Main text
Non-invasive ventilation (NIV) delivered by a helmet interface in acute respiratory distress syndrome (ARDS) has been associated with a lower rate of intubation, and mortality, compared to face mask NIV [1]. The mechanism accounting for this apparent benefit is uncertain; postulated mechanisms include more effective delivery of airway pressure due to better sealing of the interface and/or higher inspiratory flows.
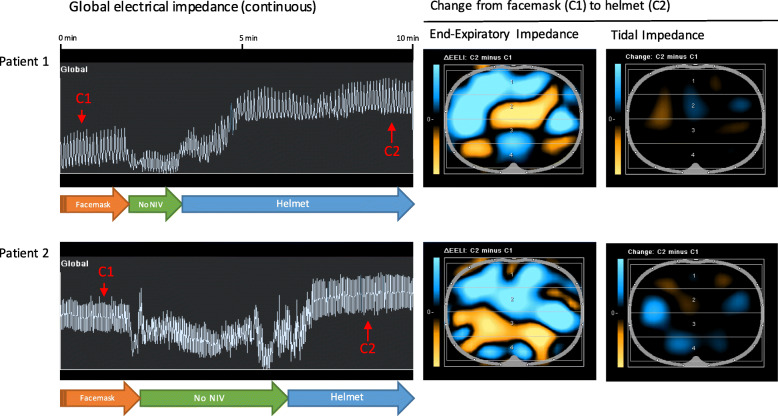
During routine care of two patients with acute hypoxemic respiratory failure, we used electrical impedance tomography (‘EIT’, Draeger Pulmovista 500) to monitor ventilation while transitioning from face mask to helmet NIV. The transition to helmet NIV was a clinical decision prompted by worsening respiratory failure on face mask NIV, with the goal of avoiding intubation. EIT is a non-invasive imaging technique that permits visualization of lung volumes and the distribution of ventilation. Its high temporal resolution can detect rapid changes in lung volume during tidal ventilation and during adjustments to ventilator settings [2]. After calibration, EIT signals were recorded while the patients were ventilated on face mask NIV (Draeger V500 or BiPAP-Vision). We then exchanged the mask interface for a helmet interface (StarMed CaStar-R, Intersurgical), resuming ventilation at the same inspiratory and expiratory positive airway pressure (IPAP, EPAP) settings. During the transition, patients breathed without support at functional residual capacity. Global and regional end-expiratory lung impedance (EELI) and tidal impedance variation (TIV) were recorded throughout (Fig. 1). Twenty breaths were recorded under each condition (Table 1). Changes in end-expiratory lung volume were computed from changes in end-expiratory lung impedance by normalizing changes in lung impedance during tidal breathing to tidal volume measured by the ventilator [3]. Consent was obtained from the patients/legal representatives.
Fig. 1.
Changes in lung volume and the distribution of ventilation following transition from face mask to helmet interface for non-invasive ventilation. NB: orange = loss of ventilation; blue = gain of ventilation
Table 1.
Lung volumes and distribution of ventilation under face mask and helmet NIV
| Patient 1 | Patient 2 | |||||
|---|---|---|---|---|---|---|
| Clinical history: | 61-year-old female with metastatic small cell lung cancer admitted to the ICU for sepsis and acute hypoxemic respiratory failure | 69-year-old female with acute myelogenous leukaemia admitted to ICU for acute hypoxemic respiratory failure | ||||
| Face mask NIV | Transition (no NIV) | Helmet NIV | Face mask NIV | Transition (no NIV) | Helmet NIV | |
| Ventilator | Draeger V500 | n/a | Draeger V500 | BiPap Vision | n/a | Draeger V500 |
| NIV setting (IPAP/EPAP), cm H2O | 12/8 | n/a | 12/8 | 10/8 | n/a | 10/8 |
| Tidal impedance variation (mean, SD) | 1404 (93) | 773 (202) | 1163 (259) | 2123 (259) | 1724 (487) | 2564 (245) |
| Tidal volume, ml (mean, SD) | 392 (26) | 216 (56) | 325 (72) | 375 (46) | 310 (86) | 462 (43) |
| End-expiratory lung impedance (mean, SD) | 550 (126) | 234 (83) | 3022 (147) | 3623 (128) | 1956 (559) | 5203 (212) |
| Computed end-expiratory lung volume above FRC, ml (mean, SE) | 88 (34) | Reference | 778 (38) | 253 (134) | Reference | 574 (140) |
| Proportion of tidal impedance in variation in dorsal lung region (%) | 56 | 50 | 57 | 45 | 42 | 57 |
| Respiratory rate (min−1) | 24 | 31 | 25 | 33 | 32 | 34 |
| Peripheral oxygen saturation (%) | 92 | n/a | 96 | 93 | n/a | 95 |
| Set FiO2* | 0.55 | n/a | 0.4 | 0.5 | n/a | 0.4 |
SD standard deviation, SE standard error of the mean
*The FiO2 stated represents the requirement as determined by the respiratory therapists (RTs). FiO2 was titrated, depending on response, within approximately 1 h of the change in interface
Transition from face mask to helmet NIV was associated with a significant increase in EELI, predominantly in the ventral lung regions (Fig. 1). These changes in EELI were consistent with increases in end-expiratory lung volume (EELV) of 690 ml and 320 ml above FRC in the first and second patients, respectively (Table 1). Tidal impedance variation was redistributed dorsally in the second patient, possibly reflecting recruitment of previously non-ventilated lung regions. In both patients, oxygen saturations improved and FiO2 requirements decrease, on helmet NIV compared to face mask NIV (Table 1). The first patient required intubation after several hours on NIV via helmet; after 7 days of invasive mechanical ventilation, the patient recovered and was discharged to the ward. The second patient recovered after 24 h on helmet NIV and was discharged to the ward.
In summary, we observed that helmet NIV interface was associated with higher EELV compared to face mask NIV, even though the applied pressures were unchanged. This effect—and the potential lung recruitment that may accrue in some patients in consequence—might explain the apparent benefit of helmet NIV observed in a recent trial [1]. The mechanism accounting for this increase is unclear, potentially due to either a reduction in leak or a reduction in expiratory muscle activation. Studies are required to confirm this clinical finding and to delineate the responsible mechanisms. Of note, this report is not intended to suggest that helmet NIV should be applied with identical settings to face mask NIV, as previous investigators have shown that increases in pressure are required to unload the respiratory muscles because of lags in the pressurization of the helmet [4]. Rather, these results suggest the possibility that for any given pressure applied, helmet NIV may more effectively maintain EELV in comparison to the face mask interface.
Acknowledgements
The authors acknowledge the valuable contributions of Mr. Tim Slogan RRT, Mr. John Traill RRT and Ms. Vagia Campbell RRT to this research letter.
Abbreviations
- ARDS
Acute respiratory distress syndrome
- EELI
End-expiratory lung impedance
- EELV
End-expiratory lung volume
- EIT
Electrical impedance tomography
- EPAP
Expiratory positive airway pressure
- IPAP
Inspiratory positive airway pressure
- NIV
Non-invasive ventilation
- TIV
Tidal impedance variation
Authors’ contributions
KCT, MK, LP, SL, LJB and ECG contributed to the study conception and design and to the analysis/interpretation of data and manuscript preparation. All authors have approved the submitted version.
Funding
N/A
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Consent for publication was obtained from the 3 patients/legal representatives, although was later withdrawn in the third case.
Consent for publication
As above, consent for publication was obtained from the 3 patients/legal representatives, although was later withdrawn in the third case.
Competing interests
KT: Dr. Tatham reports grants from National Institute for Health Research (UK), the Academy of Medical Sciences and the European Institute of Innovation and Technology, outside the submitted work.
LB: Dr. Brochard reports grants from Medtronic Covidien, grants and non-financial support from Fisher Paykel, grants and non-financial support from Air Liquide, non-financial support from General Electric, from Philips, outside the submitted work.
EG: Dr. Goligher is supported by an Early Career Investigators Award from the Canadian Institutes of Health Research. Dr Goligher also reports non-financial support from Draeger, non-financial support from Timpel, personal fees and non-financial support from Getinge, outside the submitted work.
All remaining authors have nothing to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2016;315(22):2435–2441. doi: 10.1001/jama.2016.6338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobylianskii J, Murray A, Brace D, Goligher E, Fan E. Electrical impedance tomography in adult patients undergoing mechanical ventilation: a systematic review. J Crit Care. 2016;35:33–50. doi: 10.1016/j.jcrc.2016.04.028. [DOI] [PubMed] [Google Scholar]
- 3.Mauri T, Eronia N, Abbruzzese C, et al. Effects of sigh on regional lung strain and ventilation heterogeneity in acute respiratory failure patients undergoing assisted mechanical ventilation. Crit Care Med. 2015;43(9):1823–1831. doi: 10.1097/CCM.0000000000001083. [DOI] [PubMed] [Google Scholar]
- 4.Vargas F, Thille A, Lyazidi A, Roche Campo F, Brochard LJ. Helmet with specific settings versus facemask for noninvasive ventilation. Crit Care Med. 2009;37(6):1921–1928. doi: 10.1097/CCM.0b013e31819fff93. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.