Abstract
The emergence of coronavirus disease 2019 (COVID-19) has become a worldwide pandemic after its first outbreak in Wuhan, China. However, it remains unclear whether COVID-19 death is linked to ambient air pollutants or meteorological conditions. We collected the daily COVID-19 death number, air quality index (AQI), ambient air pollutant concentrations, and meteorological variables data of Wuhan between Jan 25 and April 7, 2020. The Pearson and Poisson regression models were used accordingly to understand the association between COVID-19 deaths and each risk factor. The daily COVID-19 deaths were positively correlated with AQI (slope = 0.4 ± 0.09, R2 = 0.24, p < 0.01). Detailedly, PM2.5 was the only pollutant exhibiting a positive association (relative risk (RR) = 1.079, 95%CI 1.071–1.086, p < 0.01) with COVID-19 deaths. The PM10, SO2, and CO were all also significantly associated with COVID-19 deaths, but in negative pattern (p < 0.01). Among them, PM10 and CO had the highest and lowest RR, which equaled to 0.952 (95%CI 0.945–0.959) and 0.177 (95%CI 0.131–0.24), respectively. Additionally, temperature was inversely associated with COVID-19 deaths (RR = 0.861, 95%CI 0.851–0.872, p < 0.01). Contrarily, diurnal temperature range was positively associated with COVID-19 deaths (RR = 1.014, 95%CI 1.003–1.025, p < 0.05). The data suggested that PM2.5 and diurnal temperature range are tightly associated with increased COVID-19 deaths.
Keywords: COVID-19, Air pollution, Meteorological conditions, Wuhan, Deaths
Introduction
The novel coronavirus disease 2019 (COVID-19) is a novel viral infectious disease. Since emerging from Wuhan, China, in late 2019, the COVID-19 has rapidly propagated throughout all Chinese provinces and, subsequently, caused a global pandemic (World Health Organization 2020). By Jun 1, 2020, there are about 7 million confirmed cases and 0.4 million deaths globally (World Health Organization 2020).
Ambient air pollutant is currently considered the most significant environmental cause of respiratory illness–induced death. For example, the fatality of severe acute respiratory syndrome (SARS) in 2003 was tightly linked to environmental conditions (Wallis and Nerlich 2005) and air pollution (Cui et al. 2003). Previous multi-city studies in Europe showed that ambient air pollution has larger association with respiratory causes of death than other diseases (Atkinson et al. 2014). Recently, some studies further demonstrated that there exists a significant correlation between COVID-19 incidence and ambient air pollution (Bashir et al. 2020; Jiang et al. 2020) as well as meteorological conditions (Jiang et al. 2020). However, the knowledge of association between COVID-19 deaths and short-term air pollution/meteorological conditions exposure remains largely limited (Conticini et al. 2020; Ogen 2020).
Due to the suddenness and global scope of the COVID-19 pandemic, urgent concerns have been raised for the role of air pollution and meteorological conditions on COVID-19 deaths. In the current study, the authors aim to explore the potential association between COVID-19 deaths and air pollutants as well as meteorological variables.
Material and methods
Data sources
The current study period was from Jan 25 to April 7 in 2020, during which Wuhan was placed under strict lockdown. This study used the open-access COVID-19 death number of Wuhan, which was maintained by the Health Commission of Hubei China (Health Commission of the Hubei Province 2020). Daily average ambient air pollutant concentrations were extracted from a publicly available website called the Platform AQI (https://www.aqistudy.cn). The mean concentration of each pollutant was calculated from the average of hourly data from all stations in Wuhan. Overall, six pollutants were included in the current study, which were PM2.5, PM10, SO2, CO, NO2, and O3-8h (maximum 8-h moving average concentrations for O3). The definitions of PM2.5 and PM10 were adopted from US EPA (United States Environmental Protection Agency 2019b), whose cut-off diameters were 2.5 and 10 μm, respectively. The daily air quality index (AQI) based on PM2.5 concentration was calculated from US EPA AQI calculator (United States Enviromental Protection Agency 2020). The AQI is an index for reporting daily air quality, which is divided into six intervals to help the general population understand what local air quality means to their health (US EPA 2012). Three environmental variables were extracted from the Weather Channel (www.weather.com), including the daily temperature, relative humidity, and diurnal temperature range.
Data analysis
The effects of ambient air pollutants and meteorological variables on the COVID-19 deaths were studied using the GraphPad Prism® 8.0 (La Jolla California, USA). First, we analyzed the mean value (± standard deviations) of daily AQI, ambient air pollutant concentrations, meteorological variables, and COVID-19 death number. Next, a time series analysis using the Pearson regression model was conducted to examine the associations between overall air quality (using AQI) and COVID-19 deaths on a daily bases. Finally, the association between all risk factors and COVID-19 deaths was evaluated by the Poisson regression model. Based on the clinical feature of COVID-19 infection, all risk factors were matched with death number from 18 days later as the median time to death for COVID-19 was 18.5 days (Zhou et al. 2020). The p value < 0.05 was considered as statistically significant.
Results
Table 1 was a collection of detailed information on daily AQI, air pollutant concentrations, meteorological variables, and COVID-19 death number. Starting on Jan 25, 45 deaths of COVID-19 patients were reported. The deaths gradually increased and peaked on Feb 12 (216 deaths). After that, the deaths started decreasing and dropped to 0 on April 6.
Table 1.
Descriptive statistics of daily coronavirus disease 2019 (COVID-19) death number, air quality index (AQI), six ambient air pollutant concentrations, and three meteorological variables from 25 Jan to 6 Apr 2020 in Wuhan. The table listed the mean, standard deviation, and minimum and maximum data of each variable
| Mean | Std. deviation | Minimum | Maximum | |
|---|---|---|---|---|
| Daily COVID-19 death No. | 36.2 | 39.3 | 0 | 216 |
| AQI | 114.5 | 36.6 | 38 | 178 |
| PM2.5 | 44.7 | 22.8 | 9 | 108 |
| PM10 | 56.2 | 26.0 | 12 | 122 |
| SO2 | 7.6 | 2.5 | 5 | 17 |
| CO | 0.9 | 0.2 | 0.5 | 1.4 |
| NO2 | 25.8 | 11.9 | 10 | 76 |
| O3_8h | 75.1 | 26.5 | 28 | 135 |
| Daily temperature | 7.4 | 4.5 | 0 | 18 |
| Relative humidity | 79.5 | 9.0 | 58 | 96 |
| Diurnal temperature range | 7.9 | 3.7 | 1 | 16 |
Next, we studied the potential correlation between COVID-19 deaths and air quality. Since the AQI provides an overall assessment of air quality, we first used AQI to explore the potential correlation between air quality and COVID-19 deaths. For accurate fitness, the COVID-19 deaths on Feb 12 were removed from the analysis as it stood as an outlier data point in the analysis. The data revealed that AQI was positively correlated with daily COVID-19 deaths (slope = 0.4 ± 0.09, R2 = 0.24, p < 0.01) (Fig. 1), indicating worse air quality is paralleled with increased COVID-19 deaths. Based on this finding, the association between ambient air pollutants and COVID-19 deaths was further studied by using the Poisson regression (Table 2). Our data exhibited that among all pollutants, PM2.5, PM10, SO2, and CO were strongly associated with daily COVID-19 deaths (all p < 0.01). Among these four pollutants, PM2.5 was the only variable that exhibited a positive association (relative risk (RR) = 1.079, 95%CI 1.071–1.086) with COVID-19 deaths. Among those inversely associated with COVID-19 deaths, the PM10 and CO had the highest and lowest RR, which equaled to 0.952 (95%CI 0.945–0.959) and 0.177 (95%CI 0.131–0.24), respectively.
Fig. 1.
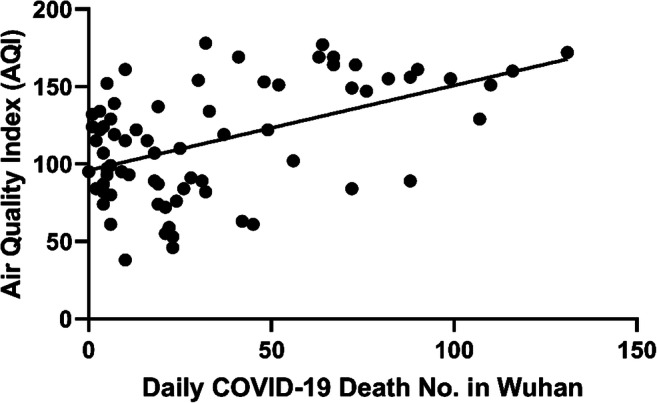
The association between daily air quality index (AQI) and death number of COVID-19 patients in Wuhan. The AQI is positively correlated with the death number of COVID-19 patients in a linear pattern (slope = 0.4 ± 0.09, R2 = 0.24, p < 0.01)
Table 2.
The correlation between the coronavirus disease 2019 (COVID-19) daily death number and six ambient air pollutants from 25 Jan to 7 Apr 2020 in Wuhan, China. The regression coefficient (RC) relative risk (RR), 95% confidence interval (95% CI), and p value for each pollutant was listed
| RC | RR | 95% CI | p | |
|---|---|---|---|---|
| PM2.5 | 0.076 | 1.079 | 1.071–1.086 | < 0.01 |
| PM10 | − 0.049 | 0.952 | 0.945–0.959 | < 0.01 |
| SO2 | − 0.051 | 0.951 | 0.919–0.984 | < 0.01 |
| CO | − 1.729 | 0.177 | 0.131–0.24 | < 0.01 |
| NO2 | 0.002 | 1.002 | 0.996–1.007 | 0.55 |
| O3_8h | 0.001 | 1.001 | 0.998–1.003 | 0.56 |
We further studied the effect of three meteorological variables on COVID-19 deaths (Table 3). Our data exhibited that temperature was significantly, but inversely, associated with COVID-19 deaths (RR = 0.861, 95%CI 0.851–0.872, p < 0.01). However, diurnal temperature range was positively associated with COVID-19 deaths (RR = 1.014, 95%CI 1.003–1.025, p < 0.05).
Table 3.
The correlation between the coronavirus disease 2019 (COVID-19) daily death number and six ambient air pollutants from 25 Jan to 7 Apr 2020 in Wuhan, China. The regression coefficient (RC) relative risk (RR), 95% confidence interval (95% CI), and p value for each meteorological variable was listed
| RC | RR | 95% CI | p | |
|---|---|---|---|---|
| Daily temperature | − 0.149 | 0.861 | 0.851–0.872 | < 0.01 |
| Relative humidity | − 0.005 | 0.995 | 0.989–1 | 0.062 |
| Diurnal temperature range | 0.014 | 1.014 | 1.003–1.025 | 0.01 |
Discussion
Emerging studies suggested that COVID-19 incidence is associated with air pollution and meteorological conditions. However, whether air pollution and meteorological conditions could affect COVID-19 deaths remains unclear. In the current study, the authors provided some preliminary evidence showing that PM2.5, PM10, SO2, and CO showed a prominent association with COVID-19 deaths, but only that of PM2.5 is positive. Additionally, temperature and diurnal temperature range also played a role in increasing and decreasing COVID-19 deaths, respectively.
Multiple prior studies had linked higher concentrations of ambient PM with increased respiratory causes of death (Park et al. 2020). For example, influenza-induced excess mortality was reported in Milan during winter 2016–2017, which was strongly associated with concomitant PM pollution (Murtas and Russo 2019). The SARS fatality also demonstrated a positive association with PM pollution in Chinese population in 2003 (Cui et al. 2003). While there is no shortage of reviews focusing on PM and health, the information regarding the outcome of exposure to PM on COVID-19 is limited. So far, only Frontera et al. (2020), Zhou et al. (2020), and Zhu et al. (2020) had investigated this issue in Italy, USA, and China, respectively, and all of them shown that severe PM2.5 pollution is linked to higher mortality in COVID-19 patients. In the current study, our data agreed with these studies as we have also shown that PM2.5 is positively associated with COVID-19 deaths in Wuhan. More interestingly, our data exhibited that PM10 is also tightly correlated with COVID-19 deaths, but in a negative pattern. The author believed that this divergent effect between PM2.5 and PM10 might be size-related. According to US EPA, the PM could be divided into PM2.5 and PM10 based on its diameter (United States Environmental Protection Agency 2019a). Although both PM features prolonged air floating capacity and could penetrate into the respiratory tract, the PM2.5 could pass the pulmonary defense barrier, disseminate into alveoli, or even enter blood circulation (Falcon-Rodriguez et al. 2016). Comparing to the strong penetration ability of PM2.5, PM10 could only reach the tracheobronchial region (Hinds 1999), which could be removed by host immune more easily. Additionally, previous studies had also demonstrated the PM could induce cellular overexpression of angiotensin-converting enzyme 2 (ACE2) receptor (Aztatzi-Aguilar et al. 2015; Frontera et al. 2020; Lin et al. 2018). Since the SARS-CoV-2 uses the ACE2 to invade host cells (Wan et al. 2020), PM2.5 appears to surpass PM10 in increasing alveolar viral load and aggravating viral infection. However, the PM2.5 is comprised of multiple other possibly relevant particles rather than being a singular particle (Croft et al. 2020). Moreover, it is still under debate that ambient particles could actually transport viruses that are still viral enough to cause COVID-19. Thus, the hypothesis proposing tight association between PM2.5 and COVID-19 deaths requires further laboratory study for confirmation.
Our study found that ambient PM10 is inversely associated with COVID-19 deaths. This finding is contrary to the observation from literatures. For example, Yao et al. (2020b) reported that PM10 increased the COVID-19 case fatality rate in 49 Chinese cities. In the subsequent study, Yao et al. (2020a) further concluded that PM10 could increase the case fatality rate of COVID-19 patients with mild to severe disease progression in Wuhan. Although the cause of this discrepancy is unknown, we think this might be related to the exact COVID-19 death number we used in the current study rather than the case fatality rate. In Wuhan, the COVID-19 incidence reached its peak on Feb 12 and started to drop afterward. Meanwhile, the peak-plateau of COVID-19 death number lasts from Feb 12 to 23. Thus, there is a reverse variation tendency between net death number and case fatality rate during this period of time in Wuhan. In addition, previous studies also presented disagreement on the association between PM10 and COVID-19 transmission (Jiang et al. 2020; Zhu et al. 2020). Thus, the role of PM10 on COVID-19 deaths is largely unknown and needs future epidemiological and laboratory studies with larger sample size.
Relationships have also been previously studied between meteorological conditions and severe outcomes in the context of respiratory illness. For example, an inverse correlation had been reported between respiratory disease mortality and temperature (Fallah Ghalhari and Mayvaneh 2016; Pinheiro Sde et al. 2014). The association between diurnal temperature range and respiratory disease mortality has also been previously presented (Kim et al. 2016). In 2003, temperature and diurnal temperature range had been suggested to affect the severe acute respiratory syndrome (SARS) outbreak in Guangdong, China (Tan et al. 2005). Recently, some studies had provided some preliminary evidence indicating the COVID-19 transmission may be partially suppressed with temperature increase (Liu et al. 2020; Wu et al. 2020). In this contribution, a recent study presented an inverse association between COVID-19 deaths and temperature (Fareed et al. 2020), which matched the conclusion from the current study. However, few studies so far have investigated the association of diurnal temperature range with COVID-19 deaths. Literature reviewing came back only one short-term epidemiological investigation, which reported that diurnal temperature ranges were positively correlated with daily COVID-19 deaths (Ma et al. 2020). The results from the current study agreed with this prior study. However, since our study was based on data from a longer investigation period, the conclusion from the current study tends to be more reliable.
There are several limitations that must be acknowledged in the current study. First, other than the daily death number, the detailed demographic data of COVID-19 deaths were unavailable. As reported in the previous study, COVID-19 death is more common in people with advanced age (mean age 78.5) and with underlying conditions (Istiuto Superiore di Sanità 2020). Thus, there exists a large overlap between external causes of death and underlying health problems in COVID-19 patients. Second, the current study is conducted only in Wuhan, China, but not in other countries on other continents. Lack of comparison (e.g., a big city with good AQI) could be a drawback of the current study. Future studies should explore the association between ambient air pollutants/meteorological variables with COVID-19 death cases with detailed clinical data from multiple regions. Last but not the least, China has recently increased Wuhan’s COVID-19 death toll by 50%. This was mainly due to the breakdown of the health care system during the pandemics, which made the death counts inaccurate. Thus, the finding from the current study might require verification of future studies from other world regions.
In conclusion, our studies demonstrated COVID-19 deaths in Wuhan has a positive association with PM2.5 and diurnal temperature range. Meanwhile, the death number is inversely associated with PM10, SO2, CO, and daily temperature.
Acknowledgments
The authors want to thank all medical works and staffs throughout the world who have been working selflessly during the COVID-19 pandemics.
Data availability
Data are however available from the authors upon reasonable request.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
Not available.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ying Jiang and Jing Xu contributed equally to this work.
Contributor Information
Ying Jiang, Email: yjiang1@vt.edu.
Jing Xu, Email: xujingjingalpha@sohu.com.
References
- Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax. 2014;69:660–665. doi: 10.1136/thoraxjnl-2013-204492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aztatzi-Aguilar OG, Uribe-Ramírez M, Arias-Montaño JA, Barbier O, De Vizcaya-Ruiz A. Acute and subchronic exposure to air particulate matter induces expression of angiotensin and bradykinin-related genes in the lungs and heart: angiotensin-II type-I receptor as a molecular target of particulate matter exposure. Particle and Fibre Toxicology. 2015;12:17. doi: 10.1186/s12989-015-0094-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir MF, et al. Correlation between environmental pollution indicators and COVID-19 pandemic: a brief study in Californian context. Environ Res. 2020;187:109652. doi: 10.1016/j.envres.2020.109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E, Frediani B, Caro D (2020) Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environmental pollution (Barking, Essex: 1987) 261 10.1016/j.envpol.2020.114465, 114465 [DOI] [PMC free article] [PubMed]
- Croft D, et al. Associations between source-specific particulate matter and respiratory infections in New York State adults. Environ Sci Technol. 2020;54:975–984. doi: 10.1021/acs.est.9b04295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y, Zhang Z, Froines J, Zhao J, Wang H, Yu S, Detels R. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ Health. 2003;2:15. doi: 10.1186/1476-069x-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falcon-Rodriguez C, Osornio-Vargas A, Sada-Ovalle I, Segura-Medina P. Aeroparticles, composition, and lung diseases. Front Immunol. 2016;7:3. doi: 10.3389/fimmu.2016.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallah Ghalhari G, Mayvaneh F. Effect of air temperature and universal thermal climate index on respiratory diseases mortality in Mashhad, Iran. Archives of Iranian medicine. 2016;19:618–624. [PubMed] [Google Scholar]
- Fareed Z, Iqbal N, Shahzad F, Shah SGM, Zulfiqar B, Shahzad K, Hashmi SH, Shahzad U. Co-variance nexus between COVID-19 mortality, humidity, and air quality index in Wuhan, China: new insights from partial and multiple wavelet coherence. Air Qual Atmos Health. 2020;13:673–682. doi: 10.1007/s11869-020-00847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G (2020) Severe air pollution links to higher mortality in COVID-19 patients: the "double-hit" hypothesis. The Journal of infection 10.1016/j.jinf.2020.05.031 [DOI] [PMC free article] [PubMed]
- Health Commission of the Hubei Province (2020) The realtime coronovirus epidemiological situationof Hubei province. http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/index.shtml. Accessed 2020
- Hinds W. Aerosol technology. 2. New York, NY: John Wiley and Sons, Inc.; 1999. [Google Scholar]
- Istiuto Superiore di Sanità (2020) Characteristics of COVID-19 patients dying in Italy - Report based on available data on March 20th, 2020
- Jiang Y, Wu XJ, Guan YJ (2020) Effect of ambient air pollutants and meteorological variables on COVID-19 incidence. Infection control and hospital epidemiology:1-11 10.1017/ice.2020.222 [DOI] [PMC free article] [PubMed]
- Kim J, et al. Comprehensive approach to understand the association between diurnal temperature range and mortality in East Asia. Sci Total Environ. 2016;539:313–321. doi: 10.1016/j.scitotenv.2015.08.134. [DOI] [PubMed] [Google Scholar]
- Lin CI, Tsai CH, Sun YL, Hsieh WY, Lin YC, Chen CY, Lin CS. Instillation of particulate matter 2.5 induced acute lung injury and attenuated the injury recovery in ACE2 knockout mice. Int J Biol Sci. 2018;14:253–265. doi: 10.7150/ijbs.23489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y, Zhao Y, Liu J, He X, Wang B, Fu S, Yan J, Niu J, Zhou J, Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murtas R, Russo AG. Effects of pollution, low temperature and influenza syndrome on the excess mortality risk in winter 2016-2017. BMC Public Health. 2019;19:1445. doi: 10.1186/s12889-019-7788-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogen Y (2020) Assessing nitrogen dioxide (NO(2)) levels as a contributing factor to coronavirus (COVID-19) fatality. The Science of the total environment 726 10.1016/j.scitotenv.2020.138605 [DOI] [PMC free article] [PubMed]
- Park S, Allen R, Lim C. A likely increase in fine particulate matter and premature mortality under future climate change. Air Qual Atmos Health. 2020;13:143–151. doi: 10.1007/s11869-019-00785-7. [DOI] [Google Scholar]
- Pinheiro Sde L, Saldiva PH, Schwartz J, Zanobetti A. Isolated and synergistic effects of PM10 and average temperature on cardiovascular and respiratory mortality. Rev Saude Publica. 2014;48:881–888. doi: 10.1590/s0034-8910.2014048005218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan J, Mu L, Huang J, Yu S, Chen B, Yin J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J Epidemiol Community Health. 2005;59:186–192. doi: 10.1136/jech.2004.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Enviromental Protection Agency (2020) AQI calculator. https://cfpub.epa.gov/airnow/index.cfm?action=airnow.calculator. Accessed 2020
- United States Environmental Protection Agency (2019a) Particulate matter (PM2.5) trends. https://www.epa.gov/air-trends/particulate-matter-pm25-trends. Accessed 2019
- United States Environmental Protection Agency (2019b) What are the air quality standards for PM? https://www3.epa.gov/region1/airquality/pm-aq-standards.html. Accessed 2019
- US EPA . Air quality index (AQI) El Salvador: San Salvador; 2012. [Google Scholar]
- Wallis P, Nerlich B (2005) Disease metaphors in new epidemics: the UK media framing of the 2003 SARS epidemic. Social science & medicine (1982) 60:2629-2639 10.1016/j.socscimed.2004.11.031 [DOI] [PMC free article] [PubMed]
- Wan Y, Shang J, Graham R, Baric R, Li F (2020) Receptor recognition by the novel coronavirus from wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol 94. 10.1128/jvi.00127-20 [DOI] [PMC free article] [PubMed]
- World Health Organization (2020) Coronavirus disease (COVID-19) outbreak situation. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 2020
- Wu Y, et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y, Pan J, Liu Z, Meng X, Wang W, Kan H, Wang W. Temporal association between particulate matter pollution and case fatality rate of COVID-19 in Wuhan. Environ Res. 2020;189:109941. doi: 10.1016/j.envres.2020.109941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y, et al. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci Total Environ. 2020;741:140396. doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F, Yu T, du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/s0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Xie J, Huang F, Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are however available from the authors upon reasonable request.


