 0.03 |
| Residential | 2124 (81.2) | 3264 (80.8) | 2087 (81.0) | 2113 (82.0) | −0.03 | ||
| Witnessed arrestb | |||||||
| Yes | 1092 (41.7) | 1799 (44.5) | 0.03c | 1099 (42.6) | 1105 (42.9) | 0.50 | −0.006 |
| No | 1524 (58.3) | 2240 (55.5) | 1479 (57.4) | 1473 (57.1) | 0.006 | ||
| Bystander CPRb | |||||||
| Yes | 752 (28.7) | 1299 (32.2) | 0.003c | 759 (29.4) | 737 (28.6) | 0.52 | 0.02 |
| No | 1864 (71.3) | 2740 (67.8) | 1819 (70.6) | 1841 (71.4) | −0.02 | ||
| No. of EMTsb | |||||||
| 2 | 1562 (59.7) | 2385 (59.0) | 0.53 | 1570 (60.9) | 1604 (62.2) | 0.62 | −0.03 |
| 3–4 | 1011 (38.6) | 1573 (38.9) | 971 (37.7) | 937 (36.3) | 0.03 | ||
| 5–6 | 43 (1.6) | 81 (2.0) | 37 (1.4) | 37 (1.4) | 0.00 | ||
| EMT certification levelb | |||||||
| Intermediate | 1422 (54.4) | 2194 (54.3) | 0.98 | 1414 (54.8) | 1465 (56.8) | 0.15 | −0.04 |
| Paramedic | 1194 (45.6) | 1845 (45.7) | 1164 (45.2) | 1113 (43.2) | 0.04 | ||
| Type of life supportb | |||||||
| BLS | 1457 (55.7) | 2275 (56.3) | 0.61 | 1448 (56.2) | 1498 (58.1) | 0.16 | −0.04 |
| ALS | 1159 (44.3) | 1764 (43.7) | 1130 (43.8) | 1080 (41.9) | 0.04 | ||
| Prehospital ROSCb | |||||||
| Yes | 112 (4.3) | 224 (5.5) | 0.02c | 117 (4.5) | 116 (4.5) | 0.95 | 0.002 |
| No | 2504 (95.7) | 3815 (94.5) | 2461 (95.5) | 2462 (95.5) | −0.002 | ||
| AEDb | |||||||
| Shockable rhythm | 561 (21.4) | 1044 (25.8) | <0.001c | 523 (20.3) | 533 (20.6) | 0.54 | −0.007 |
| Nonshockable rhythm | 2055 (78.6) | 2995 (74.2) | 2055 (79.7) | 2045 (79.4) | 0.007 | ||
| EMS parameter | |||||||
| Response time, median (IQR), min | 7 (5–9) | 7 (5–9) | 0.01c | 7 (5–9) | 7 (6–9) | 0.006 | |
| Scene time interval, median (IQR), min | 11 (9–14) | 12 (9–15) | 0.01c | 11 (9–14) | 11 (9–14) | 0.01 | |
| Transport time, median (IQR), min | 5 (3–7) | 5 (3–8) | <0.001c | 5 (3–7) | 5 (3–7) | <0.001c | |
| Transport distance, mean (SD), km | 5.3 (2.8) | 6.3 (5.7) | <0.001c | 5.9 (4.1) | 6.1 (5.3) | 0.47 | |
| CPC | |||||||
| 1 | 46 (1.8) | 129 (3.2) | <0.001c | 46 (1.8) | 59 (2.3) | 0.002c | |
| 2 | 21 (0.8) | 68 (1.7) | 19 (0.7) | 35 (1.4) | |||
| 3 | 22 (0.8) | 75 (1.9) | 21 (0.8) | 41 (1.6) | |||
| 4 | 41 (1.6) | 107 (2.6) | 40 (1.6) | 57 (2.2) | |||
| 5 | 2486 (95.0) | 3660 (90.6) | 2452 (95.1) | 2386 (92.6) | |||
Values are expressed as number (percentage) unless otherwise specified. AED indicates automated external defibrillator; ALS, advanced life support; BLS, basic life support; CAC, cardiac arrest center; CPC, Cerebral Performance Category; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; EMT, emergency medical technician; IQR, interquartile range (25%–75%); PSM, propensity score matching; ROSC, return of spontaneous circulation; and SMD, standardized mean difference.
For assessing balance after matching.
Propensity score adjusted variable.
P<0.05.
Main Results
Transporting patients with nonshockable rhythms to a CAC in <8 minutes increased the probability of survival to discharge (aOR, 1.41; 95% CI, 1.01–1.99) but not a good neurological outcome compared with transporting such patients to a non‐CAC in <8 minutes. On the other hand, patients with shockable rhythms transported to a CAC in <8 minutes were significantly more likely to survive to discharge (aOR, 1.95; 95% CI, 1.11–3.41) and have a good neurological outcome (aOR, 2.70; 95% CI, 1.40–5.22). In addition, transporting patients with shockable rhythms to a CAC in ≥8 minutes also proved to significantly increase the probabilities of survival to discharge (aOR, 1.92; 95% CI, 1.25–2.94) and a good neurological outcome (aOR, 2.20; 95% CI, 1.29–3.75) compared with transporting such patients to a non‐CAC in <8 minutes (Table 2).
Table 2.
Result of Logistic Regression Analysis of Survival to Discharge and Good Neurological Outcome at Discharge by EMS Parameter According to Initial Rhythms After PSM
| Variables | Survival to Discharge | Good Neurological Outcome | ||||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | aOR (95% CI) | P Value | OR (95% CI) | P Value | aOR (95% CI) | P Value | |
| Nonshockable rhythm after PSM (N=4215) | ||||||||
| Response time | 0.92 (0.86–0.98) | 0.003a | 0.92 (0.87–0.97) | 0.003a | 0.83 (0.76–0.92) | <0.001a | 0.84 (0.76–0.93) | 0.001a |
| Scene time interval | 0.99 (0.96–1.03) | 0.63 | 0.99 (0.96–1.02) | 0.56 | 0.97 (0.91–1.02) | 0.20 | 0.96 (0.91–1.02) | 0.16 |
| Transport time | ||||||||
| To non‐CAC <8 min | Reference group | Reference group | Reference group | Reference group | ||||
| To non‐CAC ≥8 min | 0.93 (0.53–1.62) | 0.79 | 0.96 (0.55–1.67) | 0.88 | 0.81 (0.36–1.84) | 0.62 | 0.83 (0.36–1.89) | 0.65 |
| To CAC <8 min | 1.38 (0.98–1.94) | 0.06 | 1.41 (1.01–1.99) | <0.05a | 1.02 (0.61–1.69) | 0.95 | 1.07 (0.64–1.78) | 0.81 |
| To CAC ≥8 min | 1.14 (0.74–1.76) | 0.56 | 1.19 (0.77–1.85) | 0.44 | 0.51 (0.22–1.15) | 0.10 | 0.53 (0.23–1.20) | 0.13 |
| Shockable rhythm after PSM (N=941) | ||||||||
| Response time | 0.92 (0.86–0.98) | 0.02a | 0.92 (0.86–0.99) | 0.03a | 0.94 (0.86–1.02) | 0.11 | 0.93 (0.85–1.01) | 0.10 |
| Scene time interval | 1.01 (0.97–1.05) | 0.78 | 0.99 (0.95–1.04) | 0.80 | 0.99 (0.94–1.04) | 0.74 | 0.98 (0.93–1.03) | 0.46 |
| Transport time | ||||||||
| To non‐CAC <8 min | Reference group | Reference group | Reference group | Reference group | ||||
| To non‐CAC ≥8 min | 0.40 (0.12–1.32) | 0.13 | 0.45 (0.13–1.49) | 0.19 | 0.28 (0.03–2.32) | 0.34 | 0.54 (0.12–2.35) | 0.41 |
| To CAC <8 min | 1.92 (1.26–2.94) | 0.002a | 1.95 (1.11–3.41) | 0.02a | 2.50 (1.31–4.80) | 0.006a | 2.70 (1.40–5.22) | 0.003a |
| To CAC ≥8 min | 1.78 (1.03–3.10) | 0.04a | 1.92 (1.25–2.94) | 0.003a | 2.18 (1.28–3.71) | 0.004a | 2.20 (1.29–3.75) | 0.004a |
aOR indicates adjusted OR; CAC, cardiac arrest center; EMS, emergency medical service; OR, odds ratio; and PSM, propensity score matching.
P<0.05.
As transporting patients with shockable rhythms to a CAC in ≥8 minutes was associated with a higher likelihood of good neurological outcome, it was critical to know how the probability of good neurological outcome changed with a longer transport time. Figure 3 shows the association between transport time to CAC and the probability of a good neurological outcome at discharge. The probability of a good neurological outcome at discharge decreased to 10.4% (the good CPC rate of patients with shockable rhythms) if the transport time to CAC was 14.4 minutes and 4.0% (the good CPC rate of total patients) if the transport time was 36.1 minutes.
Figure 3. Probability of good neurological outcome vs transport time from a restricted cubic spline model.
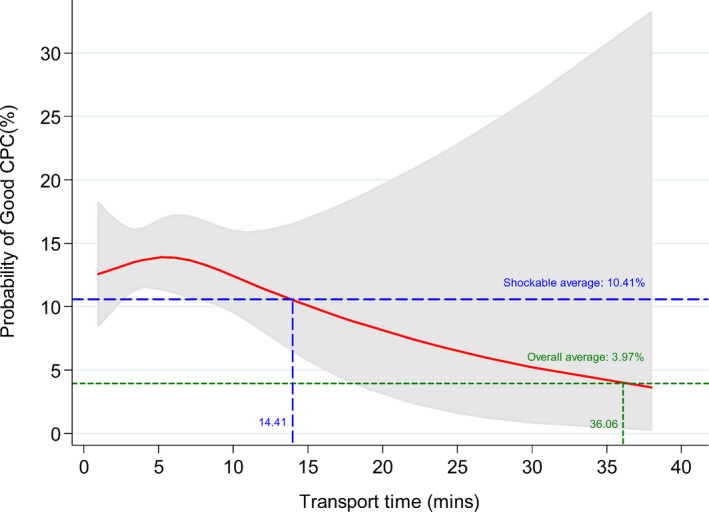
CPC indicates Cerebral Performance Category.
Discussion
This study sought to assess the relationship between transport time to CACs and outcomes in adult OHCA patients with nonshockable or shockable initial rhythms. Overall, we found that transport to CAC was associated with better probabilities of survival to discharge and good neurological outcomes at discharge in OHCA patients with shockable rhythms but not in those with nonshockable rhythms.
To address whether transport to CAC would be beneficial to the outcomes of all OHCA patients, we completed a head‐to‐head comparison of the adult OHCA patients transported to a non‐CAC and CAC in our study. After propensity score 1:1 matching, our findings showed that OHCA patients transported to a CAC had a higher rate of good neurological outcome at discharge (CPC 1 and 2) compared with those transported to a non‐CAC (3.7% versus 2.5%); this finding is in line with those of a previous study.22 This suggests that the post–cardiac arrest care that a CAC offers plays a significant role in the probability of a good neurological outcome.23 Our study as well as previous studies9, 10 have all defined CACs on the basis of their availability and type of post–cardiac arrest care. However, besides the post–cardiac arrest care that a CAC offers, it also requires an integrated and multidisciplinary approach to improve OHCA outcomes, which future research should pay attention to.
For the transport time to CAC, a previous study found that OHCA patients transported to a CAC demonstrated better rates of survival (OR, 3.19; 95% CI, 1.64–6.22) and good neurological outcomes (OR, 2.34; 95% CI, 1.43–3.85) than those transported to a non‐CAC, even though the transport time to a CAC was 20 minutes longer.12 This implies that increasing the time spent on direct transport to CACs is safe and beneficial. However, this poses another challenge to optimal EMS operation: such a bypass may remove an EMS unit from service for a longer time.24 To determine the optimal transport time associated with favorable outcomes, our present study proposed a cutoff point for transport time (ie, <8 minutes) using generalized additive model. Our results showed that transporting OHCA patients with shockable rhythms to CACs proved to be associated with better odds of survival to discharge and a good neurological outcome at discharge regardless of transport time; this relation did not hold for patients with nonshockable rhythms. However, as depicted in Figure 3, the probability of good neurological outcome decreased over transport time. More specifically, it decreased to <10% when the transport time exceeded 14.4 minutes (notably, 10% was also the proportion of good CPC of the OHCA patients with shockable rhythms group of our study) and <4.0% when the transport time exceeded 36 minutes (notably, 4% was the proportion of good CPC of our total study population). Therefore, our results for transport time may be of interest to and may serve as a reference for EMS in deciding whether to bypass the nearest hospital to a CAC to increase the probability of a better OHCA outcome.
In addition, our study revealed that the other EMS parameter (ie, response time) had a negative association with survival to discharge and good neurological outcome at discharge in OHCA patients with nonshockable rhythms (Table 2). A previous study conducted by Herlitz et al25 found that longer response time decreased the odds of survival in OHCA patients with nonshockable rhythms. The authors stated that it may be explained by shorter response time enables an earlier start of good CPR and life support provision, thereby increasing the chance of survival. In addition, Kim et al26 also reported that delayed response time with longer scene time interval decreased the odds of survival to discharge. Although a longer scene time interval decreased the likelihood of survival, it is important that EMTs do not compromise the time for the essential process of EMS, such as CPR duration and life support provision at scene.
Limitations
This study was limited by its retrospective nature. Information was lacking about the underlying diseases of the study population. Statistical bias may have been introduced by the limited local population and selection bias. Other hospital characteristics in addition to the designation of CAC that might impact OHCA outcomes were not collected and analyzed. Moreover, the present study's results may not be generalized to other countries because of the difference in geographical location. Although all OHCA patients were transported to the nearest hospital, the transport time could be influenced by distance, geographic location, and traffic. Despite some limitations, our study addressed which OHCA patient subgroups (ie, patients with either shockable or nonshockable initial rhythms) may benefit more from being treated in CACs and the effect of transport time to CACs on survival and neurological outcomes. Our results encourage the consideration of direct ambulance delivery to CACs, especially when the OHCA patient presents with shockable rhythms. To be sure, further controlled study is needed to confirm these findings.
Conclusions
Transportation to a CAC, regardless of time spent en route, was associated with higher probabilities of survival to discharge and good neurological outcome at discharge in OHCA patients with shockable initial rhythms but not in those with nonshockable initial rhythms. Transportation to a CAC in a shorter time solely increased the likelihood of survival to discharge in OHCA patients with nonshockable rhythms.
Sources of Funding
None.
Disclosures
None.
Acknowledgments
We would like to thank Editage (http://www.editage.com) for English‐language editing. A preliminary version of this article is the Master Thesis of the first author, Cheng‐Yu Chien, at the National Taiwan University (2019). We thank Dr Wen‐Chu Chiang and Dr Kuan‐Fu Chen for their instructions and advice.
(J Am Heart Assoc. 2020;9:e015544 DOI: 10.1161/JAHA.119.015544.)
For Sources of Funding and Disclosures, see page 9.
References
- 1. Berdowski J, Berg RA, Tijssen JGP, Koster RW. Global incidences of out‐of‐hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. [DOI] [PubMed] [Google Scholar]
- 2. Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in‐hospital cardiac arrest. Crit Care Med. 2010;38:101–108. [DOI] [PubMed] [Google Scholar]
- 3. Nolan J. European resuscitation council guidelines for resuscitation 2005: section 1: introduction. Resuscitation. 2005;67:S3–S6. [DOI] [PubMed] [Google Scholar]
- 4. Sunde K, Pytte M, Jacobsen D, Mangschau A, Jensen LP, Smedsrud C, Draegni T, Steen PA. Implementation of a standardised treatment protocol for post resuscitation care after out‐of‐hospital cardiac arrest. Resuscitation. 2007;73:29–39. [DOI] [PubMed] [Google Scholar]
- 5. Lund‐Kordahl I, Olasveengen TM, Lorem T, Samdal M, Wik L, Sunde K. Improving outcome after out‐of‐hospital cardiac arrest by strengthening weak links of the local Chain of Survival; quality of advanced life support and post‐resuscitation care. Resuscitation. 2010;81:422–426. [DOI] [PubMed] [Google Scholar]
- 6. Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VR, Deakin CD, Bottiger BW, Friberg H, Sunde K, Sandroni C. European Resuscitation Council and European Society of Intensive Care Medicine 2015 guidelines for post‐resuscitation care. Intensive Care Med. 2015;41:2039–2056. [DOI] [PubMed] [Google Scholar]
- 7. Bhanji F, Finn JC, Lockey A, Monsieurs K, Frengley R, Iwami T, Lang E, Ma MH, Mancini ME, McNeil MA, et al. Part 8: education, implementation, and teams: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S242–S268. [DOI] [PubMed] [Google Scholar]
- 8. Girotra S, Chan PS, Bradley SM. Post‐resuscitation care following out‐of‐hospital and in‐hospital cardiac arrest. Heart. 2015;101:1943–1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lipe D, Giwa A, Caputo ND, Gupta N, Addison J, Cournoyer A. Do out‐of‐hospital cardiac arrest patients have increased chances of survival when transported to a cardiac resuscitation center? J Am Heart Assoc. 2018;7:e011079 DOI: 10.1161/JAHA.118.011079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yeung J, Matsuyama T, Bray J, Reynolds J, Skrifvars MB. Does care at a cardiac arrest center improve outcome after out‐of‐hospital cardiac arrest? A systematic review. Resuscitation. 2019;137:102–115. [DOI] [PubMed] [Google Scholar]
- 11. Geri G, Gilgan J, Wu W, Vijendira S, Ziegler C, Drennan IR, Morrison L, Lin S. Does transport time of out‐of‐hospital cardiac arrest patients matter? A systematic review and meta‐analysis. Resuscitation. 2017;115:96–101. [DOI] [PubMed] [Google Scholar]
- 12. Kragholm K, Malta Hansen C, Dupre ME, Xian Y, Strauss B, Tyson C, Monk L, Corbett C, Fordyce CB, Pearson DA, et al. Direct transport to a percutaneous cardiac intervention center and outcomes in patients with out‐of‐hospital cardiac arrest. Circ Cardiovasc Qual Outcomes. 2017;10:e003414. [DOI] [PubMed] [Google Scholar]
- 13. Wibrandt I, Norsted K, Schmidt H, Schierbeck J. Predictors for outcome among cardiac arrest patients: the importance of initial cardiac arrest rhythm versus time to return of spontaneous circulation, a retrospective cohort study. BMC Emerg Med. 2015;15:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tsai SL, Chaou CH, Huang CH, Tzeng IS, Kuo CW, Weng YM, Chien CY. Features of hospital and emergency medical service in out‐of‐hospital cardiac arrest patients with shockable rhythm. Am J Emerg Med. 2017;35:1222–1227. [DOI] [PubMed] [Google Scholar]
- 15. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, de Caen AR, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out‐of‐hospital cardiac arrest. Circulation. 2015;132:1286–1300. [DOI] [PubMed] [Google Scholar]
- 16. Schober A, Sterz F, Laggner AN, Poppe M, Sulzgruber P, Lobmeyr E, Datler P, Keferböck M, Zeiner S, Nuernberger A, et al. Admission of out‐of‐hospital cardiac arrest victims to a high volume cardiac arrest center is linked to improved outcome. Resuscitation. 2016;106:42–48. [DOI] [PubMed] [Google Scholar]
- 17. Lee JJ, Han SJ, Kim HS, Hong KS, Choi HH, Park KT, Seo JY, Lee TH, Kim HC, Kim S, et al. Out‐of‐hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal membrane oxygenation: focus on survival rate and neurologic outcome. Scand J Trauma Resusc Emerg Med. 2016;24:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabriellia A, Silvers SM, Zaritsky AL, Merchant R, et al. Part 9: post‐cardiac arrest care: 2010 American Heart Association guideline for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S768–S786. [DOI] [PubMed] [Google Scholar]
- 19. Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, Leary M, Meurer WJ, Peberdy MA, Thompson TM, et al. Part 8: post‐cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S465–S482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163:1149–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Adelson JL, McCoach DB, Rogers HJ, Adelson JA, Sauer TM. Developing and applying the propensity score to make causal inferences: variable selection and stratification. Front Psychol. 2017;17:1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kajino K, Iwami T, Daya M, Nishiuchi T, Hayashi Y, Irisawa T, Sakai T, Kuwagata Y, Hiraide A, Kishi M, et al. Impact of transport to critical care medical centers on outcomes after out‐of‐hospital cardiac arrest. Resuscitation. 2010;81:549–554. [DOI] [PubMed] [Google Scholar]
- 23. Hassager C, Nagao K, Hildick‐Smith D. Out‐of‐hospital cardiac arrest: in‐hospital intervention strategies. Lancet. 2018;391:989–998. [DOI] [PubMed] [Google Scholar]
- 24. McCarthy JJ, Carr B, Sasson C, Bobrow BJ, Callaway CW, Neumar RW, Ferrer JME, Garvey JL, Ornato JP, Gonzales L, et al. Out‐of‐hospital cardiac arrest resuscitation systems of care: a scientific statement from the American Heart Association. Circulation. 2018;137:e645–e660. [DOI] [PubMed] [Google Scholar]
- 25. Herlitz J, Svensson L, Engdahl J, Silfverstolpe J. Characteristics and outcome in out‐of‐hospital cardiac arrest when patients are found in a non‐shockable rhythm. Resuscitation. 2008;76:31–36. [DOI] [PubMed] [Google Scholar]
- 26. Kim TH, Lee K, Shin SD, Ro YS, Tanaka H, Yap S, Wong KD, Ng YY, Piyasuwankul T, Leong B. Association of the emergency medical services‐related time interval with survival outcomes of out‐of‐hospital cardiac arrest cases in four Asian metropolitan cities using the scoop‐and‐run emergency medical services model. J Emerg Med. 2017;53:686–696. [DOI] [PubMed] [Google Scholar]


