Abstract
Background
Blacks are disproportionately affected by stroke compared with whites; however, less is known about the relationship between stroke and cigarette smoking in blacks. Therefore, we evaluated the relationship between cigarette smoking and all incident stroke in the JHS (Jackson Heart Study).
Methods and Results
JHS participants without a history of stroke (n=4410) were classified by self‐reported baseline smoking status into current, past (smoked at least 400 cigarettes/life), or never smokers at baseline (2000–2004). Current smokers were further classified by smoking intensity (number of cigarettes smoked per day [1–19 and ≥20]) and followed up for incident stroke (through 2015). Hazard ratios (HRs) for incident stroke for current and past smoking compared with never smoking were estimated with adjusted Cox proportional hazard regression models. After adjusting for cardiovascular risk factors, the risk for stroke in current smokers was significantly higher compared with never smokers (HR, 2.48; 95% CI, 1.60–3.83) but there was no significant difference between past smokers and never smokers (HR, 1.10; 95% CI, 0.74–1.64). There was a dose‐dependent increased risk of stroke with smoking intensity (HR, 2.28 [95% CI, 1.38–3.86] and HR, 2.78 [95% CI, 1.47–5.28] for current smokers smoking 1–19 and ≥20 cigarettes/day, respectively).
Conclusions
In a large cohort of blacks, current cigarette smoking was associated with a dose‐dependent higher risk of all stroke. In addition, past smokers did not have a significantly increased risk of all stroke compared with never smokers, which suggests that smoking cessation may have potential benefits in reducing the incidence of stroke in blacks.
Keywords: blacks, cigarette smoking, Jackson Heart Study, stroke
Subject Categories: Cardiovascular Disease, Epidemiology, Race and Ethnicity, Cerebrovascular Disease/Stroke
Nonstandard Abbreviations and Acronyms
- BCA
Bifurcation of the carotid artery
- CIMT
Carotid intima‐media thickness
- CRP
C‐reactive protein
- FHS
Framingham Heart Study
- HR
Hazard ratio
- JHS
Jackson Heart Study
- NHS
Nurses Health Study
- PHS
Physicians Health Study
Clinical Perspective
What Is New?
Cigarette smoking is a known modifiable risk factor for stroke; however, its role in the evolution of stroke in blacks has been largely understudied.
In the JHS (Jackson Heart Study), a large longitudinal black cohort, current cigarette smoking status and smoking intensity (cigarettes per day) were independently associated with >2 times increased risk for stroke in adjusted models, over a follow‐up period of more than a decade.
Current and past cigarette smoking were associated with higher carotid atherosclerosis (measured by carotid intima‐media thickness), suggesting accelerated atherosclerosis attributable to smoking could play a role in the development of stroke in black smokers.
What Are the Clinical Implications?
Our findings further support public health initiatives directed toward smoking cessation, especially among high‐risk groups, like blacks.
Stroke is a leading cause of morbidity and mortality,1, 2 and cigarette smoking is a known independent risk factor for the development of stroke.3, 4, 5 Blacks are disproportionately affected more by stroke than any other racial group within the US population.2 Compared with whites, the risk of having a first stroke is nearly twice as high for blacks,1 and blacks are twice as likely to die from stroke.2 Higher rates of hypertension, obesity, and diabetes mellitus among blacks might account for some of this disparity.6
However, despite evidence from previous epidemiological and clinical studies that smoking is a risk factor for stroke,3, 4, 5 there are limited data directly assessing the association between cigarette smoking and stroke in blacks. Therefore, we assessed the relationships between cigarette smoking status, intensity, and dose with incident stroke in participants of the JHS (Jackson Heart Study), a large, well‐characterized community‐based black cohort.
Several mechanisms, including inflammation, atherosclerosis, and increased platelet aggregation, have been associated with the development of stroke and cigarette smoking.7, 8, 9 We also evaluated the relationship between cigarette smoking and stroke in blacks after adjustment for CRP (C‐reactive protein) (a marker of inflammation) and by measures of carotid intima‐media thickness (CIMT; a noninvasive test for assessing the degree of atherosclerosis).
Methods
Study Population
The JHS is the largest single‐site prospective cohort study designed to investigate the risk factors for cardiovascular diseases in blacks. The study included 5306 participants, aged 21 to 84 years, who were recruited from the tricounty area surrounding Jackson, MS (Hinds, Rankin, and Madison). Participants were evaluated at baseline from 2000 to 2004 (visit 1) and completed 2 subsequent study follow‐up visits (visit 2, 2005–2008; visit 3, 2009–2013). The JHS was approved by the Institutional Review Boards of Jackson State University, Tougaloo College, and the University of Mississippi Medical Center in Jackson. Each study participant provided written informed consent.
The data, analytic methods, and study materials are available to other researchers for purposes of reproducing the results or replicating the procedure by following the JHS publication procedures and data use agreements.10
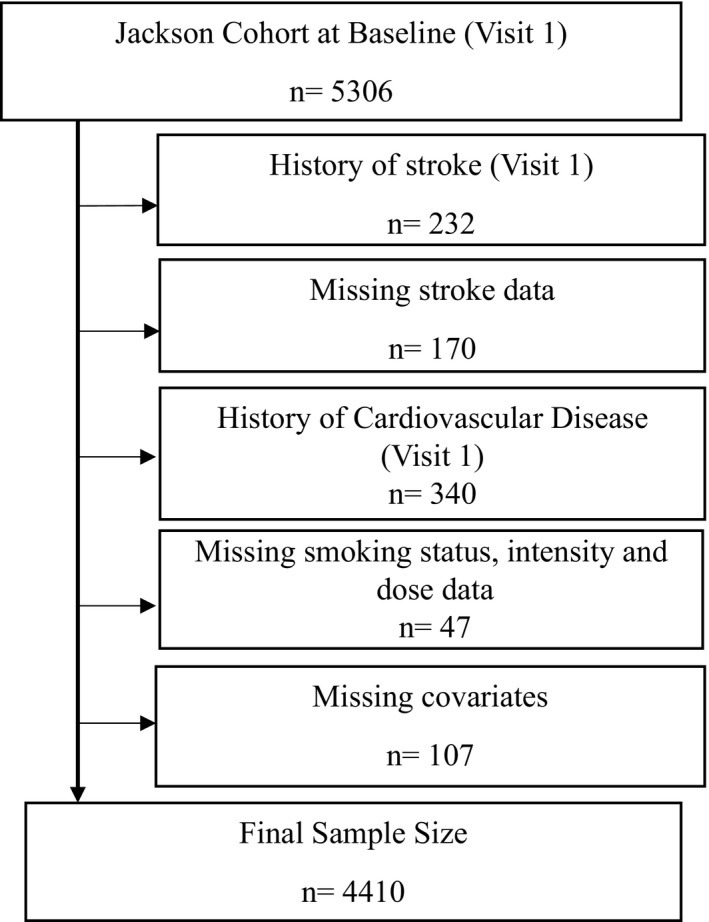
For the present analysis, we excluded all participants with a history of stroke (n=232), missing stroke data (n=170), history of cardiovascular disease (n=340), missing information on smoking status, intensity, and dose (n=47), or missing information on relevant study variables (ie, those included in multivariable analyses; n=107) at visit 1 (Figure 1).
Figure 1. Flow diagram for determination of final study population.
Smoking Information
We obtained cigarette smoking information by a self‐reported questionnaire at baseline (visit 1). Participants who responded positively to the question “Have you smoked >400 cigarettes in your lifetime” were defined as ever smokers.11, 12, 13 Participants who gave a positive response to the question, “Do you now smoke cigarettes?,” were classified as current smokers. Those who responded negatively to these questions were classified as never smokers. Participants who were classified as ever smokers who no longer smoked at the time of the examination were classified as past smokers.11 Information on the number of cigarettes smoked daily was collected to determine smoking intensity, and the number of cigarettes smoked daily was multiplied by number of years smoked (derived by subtracting the age of initiation of smoking among smokers from the end of the ascertainment period in the JHS) to determine smoking burden (pack‐years).
Ascertainment of Stroke Events
Briefly, we defined stroke on the basis of history of stroke (from personal history or stroke signs and symptoms ascertained by standardized questionnaires), transient ischemic attack, or carotid endarterectomy, angioplasty, or both.14, 15 All stroke events were ascertained via directed patient queries during annual telephone follow‐up and ongoing surveillance of hospitalizations, with subsequent transmission of hospital records and death certificates to a medical record abstraction unit for review. A computer‐generated diagnosis with physician adjudication was used to classify hospitalized and fatal stroke events. We included all ischemic and hemorrhagic stroke events that occurred after the baseline examination date.15, 16
Study Variables
Age, sex, and anthropometric data, such as body mass index, were recorded at the baseline examination of the JHS. Self‐reported use of aspirin and statins was also collected at each visit. The JHS had few participants with prevalent atrial fibrillation. Hence, we did not include details of atrial fibrillation in our analysis.
Hypertension was defined as blood pressure ≥140/90 mm Hg or use of self‐reported blood pressure–lowering medication, and diabetes mellitus was defined as fasting glucose ≥126 mg/dL, hemoglobin A1c ≥6.5%, or use of diabetes mellitus medications within 2 weeks before the clinic visit.17 Total cholesterol was measured from plasma with the use of a cholesterol oxidase method (Roche Diagnostics) on a Roche COBAS FARA centrifugal analyzer. Serum CRP was measured by the latex particle immunoturbidimetric assay (Roche Diagnostics).11
CIMT is a noninvasive test for assessing the degree of atherosclerosis. An increased CIMT has been associated with incident stroke.18, 19, 20, 21 Therefore, we examined the relationship between cigarette smoking and the incident stroke in blacks of the JHS, through CIMT values (measured at visit 1). CIMT was measured by an electrocardiography‐gated, B‐mode, and spectral Doppler; an integrated recorder ultrasound was used to obtain the carotid artery images using a 7.5‐MHz linear array transducer. CIMT was measured in millimeters, and scan images were obtained bilaterally (right and left sides) for both carotid artery walls (far and near walls) at 3 segments of the carotid artery: common carotid artery, bifurcation of the carotid artery (BCA), and internal carotid artery. The scanned values of all segments (internal carotid arteries, BCAs, or common carotid arteries), angles (anterior, lateral, or posterior), sides (right or left), and walls (far or near) of carotid artery were recorded. Mean CIMT was calculated as the average of far‐wall values across both right and left sides at the common carotid artery, BCA, and internal carotid artery segments, as measured at end diastole (at the R wave) in gated still frames.18 The most common site for carotid atherosclerosis is the BCA,22 and far wall measurements of CIMT are more reliable compared with near wall measurements.23 For our analysis, we used the mean of the BCA optimal far wall.
Statistical Analysis
We compared baseline characteristics using the χ2 tests, 1‐way ANOVA, Mann‐Whitney U test, and Kruskal‐Wallis tests for differences among never, past, and current smokers, as appropriate on the basis of the underlying distribution. Cox proportional hazard regression models were used to estimate the association between smoking status at visit 1 and incident stroke, yielding hazard ratios (HRs) for incident stroke for each smoking group compared with never smokers and by smoking intensity and burden among current smokers. All covariates were ascertained only at baseline. Kaplan‐Meier curves were constructed to assess the cumulative survival of participants free from incident stroke by smoking status and compared by log‐rank tests. Participants who died and were lost to follow‐up were censored. Schoenfeld residuals were used to test the assumption of proportionality, and there were no significant deviations from proportionality. Multivariable linear regression models were used to assess the cross‐sectional associations between smoking status, smoking intensity, and CIMT. CRP values were transformed using natural logarithms to approximate normal distributions. All statistical analyses were performed with STATA version 15 (STATA Corp, College Station, TX). A 2‐sided P<0.05 was considered significant.
Results
In this study, there were 4410 participants (83.1% of overall cohort) without missing covariates. Among these, 3083 (69.9%) participants were identified as never smokers, 781 (17.7%) were identified as past smokers, and 546 (12.4%) were identified as current smokers. Baseline characteristics of the participants grouped by smoking status are presented in Table 1. Compared with never smokers, current smokers and past smokers were more likely to be men (P<0.001). Current smokers were younger and had lower body mass index compared with never smokers and past smokers (all P<0.001). Past smokers were more likely to be less educated and had a higher prevalence of hypertension and diabetes mellitus compared with never smokers and current smokers (all P<0.001). The prevalence of statins and antiplatelet medication use was higher in past smokers compared with the other groups, and the prevalence of taking these medications in current smokers was lower than in never smokers (all P<0.001). Current smokers had higher fasting triglycerides and CRP levels compared with the other groups.
Table 1.
Baseline Characteristics at Visit 1 by Smoking Status
| Variables | Overall (n=4410) | Smoking Status | P Value | ||
|---|---|---|---|---|---|
| Never Smoker | Past Smoker | Current Smoker | |||
| (n=3083) | (n=781) | (n=546) | |||
| Age, y | 54.0 (12.7) | 53.1 (13.0) | 59.2 (11.2) | 51.6 (11.1) | <0.001 |
| Sex, men, n (%) | 1581 (36) | 937 (30) | 367 (47) | 277 (51) | <0.001 |
| Body mass index, kg/m2 | 31.8 (7.21) | 32.2 (7.3) | 31.5 (6.6) | 30.0 (7.4) | <0.001 |
| Ideal health indicator via physical activity, n (%) | |||||
| Poor health | 2101 (48) | 1439 (47) | 341 (44) | 321 (59) | <0.001 |
| Intermediate health | 1428 (32) | 1018 (33) | 271 (35) | 139 (25) | |
| Ideal health | 881 (20) | 626 (20) | 169 (22) | 86 (16) | |
| Alcohol consumption in the past 12 mo, n (%) | 2069 (47) | 1291 (42) | 382 (49) | 396 (73) | <0.001 |
| Age of initiation of smoking, y | NA | NA | 18.8 (5.1) | 19.8 (6.1) | |
| Education, n (%) | |||||
| Less than high school | 726 (16) | 424 (14) | 185 (24) | 117 (21) | <0.001 |
| High school graduate/GED | 887 (20) | 587 (19) | 171 (22) | 129 (24) | |
| Attended vocational school, trade school, or college | 2797 (63) | 2072 (67) | 425 (54) | 300 (55) | |
| Hypertension, n (%) | 2376 (54) | 1615 (52) | 495 (63) | 266 (49) | <0.001 |
| Diabetes mellitus, n (%) | 954 (22) | 644 (21) | 209 (27) | 101 (18) | <0.001 |
| Total cholesterol, mg/dL | 199.7 (39.5) | 199.4 (38.6) | 202.1 (40.7) | 198.1 (42.4) | 0.17 |
| Fasting triglyceride, mg/dL | 105.6 (80.3) | 100.5 (71.8) | 113.3 (75.5) | 123.8 (121.2) | <0.001 |
| Antiplatelet medication use, n (%) | 930 (45) | 596 (43) | 235 (57) | 99 (38) | <0.001 |
| Statin use, n (%) | 508 (12) | 340 (11) | 125 (16) | 43 (8) | <0.001 |
| CRP level, mg/dL | 0.5 (0.9) | 0.5 (0.7) | 0.5 (0.8) | 0.6 (1.7) | 0.002 |
Continuous values are presented as mean (SD), and all other values are number (percentage); χ2 tests, 1‐way ANOVA, Mann‐Whitney U test, and Kruskal‐Wallis test were used to compare baseline characteristics of participants by smoking status. CRP indicates C‐reactive protein; GED, general equivalency diploma; and NA, not applicable.
During follow‐up from baseline to 2015 (median follow‐up time was 11.8 years), 183 participants developed stroke (incidence rate, 3.49/1000 person‐years). Both past and current smokers had a higher incidence of stroke compared with never smokers (log‐rank P=0.0001) (Figure 2). Among current smokers using 1 to 19 cigarettes/day, there were 24 stroke events, whereas those using ≥20 cigarettes/day had 13 stroke events (Table 2). We also performed unadjusted analysis for incident stroke stratified by sex for each smoking category. Male smokers had higher incidence rates for stroke compared with female smokers (Table S1). After adjusting for age and sex (model 1), current smokers had higher risk for stroke compared with never smokers (HR, 2.57; 95% CI, 1.75–3.79) (Table 2). The risk of stroke was not different in past smokers compared with never smokers (HR, 1.16; 95% CI, 0.81–1.68). After further adjustment for age, sex, education level, body mass index, diabetes mellitus, systolic blood pressure, hypertension, total cholesterol, fasting triglycerides, physical activity, and statin use (model 2), current smoking was associated with an increased risk of incident stroke compared with never smoking (HR, 2.48; 95% CI, 1.60–3.83). There was a dose‐dependent increased risk of stroke in current smokers smoking 1 to 19 cigarettes/day (HR, 2.28; 95% CI, 1.38–3.86) and ≥20 cigarettes/day (HR, 2.78; 95% CI, 1.47–5.28) compared with never smokers.
Figure 2. Kaplan‐Meier survival curves of the study participants by smoking status.
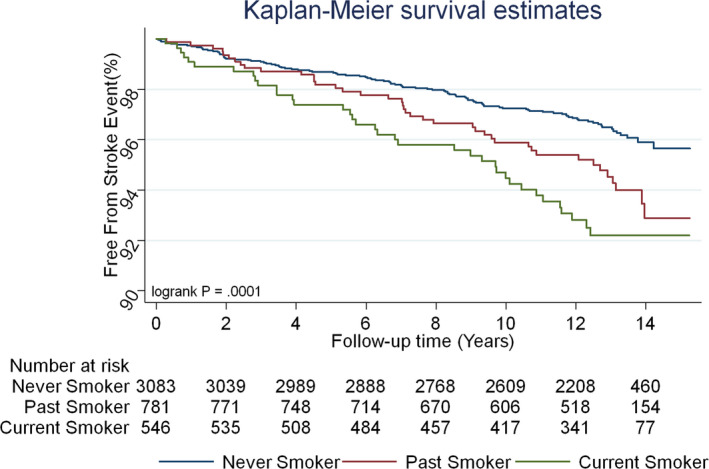
Table 2.
Association Between Smoking Status and Incident Stroke From Visit 1 to 2015
| Variable | Never Smokers | Past Smokers | Current Smokers | Current (1–19 Cigarettes/d) | Current (≥20 Cigarettes/d) |
|---|---|---|---|---|---|
| Stroke incidence, n/total (%) | 105/3089 | 41/781 | 37/546 | 24/366 | 13/180 |
| (3.4) | (5.2) | (6.8) | (6.6) | (7.2) |
| Model | Smoking Status | Smoking Intensity | ||
|---|---|---|---|---|
| Past vs Never Smokers | Current vs Never Smokers | Current (1–19 Cigarettes/d) vs Never Smokers | Current (≥20 Cigarettes/d) vs Never Smokers | |
| Model 1 | 1.16 (0.81, 1.68) | 2.57 (1.75, 3.79)a , b | 2.54 (1.62, 3.99)a , b | 2.65 (1.46, 4.80)a , b |
| Model 2 | 1.10 (0.74, 1.64) | 2.48 (1.60, 3.83)a , b | 2.28 (1.35, 3.86)a , c | 2.78 (1.47, 5.28)a , c |
| Model 3 | 1.12 (0.75, 1.67) | 2.44 (1.57, 3.78)a , b | 2.30 (1.37, 3.90)a , c | 2.62 (1.37, 5.01)a ,† |
Values are given as hazard ratio (95% CI), unless otherwise indicated. Model 1, adjusted for age and sex. Model 2, model 1 plus education level, diabetes mellitus, systolic blood pressure, body mass index, hypertension, total cholesterol, fasting triglycerides, physical activity, and statin use. Model 3, model 2 plus CRP (C‐reactive protein).
The values are statistically significant.
P<0.05.
P<0.001.
To assess the role of inflammation in the increased risk of stroke in smokers, we also adjusted for CRP (model 3). Adjustment for CRP minimally attenuated the increased risk of stroke in current smokers compared with never smokers (HR, 2.11; 95% CI, 1.38–3.22).
We assessed CIMT values measured at visit 1 among smokers by status and intensity to gain more understanding about the relationship between smoking and incident stroke (Table 3). After adjusting for age and sex (model 1), current and past smokers had increased CIMT compared with never smokers. Furthermore, current smokers smoking 1 to 19 cigarettes/day had higher CIMT compared with never smokers (β coefficient, 0.05; P=0.02), and current smokers using ≥20 cigarettes/day also had higher CIMT compared with never smokers (β coefficient, 0.08; P=0.008). After further adjustment for age, sex, education level, body mass index, diabetes mellitus, systolic blood pressure, hypertension, total cholesterol, fasting triglycerides, physical activity, and statin use (model 2), current and past smoking was associated with increased CIMT compared with never smokers. Current smokers using ≥20 cigarettes/day also had higher CIMT compared with never smokers (β coefficient, 0.12; P <0.001). However, the association between CIMT and using 1 to 19 cigarettes/day among current smokers was no longer significant (Table 3).
Table 3.
Association Between Smoking Status and CIMT at Visit 1 Among JHS Participants
| Model | Never Smokers | Past Smokers | Current Smokers | Current (1–19 Cigarettes/d) | Current (≥20 Cigarettes/d) |
|---|---|---|---|---|---|
| 1 | 0 (Reference) | 0.06 (0.02, 0.09)a , b | 0.07 (0.03, 0.10)a , c | 0.05 (0.00, 0.10)a , b | 0.08 (0.02, 0.14)a , b |
| 2 | 0 (Reference) | 0.06 (0.03, 0.09)a , b | 0.07 (0.03, 0.11)a , c | 0.05 (−0.00, 0.09) | 0.12 (0.05, 0.19)a , c |
n=2614. The mean of the bifurcation optimal far wall values in millimeters was used for CIMT measurements. Values are given as β coefficients (95% CIs). Model 1, adjusted for age and sex. Model 2, adjusted for age, sex, education level, diabetes mellitus, systolic blood pressure, body mass index, hypertension, total cholesterol, fasting triglycerides, physical activity, and statin use. CIMT indicates carotid intima‐media thickness; and JHS, Jackson Heart Study.
The values are statistically significant.
P<0.05.
P<0.001.
Testing for Interaction
We did not observe any statistically significant interaction between sex and smoking in our analysis. Furthermore, we found no statistically significant results in our test of mediation to ascertain if the association between smoking and stroke is mediated, partially or by how much, by inflammation (CRP) and atherosclerosis (CIMT).
Discussion
Our findings from this large community‐based black cohort show that current cigarette smoking and smoking intensity were associated with higher incidence of stroke, and this was dose dependent. In addition, smoking status and intensity were associated with increased CIMT (carotid atherosclerosis) after adjusting for age and sex.
Several studies have demonstrated increased risk of incident stroke in current smokers compared with never smokers. In the FHS (Framingham Heart Study), 4255 white participants were followed up for 26 years to assess the impact of cigarette smoking on the incidence of stroke, and current cigarette smoking was associated with an adjusted increased risk for stroke; the risk of stroke was higher as the number of cigarettes smoked increased. The relative risk of stroke in heavy smokers (>40 cigarettes/day) was twice that of light smokers (<10 cigarettes/day).3 However, all the participants of the FHS were white. FHS investigators reported adjusted HRs for stroke of 1.4 and 1.2 in male and female current smokers, respectively. Our results (HR of 2.44 in current versus never smokers) suggest smoking may have even greater impact in black current smokers, although these conclusions should be interpreted cautiously given the different time periods (and differing medical therapies; ie, statins) and different modeling.
In a prospective cohort study of 22 071 US male physicians (participants of the PHS [Physicians Health Study]) followed up for an average of 9.7 years, investigators found that current but not former cigarette smoking was significantly associated with an increased risk for stroke in men. Physicians currently smoking ≥20 cigarettes/day had relative risks of 2.71 and 1.46 for total nonfatal and fatal stroke, respectively, compared with never smokers after adjusting for risk factors for stroke.24 Our study showed a similar association between current smoking and increasing risk of stroke, whereas past smoking was not significantly associated with an increased risk of stroke. However, we did not distinguish between fatal and nonfatal stroke in our study and insomuch as the PHS had a large number of participants, the participants were all men and racial differences were not examined. In a prospective cohort study of 118 539 middle‐aged women (participants of the NHS [Nurses Health Study]) followed up for 8 years, the number of cigarettes smoked per day was associated positively with the risk of stroke. Compared with the women who were nonsmokers, those who smoked 1 to 14 cigarettes/day had an age‐adjusted relative risk of 2.2 (95% CI, 1.5–3.3), whereas those who smoked ≥25 cigarettes/day had a relative risk of 3.7 (95% CI, 2.7–5.1).25 Our study also showed an association between increasing smoking intensity and an increased risk of stroke. However, the participants of the NHS were primarily white women. In an ethnically diverse population of young men (aged 15–49 years), smoking was dose dependently associated with ischemic stroke.26 However, they did not specifically examine the independent effects of race in this relationship. Other studies have investigated the relationship between cigarette smoking and incident stroke.5, 27, 28, 29, 30, 31, 32, 33 Most of these studies showed a positive association between cigarette smoking and incident stroke, like our study.
Despite evidence from previous epidemiological and clinical studies that smoking is a risk factor for the development of stroke, there are limited data directly assessing the relationship between cigarette smoking and stroke in blacks. Because blacks have higher stroke rates, it is important to identify modifiable risk factors in blacks. To the best of our knowledge, our study is the first prospective study that has investigated the relationship between cigarette smoking and incident stroke solely among a large cohort of blacks while assessing multiple traditional risk factors for cardiovascular diseases and inflammation among groups subdivided by smoking status, intensity, and burden. We also investigated these relationships by measures of CIMT among groups subdivided by smoking status and intensity. Therefore, our findings have important implications considering that blacks are disproportionately affected more by stroke than any other racial group within the United States. Blacks are twice as likely to die from stroke as whites,2 and 16.5% of blacks are current smokers.34
Cigarette smoking is associated with elevated levels of inflammatory cytokines and endothelial damage, which could lead to the development of atherosclerosis and stroke.35, 36, 37, 38 Previous data have suggested that CRP (an inflammatory cytokine) is an independent predictor of the risk of future stroke.39, 40, 41, 42, 43 To determine the possible mechanisms by which smoking may cause stroke, we evaluated the relationship between cigarette smoking, CRP, and incident stroke. Current smoking and smoking intensity were associated with increased incident stroke after further adjustment for CRP. These findings suggest inflammation may play a role in the development of stroke in black smokers.
CIMT can predict future stroke events. Lorenz et al,21 in a meta‐analysis of 8 population‐based cohort studies, showed that every 0.1‐mm increase in CIMT was associated with a 13% to 18% increase in stroke events. Therefore, we assessed the relationships between smoking status and intensity with CIMT. Smoking status and intensity were associated with an increased mean of the bifurcation optimal average far wall of CIMT after controlling for age and sex. Our findings suggest that atherosclerosis could be a mechanism for the development of stroke in black smokers.
Our study is not without its limitations. First, the JHS was conducted within a single geographical area of blacks so our findings may not be generalizable to other racial groups or regions. Second, the self‐reported smoking status of participants in this study was not confirmed by urine cotinine levels, giving room for misclassification. Third, given that our study was observational, we cannot infer causality and we cannot exclude residual confounding. Fourth, we adjusted for confounders at visit 1, but acknowledge that smoking status and covariates may have changed between the baseline and when strokes occurred. In addition, we have a modest number of events; subgroup comparisons between current smoking levels (1–19 versus ≥20 cigarettes/day) and between current versus former smokers may be underpowered. Finally, CIMT was measured only at visit 1, which could limit our ability to show causality, and the number of participants with available CIMT data was limited (n=2614), which may also affect the interpretation of our results.
In conclusion, in a large prospective cohort of blacks, current cigarette smoking was associated with incident stroke in adjusted models. Furthermore, there was a dose‐dependent increased risk with increased smoking intensity. Overall, there was no significant difference in the risk of incident stroke between past and never smokers, suggesting that smoking cessation may have potential benefits in reducing the incidence of stroke in blacks. Our study builds on previous literature that predominantly investigated these relationships in whites. Blacks are disproportionately affected by cardiovascular disease, including stroke, and have worse outcomes compared with whites. Therefore, our findings have important public health implications. Furthermore, we investigated mechanistic factors and demonstrated that inflammation and atherosclerosis play important roles in the relationship between current smoking and stroke.
Sources of Funding
The JHS (Jackson Heart Study) is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I), and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I, and HHSN268201800012I) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute for Minority Health and Health Disparities. Dr Hall has also received support from National Institutes of Health (NIH)/National Institute of Diabetes and Digestive and Kidney Diseases 1K08DK099415‐01A1, NIH/National Institute of General Medical Sciences (NIGMS) P20GM104357, and NIH/NIGMS 5U54GM115428. The views expressed in this article are those of the authors and do not necessarily represent the views of the NHLBI, the NIH, or the US Department of Health and Human Services.
Disclosures
None.
Supporting information
Table S1
Acknowledgments
The authors would like to thank the staff and participants of the JHS (Jackson Heart Study).
(J Am Heart Assoc. 2020;9:e014990 DOI: 10.1161/JAHA.119.014990.)
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.119.014990
For Sources of Funding and Disclosures, see page 7.
References
- 1. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, et al; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e229–e445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yang Q, Tong X, Schieb L, Vaughan A, Gillespie C, Wiltz JL, King SC, Odom E, Merritt R, Hong Y, et al. Vital signs: recent trends in stroke death rates—United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;66:933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wolf PA, D'Agostino RB, Kannel WB, Bonita R, Belanger AJ. Cigarette smoking as a risk factor for stroke: the Framingham Study. JAMA. 1988;259:1025–1029. [PubMed] [Google Scholar]
- 4. Bonita R, Duncan J, Truelsen T, Jackson RT, Beaglehole R. Passive smoking as well as active smoking increases the risk of acute stroke. Tobacco Control. 1999;8:156–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shinton R, Beevers G. Meta‐analysis of relation between cigarette smoking and stroke. BMJ. 1989;298:789–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Howard VJ. Reasons underlying racial differences in stroke incidence and mortality. Stroke. 2013;44:S126–S128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McEvoy JW, Nasir K, DeFilippis AP, Lima JA, Bluemke DA, Hundley WG, Barr RG, Budoff MJ, Szklo M, Navas‐Acien A, et al. Relationship of cigarette smoking with inflammation and subclinical vascular disease: the Multi‐Ethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol. 2015;35:1002–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davis JW, Davis RF. Acute effect of tobacco cigarette smoking on the platelet aggregate ratio. Am J Med Sci. 1979;278:139–143. [DOI] [PubMed] [Google Scholar]
- 9. Renaud S, Blache D, Dumont E, Thevenon C, Wissendanger T. Platelet function after cigarette smoking in relation to nicotine and carbon monoxide. Clin Pharmacol Ther. 1984;36:389–395. [DOI] [PubMed] [Google Scholar]
- 10. Jackson Heart Study . JHS data access. https://www.jacksonheartstudy.org/Research/Study-Data/Data-Access. Accessed July 23, 2018.
- 11. Hall ME, Wang W, Okhomina V, Agarwal M, Hall JE, Dreisbach AW, Juncos LA, Winniford MD, Payne TJ, Robertson RM, et al. Cigarette smoking and chronic kidney disease in African Americans in the Jackson Heart Study. J Am Heart Assoc. 2016;5:e003280 DOI: 10.1161/JAHA.116.003280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kamimura D, Cain LR, Mentz RJ, White WB, Blaha MJ, DeFilippis AP, Fox ER, Rodriguez CJ, Keith RJ, Benjamin EJ, et al. Cigarette smoking and incident heart failure: insights from the Jackson Heart Study. Circulation. 2018;137:2572–2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. White WB, Cain LR, Benjamin EJ, DeFilippis AP, Blaha MJ, Wang W, Okhomina V, Keith RJ, Al Rifai M, Kianoush S, et al. High‐intensity cigarette smoking is associated with incident diabetes mellitus in black adults: the Jackson Heart Study. J Am Heart Assoc. 2018;7:e007413 DOI: 10.1161/JAHA.117.007413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu J, Butler KR, Buxbaum SG, Sung JH, Campbell BW, Taylor HA. Leptinemia and its association with stroke and coronary heart disease in the Jackson Heart Study. Clin Endocrinol (Oxf). 2010;72:32–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Keku E, Rosamond W, Taylor HA Jr, Garrison R, Wyatt SB, Richard M, Jenkins B, Reeves L, Sarpong D. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis. 2005;15:S6–62‐70. [PubMed] [Google Scholar]
- 16. Foraker RE, Greiner M, Sims M, Tucker KL, Towfighi A, Bidulescu A, Shoben AB, Smith S, Talegawkar S, Blackshear C, et al. Comparison of risk scores for the prediction of stroke in African Americans: findings from the Jackson Heart Study. Am Heart J. 2016;177:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, Skelton T, Jensen R, Sarpong D. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328:131–144. [DOI] [PubMed] [Google Scholar]
- 18. Villines TC, Hsu LL, Blackshear C, Nelson CR, Griswold M. Relation of carotid intima‐media thickness to cardiovascular events in black Americans (from the Jackson Heart Study). Am J Cardiol. 2017;120:1528–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima‐media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997;96:1432–1437. [DOI] [PubMed] [Google Scholar]
- 20. O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr; Cardiovascular Health Study Collaborative Research Group. Carotid‐artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22. [DOI] [PubMed] [Google Scholar]
- 21. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima‐media thickness: a systematic review and meta‐analysis. Circulation. 2007;115:459–467. [DOI] [PubMed] [Google Scholar]
- 22. De Syo D, Franjić BD, Lovricević I, Vukelić M, Palenkić H. Carotid bifurcation position and branching angle in patients with atherosclerotic carotid disease. Coll Antropol. 2005;29:627–632. [PubMed] [Google Scholar]
- 23. Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, Najjar SS, Rembold CM, Post WS; American Society of Echocardiography Carotid Intima‐Media Thickness Task Force . Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima‐Media Thickness Task Force: endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111; 189–190. [DOI] [PubMed] [Google Scholar]
- 24. Robbins AS, Manson JE, Lee IM, Satterfield S, Hennekens CH. Cigarette smoking and stroke in a cohort of U.S. male physicians. Ann Intern Med. 1994;120:458–462. [DOI] [PubMed] [Google Scholar]
- 25. Colditz GA, Bonita R, Stampfer MJ, Willett WC, Rosner B, Speizer FE, Hennekens CH. Cigarette smoking and risk of stroke in middle‐aged women. N Engl J Med. 1988;318:937–941. [DOI] [PubMed] [Google Scholar]
- 26. Markidan J, Cole JW, Cronin CA, Merino JG, Phipps MS, Wozniak MA, Kittner SJ. Smoking and risk of ischemic stroke in young men. Stroke. 2018;49:1276–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dagenais GR, Yi Q, Lonn E, Sleight P, Ostergren J, Yusuf S; HOPE Trial Investigators . Impact of cigarette smoking in high‐risk patients participating in a clinical trial: a substudy from the Heart Outcomes Prevention Evaluation (HOPE) trial. Eur J Cardiovasc Prev Rehabil. 2005;12:75–81. [PubMed] [Google Scholar]
- 28. Asplund K, Karvanen J, Giampaoli S, Jousilahti P, Niemelä M, Broda G, Cesana G, Dallongeville J, Ducimetriere P, Evans A, et al. Relative risks for stroke by age, sex, and population based on follow‐up of 18 European populations in the MORGAM Project. Stroke. 2009;40:2319–2326. [DOI] [PubMed] [Google Scholar]
- 29. Zhang Y, Galloway JM, Welty TK, Wiebers DO, Whisnant JP, Devereux RB, Kizer JR, Howard BV, Cowan LD, Yeh J, et al. Incidence and risk factors for stroke in American Indians: the Strong Heart Study. Circulation. 2008;118:1577–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Myint PK, Sinha S, Luben RN, Bingham SA, Wareham NJ, Khaw KT. Risk factors for first‐ever stroke in the EPIC‐Norfolk prospective population‐based study. Eur J Cardiovasc Prev Rehabil. 2008;15:663–669. [DOI] [PubMed] [Google Scholar]
- 31. Assmann G, Schulte H, Cullen P, Seedorf U. Assessing risk of myocardial infarction and stroke: new data from the Prospective Cardiovascular Münster (PROCAM) study. Eur J Clin Invest. 2007;37:925–932. [DOI] [PubMed] [Google Scholar]
- 32. Nakayama T, Yokoyama T, Yoshiike N, Zaman MM, Date C, Tanaka H, Detels R. Population attributable fraction of stroke incidence in middle‐aged and elderly people: contributions of hypertension, smoking and atrial fibrillation. Neuroepidemiology. 2000;19:217–226. [DOI] [PubMed] [Google Scholar]
- 33. Bhat VM, Cole JW, Sorkin JD, Wozniak MA, Malarcher AM, Giles WH, Stern BJ, Kittner SJ. Dose‐response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39:2439–2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Centers for Disease Control and Prevention . Current cigarette smoking among adults—United States, 2016. Morb Mortal Wkly Rep. 2018;67:53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34:509–515. [DOI] [PubMed] [Google Scholar]
- 36. Levitzky YS, Guo CY, Rong J, Larson MG, Walter RE, Keaney JF Jr, Sutherland PA, Vasan A, Lipinska I, Evans JC, et al. Relation of smoking status to a panel of inflammatory markers: the Framingham offspring. Atherosclerosis. 2008;201:217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tibuakuu M, Kamimura D, Kianoush S, DeFilippis AP, Al Rifai M, Reynolds LM, White WB, Butler KR, Mosley TH, Turner ST, et al. The association between cigarette smoking and inflammation: the Genetic Epidemiology Network of Arteriopathy (GENOA) study. PLoS One. 2017;12:e0184914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rost NS, Wolf PA, Kase CS, Kelly‐Hayes M, Silbershatz H, Massaro JM, D'Agostino RB, Franzblau C, Wilson PW. Plasma concentration of C‐reactive protein and risk of ischemic stroke and transient ischemic attack: the Framingham Study. Stroke. 2001;32:2575–2579. [DOI] [PubMed] [Google Scholar]
- 39. Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–979. [DOI] [PubMed] [Google Scholar]
- 40. Ridker PM, Buring JE, Shih H, Matias M, Hennekens CH. Prospective study of C‐reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–733. [DOI] [PubMed] [Google Scholar]
- 41. Jiménez MC, Rexrode KM, Glynn RJ, Ridker PM, Gaziano JM, Sesso HD. Association between high‐sensitivity C‐reactive protein and total stroke by hypertensive status among men. J Am Heart Assoc. 2015;4:e002073 DOI: 10.1161/JAHA.115.002073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhou Y, Han W, Gong D, Man C, Fan Y. Hs‐CRP in stroke: a meta‐analysis. Clin Chim Acta. 2016;453:21–27. [DOI] [PubMed] [Google Scholar]
- 43. Moon AR, Choi DH, Jahng SY, Kim BB, Seo HJ, Kim SH, Ryu SW, Song H, Kim TH. High‐sensitivity C‐reactive protein and mean platelet volume as predictive values after percutaneous coronary intervention for long‐term clinical outcomes: a comparable and additive study. Blood Coagul Fibrinolysis. 2016;27:70–76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


