Abstract
As the coronavirus 2019 (COVID-19) pandemic marches unrelentingly, more patients with cardiac arrhythmias are emerging due to the effects of the virus on the respiratory and cardiovascular (CV) systems and the systemic inflammation that it incurs, and also as a result of the proarrhythmic effects of COVID-19 pharmacotherapies and other drug interactions and the associated autonomic imbalance that enhance arrhythmogenicity. The most worrisome of all arrhythmogenic mechanisms is the QT prolonging effect of various anti-COVID pharmacotherapies that can lead to polymorphic ventricular tachycardia in the form of torsade des pointes and sudden cardiac death. It is therefore imperative to monitor the QT interval during treatment; however, conventional approaches to such monitoring increase the transmission risk for the staff and strain the health system. Hence, there is dire need for contactless monitoring and telemetry for inpatients, especially those admitted to the intensive care unit, as well as for outpatients needing continued management. In this context, recent technological advances have ushered in a new era in implementing digital health monitoring tools that circumvent these obstacles. All these issues are herein discussed and a large body of recent relevant data are reviewed.
Keywords: COVID-19, SARS-CoV-2, Myocarditis, Cardiac arrhythmias, Atrial fibrillation, Sudden cardiac death, Long QT syndrome, Torsade des pointes, Ventricular tachycardia, Ventricular fibrillation
Abbreviations: AAD, antiarrhythmic drug; AF, atrial fibrillation; APCs, atrial premature complexes; AZM, azithromycin; COVID-19, coronavirus 2019; CQ, chloroquine; cTn, cardiac troponin; CV, cardiovascular; CYP, cytochrome P450; ECG, electrocardiogram; HCQ, hydroxychloroquine; ICU, intensive care unit; LQTS, long QT syndrome; NSVT, non-sustained ventricular tachycardia; OOHCA, out-of-hospital cardiac arrest; SCD, sudden cardiac death; TdP, torsade des pointes; VAs, ventricular arrhythmias; VF, ventricular fibrillation; VPCs, ventricular premature complexes; VT, ventricular tachycardia
Introduction
The on-going pandemic of coronavirus disease 2019 (COVID-19) has created a global tumult [1]. According to current data, ~20-36% of patients with COVID-19 infection are afflicted by acute myocardial injury with an attendant higher mortality rate compared with those without cardiac injury, commensurate with the degree of cardiac troponin (cTn) elevation [2], [3], [4]. Furthermore, ~6-17% of patients develop cardiac arrhythmias (Table 1 ), including malignant ventricular arrhythmias (VAs) [5,6], with a higher prevalence (~44%) noted in patients admitted to the intensive care unit (ICU) [6]. Importantly, clinically stable patients may have a low prevalence of arrhythmias [7], however, critically ill patients are at much higher risk for cardiac arrhythmias [8].
Table 1.
Cardiac Arrhythmias Occurring in Patients with COVID-19 Infection.
| Sinus tachycardia |
| Sinus bradycardia |
| Conduction disturbances (AVB/BBB) |
| Atrial premature complexes |
| Atrial fibrillation |
| Supraventricular tachycardia |
| Ventricular premature complexes |
| Non-sustained ventricular tachycardia |
| Polymorphic ventricular tachycardia (Torsade des pointes) |
| Sustained ventricular tachycardia |
| Ventricular fibrillation |
| Pulseless electrical activity |
AVB = atrioventricular block; BBB = bundle branch block.
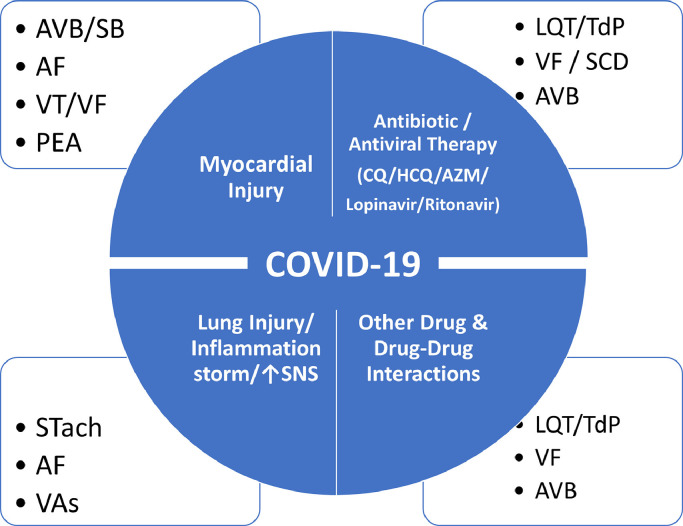
Cardiac arrhythmias, including life-threatening VAs, may be the consequence of direct effects of COVID-19 infection, but also of the deleterious effects of systemic illness and the adverse reactions to drugs employed in the treatment of this pandemic (Table 2 , Fig. 1 ) [5, [9], [10], [11]]. A recent study indicated that among 700 patients with COVID-19 (mean age 50±18 years, 45% men, 71% African American, 11% receiving care in the ICU), there were 9 cardiac arrests, 25 incident atrial fibrillation (AF) episodes, 9 bradyarrhythmias, and 10 non-sustained ventricular tachycardias (NSVTs) [5]. Arrhythmias occurring in patients admitted to the ICU included cardiac arrests (all 9 events of cardiac arrest occurred in this group), AF (odds ratio-OR 4.68 vs those not in the ICU) and NSVT (OR 8.92). Cardiac arrests were associated with acute, in-hospital mortality.
Table 2.
Mechanisms of Arrhythmogenicity in Patients with COVID-19 Infection.
| Acute myocardial injury / Myocarditis |
| Hypoxia |
| Systemic inflammation |
| Autonomic imbalance (SNS overactivity / virus-induced vagal nerve injury) |
| Electrolyte abnormalities |
| QT prolonging drugs (anti-COVID pharmacotherapies / AADs / other agents) |
| Drug-drug interactions |
| Cardiovascular comorbidities (hypertension, coronary artery disease, cardiomyopathy) |
AADs = antiarrhythmic drugs; SNS = sympathetic nervous system.
Fig. 1.
The schema illustrates the various arrhythmias encountered in patients with COVID-19 infection as a consequence of the virus infection affecting the heart and lung and/or producing systemic inflammation, the adverse (proarrhythmic) effects of COVID therapies and the drug-drug interactions that may occur (see text for discussion). AF = atrial fibrillation; AVB = atrioventricular block; LQT = long QT interval; PEA = pulseless electrical activity; SB = sinus bradycardia; SCD = sudden cardiac death; SNS = sympathetic nervous system; STach = sinus tachycardia; TdP = torsade des pointes; VAs = ventricular arrhythmias; VF = ventricular fibrillation; VT = ventricular tachycardia.
Among 187 patients with confirmed COVID-19, 52 (27.8%) exhibited myocardial injury as indicated by elevated cardiac troponin T (cTnT) levels [12]. During hospitalization, 11 (5.9%) patients developed ventricular tachycardia (VT)/ventricular fibrillation (VF); patients with elevated cTnT levels had more frequent VAs (17.3% vs 1.5%; p<0.001), compared with those with normal cTnT levels. A recent single-day snapshot survey of 132 stable patients with COVID-19 showed a 9% (12/132) incidence of arrhythmias, limited to AF in 8 and supraventricular tachycardia (SVT) in 4 patients [7]. A Heart Rhythm Society (HRS) online survey of electrophysiology professionals (n=1197) indicated that AF was the most commonly reported tachyarrhythmia (21%), whereas severe sinus bradycardia (8%) and complete heart block (8%) were the most common bradyarrhythmias in hospitalized patients with COVID-19 [13]. Ventricular tachycardia/VF arrest and pulseless electrical activity were reported by 4.8% and 5.6% of respondents, respectively. A meta-analysis of 17 retrospective cohort studies comprising 5,815 patients with COVID-19 showed that the pooled incidence was 9.3% for cardiac arrhythmia (5.7% for cardiac arrest) [14].
In this review, we present current data about the whole spectrum of cardiac arrhythmias encountered in patients with COVID-19 infection, either attributable to the effect of the virus itself on the cardiovascular (CV) and the respiratory system and/or to the effects of the treatments that these patients receive in combination with autonomic imbalance that is incurred by this unrelenting pandemic.
Acute myocardial injury and arrhythmias
As mentioned, in patients with evidence of acute myocardial injury, the prevalence of cardiac arrhythmias is higher compared to patients without myocardial injury [12]. In a recent retrospective cohort study, among 1284 patients with severe COVID-19, 1159 had a cTnI level measured upon hospital admission, of whom 170 (14.7%) had positive results showing cardiac injury [15]. In patients with cardiac injury, mortality was higher compared to patients without cardiac injury (71.2% vs. 6.6%, p<0.001). Arrhythmias were found in 44 of the 170 patients with cardiac injury (25.9%), including 6 patients with VT or VF, all of whom died [15]. A recent meta-analysis of 23 studies including 4631 COVID-19 patients showed that patients with cardiac injury and newly occurring arrhythmias were at higher risk of developing severe disease or requiring ICU admission (relative risk-RR ~13, p<0.001) [16].
Sinus tachycardia
Sinus tachycardia is the most common rhythm disturbance in patients with COVID-19 infection due to multiple reasons, such as fever, respiratory insufficiency/hypoxemia, hemodynamic compromise, fear/anxiety, pain, and several other physical and emotional symptoms [17].
Bradycardia/conduction disturbances
According to a retrospective series of 4 patients, transient sinus bradycardia lasting 1-14 days is a possible manifestation of COVID-19, hence another reason for close monitoring [18]. There may be many reasons for bradycardia, but severe hypoxia, inflammatory injury of the sinus node by circulating cytokines, and exaggerated response to medications are possible triggers. Interestingly, bradycardia has been suggested as a warning sign of the onset of a serious cytokine storm.
According to a retrospective cohort study of 756 COVID-19 patients, multivariable logistic regression indicated that, among other ECG abnormalities, the presence of one or more atrial premature contractions (APC)s (odds ratio - OR=2.57, p=0.01), a right bundle branch block (RBBB) or intraventricular block (IVB) (OR=2.61, p=0.002), increased the odds of death [19].
Another study analyzing the ECGs of 75 COVID-19 patients showed that abnormal PR interval behavior (paradoxical prolongation or lack of shortening) with increasing heart rate was associated with increased risk of death (29.7% vs 7.9%, p=0.019) and need for endotracheal intubation (43.2% vs. 21.1%, p=0.05) compared to patients with PR interval shortening [20].
Atrial fibrillation
According to a recent survey of electrophysiology professionals, atrial fibrillation (AF) was the most commonly encountered cardiac arrhythmia observed in patients with COVID-19 infection [13]. Several mechanisms could be involved in the pathogenesis of AF in these patients; virus-induced cardiac injury that could lead to perimyocarditis, hypoxemia frequently occurring in these patients, systemic infection, common occurrence of the COVID-19 infection in older patients who are already susceptible to AF, and sympathetic nervous system overactivity could all account for such a high incidence of this arrhythmia in this particular population [13,21].
Guidance on acute management of AF. In cases of AF-associated hemodynamic compromise, as done in all cases of hemodynamically unstable arrhythmias, synchronized direct current cardioversion should be used to restore sinus rhythm [22]. In all other cases, one needs to initially proceed with a rate control strategy with use of a beta-blocker, when there is no contraindication (e.g. bronchospasm, acute heart failure), a calcium channel blocker (in the absence of heart failure) and/or digoxin. In cases of heart failure, digoxin and/or amiodarone may be used to achieve rate control. For new-onset AF within the last 48 hours, restoring sinus rhythm is the next target. This can be achieved with use of class IA, IC or III antiarrhythmic drugs (AADs) with the selection of the appropriate agent made as based on the presence (where only amiodarone seems to be relatively safe) or absence of underlying structural heart disease (where all other options are available with the caveats being detailed in the discussion that follows below), also taking into account drug interactions with COVID pharmacotherapies that are in use. A major concern in using specific AADs relates to the baseline measurement of the QT interval and the co-administration of QT-prolonging drugs (see discussion below). Most importantly, all AF patients should be receiving prophylactic anticoagulation therapy with intravenous heparin.
Impact of national lockdown on new-onset AF diagnosis. Another aspect of the impact of national COVID-19 lockdowns on the diagnosis of AF has been recently reported by a Danish study [23]. Using Danish registries, the number of patients receiving a new-onset AF diagnosis during the first 3 months of 2019 and 2020 was compared. A lower incidence of new-onset AF during the 3 weeks of lockdown was noted compared with the corresponding weeks in 2019 (incidence rate ratios - RRs for the 3 weeks: 0.66, 0.53, and 0.41). There was a 47% drop in total numbers (562 vs. 1053) [23]. Patients diagnosed during lockdown were younger and with a lower CHA2DS2-VASc score, while history of cancer, heart failure, and vascular disease were more prevalent. During lockdown, 30 (5.3%) patients with new-onset AF suffered an ischemic stroke and 15 (2.7%) died, compared with 45 (4.3%) and 14 (1.3%) patients during the corresponding 2019 period, respectively. The authors concluded that following a national lockdown in Denmark, a 47% drop in registered new-onset AF cases was observed, indicating that the risk of undiagnosed AF patients developing complications could potentially translate into poorer outcomes in patients with AF during the COVID-19 pandemic.
Ventricular arrhythmias
In the setting of acute myocardial injury and acute myocarditis in patients with COVID-19 infection, various and serious ventricular arrhythmias (VAs) may occur [15]. Other important triggers include the severe respiratory insufficiency and the systemic inflammation incurred by COVID-19 infection, as well as the proarrhythmic effects of COVID therapies and other drug interactions and also the autonomic imbalance superimposed in patients afflicted by the disease [5, 9]. Furthermore, hypoxemia which is common in these patients and electrolyte disturbances occurring for various reasons in this group of patients may aggravate arrhythmogenicity. Depending on pre-existing or currently emerging CV disease, various VAs may be encountered, including ventricular premature complexes (VPCs), non-sustained VT (NSVT), and sustained VT/VF. Special attention is required for the development of polymorphic VT in the form of torsade des pointes (TdP) in the setting of QT prolongation, either pre-existing or acquired and induced by drugs, especially when combination therapies are employed that are potentially proarrhythmic [24].
Acute myocardial injury noted in ~15-30% of COVID-19 patients can be the inciting factor for various VAs [1,25]. Among 187 patients with confirmed COVID-19, malignant VAs (VT/VF) developed in 11 (5.9%) patients; during hospitalization, patients with elevated cTn levels had more frequent malignant arrhythmias (17.3% vs 1.5%) [12]. A recent retrospective cohort study of 1284 patients with severe COVID-19 indicated that among 1159 having a cTn level measured on admission, with 170 (14.7%) showing cardiac injury, arrhythmias developed in 44 of the 170 (25.9%) patients, including 6 patients with VT or VF, all of whom died [15].
Critically ill COVID-19 patients often have comorbidities that can increase the risk for malignant VAs. These include electrolyte abnormalities (hypokalemia, hypomagnesemia), fever, an inflammatory state, and most importantly, COVID-19 pharmacotherapies that are potentially proarrhythmic as they prolong the QT interval and may thus trigger TdP and sudden cardiac death (SCD) [26]. On the other hand, the acute myocardial injury induced by the virus could also independently prolong the QT interval. According to a recent report of a Kawasaki-like syndrome temporally associated with COVID-19 infection in 21 children, among whom myocarditis was diagnosed in 16 (76%) patients (left ventricular ejection fraction-LVEF range 10–57%), 2 of these 16 patients displayed important ECG changes that included QT interval prolongation and occasional VAs not attributable to any QT-prolonging drug [27].
In-hospital cardiac arrest. As mentioned, among 700 patients hospitalized with COVID-19 infection, all 9 (1.3%) cardiac arrests occurred among patients admitted to the ICU [5]. In a retrospective cohort study, in-hospital VT/VF occurred in 6 of 170 (3.5%) patients with cardiac injury, all of whom died [15].
Out-of-hospital cardiac arrest (OOHCA). A recent Italian study compared all the consecutive out-of-hospital cardiac arrests (OOHCA) in the 2 months following the first documented case of COVID-19 in the region with those which occurred in the same time frame in 2019 [28]. The cumulative incidence of COVID-19 from 21 February to 20 April 2020 in the study territory was 956 COVID-19/100 000 inhabitants and the cumulative incidence of OOHCA was 21 cases/100 000 inhabitants, with a 52% increase as compared with 2019 (490 OOHCAs in 2020 vs. 321 in 2019) (p<0.001). The authors concluded that the increase in OOHCAs in 2020 is significantly correlated to the COVID-19 pandemic and is coupled with a reduction in short-term outcome.
A French study comparing the 521 OOHCAs of the pandemic period to the mean of the 3052 total over 6 weeks in the non-pandemic period indicated that the maximum weekly OOHCA incidence increased from 13.42 to 26.64 per million inhabitants (p<0.0001), before returning to normal in the final weeks of the pandemic period [29]. There was a higher rate of OOHCA at home (90.2% vs 76.8%; p<0.0001), less bystander cardiopulmonary resuscitation (47.8% vs 63.9%; p<0.0001) and shockable rhythm (9.2% vs 19.1%; p<0.0001), and longer delays to intervention (median 10.4 min vs 9.4 min; p<0.0001). The proportion of OOHCA patients admitted alive decreased from 22.8% to 12.8% (p<0.0001) in the pandemic period. After adjustment for confounders, the pandemic period remained significantly associated with lower survival rate at hospital admission (odds ratio 0.36; p<0.0001). COVID-19 infection accounted for about one third of the increase in OOHCA incidence during the pandemic.
Drug-induced prolongation of QTc interval and torsade des pointes
Several agents employed for treating COVID-19 infection may prolong the QT interval and lead to polymorphic VT in the form of TdP (Table 3 ). Chloroquine/hydroxychloroquine and azithromycin, which have been recently used for potential prophylaxis or treatment for COVID-19 infection, are listed as definite causes of TdP at crediblemeds.org [26]. According with the FDA, azithromycin, other macrolides, and fluoroquinolones can cause lethal arrhythmias as a potential consequence of QT-interval prolongation [30].
Table 3.
QT-Prolonging Drugs in COVID-19 Infection.
| Antibiotics | Chloroquine/Hydroxychloroquine |
| Macrolides (Azithromycin) | |
| Quinolones | |
| Antiviral agents | Lopinavir/Ritonavir |
| Favipiravir | |
| Tocilizumab | |
| Fingolimod | |
| Anesthetics | Propofol |
| Antiemetics | Domperidone |
| Antiarrhythmics | Class IA |
| Class III | |
| Antipsychotics | Haloperidol |
Chloroquine / hydroxychloroquine
Chloroquine (CQ) and hydroxychloroquine (HCQ) have been used for treatment and prophylaxis of malaria, while they have also been employed for treatment of amebiasis that is occurring outside the gastrointestinal tract, rheumatoid arthritis, and lupus erythematosus. These agents were also found to have antiviral effects and have been proposed for the treatment of COVID-19 infection [31]. However, both these agents can be proarrhythmic by prolonging the QT interval and potentially initiating life-threatening VAs including TdP; they can also cause QRS widening. Chloroquine interacts with multiple cardiac ion channels including the human ether-a-go-go-related gene (hERG) potassium channel; a reduction in hERG channel potassium current is the main cause of acquired drug-induced long QT syndrome. Recent experimental data indicated that HCQ markedly increases the action potential dispersion and results in the development of repolarization alternans and initiates polymorphic VT [32].
Preliminary findings from a recent study suggested that the QTc prolonging effect of CQ is dose-dependent [33]. Among 81 patients enrolled with COVID-19 infection, 41 (50.6%) were allocated to high-dosage group (i.e., 600 mg CQ bid for 10 days) and 40 (49.4%) to low-dosage group (i.e., 450 mg bid on day 1 and qd for 4 days). Lethality until day 13 was 39% in the high-dosage group (16 of 41) and 15% in the low-dosage group (6 of 40). The high-dosage group presented more instance of QTc interval >500 ms (18.9%) compared with the low-dosage group (11.1%). Respiratory secretion at day 4 was negative in only 6 of 27 patients (22.2%). The authors suggested that the higher CQ dosage should not be recommended for critically ill patients with COVID-19 because of its potential safety hazards, especially when taken concurrently with azithromycin and oseltamivir.
A recent disproportionality analysis of HCQ-associated CV adverse reactions using the FDA adverse event reporting system (FAERS) database of >11,901,836 datasets and 10,668,655 patient records indicated that HCQ was associated with higher reporting odds ratios (ROR) of TdP (ROR: 3.05; 95% CI: 2.30 to 4.10), complete atrioventricular (AV) block (ROR: 2.30; 95% CI: 1.55 to 3.41) and QT prolongation (ROR: 2.09; 95% CI: 1.74 to 2.52) [9]. QT prolongation and TdP are more frequent with high doses for a comparatively short period and represent the most common HCQ-associated side-effects
A systematic review of data on 1515 COVID-19 patients showed that ~10% of COVID-19 patients treated with CQ/HCQ developed QT prolongation [34]. Ventricular arrhythmias developed in 2 COVID-19 patients from a group of 28 treated with high-dose CQ. The authors suggest daily ECG monitoring and other risk mitigation strategies to be adopted in order to prevent possible arrhythmic side-effects.
Macrolide antibiotics
Azithromycin (AZM) also can cause modest QT interval prolongation, but not through potent hERG channel blockade, rather when used chronically through an increase in peak and late cardiac sodium current to cause potential loading of cardiomyocytes with sodium and calcium to produce calcium overload. Advanced age and female gender are considered risk factors [26]. Azithromycin can also provoke non-pause–dependent polymorphic VT in the absence of QT prolongation [35,36].
After reviewing the data of AZM regarding risk of QT prolongation and associated TdP, the FDA revised AZM product labels advising against its use in patients with known risk factors such as QT-interval prolongation, hypokalemia, hypomagnesemia, bradycardia, or use of certain QT-prolonging antiarrhythmic agents, including class IA (e.g., quinidine and procainamide) and class III (e.g., dofetilide, amiodarone, and sotalol) agents [30].
Antiviral agents
The combined antiviral regimen of ritonavir/lopinavir, approved for human immunodeficiency virus (HIV) infection, was also considered to be able to suppress SARS-CoV-2 replication [11,37]. Lopinavir is metabolized by the hepatic cytochrome P450 system (CYP3A) [38]; it also inhibits drug transporters such as P-glycoprotein (Pgp) [11]. Thus, ritonavir/lopinavir may increase plasma concentrations of drugs primarily metabolized by CYP3A or substrates of these drug transporters. Ritonavir/lopinavir may require dose reductions or avoidance of CYP3A-mediated drugs such as rivaroxaban and apixaban. Ritonavir/lopinavir has also been shown to cause QT and PR interval prolongation or occasionally second- or third-degree AV block, particularly in patients with underlying structural heart disease and preexisting conduction system abnormalities [11].
Due to its competitive inhibition of the RNA-dependent RNA polymerase, favipiravir is being evaluated in treating patients with COVID-19, alone or in combination therapies; the risk for QT interval prolongation by favipiravir is considered to be low [11].
Other agents. Fingolimod is an immunomodulator and immunosuppressant which reduces lymphocyte migration and is used in the treatment of multiple sclerosis [39]; it has been proposed as a potential adjuvant therapeutic agent against COVID-19 [11]. Fingolimod has L-type calcium channel blockade effect causing prolongation of PR, RR, and QT interval. It also activates acetylcholine-dependent potassium channels (IKach) in sinoatrial node causing dose-dependent bradycardia [40]. Thus, fingolimod increases the risk of bradycardia and heart block through L-type calcium channel and IKach blockade [41].
Combined therapies
Treatments employed for COVID-19 may increase arrhythmia risk, particularly the risk for VAs, through drug interactions. Drug combinations can lead to greater prolongation of cellular action potential duration, analogous to QT prolongation, compared with single drug therapies [24]. The combination effect can result from both pharmacokinetic and pharmacodynamic drug interactions. Importantly, females with pre-existing CV disease seem to be more susceptible to drug-induced arrhythmias, compared to males with CV disease or healthy persons of either gender.
An online survey of electrophysiology professionals revealed that 60 of 489 respondents (12.3%) reported having to discontinue therapy with HCQ + AZM due to significant QTc prolongation and 20 (4.1%) reported cases of TdP in patients on HCQ/CQ and AZM [13]. Amiodarone was the most common antiarrhythmic drug used for VA management.
Among 98 (73 COVID-19 positive, 25 suspected) patients studied (age 62±17 years, 61% male), 28% received AZM, 10% HCQ, and 62% received both drugs [42]. Baseline mean QTc was 448±29 ms and increased to 459±36 ms (p=0.005) with medications. Significant prolongation was observed only in men (18±43 ms vs -0.2±28 ms in women, p=0.02); 12% of patients reached critical QTc prolongation (maximum QTc ≥500 ms if QRS <120 ms or QTc ≥550 ms if QRS ≥120 ms, or QTc increase of ≥60 ms). Changes in QTc were highest with the combination compared to either drug, with much greater prolongation with combination vs. AZM (17±39 vs. 0.5±40 ms, p=0.07). No patients manifested TdP.
Another recent cohort study of 201 patients treated for COVID-19 with CQ/HCQ reported that 10 (5%) patients received CQ, 191 (95%) received HCQ and 119 (59.2%) also received AZM [43]. Although the maximum QTc during treatment was significantly longer in the combination group vs the monotherapy group (470.4±45.0 ms vs. 453.3±37.0 ms, p=0.004), TdP was not observed in the entire population and there were no arrhythmogenic deaths reported. A study of 22 COVID patients receiving combined HCQ/AZM therapy indicated longer QTc-interval than before therapy (450 vs 426 ms, p=0.02); 4 patients with a QTc ≥480 ms had higher values of transaminases (p<0.01) compared with those with QTc < 480 ms [44]. At 24 h Holter ECG monitoring, 1 COVID-19 patient and no control had ≥1 run of NSVT (p=0.4). No patients showed "R on T" VPCs. Analysis of 24 h QTc dynamics revealed that COVID-19 patients had higher QTc values than controls, with no significant hourly variability. Therapy with HCQ and AZM prolongs QTc interval in patients with COVID-19, particularly in those with high levels of transaminases.
Interestingly, in non-COVID patients, a retrospective cohort study identified only two SCD/VA events among >145,000 combination users (CQ/HCQ plus AZM) [45]. However, the doses were lower in this study compared to doses used in COVID-patients, drugs were not used acutely in a hospital setting as currently done for COVID patients, fewer cardiac patients received the drugs, all suggesting an attenuated risk for cardiac arrhythmias in this particular cohort.
Nevertheless, when all measures and precautions are taken (Table 4 ), the incidence of QT prolongation and the TdP-event rate may remain low. In a recent study of 73 patients with COVID-19 infection (mean age 62±14 years, male 67%), HCQ/AZM was initiated only if baseline QTc was ≤ 480ms and potassium level >4.0 mmol/L [46]. Two patients (2.7 %) were not eligible for drug initiation (QTc ≥ 500 ms). Baseline average QTc was 415±29 ms and increased to 438±40 ms after 48 h of combined therapy. The treatment had to be stopped because of significant QTc prolongation in 2 (2.8 %) patients. No drug-induced TdP, nor death was observed. In this specific population, HCQ/AZM could not be initiated or had to be interrupted in <6% of the cases.
Table 4.
Measures to Prevent Arrhythmias in Patients with COVID-19 Infection.
| • Withhold QT prolonging drugs in patients with baseline QTc > 500 ms or with known LQTS |
| • Withdraw QT-prolonging drugs when QTc increases to >500 ms or if QTc is prolonged by >60 ms compared to baseline measurement |
| • Do not use chloroquine/hydroxychloroquine, azithromycin, other macrolides, fluoroquinolones, lopinavir/ritonavir or favipiravir in patients with known risk factors such as prolonged QTc, hypokalemia, hypomagnesemia, bradycardia, or concomitant use of certain QT-prolonging antiarrhythmic drugs, including class IA (e.g., quinidine and procainamide) and class III (e.g., dofetilide, amiodarone, and sotalol) agents |
| • Maintain K+ level to >4 mEq/L and Mg++ level to >2 mg/dL |
| • Monitor QTc via ECG or preferably via telemetry monitor or smart phone measurements |
QTc monitoring
Congenital long QT syndrome (LQTS) with a prevalence of 1:2000 in the general population, may often be asymptomatic and if an ECG has not been recorded, it will remain unknown to the affected person and the first manifestation may be SCD, usually triggered by a drug [47]. Furthermore, silent genetic variants or “forme fruste” of congenital LQTS encountered in ~4% of people, may render a person vulnerable to QT prolongation, TdP and SCD [48]. Therefore, a large number of healthy individuals will be at an increased risk of a drug-induced LQTS.
Data suggest that 1 in 13 African Americans may be at a higher risk of drug-induced TdP, during the COVID-19 pandemic due to clustering of intrinsic genetic susceptibility (i.e., 8% exclusive occurrence of the proarrhythmic ion channel variant p.Ser1103Tyr-SCN5A), acquired risk factors (e.g., electrolyte disturbances and QTc-prolonging drug use), and COVID-19–specific risk factors (e.g., profound hypoxemia and cytokine storm) [49].
A heart rate-corrected QT (QTc) interval is measured with use of various formulas, among which the Bazett's correction formula is most commonly used: QTc = QT/√RR(sec). QTc is defined as prolonged when it exceeds 450 ms in males and 460 ms in females as measured preferably in lead II or V5 on a standard 12-lead ECG [50]. A prolonged QTc predisposes to polymorphic VT in the form of TdP, that may degenerate into VF and SCD. For the wide-QRS adjusted QTc, methods that have been suggested include the JT adjustment obtained as QTc–QRS [51] or subtracting 48.5% of the QRS duration from the measured QT [52].
For patients receiving QT-prolonging drugs, it is imperative to monitor the QTc interval during treatment (Table 4). Traditionally, this can be accomplished by obtaining a 12-lead ECG, however, in the era of the COVID-19 pandemic, this poses a certain risk and puts considerable strain on medical personnel and the health system [53]. Many telemetry systems are equipped with features of real time QTc monitoring and could be used in hospitalized patients and those managed in the ICU setting. In addition, smart phone heart monitors are also capable of providing remote accurate QTc measurements [54]. In this context, AliveCor has recently received clearance from the FDA to market the KardiaMobile-6L device, a previously FDA-approved device for AF detection, for QTc monitoring of COVID-19 patients treated with QT prolonging drugs such as CQ/HCQ [55]. Similarly, the Apple Watch ECG, an FDA-cleared device for detecting AF, was recently studied for QT monitoring; when lead I, the lead recorded by the Apple Watch, proves suboptimal for measuring QT interval, other leads can be used by placing the smartwatch on the left ankle or chest; Apple Watch ECG tracings obtained in 100 patients allowed for adequate QT measurements when the smartwatch was worn on the left wrist in 85% of patients and in 94% of patients when the smartwatch was moved to alternative positions (left ankle or chest) [56].
Those COVID-19 patients with a QTc ≥500 ms, either during baseline measurement or while on therapy, are at increased risk; also, at risk are patients with a change of QTc of >60 ms during treatment with QT prolonging drugs. In such cases, QT-prolonging drugs should be avoided or when used, should be discontinued or the dose reduced, while other potential causes of QT prolongation (e.g. electrolyte abnormalities, other QT prolonging drugs, etc.) should be sought and corrected, if at all possible (Table 4). These patients should be closely monitored for possibly occurrence of TdP.
When using the 12-lead ECG machine for QT measurement and monitoring, one machine should be designated for data acquisition and a limited number of ECG technicians/personnel should be involved to minimize staff exposure and personal protective equipment (PPE) utilization. This approach also entails limiting QTc assessments to those absolutely necessary. A plausible scenario would include an initial on-treatment QTc measurement followed by repeat measurements initially at 2–4 h after the first dose and then at 48 h and 96 h. With the smart phone or telemetry approach, ECG technician exposure risk and frequent PPE use is drastically curtailed, and the QTc could be assessed per shift, enabling earlier discovery of QT prolongation occurrence and prompt implementation of countermeasures [53].
Management of torsade des pointes (TdP)
Intravenous magnesium sulfate is the first-line pharmacologic therapy in TdP (Table 5 ) [57]. In cases of TdP degenerating into VF, prompt electrical cardioversion should be employed. However, TdP is known to keep recurring for a while until further measures are taken. Importantly, increasing the heart rate seems to be crucial to suppress recurring TdP. This can be done pharmacologically, e.g. with isoproterenol, used as a temporizing measure, until overdrive pacing is established with the insertion of a temporary pacing wire [58]. Ventricular pacing rates of 90-110 bpm are usually sufficient to suppress the arrhythmia [57,58]. Of course, the offending agent should be promptly stopped.
Table 5.
Management of Torsade des Pointes (TdP).
| • Intravenous administration of 2 g magnesium sulfate (MgSO4)* |
| • Isoproterenol infusion to increase the heart rate until a temporary pacemaker wire is inserted† |
| • Overdrive temporary pacing at 90–110 bpm |
| • Direct current (DC) cardioversion if TdP has degenerated into ventricular fibrillation (VF) |
| • Promptly halt offending agent(s) / correct electrolyte abnormalities |
This dose may be repeated, if needed, at 5-15 min. Alternatively, an infusion of 1-4 gm/h may be started to keep the magnesium levels >2 mmol/L. Once the magnesium level reaches ~ 3 mmol/L, the infusion can be stopped to avoid toxicity noted with levels >3.5 mmol/L. Serum potassium should be maintained at 4.5-5 mmol/L.
Isoproterenol is given at an infusion rate of 1-4 μg/min titrated to maintain a heart rate of ~100 bpm. Isoproterenol is, however, contraindicated in patients with congenital LQTS, as it may paradoxically prolong the QT interval.
Interactions of antiarrhythmic drugs with COVID-19 pharmacotherapy
Many COVID-19 pharmacotherapies have actions including potassium channel (IKr) blockade, inhibition of cytochrome P450 isoenzymes (CYPs) and P-glycoprotein inhibition that are responsible to drug-drug interactions with antiarrhythmic drugs (AADs) [59]. Class IA agents, quinidine and procainamide, have been used for AF conversion; quinidine has also been used for AF prophylaxis, while procainamide has been used for VT conversion; however, lately, quinidine has not been available for use in many countries [60]. The third IA agent, disopyramide, has been practically phased out of use. Quinidine, a sodium (INa) and potassium channel (IKr) blocker, and therefore a QT interval prolonging AAD, is primarily metabolized by CYP3A4 [61]. Plasma concentration of quinidine can be decreased with CYP3A4 inducers (tocilizumab and sarilumab) and can be increased with CYP3A4 inhibitors (lopinavir/ritonavir) [62]. Procainamide, an INa and IKr blocker, used intravenously for acute arrhythmia conversion in patients with AF, including Wolff-Parkinson-White Syndrome presenting with pre-excited AF, and also in patients with wide-complex or ventricular tachycardia, is partially metabolized by CYP2D6 and mainly (60%) excreted by the kidney [63]. Plasma concentration of procainamide can be decreased with CYP2D6 inducers (tocilizumab and sarilumab) [59].
Any Class IA AAD should be used with caution when combined with CQ/HCQ, AZM, fingolimod, or lopinavir/ritonavir. Obtaining baseline and serial QT intervals following initiation of an AAD is recommended.
Class IC agents, flecainide and propafenone, mainly used as prophylaxis for AF recurrences, are use-dependent INa blockers with moderate negative inotropic effect. These agents prolong the QRS complex with minimal effect on the QT interval [61]. However, there are case reports where flecainide was shown to prolong the QT interval and lead to TdP [64]. Importantly, class IC agents have been implicated with proarrhythmia leading to SCD in patients with underlying structural heart disease [65]. Flecainide and propafenone are predominantly metabolized by CYP2D6. Due to their notorious proarrhythmic effect, they are only used in patients without coronary artery disease or structural heart disease [66]. Because of possible increases in plasma concentration of flecainide when co-administered with CQ/HCQ and lopinavir/ritonavir (CYP2D6 inhibitors) and/or the potential QT prolonging effects of these drugs and also of AZM, serial ECG monitoring is recommended before and after initiating drug therapy [59].
Due to their grave arrhythmogenic potential and negative inotropic effect, great caution should be exercised in their use, if at all, in COVID-19 patients, especially in critically ill COVID-19 patients, who are prone to or have already developed myocarditis and heart failure [1]. Due to their interactions with CYP2D6 inducers (tocilizumab and sarilumab) and CYP2D6 inhibitors (litonavir/ritonavir), close ECG monitoring is required.
Beta-blockers may be used for rate-control in AF with COVID-19 infection [67]. However, these agents may interact with lopinavir/ritonavir, and produce PR prolongation, second-degree, and third-degree AV block [59]. Furthermore, lopinavir/ritonavir, as well as CQ and HCQ, may increase carvedilol and metoprolol serum concentration through CYP2D6 inhibition. Finally, beta-blockers should be avoided in patients developing acute heart failure symptoms or bronchospasm [68].
Among the class III agents, amiodarone, a multichannel blocker is the most effective and a most commonly used AAD, despite its well-known toxicity, as it confers the least proarrhythmic effect; the drug prolongs QT but it rarely causes TdP (<0.5%) [61, 69]. Amiodarone is used both for atrial arrhythmia (AF) and ventricular arrhythmia prevention. It is preferred for AF rate and rhythm control in critically ill COVID-19 patients with myocardial involvement or borderline blood pressure. Surveillance for liver, lung, and thyroid toxicity is recommended, especially during long-term therapy [70, 71]. In COVID-19 patients with severe pneumonia requiring prolonged mechanical ventilation, there may be a concern for amiodarone use, especially for patients who have already been on chronic therapy with the drug due to its known pulmonary toxicity [70]. Amiodarone should be used with caution, if at all, in patients receiving other QT prolonging drugs, such as lopinavir/ritonavir and/or HCQ/AZM.
The use of other class III agents, like dronedarone sharing similar pharmacokinetics with amiodarone [72,73], or dofetilide/ibutilide (IKr blockers) [74] is generally limited, and more so in COVID-19 patients already receiving CQ/HCQ, macrolides, or lopinavir/ritonavir due to their intrinsic dose-dependent QT-prolonging effects. Nevertheless, the use of ibutilide may be an option for conversion of acute symptomatic AF. Sotalol, a dose-dependent IKr blocker with moderate β-blockade effect [61], is renally excreted and thus it should be used with great caution in the presence of potentially nephrotoxic agents, like lopinavir/ritonavir, whilst the drug is also highly proarrhythmic due to its QT prolonging effect and should be avoided in patients receiving other QT prolonging drugs, such as lopinavir/ritonavir, CQ/HCQ, and/or AZM; sotalol is also contraindicated in patients with myocardial injury or compromised left ventricular dysfunction [75]. Class III AADs are generally contraindicated in patients who are treated with fingolimod because of QT prolongation and risk of TdP [41]. Finally, with regards to vernakalant, a class III, albeit atrial-selective, agent, one should be cautious in COVID-19 patients prone to hemodynamic compromise, due to its known bradycardic and hypotensive effects [76].
Calcium channel blockers, verapamil and diltiazem, are used as first line rate-control agents in AF, except for those with heart failure and/or left ventricular dysfunction due to their negative inotropic effect [66,67]. Diltiazem is metabolized by CYP2C19 and CYP3A4. Lopinavir/ritonavir may cause prolonged PR, and second- or third-degree AV block when used with calcium channel blockers [59]. Lopinavir/ritonavir can increase plasma levels of calcium channel blockers through CYP3A4 inhibition and should be closely monitored [77].
Digoxin may be used in heart failure patients given its lack of negative inotropic effect and in patients with marginal blood pressure who do not tolerate calcium channel blockers or β-blocker [66]. Lopinavir/ritonavir increases serum digoxin concentration and toxicity through inhibition of P-glycoprotein [78]. Lopinavir/ritonavir may cause prolonged PR, and second- or third-degree heart block when used with digoxin [59]. Routine monitoring of digoxin levels should be considered. COVID-19 patients treated with both fingolimod and digoxin should receive ECG prior to drug initiation, serial ECG and telemetry monitoring for bradycardia and QT prolongation [41].
Autonomic imbalance
Autonomic imbalance is notorious for its implication in arrhythmogenicity [79]. It is also well-known that various conditions can activate the sympathetic nervous system (SNS), such as physical (e.g. pain, dyspnea) or emotional stress, sleep disorders, metabolic conditions, medical illnesses and procedures, and certain drugs, with all of these noted to occur in clusters at different stages of the COVID-19 infection. Furthermore, there is evidence that COVID-19 reaches the brain stem region, possibly via the nasopharyngeal epithelium and/or crossing the blood-brain barrier or hematogenously via circumventricular organs where the blood-brain barrier is lacking [80]. In the brain stem, there are structures that belong to the dorsal vagal complex situated in the medulla oblongata, the lowest region of the brainstem that controls several autonomic activities, including the heart, breathing, and food intake. Thus, injuries of this specific region of the brainstem could be detrimental for the maintenance of homeostasis [80]. This neurotropism of the virus occurring at the level of the vagus nerve can produce initial bradycardic responses which, in addition to their own hemodynamic effects, could also lead to bradycardia- or pause-dependent TdP, via the arrhythmogenic mechanism of long-short sequence, unassociated with QT prolonging drugs [79].
On the other hand, an anti-inflammatory mechanism has been ascribed to the parasympathetic system which is proposed to monitor systemic inflammation through a reflex system and to activate a neuronal anti-inflammatory signal to prevent deleterious inflammation [81]. In contradistinction to SNS hyperactivation, which appears to be of particular significance for injury to the CV system [82], inflammatory cytokines can activate the afferent sensory vagus nerve that transmits the information to the central nervous system which then can activate the efferent vagus nerve to control inflammation via acetylcholine, its principal neurotransmitter, and a nicotinic anti-inflammatory pathway and modulate the immune system by inhibiting the production of inflammatory cytokines in macrophages and the spleen [83,84]. In this context, diminished cardiac vagal activity, found in patients with pulmonary and cardiometabolic disease, has been shown to adversely affect patients with critical illness, such as COVID-19 infection [85]. On the contrary, patients with an increased vagal tone might be protected from a cytokine release syndrome [82]. Such data support the significance of the cholinergic anti-inflammatory pathway uniquely in COVID-19 patients, hence the suggestion for neuromodulation therapy to control inflammation and related organ dysfunction in COVID-19 [82].
Thus, SNS hyperactivation, an important component of the autonomic dysregulation in the setting of infections and related hyper-inflammatory release syndromes, together with the initial stimulation followed eventually by subsequent attenuation of the vagal activity caused by injury to the vagus nerve produced by the virus itself, can all lead to a serious autonomic imbalance that could contribute to the arrhythmogenicity that complicates COVID-19 infection.
Current literature limitations and future directions
Current literature is limited by the lack of reliable and detailed data on COVID-19-related arrhythmias. In addition, available data do not allow us to distinguish between arrhythmias caused by hypoxemia, metabolic and electrolyte abnormalities, inflammatory syndrome, other comorbidities, and medications as opposed to direct myocardial effect of the virus. A recent study of 234 COVID-19 patients suggested that cardiac arrhythmia, noted in 10 (4.3%) patients, was likely associated with COVID-19 because most of patients had no previous CV morbidities [86]. Of the 10 patients with arrhythmia, only 3 had pre-existing hypertension and 2 had coronary disease; 8 patients were critically ill, one was severe and one moderate. Admission creatine kinase had the highest performance in predicting the occurrence of arrhythmia [86], in keeping with other data indicating that cardiac injury is a critical risk factor for arrhythmogenesis and mortality [15]. Importantly, myocardial injury, as suggested by increases in cTn, is common in patients with COVID-19 and associated with adverse outcomes, such as arrhythmias and death [87], more likely to occur in those with chronic CV conditions and in those with severe COVID-19 infection [87,88].
The data are even more limited regarding the electrophysiological abnormalities and arrhythmias in children with COVID-19 [89,90]. A recent study of 36 pediatric patients reported that significant arrhythmias were infrequent (albeit, more common than expected in a general pediatric population), observed in 6 children (NSVT in 5 and sustained atrial tachycardia in 1), all self-resolving; prophylactic antiarrhythmic therapy was employed in half [91]. Patients with significant arrhythmias were likely to have noncardiac comorbidities (4/6), but these were not more common than in patients without arrhythmias (20/30, p=1). The use of HCQ with or without AZM was associated with significant QTc prolongation (411 ± 19 ms vs 426 ± 15 ms, p<0.0001), however, QTc was not different in patients with and without arrhythmias (425 ± 15 ms vs 425 ± 15 ms, p=1).
Due to limited information about specific arrhythmias and the exact arrhythmogenic mechanisms involved in COVID-19 patients, we are in dire need of studies evaluating the prevalence of arrhythmias in this rapidly growing patient population, both among clinically stable and critically ill patients, studies investigating the involved mechanisms, the prophylactic measures that need to be taken, selection of safe therapies, and appropriate in-hospital and out-of-hospital monitoring of these patients.
Digital medicine
Important lessons have been and continue to be learnt during this on-going pandemic of COVID-19. Apparently, the need for contactless monitoring and telemetry for inpatients, especially those admitted to the ICU, as well as for outpatients needing continued management, has ushered in a new era in implementing digital health monitoring tools [92]. The use of smart watches, smartphones, and even smart beds (with elimination of cables and skin electrodes) for in-hospital telemetry, and even wireless monitoring after discharge, is a novel approach [93]. Bracelet technologies may transmit several parameters (e.g., heart rate and rhythm, oxygen saturation, blood pressure) via a link to centralized stations, providing a solution for extended monitoring. These devices, endorsed by professional societies, allow for convenient remote measurement of the QT interval, real-time monitoring for arrhythmias and other important telehealth services, e.g. implantable device remote monitoring and/or (limited forms of) device programming [53,92].
In keeping with the idea of remote telehealth services, a European project (TeleCheck-AF project featured on the ESC website: bit.ly/34R2F65) was recently launched for on-demand heart rate and rhythm monitoring in order to maintain AF management while keeping patients out of hospital during COVID-19 [94]. To date, 23 European hospitals across nine countries have joined the project.
Conclusion
Cardiac arrhythmias, including atrial arrhythmias (e.g. AF) as well as life-threatening VAs, may be the consequence of direct effects of COVID-19 infection, but also the outcome of the detrimental effects of systemic illness and the adverse proarrhythmic reactions to drugs employed in the treatment of this pandemic (Table 1, Table 2, Table 3, Fig. 1). Drug combinations, especially of QT-prolonging agents, can lead to higher arrhythmogenicity, compared with single drug therapies. Furthermore, critically ill COVID-19 patients often have comorbidities that can trigger life-threatening VAs; among them, electrolyte abnormalities (hypokalemia, hypomagnesemia), fever, systemic inflammatory state, and labile autonomic balance, are highly proarrhythmic and may lead to SCD. Most importantly, in patients with evidence of acute myocardial injury the prevalence of cardiac arrhythmias is higher compared to patients without myocardial injury.
In this context, ECG and QTc monitoring and taking appropriate measures (Table 4) is of paramount importance to prevent, detect and manage cardiac arrhythmias in COVID-19 patients (Table 5). However, a conventional approach to patient monitoring has serious problems with logistics and may pose health risks to personnel and strain the health systems; hence, the need for contactless monitoring and telemetry for inpatients, especially those admitted to the ICU, as well as for outpatients needing continued management. Such an approach has recently been introduced by implementing digital health monitoring tools, a most desirable and practical technology that is here to stay. Among these tools, smart watches, smartphones, and even smart beds (without cables and skin electrodes) for in-hospital telemetry, and even wireless monitoring after discharge, are offering a novel approach to practice contemporary medicine.
Footnotes
Declaration of Competing Interest: None to be declared.
References
- 1.Manolis AS, Manolis TA. Cardiovascular complications of the coronavirus (COVID-19) infection. Rhythmos. 2020;15:23–28. [Google Scholar]
- 2.Parohan M, Yaghoubi S, Seraji A. Cardiac injury is associated with severe outcome and death in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Eur Heart J Acute Cardiovasc Care. 2020 Jun 21 doi: 10.1177/2048872620937165. . Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76(5):533–546. doi: 10.1016/jjacc202006007. . Epub 2020 Jun 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu Y, Xu D, Fu S, Zhang J, Yang X, Xu L, et al. Patients with COVID-19 in 19 ICUs in Wuhan, China: a cross-sectional study. Crit Care. 2020;24:219. doi: 10.1186/s13054-020-02939-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhatla A, Mayer MM, Adusumalli S, Hyman MC, Oh E, Tierney A, et al. COVID-19 and cardiac arrhythmias. Heart Rhythm. 2020 Jun 20 doi: 10.1016/j.hrthm.2020.06.016. S1547-5271(20)30594-4Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Jama. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sala S, Peretto G, De Luca G, Farina N, Campochiaro C, Tresoldi M, et al. Low prevalence of arrhythmias in clinically stable COVID-19 patients. Pacing Clin Electrophysiol. 2020 Jun 16 doi: 10.1111/pace.13987. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lazaridis C, Vlachogiannis NI, Bakogiannis C, Spyridopoulos I, Stamatelopoulos K, Kanakakis I, et al. Involvement of cardiovascular system as the critical point in coronavirus disease 2019 (COVID-19) prognosis and recovery. Hellenic J Cardiol. 2020 doi: 10.1016/j.hjc.2020.05.004. Jun 10;S1109-9666(20)30093-2 doi: 101016/jhjc202005004 Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh AP, Tousif S, Umbarkar P, Lal H. A pharmacovigilance study of hydroxychloroquine cardiac safety profile: potential implication in COVID-19 mitigation. J Clin Med. 2020;9:E1867. doi: 10.3390/jcm9061867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naksuk N, Lazar S, Peeraphatdit TB. Cardiac safety of off-label COVID-19 drug therapy: a review and proposed monitoring protocol. Eur Heart J Acute Cardiovasc Care. 2020;9:215–221. doi: 10.1177/2048872620922784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu WL, Toh HS, Liao CT, Chang WT. A double-edged sword-cardiovascular concerns of potential anti-COVID-19 drugs. Cardiovasc Drugs Ther. 2020 Jun 17:1–10. doi: 10.1007/s10557-020-07024-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular Implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):1–8. doi: 10.1001/jamacardio.2020.1017. . Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gopinathannair R, Merchant FM, Lakkireddy DR, Etheridge SP, Feigofsky S, Han JK, et al. COVID-19 and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies. J Interv Card Electrophysiol. 2020:1–8. doi: 10.1007/s10840-020-00789-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kunutsor SK, Laukkanen JA. Cardiovascular complications in COVID-19: a systematic review and meta-analysis. J Infect. 2020;81:e139–ee41. doi: 10.1016/j.jinf.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Si D, Du B, Ni L, Yang B, Sun H, Jiang N, et al. Death, discharge and arrhythmias among patients with COVID-19 and cardiac injury. CMAJ. 2020 Jun 24;192(28):E791–E798. doi: 10.1503/cmaj.200879. cmaj.200879. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li X, Pan X, Li Y, An N, Xing Y, Yang F, et al. Cardiac injury associated with severe disease or ICU admission and death in hospitalized patients with COVID-19: a meta-analysis and systematic review. Crit Care. 2020;24:468. doi: 10.1186/s13054-020-03183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Q, Xu L, Dai Y, Ling Y, Mao J, Qian J, et al. Cardiovascular manifestations in severe and critical patients with COVID-19. Clin Cardiol. 2020;43(7):796–802. doi: 10.1002/clc.23384. . Epub 2020 Jun 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amaratunga EA, Corwin DS, Moran L, Snyder R. Bradycardia in patients with COVID-19: a calm before the storm? Cureus. 2020;12:e8599. doi: 10.7759/cureus.8599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCullough SA, Goyal P, Krishnan U, Choi JJ, Safford MM, Okin PM. Electrocardiographic findings in COVID-19: insights on mortality and underlying myocardial processes. J Card Fail. 2020;26(7):626–632. doi: 10.1016/j.cardfail.2020.06.005. . Epub 2020 Jun 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pavri BB, Kloo J, Farzad D, Riley JM. Behavior of the PR interval with increasing heart rate in patients with COVID-19. Heart Rhythm. 2020 Jun 11 doi: 10.1016/j.hrthm.2020.06.009. S1547-5271(20)30551-8. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russo V, Rago A, Carbone A, Bottino R, Ammendola E, Della Cioppa N, et al. Atrial fibrillation in COVID-19: from epidemiological association to pharmacological implications. J Cardiovasc Pharmacol. 2020;76(2):138–145. doi: 10.1097/FJC.0000000000000854. [DOI] [PubMed] [Google Scholar]
- 22.Manolis AS. Rhythm or rate control management of atrial fibrillation: an overrated dilemma. Hellenic J Cardiol. 2015;56:495–500. [PubMed] [Google Scholar]
- 23.Holt A, Gislason GH, Schou M, Zareini B, Biering-Sørensen T, Phelps M, et al. New-onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur Heart J. 2020 Jun 24 doi: 10.1093/eurheartj/ehaa494. ehaa494. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Varshneya M, Irurzun-Arana I, Campana C, Dariolli R, Gutierrez A, Pullinger TK, et al. Investigational treatments for COVID-19 may increase ventricular arrhythmia risk through drug interactions. medRxiv. 2020 doi: 10.1101/2020.05.21.20109397. 2020.05.21.20109397Preprint. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL. Acute myocardial injury in patients hospitalized with COVID-19 infection: A review. Prog Cardiovasc Dis. 2020 doi: 10.1016/j.pcad.2020.05.013. S0033-0620(20)30123-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roden DM, Harrington RA, Poppas A, Russo AM. Considerations for drug interactions on QTc interval in exploratory COVID-19 treatment. J Am Coll Cardiol. 2020;75:2623–2624. doi: 10.1016/j.jacc.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. Bmj. 2020;369:m2094. doi: 10.1136/bmj.m2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020 Jun 20 doi: 10.1093/eurheartj/ehaa508. ehaa508Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5(8):e437–e443. doi: 10.1016/S2468-2667(20)30117-1. Epub 2020 May 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mosholder AD, Mathew J, Alexander JJ, Smith H, Nambiar S. Cardiovascular risks with azithromycin and other antibacterial drugs. N Engl J Med. 2013;368:1665–1668. doi: 10.1056/NEJMp1302726. [DOI] [PubMed] [Google Scholar]
- 31.Devaux CA, Rolain JM, Colson P, Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uzelac I, Iravanian S, Ashikaga H, Bhatia NK, Herndon C, Kaboudian A, et al. Fatal arrhythmias: another reason why doctors remain cautious about chloroquine/hydroxychloroquine for treating COVID-19. Heart Rhythm. 2020 doi: 10.1016/j.hrthm.2020.05.030. S1547-5271(20)30526-9Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borba MGS, Val FFA, Sampaio VS, Alexandre MAA, Melo GC, Brito M, et al. Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a randomized clinical trial. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.8857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jankelson L, Karam G, Becker ML, Chinitz LA, Tsai MC. QT prolongation, torsades de pointes, and sudden death with short courses of chloroquine or hydroxychloroquine as used in COVID-19: A systematic review. Heart Rhythm. 2020 May 11 doi: 10.1016/j.hrthm.2020.05.008. S1547-5271(20)30431-8Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim MH, Berkowitz C, Trohman RG. Polymorphic ventricular tachycardia with a normal QT interval following azithromycin. Pacing Clin Electrophysiol. 2005;28:1221–1222. doi: 10.1111/j.1540-8159.2005.50146.x. [DOI] [PubMed] [Google Scholar]
- 36.Yang Z, Prinsen JK, Bersell KR, Shen W, Yermalitskaya L, Sidorova T, et al. Azithromycin causes a novel proarrhythmic syndrome. Circ Arrhythm Electrophysiol. 2017:10. doi: 10.1161/CIRCEP.115.003560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe COVID-19. N Engl J Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van der Lee M, Sankatsing R, Schippers E, Vogel M, Fätkenheuer G, van der Ven A, et al. Pharmacokinetics and pharmacodynamics of combined use of lopinavir/ritonavir and rosuvastatin in HIV-infected patients. Antivir Ther. 2007;12:1127–1132. [PubMed] [Google Scholar]
- 39.David OJ, Kovarik JM, Schmouder RL. Clinical pharmacokinetics of fingolimod. Clin Pharmacokinet. 2012;51:15–28. doi: 10.2165/11596550-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 40.Pilote S, Simard C, Drolet B. Fingolimod (Gilenya(®)) in multiple sclerosis: bradycardia, atrioventricular blocks, and mild effect on the QTc interval. Something to do with the L-type calcium channel? Fundam Clin Pharmacol. 2017;31:392–402. doi: 10.1111/fcp.12284. [DOI] [PubMed] [Google Scholar]
- 41.Vargas WS, Perumal JS. Fingolimod and cardiac risk: latest findings and clinical implications. Ther Adv Drug Saf. 2013;4:119–124. doi: 10.1177/2042098613481023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramireddy A, Chugh H, Reinier K, Ebinger J, Park E, Thompson M, et al. Experience with hydroxychloroquine and azithromycin in the coronavirus disease 2019 pandemic: implications for QT interval monitoring. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.017144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saleh M, Gabriels J, Chang D, Kim BS, Mansoor A, Mahmood E, et al. Effect of chloroquine, hydroxychloroquine and azithromycin on the corrected QT interval in patients with SARS-CoV-2 infection. Circ Arrhythm Electrophysiol. 2020;13 doi: 10.1161/CIRCEP.120.008662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cipriani A, Zorzi A, Ceccato D, Capone F, Parolin M, Donato F, et al. Arrhythmic profile and 24-hour QT interval variability in COVID-19 patients treated with hydroxychloroquine and azithromycin. Int J Cardiol. 2020 doi: 10.1016/j.ijcard.2020.05.036. S0167-5273(20)32223-3Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vouri SM, Thai TN, Winterstein AG. An evaluation of co-use of chloroquine or hydroxychloroquine plus azithromycin on cardiac outcomes: A pharmacoepidemiological study to inform use during the COVID19 pandemic. Res Social Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.031. S1551-7411(20)30468-XOnline ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bun SS, Taghji P, Courjon J, Squara F, Scarlatti D, Theodore G, et al. QT interval prolongation under hydroxychloroquine/ azithromycin association for inpatients with SARS-CoV-2 lower respiratory tract infection. Clin Pharmacol Ther. 2020 doi: 10.1002/cpt.1968. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gollob MH. Clinical trials and qt-prolonging prophylactic therapy in healthy subjects: first, do no harm. J Am Coll Cardiol. 2020;75:3184–3186. doi: 10.1016/j.jacc.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schwartz PJ, Woosley RL. Predicting the unpredictable: drug-induced qt prolongation and torsades de pointes. J Am Coll Cardiol. 2016;67:1639–1650. doi: 10.1016/j.jacc.2015.12.063. [DOI] [PubMed] [Google Scholar]
- 49.Giudicessi JR, Roden DM, Wilde AAM, Ackerman MJ. Genetic susceptibility for COVID-19-associated sudden cardiac death in African Americans. Heart Rhythm. 2020 May 5 doi: 10.1016/j.hrthm.2020.04.045. S1547-5271(20)30419-7Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Giudicessi JR, Noseworthy PA, Ackerman MJ. The QT interval. Circulation. 2019;139:2711–2713. doi: 10.1161/CIRCULATIONAHA.119.039598. [DOI] [PubMed] [Google Scholar]
- 51.Rautaharju PM, Zhang ZM, Prineas R, Heiss G. Assessment of prolonged QT and JT intervals in ventricular conduction defects. Am J Cardiol. 2004;93:1017–1021. doi: 10.1016/j.amjcard.2003.12.055. [DOI] [PubMed] [Google Scholar]
- 52.Bogossian H, Frommeyer G, Ninios I, Hasan F, Nguyen QS, Karosiene Z, et al. New formula for evaluation of the QT interval in patients with left bundle branch block. Heart Rhythm. 2014;11:2273–2277. doi: 10.1016/j.hrthm.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 53.Giudicessi JR, Noseworthy PA, Friedman PA, Ackerman MJ. Urgent guidance for navigating and circumventing the QTc-prolonging and torsadogenic potential of possible pharmacotherapies for coronavirus disease 19 (COVID-19) Mayo Clin Proc. 2020;95:1213–1221. doi: 10.1016/j.mayocp.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Garabelli P, Stavrakis S, Albert M, Koomson E, Parwani P, Chohan J, et al. Comparison of QT interval readings in normal sinus rhythm between a smartphone heart monitor and a 12-lead ECG for healthy volunteers and inpatients receiving sotalol or dofetilide. J Cardiovasc Electrophysiol. 2016;27:827–832. doi: 10.1111/jce.12976. [DOI] [PubMed] [Google Scholar]
- 55.New FDA Guidance Allows Use of KardiaMobile 6L to Measure QTc in COVID-19 Patients. 2020. https://www.alivecor.com/press/press_release/new-fda-guidance-allows-use-of-kardiamobile-6l-to-measure-qtc-in-covid-19-patients/(Accessed June 12, 2020).
- 56.Strik M, Caillol T, Ramirez FD, Abu-Alrub S, Marchand H, Welte N, et al. Validating QT-Interval measurement using the apple watch ECG to enable remote monitoring during the COVID-19 pandemic. Circulation. 2020;142(4):416–418. doi: 10.1161/CIRCULATIONAHA.120.048253. . Epub 2020 Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Roden DM. A practical approach to torsade de pointes. Clin Cardiol. 1997;20:285–290. doi: 10.1002/clc.4960200318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Poulidakis E, Manolis AS. Transvenous temporary cardiac pacing. Rhythmos. 2014;9:20–27. [Google Scholar]
- 59.Rattanawong P, Shen W, El Masry H, Sorajja D, Srivathsan K, Valverde A, et al. Guidance on acute management of atrial fibrillation in COVID-19. J Am Heart Assoc. 2020 doi: 10.1161/JAHA.120.017529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Viskin S, Wilde AA, Krahn AD, Zipes DP. Inaccessibility to quinidine therapy is about to get worse. J Am Coll Cardiol. 2013;62:355. doi: 10.1016/j.jacc.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 61.Zimetbaum P. Antiarrhythmic drug therapy for atrial fibrillation. Circulation. 2012;125:381–389. doi: 10.1161/CIRCULATIONAHA.111.019927. [DOI] [PubMed] [Google Scholar]
- 62.Nielsen TL, Rasmussen BB, Flinois JP, Beaune P, Brosen K. In vitro metabolism of quinidine: the (3S)-3-hydroxylation of quinidine is a specific marker reaction for cytochrome P-4503A4 activity in human liver microsomes. J Pharmacol Exp Ther. 1999;289:31–37. [PubMed] [Google Scholar]
- 63.Lessard E, Fortin A, Bélanger PM, Beaune P, Hamelin BA, Turgeon J. Role of CYP2D6 in the N-hydroxylation of procainamide. Pharmacogenetics. 1997;7:381–390. doi: 10.1097/00008571-199710000-00007. [DOI] [PubMed] [Google Scholar]
- 64.Oguayo KN, Oyetayo OO, Costa SM, Mixon TA. An unusual case of flecainide-induced QT prolongation leading to cardiac arrest. Pharmacotherapy. 2014;34:e30–e33. doi: 10.1002/phar.1403. [DOI] [PubMed] [Google Scholar]
- 65.Cardiac Arrhythmia Suppression Trial (CAST) Investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction N Engl J Med. 1989;321:406–412. doi: 10.1056/NEJM198908103210629. [DOI] [PubMed] [Google Scholar]
- 66.Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS: the task force for the management of atrial fibrillation of the European society of cardiology (ESC)developed with the special contribution of the european heart rhythm association (EHRA) of the ESCEndorsed by the European stroke organisation (ESO) Eur Heart J. 2016;37:2893–2962. [Google Scholar]
- 67.Van Gelder IC, Rienstra M, Crijns HJ, Olshansky B. Rate control in atrial fibrillation. Lancet. 2016;388:818–828. doi: 10.1016/S0140-6736(16)31258-2. [DOI] [PubMed] [Google Scholar]
- 68.Lydtin H. Side effects and contraindications of beta-receptor blocking agents. Klin Wochenschr. 1977;55:415–422. doi: 10.1007/BF01488578. [DOI] [PubMed] [Google Scholar]
- 69.Kaufman ES, Zimmermann PA, Wang T, Dennish GW, 3rd, Barrell PD, Chandler ML, et al. Risk of proarrhythmic events in the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study: a multivariate analysis. J Am Coll Cardiol. 2004;44:1276–1282. doi: 10.1016/j.jacc.2004.06.052. [DOI] [PubMed] [Google Scholar]
- 70.Manolis AS, Tordjman T, Mack KD, Estes NA 3rd. Atypical pulmonary and neurologic complications of amiodarone in the same patient. Report of a case and review of the literature. Arch Intern Med. 1987;147:1805–1809. [PubMed] [Google Scholar]
- 71.Manolis AS, Uricchio F, Estes NA 3rd. Prognostic value of early electrophysiologic studies for ventricular tachycardia recurrence in patients with coronary artery disease treated with amiodarone. Am J Cardiol. 1989;63:1052–1057. doi: 10.1016/0002-9149(89)90077-5. [DOI] [PubMed] [Google Scholar]
- 72.Manolis AS. Dronedarone: the hope and the hype. Rhythmos. 2011;6:21–23. [Google Scholar]
- 73.Manolis AS. Did PALLAS deliver the final blow to dronedarone? Rhythmos. 2012;7:1–2. [Google Scholar]
- 74.Chiladakis JA, Kalogeropoulos A, Patsouras N, Manolis AS. Ibutilide added to propafenone for the conversion of atrial fibrillation and atrial flutter. J Am Coll Cardiol. 2004;44:859–863. doi: 10.1016/j.jacc.2004.04.056. [DOI] [PubMed] [Google Scholar]
- 75.Waldo AL, Camm AJ, deRuyter H, Friedman PL, MacNeil DJ, Pauls JF, et al. Effect of d-sotalol on mortality in patients with left ventricular dysfunction after recent and remote myocardial infarction. The SWORD Investigators. Survival With Oral d-Sotalol. Lancet. 1996;348:7–12. doi: 10.1016/s0140-6736(96)02149-6. [DOI] [PubMed] [Google Scholar]
- 76.Manolis AS, Bethanis S, Metaxa S, Polytarchou K, Sakellaris N, Pyrros I. Use of intravenous vernakalant for atrial fibrillation conversion in the regular ward under only bedside monitoring. Hellenic J Cardiol. 2019;60:54–56. doi: 10.1016/j.hjc.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 77.Cattaneo D, Formenti T, Astuti N, Meraviglia P, Ridolfo A, Gervasoni C. How relevant are the drug-drug interactions between antiretroviral boosted-based regimens and calcium channel blockers in real life? J Antimicrob Chemother. 2018;73:2271–2273. doi: 10.1093/jac/dky139. [DOI] [PubMed] [Google Scholar]
- 78.Ding R, Tayrouz Y, Riedel KD, Burhenne J, Weiss J, Mikus G, et al. Substantial pharmacokinetic interaction between digoxin and ritonavir in healthy volunteers. Clin Pharmacol Ther. 2004;76:73–84. doi: 10.1016/j.clpt.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 79.Manolis AA, Manolis TA, Apostolopoulos EJ, Apostolaki NE, Melita H, Manolis AS. The role of the autonomic nervous system in cardiac arrhythmias: the neuro-cardiac axis, more foe than friend? Trends Cardiovasc Med. 2020 May 17 doi: 10.1016/j.tcm.2020.04.011. S1050-1738(20)30066-9Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 80.Chigr F, Merzouki M, Najimi M. Autonomic brain centers and pathophysiology of COVID-19. ACS Chem Neurosci. 2020;11:1520–1522. doi: 10.1021/acschemneuro.0c00265. [DOI] [PubMed] [Google Scholar]
- 81.Ulloa L. The vagus nerve and the nicotinic anti-inflammatory pathway. Nat Rev Drug Discov. 2005;4:673–684. doi: 10.1038/nrd1797. [DOI] [PubMed] [Google Scholar]
- 82.Fudim M, Qadri YJ, Ghadimi K, MacLeod DB, Molinger J, Piccini JP, et al. Implications for neuromodulation therapy to control inflammation and related organ dysfunction in COVID-19. J Cardiovasc Transl Res. 2020:1–6. doi: 10.1007/s12265-020-10031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tracey KJ. The inflammatory reflex. Nature. 2002;420:853–859. doi: 10.1038/nature01321. [DOI] [PubMed] [Google Scholar]
- 84.Bassi GS, Kanashiro A, Coimbra NC, Terrando N, Maixner W, Ulloa L. Anatomical and clinical implications of vagal modulation of the spleen. Neurosci Biobehav Rev. 2020;112:363–373. doi: 10.1016/j.neubiorev.2020.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ackland GL, Whittle J, Toner A, Machhada A, Del Arroyo AG, Sciuso A, et al. Molecular mechanisms linking autonomic dysfunction and impaired cardiac contractility in critical illness. Crit Care Med. 2016;44:e614–e624. doi: 10.1097/CCM.0000000000001606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liu Q, Chen H, Zeng Q. Clinical characteristics of COVID-19 patients with complication of cardiac arrhythmia. J Infect. 2020;81(3):e6–e8. doi: 10.1016/j.jinf.2020.07.012. . Epub 2020 Jul 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sandoval Y, Januzzi JL, Jr., Jaffe AS. Cardiac troponin for the diagnosis and risk-stratification of myocardial injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.06.068. S0735-1097(20)35888-5Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zaman S, MacIsaac AI, Jennings GL, Schlaich MP, Inglis SC, Arnold R, et al. Cardiovascular disease and COVID-19: Australian and New Zealand consensus statement. Med J Aust. 2020 doi: 10.5694/mja2.50714. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 89.Manolis AS, Manolis TA. Pediatric inflammatory multisystem syndrome temporally associated with SARS-Cov-2 infection (PIMS-TS): Kawasaki-like multisystem inflammatory syndrome in children (MIS-C) during the COVID-19 pandemic with predominant myocarditis. Rhythmos. 2020;15:42–46. [Google Scholar]
- 90.Yasuhara J, Kuno T, Takagi H, Sumitomo N. Clinical characteristics of COVID-19 in children: a systematic review. Pediatr Pulmonol. 2020 doi: 10.1002/ppul.24991. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 91.Samuel S, Friedman RA, Sharma C, Ganigara M, Mitchell E, Schleien C, et al. Incidence of arrhythmias and electrocardiographic abnormalities in symptomatic pediatric patients with PCR-positive SARS-CoV-2 infection, including drug-induced changes in the corrected QT interval. Heart Rhythm. 2020 doi: 10.1016/j.hrthm.2020.06.033. S1547-5271(20)30632-9. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Varma N, Marrouche NF, Aguinaga L, Albert CM, Arbelo E, Choi JI, et al. HRS/EHRA/APHRS/LAHRS/ACC/AHA worldwide practice update for telehealth and arrhythmia monitoring during and after a pandemic. Europace. 2020:euaa187. doi: 10.1093/europace/euaa187. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Steinberg JS, Varma N, Cygankiewicz I, Aziz P, Balsam P, Baranchuk A, et al. 2017 ISHNE-HRS expert consensus statement on ambulatory ECG and external cardiac monitoring/telemetry. Heart Rhythm. 2017;14:e55–e96. doi: 10.1016/j.hrthm.2017.03.038. [DOI] [PubMed] [Google Scholar]
- 94.Linz D, Pluymaekers N, Hendriks JM. TeleCheck-AF for COVID-19. Eur Heart J. 2020;41:1954–1955. doi: 10.1093/eurheartj/ehaa404. [DOI] [PMC free article] [PubMed] [Google Scholar]