Abstract
The outbreak of SARS-CoV-2 coronavirus rapidly altered radiotherapy service delivery around the world.
Aim
The main objective of this study was to assess the impact of precautionary measures implemented in response to the COVID-19 pandemic on the performance of a radiation oncology departments and on mitigation the risk of COVID-19 contagion between and among patients and staff.
Methods
The study period was from March 15 until May 22, 2020. We evaluated total number of patients irradiated and those who initiated treatments, taking into account tumours localisations. We assessed the relationship of potential risk of contagion with patients’ domiciles locations in regions with high number of COVID19 case.
Results and conclusions
The number of patients treated with radiotherapy during the study period decreased due to precautionary measures. After five weeks, the number of radiotherapy treatments began to increase. Just over half of the radiotherapy patients (53.5%) treated at the GPCC reside in the city of Poznan or in one of the ten surrounding counties where COVID19 incidence was low and reached at the end of the study period cumulative number of cases n = 204. The precautionary measures were effective qRT-PCR tests were performed in 1545 individuals (patients and hospital staff) revealing four staff members and none patient with a positive PCR result. Immunoglobulin testing was performed in 1132 individuals (patients and hospital staff). A total of 63 individuals were positive for antibodies.
Keywords: Radiotherapy, COVID19, qPCR, Antibodies, Cancer incidence
1. Introduction
The outbreak of SARS-CoV-2 coronavirus disease started in 2019 (COVID-19) has and rapidly altered radiotherapy service delivery around the world.1, 2, 3, 4, 5 However, the specific precautionary measuares implemented at cancer centres and radiation oncology departments have varied widely depending on local factors and situation.6, 7, 8 An important factor influencing the measures implemented is the incidence of COVID-19 in the area where patients and hospital staff live.9, 10, 11
In response to the COVID-19 pandemic, in March 2020 the government of Poland implemented a series of measures designed to limit public activities (https://koronawirusunas.pl/; accessed from 8th of March. The specific measures are shown in Table 1 by date of implementation.
Table 1.
Specific measures designed to limit public activities due to COVID-19 spread by date of implementation.
| Date | Measure |
|---|---|
| 8 March | The Chief Sanitary Inspectorate in Poland (abbreviation. GIS) recommended prohibiting all public gatherings, including the closure of shopping centres. |
| 12 March | All classes at schools were cancelled, although children were allowed to attend school for basic care supervision under specific circumstances. In the city of Poznan, schools were closed on March 10. |
| 15 March | Closure of international country borders (air and train) in Poland. |
| 16 March | Total closure for all schools and universities. |
| 20 March | State of epidemic status declared in Poland. |
| 25 March | Partial lockdown, including a stay-at-home order; no public gathering allowed. |
| 1 April | Implementation of additional restrictions in open space areas (closure of forests, parks, beaches, etc.). |
| 20 April | Phase I: Certain restrictions eased. |
| 4 May | Phase II: Commerce and industry open (shopping centres, hotels, libraries, museums). All of these are permitted to open partially. Partial opening of pre-schools. |
| 18 May | Phase III: Full opening of commerce and industry, including hair salons, bars and restaurants. |
The restrictions related to COVID-19 have affected many aspects of daily life. Health care system was also influenced. Due to the risk of widespread contagion and the restrictions imposed by the state of epidemic, treatment for medical conditions unrelated to COVID-19 has been severely affected, including radiotherapy for cancer patients. Although radiotherapy can be conditionally interrupted or postponed in some patients, However, in most cases uninterrupted radiotherapy is essential for optimal treatment effects. However, during the pandemic status, radiation oncology departments worldwide have been forced to implement numerous prophylactic and precautionary measures. To our knowledge, the impact of these precautionary measures on radiation therapy for patients with cancer in Poland has not been assessed, till now.
1.1. Aim
The main objective of this study was to assess the impact of precautionary measures implemented in response to the COVID-19 pandemic on the performance of a radiation oncology departments in given cancer centre in Poland. Secondly, we describe the measures introduced to reduce the risk of COVID-19 contagion between and among patients and staff.
2. Material and methods
This observational study was performed to assess the impact of the COVID-19 epidemic—specifically, the precautionary measures implemented at our centre (Greater Poland Cancer Centre; GPCC)—on the clinical practice of radiation oncology at our centre. To assess the impact of these measures, we determined the number of patients treated with radiotherapy during the 10-week period from March 15 to May 22, 2020 at the peak of the pandemic restrictions and compared these to the usual number of patients treated prior to the pandemic. We also sought to correlate the place of residence of both patients and staff with the severity of the epidemic (i.e., the incidence rate) in that region.
To mitigate the risk of disease spread to or among staff and patients, the GPCC and the radiation oncology department introduced a series of precautionary measures. All efforts were directed to minimize the risk that anyone (patient or staff member) infected by SARS-CoV-2 would enter the hospital or radiation oncologydepartment. These measures included the establishment of a new designated laboratory to perform testing for COVID-19, with the daily capacity to evaluate 100 nasopharyngeal swab samples (using quantitative reverse-transcription polymerase chain reaction [qRT-PCR]) and 100 serum antibody tests. Importantly, this testing activity did not alter in any way the regular laboratory work related to diagnostic tests for cancer patients.
For qRT-PCR testing, the swab was obtained from the posterior wall of the nasopharynx. Viral RNA was automatically isolated using MagCore Viral Nucleic Acid Extraction Kit (RBC Bioscience, Taiwan). RT-PCR was performed using the qPCR SARS-CoV-2 kit (Vitassay Healthcare S.L.U, Spain) and the CFX96 Touch Real-Time PCR Detection System (Bio-Rad, CA).
Anti-SARS-CoV-2 antibodies, such as immunoglobulin M and G (IgM and IgG) antibodies in serum were determined using the COVID-19 Rapid Test Kit (Biopanda Reagents Ltd. Belfast, United Kingdom) and 2019-nCoV IgG/IgM Detection Kit (Nanjing Vazyme Medical Technology Co., Ltd. Nanjing, China). These tests used qualitative immunochromatography methods for the detection of IgM and IgG antibodies to SARS-CoV-2.
3. Results
3.1. Treatment of patients
For the reason of assessing the potential risk of contagion by patients’ domiciles locations in regions with high number of COVID19 case, we used outcomes for a year of 2013 from the study performed by Paczkowska.12 The population of the city of Poznan in 2013 was 549,082. The county of Poznan, which includes the city, had in 2013, 348,730 inhabitants. (as of June 30, 2013; http://demografia.stat.gov.pl/bazademografia/Tables.aspx). The GPCC employs approximately 1200 people, most of whom live in the city of Poznan itself or within the county.
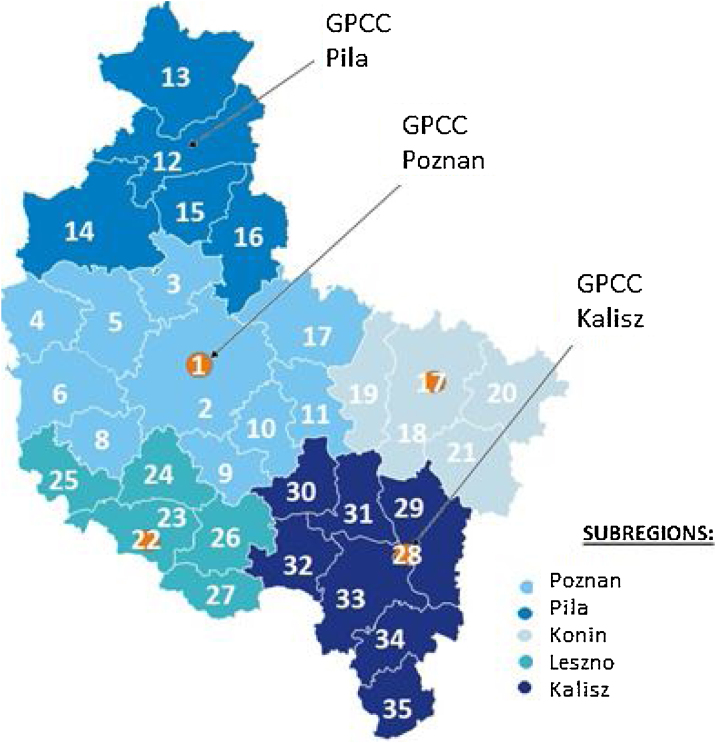
Just over half of the radiotherapy patients (53.5%) treated at the GPCC reside in the city of Poznan or in one of the ten surrounding counties (Fig. 1).
Fig. 1.
Subregions in the province of Greater Poland (with counties). The cities of Poznan, Kalisz, Konin, and Leszno are considered separate from the surrounding counties. The Greater Poland Cancer Centre (GPCC) has locations in Poznan, Kalisz, and Pila. The numbers in the map correspond to the names of the counties provided in Table 2.
The most populous regions in the hospital’s coverage area are the city and county of Poznan, where more than one-third of radiotherapy patients (35.3%) reside, according to data from a study conducted in 2013.12 We used these data for the patients in the study period (March 15 to May 22, 2020). Note that the percentage of oncology patients treated with radiotherapy at the GPCC with domiciles in the city and county of Poznan was 33.6% lower than for whole Poznan subregion (grouping all 11 counties) and lower than the figure (52%) calculated for Poland in the ESTRO-HERO study.13,14 The geographic origin (i.e., place of residence) of patients treated with radiotherapy at the GPCC is shown in Table 2.
Table 2.
Geographic origin (city or county of residence) of patients who received radiotherapy at the Greater Poland Cancer Centre in 2013. The table shows the subregions with major cities, counties, population, cancer incidence, number of patients from each region, and percentage of patients from each region relative to the cancer incidence in that subregion.12,15
| City or County | Radiotherapy patients from a given subregion |
||||||
|---|---|---|---|---|---|---|---|
| Subregion (main city) |
# | Name | Population | New cancer patients from a given subregion |
n | % of incidence | % of all radiotherapy patients |
|
Poznan |
1 2 |
* City of Poznan Land county of Poznan |
897 812 | 4 618 | 1551 | 33.6 | 35.2 |
| 1 2 3 4 5 6 7 8 9 10 11 |
* City of Poznan Land counties/districts of Poznan Oborniki Miedzychod Szamotuly Nowy Tomysl Gniezno Grodzisk Srem Sroda Wrzesnia |
1 547 256 | 7 385 | 3006 |
40.7 | 68.2 | |
|
Pila |
12 13 14 15 16 |
Land counties/districts of Pila Zlotow Czarnkow-Trzcianka Chodziez Wagrowiec |
414 003 |
1 615 |
383 |
23.7 |
8.7 |
|
Konin |
17 18 19 20 |
* City of Konin Land counties/districts of Konin Słupca Kolo Turek |
439 157 | 1 847 | 344 | 18.6 | 7.8 |
|
Leszno |
21 22 23 24 25 |
* City of Leszno Land counties/districts of Leszno Koscian Wolsztyn Gostyn Rawicz |
390 508 | 1 615 |
331 | 20.5 | 7.5 |
| Kalisz |
26 27 28 29 30 31 32 |
* City of Kalisz, Land counties/districts of Kalisz Jarocin Pleszew Krotoszyn Ostrow Ostrzeszow Kepno |
672 495 | 2 587 | 342 | 13.2 | 7.8 |
| All | 3 463 419 | 15 049 | 4406 | ||||
* Cities of Poznan, Kalisz, Konin and Leszno form separate administrative districts, while the area around these cities fall into separate land districts even though they have the same name as the cities.
Table 3 shows the number of new patients initiating radiotherapy and the number of patients receiving daily radiotherapy treatment in Poznan and at the two satellite sites in Kalisz and Pila. Poznan is equipped with five linear accelerators, a Tomotherapy and a Cyberknife unit, while Kalisz and Pila possess two linear accelerators each.
Table 3.
Number of new patients initiating radiotherapy (first fraction) each week and number of patients treated with radiotherapy per day at the Greater Poland Cancer Centre from March 15 through May 22, 2020 (10 weeks) compared to the mean number in the pre-pandemic period (December 30 to February 28).
| March |
April |
May |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Week |
Weekly mean from Dec 30 to Feb 28 | 02−06 | 09−13 | 16−20 |
23−27 |
30−03 |
6−10 |
13−17 |
20−24 |
27−30 |
4−8 |
11−15 |
18−22 |
| Patients/week initiating radiotherapy |
102.4 | 108 | 104 | 51 | 45 | 53 | 59 | 68 | 87 | 57 | 101 | 123 | 106 |
| Daily mean from 30 Dec to Feb 28 | |||||||||||||
| Patients/day receiving radiotherapya |
301 | 327 | 325 | 290 | 253 | 214 | 200 | 190 | 198 | 191 | 208 | 238 | 268 |
Refers to patients who initiated radiotherapy plus those who continued treatment. The daily numbers vary because some patients had one fraction or a shorter course and may initiate or end treatment during weekdays (the mean value from all weekdays is given).
As Table 3 shows, during the study period, fewer new patients were treated at our centre compared to the weekly average for 2019. Similarly, the mean number of patient receiving daily treatment prior to the epidemic was 301, declining progressively until it reached a nadir (n = 190) during the week of April 13−17 (the 5th week after implementation of precautionary measures at the GPCC) of 190 patients, a decrease of 36.9%. Afterwards, there was an irregular trend towards an increase in weekly numbers.
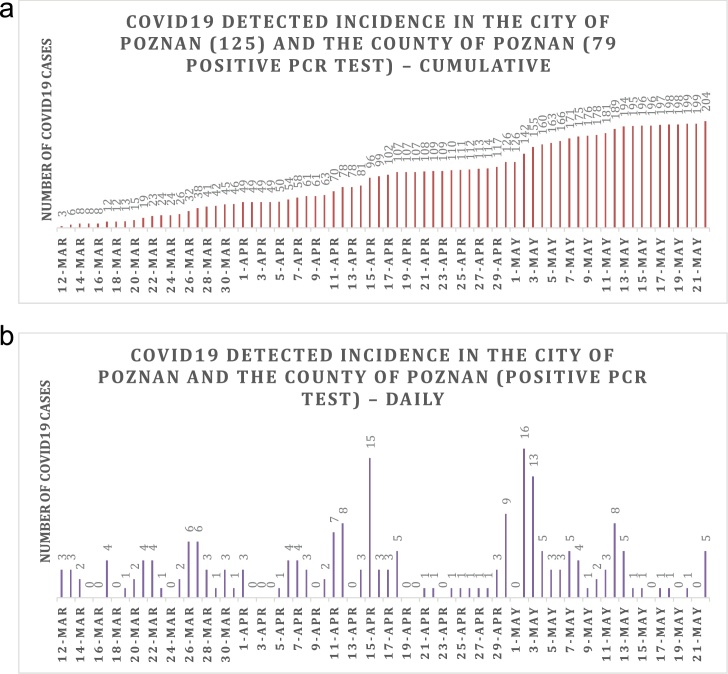
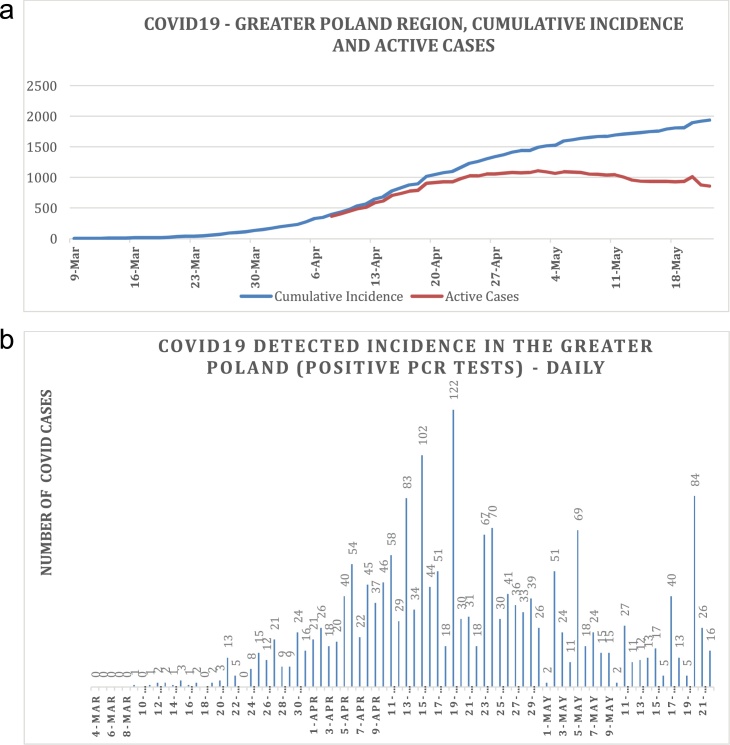
3.2. Distribution of COVID-19 cases in the Greater Poland province
In the Greater Poland region, with a population of 3.473 million inhabitants (2019 data) [ Europejski Urząd Statystyczny ], the incidence of COVID-19 varied highly from county to county (Table 4). During the study period, the number of COVID-19 cases (number of people diagnosed with COVID-19 per day) from Poznan (city and county) was quite stable and low (despite the fact that this area is the most populated and urbanised in the entire Greater Poland region), and reached at the end of the study period cumulative number of cases n = 204 (218 cases per million inhabitants as of May 22) (Fig. 2, Table 4). In the whole province of Greater Poland, the daily number of COVID-19 cases increased during the study period, mainly due to two epidemic “hot spots” in the counties of Krotoszyn and Kalisz, which are located, respectively, in the south and southeast regions of Greater Poland (Table 4). The cumulative number of cases in the entire Greater Poland region at the end of the study period was n = 194 (555 per million inhabitants as of May 22) (Fig. 3, Table 4).
Table 4.
Cumulative incidence of COVID-19 as of May 22, 2020 in the Greater Poland region by county (https://koronawirusunas.pl/wojewodztwo-wielkopolskie and https://stat.gov.pl/obszary-tematyczne/ludnosc/ludnosc/ludnosc-stan-i-struktura-ludnosci-oraz-ruch-naturalny-w-przekroju-terytorialnym-stan-w-dniu-31-12-2019,6,27.html).
| Subregion (main city) | City or County | Cumulative incidence from March 15 to May 22 | Population (as of December 31, 2019) | Cumulative incidence per million inhabitants |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| Poznan |
*City of Poznan Land county of Poznan |
204 | 934085 | 218 |
| City of Poznan | 125 | 534813 | 234 | |
| Land counties/districts of | ||||
| Poznan | 79 | 399272 | 198 | |
| Oborniki | 11 | 59825 | 184 | |
| Miedzychod | 2 | 36751 | 54 | |
| Szamotuly | 1 | 91664 | 11 | |
| Nowy Tomysl | 1 | 75543 | 13 | |
| Gniezno | 171 | 145418 | 1176 | |
| Grodzisk | 2 | 51893 | 39 | |
| Srem | 10 | 61425 | 163 | |
| Sroda | 4 | 58879 | 68 | |
| Wrzesnia | 2 | 77994 | 26 | |
| Pila | Land counties/districts of | |||
| Pila | 17 | 136112 | 125 | |
| Zlotow | 1 | 69433 | 14 | |
| Czarnkow-Trzcianka | 49 | 86990 | 563 | |
| Chodziez | 9 | 47055 | 191 | |
| Wagrowiec | 19 | 70233 | 271 | |
| Konin | City of Konin | 4 | 73522 | 54 |
| Land counties/districts of | ||||
| Konin | 10 | 130053 | 77 | |
| Slupca | 2 | 59077 | 34 | |
| Kolo | 0 | 86727 | 0 | |
| Turek | 6 | 83894 | 72 | |
| Leszno | City of Leszno | 25 | 63505 | 394 |
| Land counties/districts of | ||||
| Leszno | 10 | 57201 | 175 | |
| Koscian | 7 | 79183 | 88 | |
| Wolsztyn | 2 | 57446 | 35 | |
| Gostyn | 9 | 75908 | 119 | |
| Rawicz | 12 | 60262 | 199 | |
| Kalisz | City of Kalisz | 371 | 100246 | 3701 |
| Land counties/districts of | ||||
| Kalisz | 177 | 83026 | 2132 | |
| Jarocin | 10 | 71563 | 140 | |
| Pleszew | 185 279 |
63014 77274 |
2936 3611 |
|
| Krotoszyn | ||||
| Ostrow | 126 | 161581 | 780 | |
| Ostrzeszow | 38 | 55500 | 685 | |
| Kepno | 165 | 56451 | 2923 | |
| All | 1941 | 3498733 | 555 |
Fig. 2.
COVID-19 incidence in the city of Poznan and county of Poznan (positive PCR test): 2a. cumulative; 2b. daily.
Fig. 3.
COVID-19 incidence in Greater Poland (positive RT-PCR test): 3a. cumulative (blue), active cases (red); 3b. daily. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
3.3. Screening for COVID-19 at the GPCC
To detect the presence of COVID-19 among radiotherapy patients, we targeted three main patient subgroups for screening. The primary target for qRT-PCR testing were patients admitted for chemoradiotherapy (mainly those with head and neck cancer) as these patients were expected to be hospitalised for several weeks and it was essential to minimize the risk of infecting other patients or staff. These patients underwent screening tests on their first arrival or admission (due to repeated treatments) to the hospital. The second group comprised patients staying at hotels/hostels located near the hospital. In this group, testing was considered necessary because most of these patients were expected to spend substantial time at the hospital (daily visits to receive radiotherapy treatments). The third group consisted of patients residing in the region who received daily radiotherapy on an outpatient basis. For this group, the main precautionary measures included a careful check at the main entrance to the hospital for any sign of infection, which included questions about the presence of possible COVID-19 symptoms and a body temperature check. Pulse oximetry was performed in some patients, with random qRT-PCR testing as well. Anti-SARS-CoV-2 immunoglobulin (IgM and IgG) testing was also performed.
3.4. Staff screening
Starting on March 15, 2020 precautionary measures were introduced for departmental staff (nurses, technicians, physicians and administrative staff). One measure was to divide the staff into two groups with separate shifts. Another measure was to limit the number of patients scheduled for radiotherapy (two patients per hour). All hospital staff (n = 1200) also underwent PCR testing for COVID-19 infection, andanti-SARS-CoV-2 immunoglobulin (IgM and IgG) testing (repeated regularly).
3.5. qRT-PCR test results
The qRT-PCR tests were performed from March 27. Until May 22, 2020 a total of 1620 tests were performed in 1545 individuals (patients and hospital staff); in 39 and 16 cases, respectively, the test was repeated two or three times. Four staff members had a positive PCR result. Additionally, one staff member was detected PCR positive while being on sick leave for other reason (test performed outside GPCC). In patients, a total of 471 qRT-PCR tests were performed in 450 patients (repeated twice in 19 patients and three times in another case).
Immunoglobulin testing was conducted from March 22. During the study period, 1156 antibody tests were performed in 1132 individuals (patients and hospital staff). A total of 65 tests (63 individuals) were positive for antibodies; of these, 27 were IgM+/IgG−; five were IgM+/IgG+; and 33 were IgM-/IgG+ (two people obtained the results IgM+/IgM− twice).
A total of 145 qRT-PCR tests were performed in 138 radiotherapy patients; in 7 cases the test was performed twice. Tests were repeated if necessary, according to standardized procedures established by the Polish Government to ensure the validity of negative results after suspected contact with a patient diagnosed with COVID-19.
Of the 235 staff members associated with the radiotherapy department, we performed qRT-PCR tests in 159 individuals (24 repeated) and 171 antibody tests (one repeated). Two staff members tested positive for COVID-19; none of the patients tested positive. Table 5 shows the distribution of staff members by professional groups.
Table 5.
Results of genetic qRT-PCR from nasopharyngeal swab samples and antibodies from blood serum. Abbreviations: PCR - polymerase chain reaction, IgM, IgG: immunoglobulin type M, G.
| # of staff | PCR test | PCR test positive | Antibody test | Antibody result positive |
|||
|---|---|---|---|---|---|---|---|
| IgM + IgG - |
IgM + IgG + |
IgM - IgG + |
|||||
| Radiation Oncologists | 37 | 26 |
2 |
23 |
4 |
1 |
4 |
| Physicists | 27 | 23 | 28 | ||||
| Radiation terapists (RTTs) | 69 | 44 | 59 | ||||
| Nurses | 69 | 52 | 53 | ||||
| Other | 33 | 17 | 34 | ||||
| All | 235 | 159 | 171 | ||||
3.6. Precautionary measures implemented in the radiation oncology department
Due to the size (in terms of number of employees) of the GPCC and its coverage area, the institution has a total of four radiotherapy departments, two located in the samehospital in Poznan and two others sites located in Kalisz and Pila.
The first precautionary measure, taken on March 15, was the creation of separate areas for patients, including separate entrances with control posts. In addition, no new patients were scheduled for treatment during the week of March 15–20 in order to prepare for the implementation of these measures. Some hospital staff members were advised to stay at home, particularly these whose presence could be spared when precautionary measures were newly tested and those who could performed distant work from home. Starting the week of March 23–28, the department working hours were extended and shifts introduced to minimize the number of patients in the department at any one time. A limit of two patients/hour on the linear accelerators was introduced. The use of surgical masks was mandatory for all outpatients. inpatients were excepted from this obligation (tested on admittance to the hospital and therefore considered COVID19 free).
In the following weeks, the department staff was provided with visors and the treatment rooms were equipped with thermometers to check the patients’ body temperature in cases with suspected symptoms of infection. A brief questionnaire was introduced to assess the patients’ health status and possible contact with individuals positive for COVID-19, and about visits to known disease “hot spots” (e.g., the counties of Krotoszyn and Kalisz).
Every week thereafter, we reviewed the case mix and status of treated patients based on radiotherapy accepting new patients who met newly elaborated national and international radiotherapy and COVID-19 guidelines.8,16
4. Discussion
The main aim of this observational study was to assess impact of safety measures implemented at our hospital to prevent the spread of COVID-19 on the performance of our radiation oncology department. Specifically, we assessed the impact of these measures on the number of patients who received radiotherapy on a daily and weekly basis during the study period. We observed a substantial decrease in the number of patients undergoing daily radiotherapy treatment from 301 per day (pre-epidemic) to a low of 190 in late April, a reduction of nearly 37%. However, these numbers began to rapidly increase in the following weeks, reaching 268 patients in the next few weeks. Similarly, in the pre-pandemic period, the mean number of weekly treatment initiations was 102.4, falling to a low of 59 in the week of March 30–May 3, a reduction of nearly 43%. By the week of May 11–15, these numbers have risen again, reaching 122 treatment initiations, exceeding by nearly 20% the weekly mean numbers from the pre-epidemic period.
At our centre, we took a careful approach in order to assure the safety of both patients and hospital staff. Our aim was to find ensure that all patients who required radiotherapy treatment during this difficult period received the necessary care while, at the same time, guaranteeing the safety of both patients and staff. We implemented a series of measures that, as we show here, were quite effective in minimising or even eliminating spread of disease at the hospital. Theese measures included the following: 1) interruption of certain preparatory aspects of radiotherapy treatment for a few days in the week of March 23–28 in order develop plans for continuing radiotherapy treatment in the midst of the pandemic; 2) broad use of qRT-PCR and antibody testing for both patients and staff, with tests conducted in a dedicated laboratory; 3) the introduction of two shifts for certain staff members, extension of the working day, and a limit of 2 patients/hour to minimize contact among patients and staff; 4) separate entrances with a control point to check for signs of infection (including a questionnaire and temperature check); and 5) mandatory use of surgical masks for patients and visors for staff. The implementation of these rigorous precautionary measures allowed us to continue working and treating patients safely. Only two radiotherapy staff members testedpositive for COVID-19, and none of the patients did.
The Greater Poland region is among the largest in Poland and it is the second largest by area (29826.5 km²) and the third largest by population (3,367,016). In the year 2013, the annual incidence of cancer diagnoses in this region was 15,049 cases, with a mean of 289 new cancer cases and 139 deaths per week, which is a significantly greater number of deaths than caused by COVID-19.15 In the context of a pandemic such as COVID-19, numerous factors must be cosidered when planning radiotherapy treatment. Clearly, a full workload is not possible due to staff shortages (non-overlapping shifts, social leaves to attend children owing to pandemic social regulation) and the extended period of time required between consecutive patients (to minimize risks of disease spread among patients in waiting areas). In some patients, treatment can be safely postponed until the epidemic abates, or the hospital has implemented sufficient measures to allow for a larger caseload. In our sample, some patients decided to postpone treatment initiation for a short poriod. The precautionary measures implemented during the epidemic helped to keep the hospital and radiotherapy environment safe. Similar approach and observations were reported in rapidly growing number of publications.1, 2, 3, 4, 5, 6, 7
The precautionary measures taken at our centre had a major impact on radiotherapy treatment. As Table 2 shows, fewer new patients received treatment during the study period compared to the weekly average for the early period of 2020 (before COVID 19 empidemia). Interestingly, patient numbers were, at least initially, primarily affected by national restrictions, which were introduced on March 15 (see Table 1). The precautionary measures introduced at our hospital started the following week. The weekly number of new patients did not recover pre-epidemic levels until May 4−8, which was the 8th week after the introduction of these extraordinary measures at the GPCC. These figures reflect the improvement in the epidemic in the Greater Poland province, as shown in Fig. 3b). At the same time, the daily number of new COVID-19 cases for the whole Poland continued to rise (a wide plateau rather than a peak). We believe that the combination of practical and psychological adjustments to the new situation and safety measures among both staff and patients created a path to bring the department’s performance rapidly back to the pre-epidemic period.
Although there were two counties (Kalisz and Krotoszyn) with a high incidence of COVID-19 cases in the Greater Poland region, this did not materially raise the risk of COVID-19 spread because the number of patients from these counties treated with radiotherapy at the GPCC in Poznan was limited. The patients from these two hot spots in fact used to choose the satellite radiotherapy department in Kalisz. The current situation reflects the establishment of this satellite in 2017 on demand of patients organisations who opted for shorter than to Poznan distance from their domiciles to radiotherapy service.17, 18, 19 In radiotherapy department in Kalisz social distancing and other measures could be more effectively introduced because this satellite department is much less crowded by patients and visitors. Noteworthy, most of the staff live in or near Poznan (city or county), where the incidence of COVID-19 was relatively low (< one new case/per day). For practical reason, we believe that it is more reasonable to assess the prevalence of COVID-19 in the regions where staff and patients live, rather than evaluating data for whole country of Poland.
Treatment initiation for certain patients was temporarily suspended, however, as radiotherapy cannot be postponed indefinitely, therefore, once all necessary precautionary measures were put in place, the number of patients treated with radiotherapy gradually increased, as shown in Table 1, Table 2. Although the number of patients treated daily have not yet reached the pre-pandemic levels (now 268 vs. 301), the trend is clear, confirmed by the number of patients initiating radiotherapy each week. In the last two weeks of the study period, the numbers significantly exceeded the pre-epidemic weekly average of 102.4. Therefore, we expect to return to pre-epidemic performance of the radiotherapy department in the very near future.
5. Conclusions
The number of patients treated with radiotherapy during the study period decreased due to precautionary measures, as well as to the patients’ own decisions to postpone radiotherapy. After five weeks, the number of radiotherapy treatments began to increase. The precautionary measures were effective and we did not detect any spread of COVID-19 among staff or patients in the radiotherapy departments.
Conflict of interest
None.
Financial disclosure
None.
References
- 1.Filippi A.R., Russi E., Magrini A.M., Corvo R. Letter from Italy: First practical indications for radiation therapy departments during COVID-19 outbreak. Int J Radiat Oncol Biol Phys. 2020;107(3):597–599. doi: 10.1016/j.ijrobp.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guckenberger M., Belka C., Bezjak A. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus statement. Radiother Oncol. 2020;146:223–229. doi: 10.1016/j.radonc.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomson D.J., Palma D., Guckenberger M. Practice recommendations for risk-adapted head and neck Cancer radiation therapy during the COVID-19 pandemic: An ASTRO-ESTRO consensus statement. International Journaln of Radiation Oncology, Biology Physics. 2020;107(4):618–627. doi: 10.1016/j.ijrobp.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coles C.E., Aristei C., Bliss J. International guidelines on radiation therapy for breast Cancer During the COVID-19 pandemic. Clin Oncol. 2020;32:279–281. doi: 10.1016/j.clon.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marijnen C.A.M., Peters F.P., Rödel C. International expert consensus statement regarding radiotherapy treatment options for rectal cancer during the COVID 19 pandemic. Radiother Oncol. 2020;148:213–215. doi: 10.1016/j.radonc.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braunstein L.Z., Gillespie E.F., Hong L. Breast radiation therapy under COVID-19 pandemic resource constraints—Approaches to defer or shorten treatment from a comprehensive Cancer center in the United States. Advances in Radiation Oncologu. 2020;xx:1–7. doi: 10.1016/j.adro.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.We Wei, Zheng Dandan, Lei Yu. Radiotherapy workflow and protection procedures during the Coronavirus Disease 2019 (COVID-19) outbreak: Experience of the Hubei Cancer hospital in Wuhan, China. Radiother Oncol. 2020;148:203–210. doi: 10.1016/j.radonc.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dziadziuszko R., Fijuth J., Gabryś D. 2020. Rekomendacje Zarządu Polskiego Towarzystwa Radioterapii Onkologicznej i Konsultanta Krajowego w dziedzinie radioterapii onkologicznej dotyczące funkcjonowania zakładów radioterapii w warunkach istotnego zmniejszenia zasobów ludzkich, skutkujących ograniczeniem możliwości prowadzenia leczenia napromienianiem. www.ptro.org.pL. [Google Scholar]
- 9.Daily-Practice/COVID-19-Recommendations-and-information/Summary. www.astro.org.
- 10.Gudiance for management of urothelial cancer during COVID-19 pandemic. www.nice.org.uk, 2020.
- 11.Management of Prostate cancer during the COVID-19 pandemic. www.nccn.org/covid-19/, 2020. [DOI] [PMC free article] [PubMed]
- 12.Paczkowska K. Analiza rozkładu pacjentów kwalifikowanych do radioterapii z placówek wielkopolski ze względu na rozpoznanie z uwzględnieniem zachorowalności w regionie. Zeszyty Naukowe Wielkopolskie Centrum Onkologii. 2016;13(2):38–44. doi: 10.21641/los.13.2.11. [DOI] [Google Scholar]
- 13.Borras J.M., Barton M., Grau C. The impact of cancer incidence and stage on optimal utilization of radiotherapy: Methodology of a population based analysis by the ESTRO – HERO project. Radiother Oncol. 2015;116(1):45–50. doi: 10.1016/j.radonc.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 14.Borras J.M., Lievens Y., Dunscombe P. The optimal utilization proportion of external beam radiotherapy in European countries: An ESTRO- HERO analysis. Radiother Oncol. 2015;116(1):38–44. doi: 10.1016/j.radonc.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 15.Dyzmann-Sroka A., Malicki J., Jędrzejczak A. Cancer incidence in the Greater Poland region as compared to Europe. Rep Pract Oncol Radiother. 2020;25(4):632–636. doi: 10.1016/j.rpor.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Covid19 Yale Radiaton Oncology Flowchart – July 6, 2020, www.covid-19.gale.edu.
- 17.Dyzmann-Sroka A., Malicki J. Cancer incidence and mortality in the Greater Poland Region- Analysis of the year 2010 and future trends. Rep Pract Oncol Radiother. 2014;19(5):296–300. doi: 10.1016/j.rpor.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reinfuss M., Byrski E., Malicki J. Radiotherapy facilities, equipment, and staffing in Poland: 2005-2011. Reporte of Practical Oncology and Radiotherapy. 2013;18(3):159–172. doi: 10.1016/j.rpor.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalbarczyk W.P., Zespołem Brzozowski Swrazz. 2015. Stan dostępności do leczniczych świadczeń onkologicznych w Polsce – Analiza i rekomendacje. Raport przygotowany dla Polskiego Towarzystwa Onkologicznego. [Google Scholar]