Introduction
The transition to virtual health care delivery during the COVID-19 pandemic has been especially important for individuals living with a rheumatic disease given their increased risk for comorbidities and susceptibility to infection [1, 2]. As health care systems and providers rapidly shift to providing virtual care, it is crucial to ensure that efforts to develop and implement virtual care are informed by the patients. We therefore aimed to explore the perspectives of individuals living with rheumatic diseases towards virtual rheumatology appointments during the COVID-19 pandemic.
Methods
We conducted an international online survey (www.unifiedcovid.com). With the support of patient partners and arthritis organizations, we recruited participants through social media. Participants were eligible if they were ≥ 18 years of age, diagnosed with a rheumatic disease, and able to complete the survey in English or French. The survey included questions on demographics, type of rheumatic disease(s) and treatments, and experiences with virtual rheumatology appointments. Descriptive statistics were based on non-missing responses. Ethical approval was obtained from the University of British Columbia (H20-01164).
Results
Overall, 429 individuals (median age, 41 years; 90.7% female) completed the survey between April 23, 2020, and June 9, 2020. The majority of participants were from North America and diagnosed with rheumatoid arthritis (57.6%) (Table 1). Ninety-four (26.4%) participants indicated that their rheumatic disease treatment changed and 48 (13.6%) indicated that they discontinued a prescribed medication during the COVID-19 pandemic. Altogether, 58.6% of participants felt supported by their rheumatology care provider(s) during the COVID-19 pandemic.
Table 1.
Participant characteristics (n = 429)
| Characteristic | |
|---|---|
| Age, median (range) | 41.1 (17.6–90.6) |
| Female, n (%) | 330 (90.7) |
| Country, n (%) | |
| Canada | 164 (38.2) |
| USA | 147 (34.3) |
| Other | 118 (27.5) |
| Highest level of education, n (%) | |
| Secondary school | 56 (15.5) |
| Post-secondary (university, college, technical school) | 305 (84.5) |
| Rheumatic disease typea, n (%) | |
| Rheumatoid arthritis | 247 (57.6) |
| Osteoarthritis | 58 (13.5) |
| Psoriatic arthritis | 45 (10.5) |
| Systemic lupus erythematosus | 43 (10.0) |
| Sjogren syndrome | 32 (7.5) |
| Ankylosing spondylitis | 27 (6.3) |
| Juvenile idiopathic arthritis | 21 (4.9) |
| Mixed connective tissue disease | 19 (4.4) |
| Gout | 9 (2.1) |
| Systemic sclerosis | 4 (0.9) |
| Systemic vasculitis | 4 (0.9) |
| Myositis | 4 (0.9) |
| Other | 33 (7.7) |
| Disease severity (past week)b, n (%) | |
| Under control | 54 (14.8) |
| Mild | 113 (31.0) |
| Moderate | 152 (41.6) |
| Severe | 46 (12.6) |
| Duration of diagnosis, n (%) | |
| Less than 1 year | 58 (13.5) |
| 1 to 5 years | 145 (33.8) |
| 6 to 10 years | 101 (23.5) |
| Over 10 years | 125 (29.1) |
| Medications, n (%)c | |
| Prescription medication(s) | 339 (79.0) |
| csDMARDd | 261 (60.8) |
| Methotrexate | 144 (33.6) |
| Chloroquine | 134 (31.2) |
| Hydroxychloroquine | 129 (30.1) |
| Biologic or targeted DMARD | 170 (39.6) |
| Corticosteroid | 91 (21.2) |
| Non-prescription medication(s) | 137 (31.9) |
| Tested for COVID-19 | |
| No | 310 (91.2) |
| Yes | 30 (8.8) |
| Positive test | 3 (10.0) |
| Negative test | 27 (90.0) |
aNot discrete as participants can report ≥ 1 type
bDisease activity was self-reported
cNot discrete as participants can report ≥ 1 medication
dOnly the most commonly prescribed csDMARDs are listed
Number of missing responses ranged from 0 (0%) to 113 (26.3%)
csDMARD, conventional synthetic disease-modifying anti-rheumatic drug
In total, 154 (44.0%) participants had a virtual rheumatology appointment during the COVID-19 pandemic. The majority (n = 233, 68.5%) stated that they did not have a choice between an in-person or virtual appointment for their most recent rheumatic disease medical appointment. Most participants (73.8%) were not bothered by a lack of choice regarding appointment format and 71.2% were satisfied with their virtual appointment. Disease severity and satisfaction with virtual appointments were significantly associated, with higher satisfaction among participants under control (19.3% vs. 4.5%) and with severe disease (11.9% vs. 4.5%) and lower satisfaction among participants with mild (27.5% vs. 43.5%) and moderate disease (41.3% vs. 47.7%) (chi-square p value < 0.05).
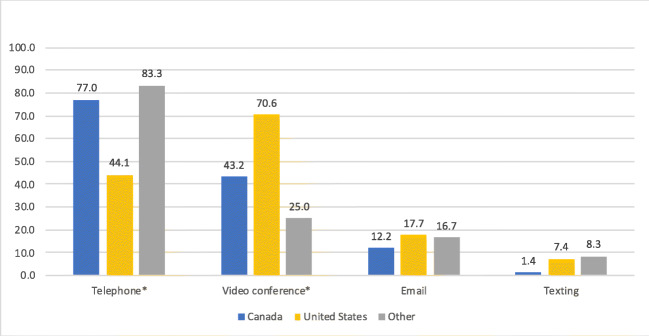
Platforms used for virtual appointments differed by country, with telephone being the predominant modality in Canada (77.0%) and other countries (83.3%) in comparison with the USA (44.1%; chi-square p value < 0.05) (Fig. 1). Patient preference for seeing health providers during videoconference was mixed (no—14.3%; yes—42.9%; no preference—42.9%). The preferred appointment type when receiving difficult news was largely in-person (64.5%), with telephone (19.9%), and video conference (15.7%) being less favored options.
Fig. 1.
Frequency of each platform used for virtual rheumatology appointment(s) during the COVID-19 pandemic according to country. *Chi-square p value < 0.05
Discussion
The COVID-19 pandemic has generated notable changes to the delivery of rheumatology care, as preliminary results from our international survey show nearly half of participants attended a virtual rheumatology appointment. Recommendations arising from our findings include prioritizing in-person appointments when discussing difficult news, considering a patient’s disease severity and providing the option for telephone or video conference, where possible, for virtual follow-up appointments to ensure that patient preferences are considered while supporting practical allocation of resources. Our survey has also demonstrated gaps in care, with only 58.6% of patients feeling supported during the COVID-19 pandemic and 13.6% stopping medications, a particular concern giving recommendations to continue rheumatic disease medications during the pandemic [3]. Quality of virtual care could be improved by adopting an interprofessional collaborative approach and designing electronic health infrastructure that supports information exchange and communication between health professionals [4].
Although ongoing, our survey is limited by its small sample size, low representation of certain rheumatic diseases, and restriction to online survey distribution. Our study sample also consists of a far greater proportion of women than the general rheumatic disease population. Nonetheless, as the delivery of rheumatology care continues to be modified during the COVID-19 pandemic, it is critical to have rapid and responsive patient-centered research to inform decisions that impact care and outcomes of people living with rheumatic diseases.
Acknowledgments
The authors would like to thank participants who have shared their experiences through the survey study.
Funding information
Dr. De Vera holds a Tier 2 Canada Research Chair and is a recipient of a Scholar Award from the Michael Smith Foundation for Health Research. Dr. Avina-Zubieta is the Walter and Marilyn Booth Research Scholar and a recipient of a grant award (COV-2020-1075) from the Michael Smith Foundation for Health Research. Mrs. Howren is a recipient of a Canadian Institutes of Health Research Frederick Banting and Charles Best Canada Graduate Scholarship – Doctoral Award and a Wayne Riggs Interdisciplinary Doctoral Scholarship in Pharmaceutical Sciences (University of British Columbia).
Compliance with ethical standards
Disclosures
None.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aviña-Zubieta JA, Choi HK, Sadatsafavi M, Etminan M, Esdaile JM, Lacaille D. Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum. 2008;59(12):1690–1697. doi: 10.1002/art.24092. [DOI] [PubMed] [Google Scholar]
- 2.Solomon DH, Love TJ, Canning C, Schneeweiss S. Risk of diabetes among patients with rheumatoid arthritis, psoriatic arthritis and psoriasis. Ann Rheum Dis. 2010;69(12):2114–2117. doi: 10.1136/ard.2009.125476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McInnes IB. COVID-19 and rheumatology: first steps towards a different future? Ann Rheum Dis. 2020;79(5):551–552. doi: 10.1136/annrheumdis-2020-217494. [DOI] [PubMed] [Google Scholar]
- 4.Décary S, Barton JL, Proulx L et al (2020) How to effectively support patients with rheumatic conditions now and beyond COVID-19. ACR Open Rheumatol. 10.1002/acr2.11152 [DOI] [PMC free article] [PubMed]