Abstract
Maternal mortality in the United States is the highest among all developed nations, partly because of the increased prevalence of cardiovascular disease in pregnancy and beyond. There is growing recognition that specialists involved in caring for obstetric patients with cardiovascular disease need training in the new discipline of cardio‐obstetrics. Training can include integrated formal cardio‐obstetrics curricula in general cardiovascular disease training programs, and developing and disseminating joint cardiac and obstetric societal guidelines. Other efforts to help strengthen the cardio‐obstetric field include increased collaborations and advocacy efforts between stakeholder organizations, development of US‐based registries, and widespread establishment of multidisciplinary pregnancy heart teams. In this review, we present the current challenges in creating a cardio‐obstetrics community, present the growing need for education and training of cardiovascular disease practitioners skilled in the care of obstetric patients, and identify potential solutions and future efforts to improve cardiovascular care of this high‐risk patient population.
Keywords: cardio‐obstetrics, cardiovascular disease prevention, preeclampsia/pregnancy, pregnancy and postpartum, training
Subject Categories: Cardiovascular Disease, Quality and Outcomes, Statements and Guidelines, Ethics and Policy
Cardiovascular disease (CVD) is the leading cause of maternal morbidity and mortality in the United States and accounts for 26.5% of pregnancy‐related deaths.1, 2, 3 Although other countries have had a decline in maternal mortality, the US rate has continued to increase for the past 14 years, partially because of increased prevalence of CVD and its risk‐factors.4 CVD can directly lead to peripartum morbidity and mortality. In addition, some pregnancy‐specific conditions, particularly hypertensive disorders of pregnancy, can lead to short‐term and long‐term cardiovascular events, such as peripartum cardiomyopathy, chronic hypertension, or accelerated CVD.5, 6 Although CVD and pregnancy‐specific conditions can be managed during pregnancy, identifying women at high risk and optimizing antenatal, birth, and postpartum care require care from multiple specialties. In addition to maternal‐fetal medicine specialists, these women need cardiologists with focused expertise in cardio‐obstetrics. In this article, we review the spectrum of preexisting‐ or pregnancy‐associated CVD that requires management by cardiologists trained in cardio‐obstetrics; identify current gaps in training and opportunities to improve cardio‐obstetric competencies; and describe the role of multidisciplinary approaches, research, professional societies, advocacy, and social medial networks in championing the care of this unique population.
Preexisting and Pregnancy‐Associated CVD
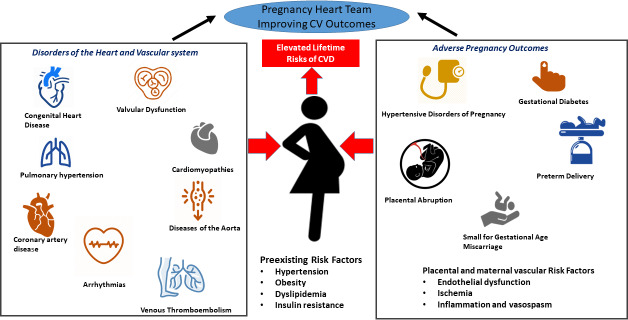
CVD may be preexistent or develop during pregnancy or in the postpartum period. For women with established CVD (eg, coronary artery disease, pulmonary hypertension, valvular disease, cardiomyopathies, arrhythmias, aortopathies, adult congenital heart disease, and genetic cardiac syndromes), the management of pregnancy and CVD has been previously addressed in guidelines and obstetrical practice bulletins.3, 7, 8, 9 The care of this population requires a multidisciplinary approach, starting with preconception counseling and categorization of risk, and ending with recommendations for lactation, mental health, and conception planning.3
There are fewer recommendations addressing cardiovascular health in other groups of pregnant women. Approximately 20% of pregnant women develop adverse pregnancy outcomes (APOs), including fetal growth restriction, placental abruption, preterm delivery, gestational diabetes mellitus, or hypertensive disorders of pregnancy.10, 11 Most APOs are associated with decreased uterine artery blood flow, vascular endothelial dysfunction, inflammation, and vasospasm,12, 13, 14 all of which may increase the risk of short‐ and long‐term CVD events.5, 10, 11, 12, 13 In particular, hypertensive disorders of pregnancy, especially the subset with preeclampsia, increase the risk of acute cardiovascular events and chronic hypertension, left ventricular dysfunction, heart failure, coronary artery disease, stroke, and renal dysfunction.5, 6, 15 However, many CVD specialists are not aware of the risks posed by APOs, and few incorporate a detailed pregnancy history in their risk assessment of women,16, 17, 18 although preeclampsia is considered a risk enhancer in newer atherosclerotic CVD risk‐assessment tools.10, 11, 19, 20
In summary, pregnancy associated with manifestations of CVD or APOs should trigger efforts to engage women to understand their future CVD risk (Figure 1). More important, these patients need counseling to develop sustainable healthy lifestyle choices as well as undertake treatments that could reduce subsequent CVD risk.
Figure 1. Preexisting and pregnancy‐associated cardiovascular disease (CVD) affecting maternal morbidity and mortality.
Improving Cardio‐Obstetrics Training
Because pregnancy can unmask or lead to acute and chronic CVD, there is a strong need for training in cardio‐obstetrics. At a minimum, establishment of clinical workforce competencies for general CVD specialists and the widespread implementation of cardio‐obstetric subspecialty fellowships can help focus the CVD community to prevent, detect, risk stratify, and optimally treat CVD in pregnancy while addressing the long‐term cardiac needs of this population. The clinical areas of focus should include the following: (1) preconception risk stratification and counseling in patients with existing CVD; (2) health optimization before pregnancy; (3) personalizing antenatal care and delivery on the basis of risk profile; and (4) early diagnosis and treatment of complications during pregnancy and postpartum.
However, most CVD fellowship training programs currently do not provide extensive exposure to cardio‐obstetrics, although the Accreditation Council for Graduate Medical Education requires that all CVD fellowship programs cultivate competence in preventing, evaluating, and managing heart disease in pregnancy.21 However, there are no specific recommendations addressing cardio‐obstetric care beyond mandating outpatient clinic experiences that include patients of varied ages and sex, which presumably would include pregnant women.21 Similarly, the American Board of Internal Medicine does not have a cardio‐obstetrics category in the certification examination blueprints, and has no mandates devoted to this population.22 Finally, Core Cardiology Training Statement CVD fellowship training guidelines do encourage exposure to pregnant women with heart disease in high‐risk obstetrical clinics.23 Trainees are also required to learn the impact of pregnancy on the risk of CVD or heart failure, as well as becoming proficient in managing the complications of pregnant patients with valvular heart disease, adult congenital heart disease, or heart failure.22, 23, 24 However, Core Cardiology Training Statement guidelines are brief in comparison to other topics, leaving large gaps in cardiology training and knowledge acquisition.25 Mandating more structured education, development and assessment of cardio‐obstetric competencies, and joint support from the American College of Obstetrics and Gynecology (ACOG), American Heart Association, American College of Cardiology, American Board of Internal Medicine, and the Accreditation Council for Graduate Medical Education are needed to ensure the establishment of adequate training. Joint recommendations with specialty groups outside of the United States would also be helpful, because working groups within the European Society of Cardiology have also recommended training in CVD in pregnancy.26
Aside from formal graduate medical education training models, training in cardio‐obstetrics is also limited, although sessions and workshops are starting to occur at the local, national, and international level. For example, at the last 3 American College of Cardiology Annual Scientific Sessions, at least 1 session was devoted to cardiac disease in pregnancy.27, 28, 29 Similarly, the American Heart Association has allocated similar numbers of sessions at each of its recent annual meetings.30 Smaller cardio‐obstetric conferences offering continuing medical education are now more prolific, and there are several online‐only courses.
Several challenges remain in providing cardio‐obstetric recommendations and training. Although there are well‐written guidelines for managing CVD in pregnancy, they have not been jointly developed or endorsed by major cardiology societies.3, 7, 9, 26 In addition, much of the data derived for these guidelines were obtained from large, multinational registries in Canada and Europe, which limits the generalizability to a US population, who has higher rates of obesity and cardiovascular risk factors. Therefore, we urge obtaining additional US‐based data and the subsequent development of multisocietal cardio‐obstetrics guidelines jointly endorsed by US and international CVD and obstetric societies. Establishing widely accepted guidelines is critically important in mandating standards in care and training and will enable credentialing organizations to incorporate required knowledge‐based questions in CVD fellowship examinations. At a minimum, guidelines should encourage implementation of curricula that facilitate a deeper understanding of the (1) cardiovascular pharmacotherapies in pregnancy, (2) physiologic and pathological cardiovascular changes that occur during pregnancy and beyond, (3) knowledge of basic obstetrical modes of delivery, (4) an overview of echocardiographic changes and development of pregnancy‐specific normal values, and (5) case‐based reviews of pregnant and postpartum patients with simple or complex CVD. If these guidelines are incorporated in Accreditation Council for Graduate Medical Education standards, American Board of Internal Medicine blueprints, and Core Cardiology Training Statement requirements (Table 1 and Figure 2), training programs would be further incentivized to support dedicated cardio‐obstetric educational efforts, including developing dedicated subspecialized fellowship tracks.
Table 1.
Current Challenges in Training and Potential Solutions
| Developing Competencies in Cardio‐Obstetrics | Current Challenges | Potential Solutions |
|---|---|---|
| Designing a curriculum in cardio‐obstetrics |
|
|
| Increasing cardio‐obstetric research |
|
|
| Gaining institutional support to start a cardio‐obstetric service line |
|
|
| Increasing community engagement and social support |
|
|
ACC indicates American College of Cardiology; ACGME, Accreditation Council for Graduate Medical Education; ACHD, adult congenital heart disease; AHA, American Heart Association; APO, adverse pregnancy outcome; COCATS, Core Cardiology Training Statement; MFM, maternal‐fetal medicine; NIH, National Institutes of Health; PHT, pregnancy heart team; QI, quality improvement; SoME, social media; and WHO, World Health Organization.
Figure 2. Improving cardiovascular workforce competencies in cardio‐obstetrics.

Role of Partnerships in Advancing Cardio‐Obstetric Care
Multidisciplinary Team–Based Care
Improving workplace competencies in cardio‐obstetrics requires strong partnerships and exposure to multidisciplinary team–based care. At some institutions, this type of care formally exists in dedicated heart centers for women or informally between adult congenital heart disease and high‐risk obstetric programs.31 Because well‐run multidisciplinary teams reduce adverse cardiovascular outcomes in high‐risk pregnancies, we suggest establishing formal pregnancy heart teams (PHTs) that include cardiologists with expertise in cardio‐obstetrics, obstetricians, maternal‐fetal medicine specialists, primary healthcare providers, obstetric anesthesiologists, neonatologists, geneticists, pharmacists, social workers, nurses, and other care team members. Depending on the complexity of CVD (Tables 2 and 3), each team member's involvement and the frequency of prenatal visits can vary. For all patients, review of medications by maternal‐fetal medicine specialists, cardiologists, and pharmacists is especially important, because each specialty can balance the risks and benefits of treatments during pregnancy and lactation. Many patients should also interact with a social worker, who can streamline access to medical coverage for postpartum maternal and neonatal care.3 For patients living a large distance from a specialized high‐risk delivery hospital, the PHT needs additional involvement before the third trimester, with detailed antepartum care and delivery plans developed to avoid inadvertent unplanned delivery at a hospital with fewer resources or physicians.
Table 2.
Suggested Timetable for Involvement of the Pregnancy Heart Team During Prepregnancy, Antenatal, Labor and Delivery, and Postnatal Time Periods for Patients With Cardio‐Obstetric Conditions
| Variable | HDP | GDM | CAD | Cardiomyopathy | ACHD‐Modified WHO Category | ||
|---|---|---|---|---|---|---|---|
| Ia | IIb | IIIc | |||||
| Prepregnancy consultation | +/− | +/− | + | + | + | + | + |
| Pregnancy heart team consultation/counseling during antenatal care | + | + | + | + | + | + | |
| Delivery at tertiary care center (level III maternal care capability facilityd) | +/− | + | + | +/− | +/− | + | |
| Long‐term follow‐up by cardiovascular specialist | +/− | +/− | + | + | + | + | + |
ACHD indicates adult congenital heart disease; CAD, coronary artery disease; GDM, gestational diabetes mellitus; HDP, hypertensive disorders of pregnancy; and WHO, World Health Organization; +, needed; ‐, not needed.
ACHD‐modified WHO category I: Simple disease, such as small atrial septal defects or repaired ductus arteriosus.
ACHD‐modified WHO category II: Moderate complexity disease, such as ostium primum atrial septal defects or repaired tetralogy of Fallot.
ACHD‐modified WHO category III: Great complexity disease, including transposition of the great arteries, mitral atresia, or single‐ventricle physiological features.
Level III maternal care capability facilities are able to provide care for complex medical conditions, obstetrical complications, and fetal conditions.
Table 3.
Suggested Involvement of Pregnancy Heart Team Members for Patients With Cardio‐Obstetric Conditionsa
| Variable | HDP | GDM | CAD | Cardiomyopathy | ACHD‐Modified WHO Category | ||
|---|---|---|---|---|---|---|---|
| Ib | IIc | IIId | |||||
| Cardiologist∥ | + | + | + | +/− | + | + | |
| Cardiologist subspecialist¶ | − | − | + | + | − | − | + |
| Obstetrician | + | + | + | + | + | + | + |
| Maternal‐fetal medicine# | + | + | + | + | + | + | + |
| Obstetric anesthesiologist | + | + | + | + | + | ||
| Pharmacist | + | + | + | + | |||
| Primary care physician/provider | + | ||||||
| Geneticist** | |||||||
| Social worker | + | + | + | ||||
Modified WHO: category I, II, III, and IV, cardiomyopathy, HDP, GDM, and ischemic heart disease. Consultation as needed. Members with expertise identified and involved in multidisciplinary case reviews. ACHD indicates adult congenital heart disease; CAD, coronary artery disease; GDM, gestational diabetes mellitus; HDP, hypertensive disorders of pregnancy; and WHO, World Health Organization.
Subspecialists for ACHD, aortopathy, heart failure, pulmonary hypertension, cardiac imaging, cardiac surgery, and interventional cardiology would be ad hoc members depending on the cardiac disease.
ACHD Modified WHO Category I: Simple disease, such as small atrial septal defects or repaired ductus arteriosus.
ACHD Modified WHO Category II: Moderate complexity disease, such as ostium primum atrial septal defects or repaired tetralogy of Fallot.
CHD Modified WHO Category III: Great complexity disease, including transposition of the great arteries, mitral atresia, or single ventricle physiology.
PHTs should also focus on quality improvement (QI) initiatives for their entire cohort of pregnant patients, which can be incorporated at routine monthly multidisciplinary meetings. Other QI initiatives could be developed during meetings with stakeholders, such as community caregivers, health advocates, and health system administrators. In addition, PHT members can share QI initiatives with other institutions, especially if they participate in well‐run state maternal mortality review committees.
Well‐developed PHTs are also essential in providing trainees an immersive cardio‐obstetrics educational experience. PHTs can help facilitate outpatient cardio‐obstetrics clinic experiences for general CVD fellows, especially because these experiences are less time intensive. In addition, these teams can offer specialized inpatient rotations on labor and delivery teams for advanced trainees, who have fewer time constraints. Both types of experiences will facilitate greater encounters with women with heart disease who are considering pregnancy or are pregnant. In addition, there would be more opportunities to witness the effect of APOs on long‐term cardiovascular outcomes. Finally, there will be increased occasions to discuss CVDs with different presentations in women, including coronary artery disease, pulmonary hypertension, spontaneous coronary artery dissection, valvular disease, cardiomyopathies, familial hypercholesterolemia, and coronary microvascular dysfunction.
Research
Despite the increasing number of pregnant women with preexisting CVD and the greater awareness associating APOs with increased short‐ and long‐term risks, few resources are directed at addressing pathogenic factors, developing effective treatments, and creating research and QI initiatives. In particular, more efforts are needed to determine the risk factors, epidemiological features, and pathogenesis of APO‐related cardiac dysfunction because this could guide efforts to prevent and effectively treat subsequent CVD. In addition, there is a need for a large US‐based multicenter registry collecting CVD management data before, during, and after pregnancy.32 We suggest modeling this type of large national registry on the basis of the CMQCC (California Maternal Quality Care Collaborative) registry, which tracks data for all births in that state.33 If created, this type of registry can guide PHT members in determining current practices and outcomes and help shape management protocols to preserve cardiovascular health. Furthermore, it can record outcomes of future pregnancies and corresponding neonatal health into early childhood.32 In addition, a large‐inclusive registry can be immensely useful for QI initiatives that can identify and address disparities in maternal and postpartum morbidity and mortality, which could then focus on hospitals with better outcomes to identify and champion best practices.33 This is particularly important for black women, who have much higher adverse outcomes, especially for those aged >39 years.1 Finally, research and QI efforts are also critical for women who are farther from pregnancy, because the optimal timing for CVD surveillance, risk stratification, pharmacological management, and follow‐up remains unknown.10
Role of Professional Societies and Stakeholder Partnerships
Professional societies are instrumental in the widespread dissemination of knowledge because they develop and distribute guidelines and educational programs. Guidelines now exist for the management of CVD in pregnancy.3, 7 Also, recent guidelines for CVD risk assessment include preeclampsia and premature menopause as risk enhancers.19 However, none of these guidelines is jointly endorsed by major obstetric and cardiovascular societies, and none addresses short‐ or long‐term CVD complications for patients who develop APOs. Multiple societies, including the American Heart Association, American College of Cardiology, and ACOG, should develop collaborations and guidelines that clinicians can use to care for the short‐ and long‐term CVD needs of pregnant women.34 These efforts can expand on joint statements by ACOG and American Heart Association that have stressed the importance of well‐woman visits to screen, counsel, and educate women on heart health and timely recognition of APOs.8 They should also build on recent ACOG efforts, which formed a task force focused on CVD in pregnancy that provides comprehensive recommendations and supplements previous practice bulletins that address hypertensive disorders of pregnancy and gestational diabetes mellitus.35, 36, 37 They can champion the national efforts of the Alliance for Innovation on Maternal Health, which is a national coalition endorsed by ACOG focused on reducing maternal mortality by encouraging systematic implementation of maternal safety bundles.38
Advocacy
Enhancing cardio‐obstetrics care requires health policies that improve structural supports for pregnant women. In particular, cardiologists need to be more involved, seeking out collaborations with obstetricians, professional societies, patient support groups, healthcare institutions, and health policy makers. They can build on recent successful advocacy efforts, such as the Indiana‐based OB Navigators program, which provides newly pregnant high‐risk women with a navigator who makes home visits and guides them during pregnancy and the first postpartum year. This type of pilot program can be encouraged and propagated in other states to increase coordination of care and address CVD and its risk factors. Other advocacy efforts should include championing patient support organizations, which often have trustworthy peer‐support structures and are intrinsically motivated to improve care. As an example, the Preeclampsia Foundation supports a community of pregnant and postpartum women and their partners, and shares information about the effects of preeclampsia on short‐ and long‐term cardiac outcomes with interested health professionals, governmental officials, and the public.39 Notably, this group is also involved in advocacy, spearheading a grassroots campaign to support bipartisan legislation, such as the Preventing Maternal Deaths Act of 2017, H.R 1318, 115TH Congress, and the Maternal Health Accountability Act of 2017, S.1112, 115TH Congress.
Social Media Platforms
Social media can increase the dissemination of guidelines, best practices, and research publications. In the cardio‐obstetrics world, social media has started to connect varied interested clinicians and researchers with key stakeholders, such as policy makers, medical societies, patient‐advocacy foundations, and other members of the public.40 For example, multiple organizations, including ACOG, National Institutes of Health, Centers for Disease Control and Prevention, and other foundations, have shared late‐breaking information on Twitter using the hashtag #PregnancyCardioHealth. Building on these past efforts, we encourage raising awareness in cardio‐obstetrics using social media and making it a core part of their communication strategy.
Conclusions
There is growing interest in cardio‐obstetrics because of the well‐described manifestations of CVD during pregnancy and because there is increased awareness that APOs are associated with subsequent CVD events. It is time to increase the numbers of practitioners in cardio‐obstetrics and to increase the amount of training and knowledge in this field. It is especially important to incorporate more cardio‐obstetrics topics in general CVD‐training programs and to establish formalized dedicated cardio‐obstetrics tracks. In addition, institutions should establish more team‐based care programs and PHTs to improve care, augment trainee education, and encourage research efforts. Professional societies and stakeholders should also help by organizing efforts to educate and advocate for the needs of this patient population through traditional methods and social media. Ultimately, by committing to all these strategies, we can ensure that our clinical practices, policies, and systems reflect our obligation to improve the cardiovascular health and well‐being of mothers during pregnancy and beyond.
Disclosures
None.
(J Am Heart Assoc. 2020;9:e015569 DOI: 10.1161/JAHA.119.015569.)
For Disclosures, see page 7.
References
- 1. Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy‐related mortality in the United States, 2011–2013. Obstet Gynecol. 2017;130:366–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Knight M, Nair M, Tuffnell D, Kenyon S, Shakespeare J, Brocklehurs P, Kurinczuk JJ. Saving lives, improving mothers’ care. EMBRRACE UK 2017. Available at: https://www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/MBRRACE-UK%20Maternal%20Report%202017%20-%20Web.pdf. Accessed April 22, 2020.
- 3. ACOG Practice Bulletin No. 212: pregnancy and heart disease. Obstet Gynecol. 2019;133:e320–e356. [DOI] [PubMed] [Google Scholar]
- 4. Koch AR, Lightner S, Geller SE. Identifying maternal deaths in Texas using an enhanced method, 2012. Obstet Gynecol. 2018;132:520–521. [DOI] [PubMed] [Google Scholar]
- 5. Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, Zaman A, Fryer AA, Kadam U, Chew‐Graham CA, et al. Preeclampsia and future cardiovascular health: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2017;10:e003497. [DOI] [PubMed] [Google Scholar]
- 6. Vaught AJ, Kovell LC, Szymanski LM, Mayer SA, Seifert SM, Vaidya D, Murphy JD, Argani C, O'Kelly A, York S, et al. Acute cardiac effects of severe pre‐eclampsia. J Am Coll Cardiol. 2018;72:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. ESC guidelines for the management of cardiovascular diseases during pregnancy. Rev Esp Cardiol (Engl Ed). 2019;72:161. [DOI] [PubMed] [Google Scholar]
- 8. Brown HL, Warner JJ, Gianos E, Gulati M, Hill AJ, Hollier LM, Rosen SE, Rosser ML, Wenger NK; American Heart Association and the American College of Obstetricians and Gynecologists . Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a presidential advisory from the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation. 2018;137:e843–e852. [DOI] [PubMed] [Google Scholar]
- 9. Canobbio MM, Warnes CA, Aboulhosn J, Connolly HM, Khanna A, Koos BJ, Mital S, Rose C, Silversides C, Stout K, et al. Management of pregnancy in patients with complex congenital heart disease: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2017;135:e50–e87. [DOI] [PubMed] [Google Scholar]
- 10. Grandi SM, Filion KB, Yoon S, Ayele HT, Doyle CM, Hutcheon JA, Smith GN, Gore GC, Ray JG, Nerenberg K, et al. Cardiovascular disease‐related morbidity and mortality in women with a history of pregnancy complications: systematic review and meta‐analysis. Circulation. 2019;139:1069–1079. [DOI] [PubMed] [Google Scholar]
- 11. Wu P, Gulati M, Kwok CS, Wong CW, Narain A, O'Brien S, Chew‐Graham CA, Verma G, Kadam UT, Mamas MA. Preterm delivery and future risk of maternal cardiovascular disease: a systematic review and meta‐analysis. J Am Heart Assoc. 2018;7:e007809 DOI: 10.1161/JAHA.117.007809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lane‐Cordova AD, Khan SS, Grobman WA, Greenland P, Shah SJ. Long‐term cardiovascular risks associated with adverse pregnancy outcomes: JACC review topic of the week. J Am Coll Cardiol. 2019;73:2106–2116. [DOI] [PubMed] [Google Scholar]
- 13. Cain MA, Salemi JL, Tanner JP, Kirby RS, Salihu HM, Louis JM. Pregnancy as a window to future health: maternal placental syndromes and short‐term cardiovascular outcomes. Am J Obstet Gynecol. 2016;215:484.e1–484.e14. [DOI] [PubMed] [Google Scholar]
- 14. Ridder A, Giorgione V, Khalil A, Thilaganathan B. Preeclampsia: the relationship between uterine artery blood flow and trophoblast function. Int J Mol Sci. 2019;20:E3263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Buddeberg BS, Sharma R, O'Driscoll JM, Kaelin Agten A, Khalil A, Thilaganathan B. Cardiac maladaptation in term pregnancies with preeclampsia. Pregnancy Hypertens. 2018;13:198–203. [DOI] [PubMed] [Google Scholar]
- 16. Roberts JM, Catov JM. Pregnancy is a screening test for later life cardiovascular disease: now what? Research recommendations. Womens Health Issues. 2012;22:e123–e128. [DOI] [PubMed] [Google Scholar]
- 17. Young B, Hacker MR, Rana S. Physicians’ knowledge of future vascular disease in women with preeclampsia. Hypertens Pregnancy. 2012;31:50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nijdam ME, Timmerman MR, Franx A, Bruinse HW, Numans ME, Grobbee DE, Bots ML. Cardiovascular risk factor assessment after pre‐eclampsia in primary care. BMC Fam Pract. 2009;10:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, Zaman A, Fryer AA, Kadam U, Chew‐Graham CA, et al. Preeclampsia and future cardiovascular health. Circ Cardiovasc Qual Outcomes. 2017;10:e003497. [DOI] [PubMed] [Google Scholar]
- 20. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd‐Jones D, McEvoy JW, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary. J Am Coll Cardiol. 2019;74:1376–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Accreditation Council for Graduate Medical Education . ACGME program requirements for graduate medical education in cardiovascular disease (subspecialty of internal medicine). Editorial Revision: Effective July 1, 2019. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/141_CardiovascularDisease_2019.pdf?ver=2019-06-18-142306-937. Accessed August 30, 2019.
- 22. American Board of Internal Medicine . Cardiovascular disease certification examination blueprints. https://www.abim.org/~/media/ABIM%20Public/Files/pdf/examblueprints/certification/cardiovascular-disease.pdf. Accessed August 30, 2019.
- 23. American Board of Internal Medicine . Cardiovascular disease certification examination blueprints. https://www.abim.org/~/media/ABIM%20Public/Files/pdf/exam14blueprints/certification/cardiovascular-disease.pdf. Accessed August 30, 2019.
- 24. Jessup M, Ardehali R, Konstam MA, Manno BV, Mathier MA, McPherson JA, Sweitzer NK. COCATS 4 Task Force 12: training in heart failure. J Am Coll Cardiol. 2015;65:1866–1876. [DOI] [PubMed] [Google Scholar]
- 25. Davis MB, Walsh MN. Cardio‐obstetrics. Circ Cardiovasc Qual Outcomes. 2019;12:e005417. [DOI] [PubMed] [Google Scholar]
- 26. Baumgartner H, Budts W, Chessa M, Deanfield J, Eicken A, Holm J, Iserin L, Meijboom F, Stein J, Szatmari A, et al. Recommendations for organization of care for adults with congenital heart disease and for training in the subspecialty of “grown‐up congenital heart disease” in Europe: a position paper of the 1 Working Group on Grown up Congenital Heart Disease of the Europe. Eur Heart J. 2014;35:686–690. [DOI] [PubMed] [Google Scholar]
- 27. McNamara DM, Poppas A; Co‐chairs . ACC.19: session 726: pregnancy and cardiovascular disease: at the heart of mother and the baby. https://www.abstractsonline.com/pp8/#!/5758/session/429. Accessed August 30, 2019.
- 28. Arany Z, Elkayam U; Co‐chairs . ACC.18: session 603: HELP! my patient with heart disease is now pregnant. https://www.acc.org/~/media/ScientificSessions/ACC18/2018/01/Itinerary-Planning-Tools/31/ACC18-Program-Saturday-March-2-2018.pdf. Accessed August 30, 2019.
- 29. Givertz M, Rubin S; Co‐chairs . ACC.17: session 716: pregnancy and heart disease. https://www.acc.org/~/media/ScientificSessions/ACC17/PDFs/Itinerary-Planning-Tools/ACC17-Program-PDFs-ByPathway-Heart-Failure-and-Cardiomyopathies.pdf. Accessed August 30, 2019.
- 30. American Heart Association Scientific Sessions. 2019. Available at: https://www.professional.heart.org/professional/EducationMeetings/MeetingsLiveCME/ScientificSessions/UCM_316935_Archive-Scientific-Sessions.jsp. Accessed April 20, 2020.
- 31. Lundberg GP, Mehta LS, Sanghani RM, Patel HN, Aggarwal NR, Aggarwal NT, Braun LT, Lewis SJ, Mieres JH, Wood MJ, et al. Heart centers for women historical perspective on formation and future strategies to reduce cardiovascular disease. Circulation. 2018;138:1155–1165. [DOI] [PubMed] [Google Scholar]
- 32. Grodinsky A, Florio K, Spertus JA, Daming T, Schmidt L, Lee J, Rader V, Nelson L, Gray R, White D, et al. Maternal mortality in the United States and the HOPE Registry. Curr Treat Options Cardiovasc Med. 2019;27:505. [DOI] [PubMed] [Google Scholar]
- 33. Markow C, Main EK. Creating change at scale: quality improvement strategies used by the California Maternal Quality Care Collaborative. Obstet Gynecol Clin North Am. 2019;46:317–328. [DOI] [PubMed] [Google Scholar]
- 34. Ying W, Catov JM, Ouyang P. Hypertensive disorders of pregnancy and future maternal cardiovascular risk. J Am Heart Assoc. 2018;7:e009382 DOI: 10.1161/JAHA.118.009382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. ACOG Committee on Obstetric Practice . Presidential task force on redefining the postpartum visit committee on obstetric practice. Obstet Gynecol. 2018;131:e140–e150.29683911 [Google Scholar]
- 36. ACOG Guidelines: Hypertension in pregnancy. Obstet Gynecol. 2019;133:e1–e25.30575675 [Google Scholar]
- 37. ACOG Practice Bulletin No. 190: gestational diabetes mellitus. Obstet Gynecol. 2018;131:e49–e64. [DOI] [PubMed] [Google Scholar]
- 38. Mahoney J. The alliance for innovation in maternal health care: a way forward. Clin Obstet Gynecol. 2018;61:400–410. [DOI] [PubMed] [Google Scholar]
- 39. Tsigas E. Advocacy is essential to supporting women with pre‐eclampsia. Obstet Med. 2017;10:33–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Parwani P, Choi AD, Lopez‐Mattei J, Raza S, Chen T, Narang A, Michos ED, Erwin JP, Mamas MA, Gulati M. Understanding social media: opportunities for cardiovascular medicine. J Am Coll Cardiol. 2019;73:1089–1093. [DOI] [PubMed] [Google Scholar]


