Abstract
Background:
To examine trends in state-level policy support for sexual minorities and HIV outcomes among MSM.
Methods:
This longitudinal analysis linked state-level policy support for sexual minorities (N=94 Metropolitan Statistical Areas [MSAs] in 38 states) to 7 years of data (2008–2014) from CDC on HIV outcomes among MSM. Using latent growth mixture modeling, we combined 11 state-level policies (e.g., non-discrimination laws including sexual orientation as a protected class) from 1999–2014, deriving 3 latent groups: consistently low policy support; consistently high policy support; and increasing trajectory of policy support. Outcomes were HIV diagnoses per 10,000 MSM; late diagnoses (number of deaths within 12 months of HIV diagnosis and AIDS diagnoses within three months of HIV diagnosis) per 10,000 MSM; AIDS diagnoses per 10,000 MSM with HIV; and AIDS-related mortality per 10,000 MSM with AIDS.
Results:
Compared to MSAs in states with low levels and increasing policy support for sexual minorities, MSAs in states with the highest level of policy support had lower risks of HIV diagnoses (Risk Difference [RD]=−37.9, 95% Confidence Interval [CI]: −54.7, −21.0), late diagnoses (RD=−12.5, 95% CI: −20.4, −4.7), and AIDS-related mortality (RD=−33.7, 95% CI: −61.2, −6.2), controlling for time and 7 MSA-level covariates. In low policy support states, 27% of HIV diagnoses, 21% of late diagnoses, and 10% of AIDS deaths among MSM were attributable to policy climate.
Conclusion:
State-level policy climate related to sexual minorities was associated with HIV health outcomes among MSM and could be a potential public health tool for HIV prevention and care.
Keywords: HIV, AIDS, Men who have sex with men, sexual minority, policy
HIV has disproportionately affected men who have sex with men (MSM), the group experiencing the highest prevalence of HIV in the United States (U.S.). In 2017, gay and bisexual men and other MSM accounted for 70% of new HIV diagnoses, and 82% of diagnoses among men ages 13 and older.1,2 At current rates, an estimated 1 in 6 MSM in the U.S. will be diagnosed with HIV in their lifetime.3,4 Ecosocial5 and social stress6,7 theories posit that the social conditions in which individuals are embedded influence their health. Drawing on these theories, researchers have examined legal and policy environments as determinants of population health outcomes—ranging from smoking8,9 to violence/victimization10,11 to mental health12,13—because these policy environments shape individuals’ exposures to social conditions that either promote or undermine health. While HIV outcomes are influenced by a wide range of social, economic, epidemiologic, and structural forces,14–22 there is a relative dearth of research on the influence of population-level legal and policy environments on HIV outcomes among MSM.
In the past 20 years, all 50 states have either implemented policies that provide protections based on sexual orientation (e.g., in public accommodations and in hate crime laws) or that have limited legal protections for sexual minorities (e.g., constitutional amendments banning same-sex marriage, HIV criminalization). An emerging literature over the past decade has demonstrated that these state-level policies are associated with a wide range of outcomes among lesbian, gay, and bisexual (LGB) populations, including mental (e.g., suicidality, psychiatric morbidity), behavioral (e.g., problematic alcohol use), and physical (e.g., physiological stress reactivity) health.23–25 Further, recent studies have documented associations between state- and national-level policies and HIV prevention behavior among MSM, such as pre-exposure prophylaxis (PrEP) use, HIV testing, and condom use.26,27 While these studies have provided important initial insights, they have a number of limitations, including relying on cross-sectional designs, using select samples of MSM, examining a relatively small number of laws and policies, and combining measures of laws and policies with other social determinants (e.g., community-level attitudes),26,27 which makes it difficult to disentangle the potentially unique role of laws and policies in shaping HIV outcomes.
To better understand whether structural factors shape HIV-related outcomes among MSM, we used a prospective design that modeled the historical trajectory of the adoption of state-level policy support for sexual minorities (1999–2014), and grouped states according to their historical record. We then determined whether historical policy trajectories were associated with failure to achieve specific population-level stages of the HIV care continuum among MSM, including: 1) incident HIV diagnoses; 2) late HIV/AIDS diagnoses; 3) AIDS diagnoses among MSM living with HIV; and 4) AIDS-related mortality among MSM living with AIDS. We examined these outcomes from 94 large metropolitan statistical areas (MSAs) in the U.S., and hypothesized that MSAs located within states with more legal protections for sexual minorities would evidence more beneficial HIV outcomes among MSM, relative to MSAs within states with fewer legal protections.
Methods
This analysis examined associations between state-level policy trajectories and HIV outcomes among all large MSAs (>500,000 residents in the 1990 Census) in the United States (N=94 MSAs), except two: Puerto Rico was excluded because of incomplete outcome monitoring, and Washington, D.C. was excluded given our focus on state-level policies. These 94 MSAs were nested within 38 states. The four MSAs that crossed state boundaries were assigned to the state where the majority of respondents resided (Table S1).
Outcomes
The four study outcomes were obtained from the Centers for Disease Control and Prevention (CDC). We requested and were granted access to anonymized, longitudinal HIV/AIDS surveillance data aggregated to the MSA level via the National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention. Study outcomes include: 1) HIV diagnoses per 10,000 MSM; 2) late diagnoses, defined as number of deaths within 12 months of HIV diagnosis and AIDS diagnoses within 3 months of HIV diagnosis per 10,000 MSM; 3) AIDS diagnoses per 10,000 MSM with HIV; and 4) AIDS mortality, defined as death (from any cause) for any person ever classified as having AIDS, per 10,000 MSM with AIDS.
We examined these outcomes from 2008–2014. Nationwide, name-based HIV surveillance was considered complete beginning in 2008.28 We chose to terminate the study in 2014 because policy coding of the primary exposure (below) was only available through 2014.
Exposure
Our primary exposure was the trajectory of state-level support for sexual minorities in the 38 states that contained the 94 MSAs. We chose to examine state laws because the majority of protections for sexual minorities are enacted at the state level, rather than at the MSA level. The creation of the state policy variable included two steps. First, we used measures of nine different laws that provide protections based on sexual orientation, and measures of two laws that limit legal protections for sexual minorities (Table 1). Laws were obtained from 1999 to 2014. Following best practices in public health law research, policy coding was performed by two coders with expertise in legal and policy analysis (inter-coder reliability was over 95%). We chose to group multiple policies, rather than examine the effects of single policies individually, because individual policies are highly correlated with each other, and because our interest was in capturing the overall influence of state policies on HIV health outcomes.
Table 1.
State Laws by Category
| Laws conferring legal protections for sexual minorities |
|---|
| Employment non-discrimination |
| Housing non-discrimination |
| Public accommodations non-discrimination |
| State joint adoption |
| Same-sex marriage and comprehensive relationship recognition |
| Medical-decision making |
| School anti-bullying |
| School non-discrimination |
| Hate crimes |
| Laws limiting protections for sexual minorities |
| HIV criminalization |
| Same-sex marriage ban |
After obtaining the state policy values for each state in each year, we next used a growth mixture model to create a policy class variable. We chose this approach, rather than modeling the laws continuously over time, because we were interested both in capturing the overall trajectory of state policy support and in classifying similar states according to these trajectories, rather than in evaluating individual state variations in policy adoption. Growth mixture models identify latent, shared time trends among states.29 Using this methodology, we assigned states to one of three classes (based on interpretability and model fit): 1) states with “consistently high policy support” had a relatively high number of legal protections throughout the study duration (21% of states); 2) states with “increasing trajectory of policy support” had a low number of legal protections in 1999 but by 2014 had evidenced a sharp increase (21% of states); 3) and states with “consistently low policy support” had very few legal protections throughout (58% of states). Figure 1 shows the civil rights policy classes generated by the growth mixture model. Figure 2 shows a map of the states grouped by policy class. More detailed information regarding the state policy variable is available in the Online Supplement (Appendix A).
Figure 1: Three-Group Solution of State Policy Classes Based on Historical Trajectories of State Policy Support for Sexual Minorities in the United States, 1999–2014.
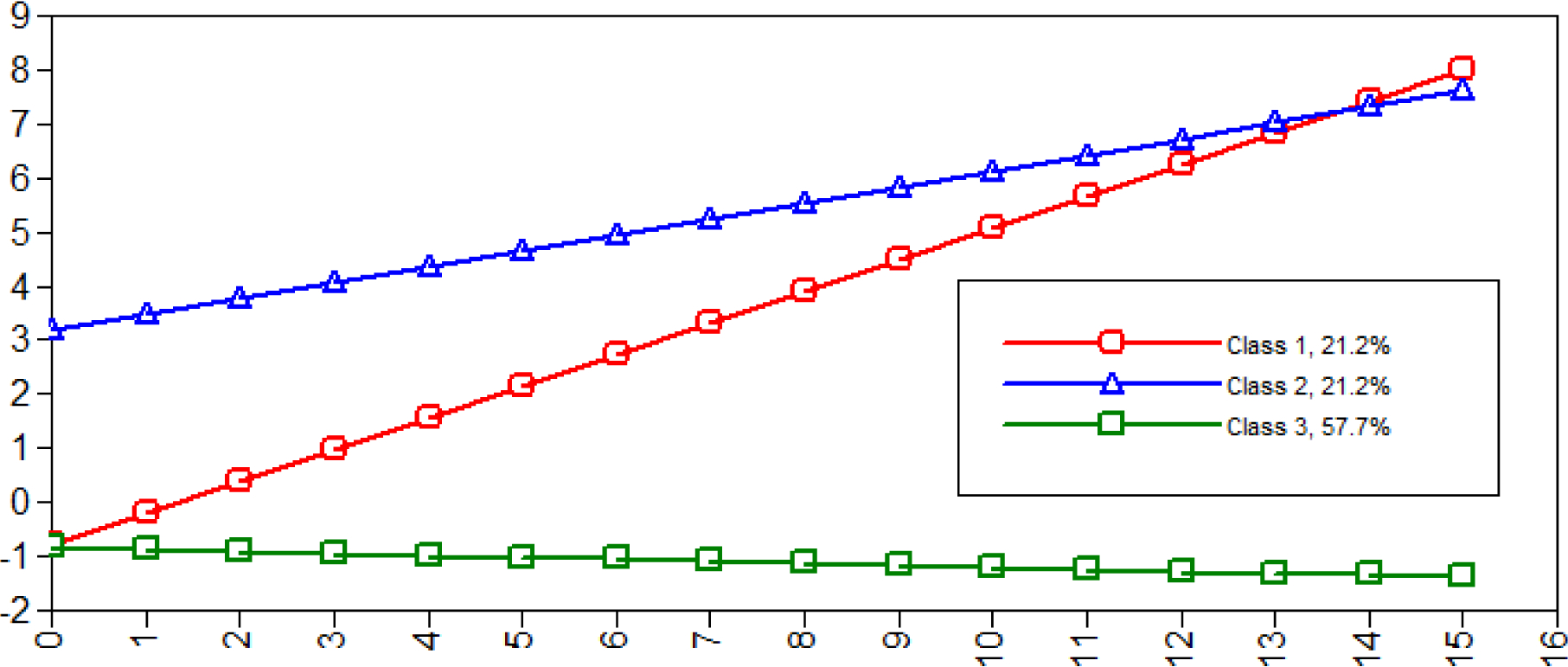
Note: X-axis is time, with 1999 equivalent to time 0 and 2014 equivalent to time 15; Y-axis is number of laws, where laws providing protection are coded as “1” and laws limiting protection were coded as “−1” for each state at every time point. Using the three-group solution, we refer to states categorized in Class 1 as “Increasing trajectory of policy support,” those in Class 2 as “Consistently high policy support,” and those in Class 3 as “Consistently low policy support.”
Figure 2: State Policy Support for Sexual Minorities in the United States, 1999–2014.
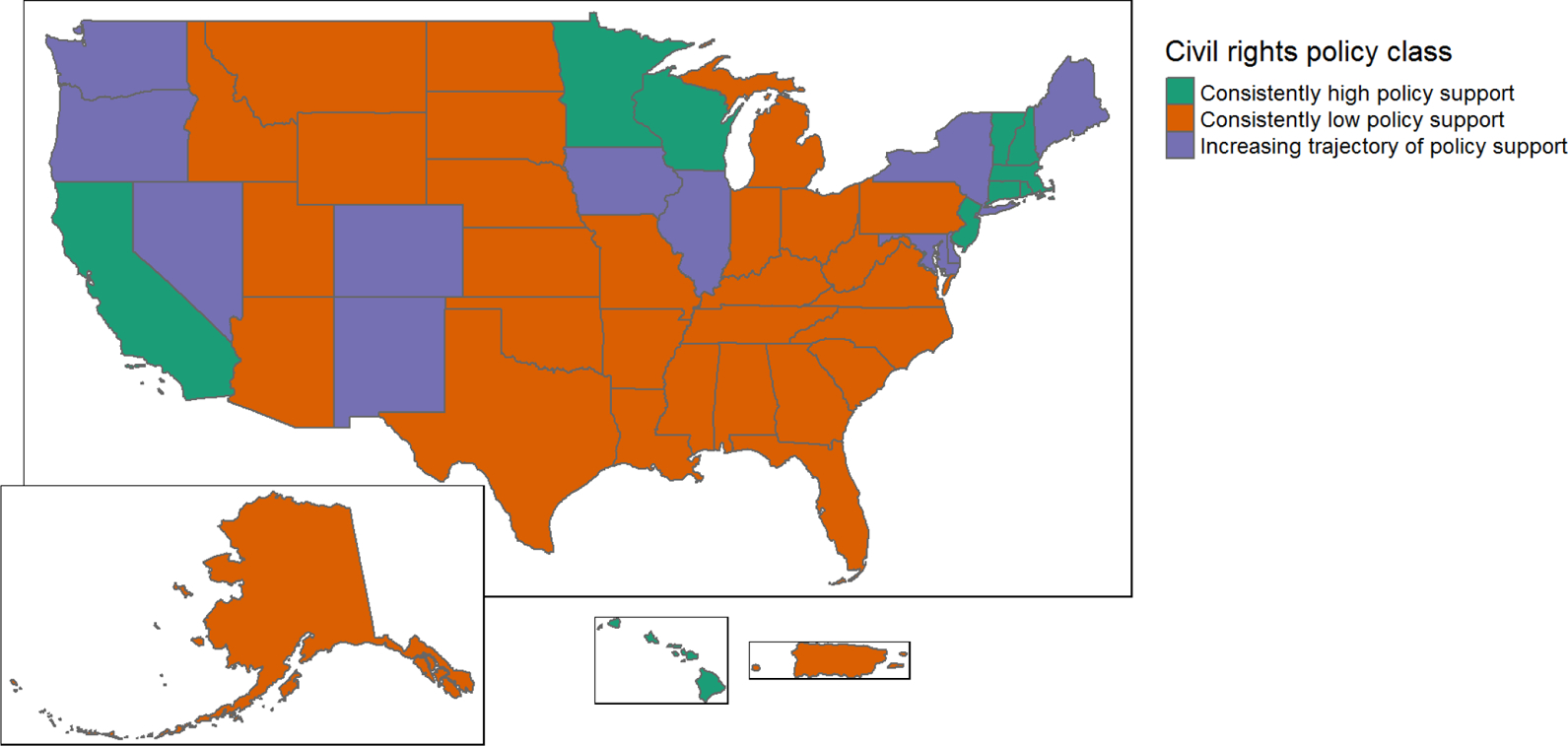
Note: PR was excluded from subsequent regression models due to incomplete outcome monitoring; Washington, D.C., was excluded because our research question pertained only to laws at the state level.
The majority of the 94 MSAs included in our analysis (N=54, 57%) were in states with the fewest legal protections, 25 MSAs (27%) were in states with the most legal protections, and 15 (16%) were in states with increasing legal protections. Supplemental Table S1 provides details on which MSAs were included from which states, and how each state was classified according to its policy trajectory.
Covariates
Laws are not randomly assigned. Consequently, to minimize spurious associations between HIV outcomes and state-level policies, we controlled for their potential common causes, including the percent non-Hispanic White adults ages 15–64 per total population ages 15–64; the sex ratio among the non-Hispanic White population, defined as total non-Hispanic White males divided by females in the population ages 18–64; the percentage of men below the poverty line; the percentage of men ages 25 and up without a high school diploma or equivalent, per the entire male population ages 25 and up; and population density, defined as the total population per the total MSA land area in square miles. HIV/AIDS transmission and outcomes are influenced by these demographic and economic characteristics of communities;1–5 further, these area-level demographic and economic characteristics may also shape social norms that influence the enactment of state-level policies related to sexual orientation.6,7 Because presence of MSM in the population influences HIV/AIDS prevalence and sexual networks,8 and may also predict political mobilization and/or organization,9,10 we additionally controlled for the total number of MSM per total population ages 15–64. For a detailed description of how MSM were measured, and a sensitivity analysis using an alternate measure, see Appendix D. Religious attitudes may confound the relationship between area-level policies and HIV outcomes for various reasons: they may serve as a proxy for homonegative attitudes;11–13 they influence political mobilization;14,15 and the presence of religious institutions predicts some HIV/AIDS outcomes (particularly among Black MSM).16 Consequently, we further controlled for the concentration of religious congregations, defined as total number of congregations per total population multiplied by 10,000.
All covariates were measured at the MSA level and were standardized to the mean value across all MSAs in 2008. See Supplemental Table S2 for further details about variable measurement, data sources and years of coverage, as well as Appendix C for further details about measurement of MSM and sensitivity analyses with an alternative measure of that variable.
All models were additionally controlled for calendar year, centered at 2008, given preliminary analyses showing that rates of late diagnoses, AIDS diagnoses, and AIDS mortality declined over time.
Statistical Analysis
We used multilevel modeling to assess associations between state policy class and the HIV outcomes among MSM. We performed 3-stage multilevel modeling, nesting repeated observations over time within MSAs, and MSAs within states, to account for clustering within MSAs and within states. We chose to use repeated measures rather than state and MSA fixed effects because we were not only concerned about confounding due to differential state- or MSA-level characteristics but also about non-independence of outcomes due to clustering within states and MSAs. Additionally, to understand the impact of differential policy climates on HIV outcomes for which we observed clinically meaningful reductions, we calculated a population attributable fraction (PAF), with the formula , for the groups being compared, i.e., those living in the highest vs. lowest policy support environment.30,31 We compared the MSAs with consistently low policy support (“exposed”) to those with consistently high policy support (“unexposed”) to determine the proportion of HIV outcomes in the MSAs with consistently low policy support that are attributable to state-level policy climate, adjusted for all other covariates. Another interpretation of the PAF is the proportion of HIV outcomes in the MSAs with consistently low policy support that could have theoretically been prevented if the MSAs instead had consistently high policy support. More detail on calculation of PAF is included in the Supplement in Appendix D.
Outcomes were distributed approximately normally and were not transformed; risks of each outcome were estimated using the covariate-adjusted model-based predicted marginal effects per 10,000 at risk, and the comparative statistics shown are risk differences per 10,000 at risk, with the reference group set at MSAs with consistently low policy support. There were no missing data for the 94 MSAs included in the analysis between 2008–2014.
Growth curve analyses and figures were produced using MPlus.32 All other analyses were performed using SAS 9.4 and figures were produced using R.33 The statistical code for all models is available in the Supplement in Appendix E.
Results
MSAs in states with consistently low policy support had on average 97 new cases of HIV diagnoses per 10,000 MSM, adjusted for covariates (Table 2). MSAs in states with increasing trajectory of policy support experienced an 18% decrease in HIV diagnoses, with an adjusted average of 79 new cases of HIV (Risk Difference [RD]=−28.0, 95% Confidence Interval [CI]=−49.5, −6.4; adjusted RD [ARD]=−17.3, 95% CI: −35.3, 0.7). MSAs in states with consistently high policy support experienced a 39% decrease in HIV diagnoses, with an adjusted average of 59 new cases (RD=−30.5, 95% CI: −48.3, −12.6; ARD=−37.9, 95% CI: −54.7, −21.0).
Table 2:
Associations between State Policy Class and HIV Outcomes among Men Who Have Sex with Men, 2008–2014
| Model | Policy class | Outcome | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HIV diagnoses per 10,000 MSM | Late diagnoses per 10,000 MSM | AIDS diagnoses per 10,000 MSM with HIV | AIDS mortality per 10,000 MSM with AIDS | ||||||
| Risk | RD 95% CI | Risk | RD 95% CI | Risk | RD 95% CI | Risk | RD 95% CI | ||
| Controlled for time only | Consistently low policy support (reference) | 96.1 | N/A | 39.8 | N/A | 329.7 | N/A | 244.4 | N/A |
| Increasing trajectory of policy support | 68.1 | −27.9 (−49.5, −6.4) | 28.1 | −11.7 (−21.0, −2.3) | 294.0 | −35.7 (−74.2, 2.8) | 203.8 | −40.5 (−66.5, −14.6) | |
| Consistently policy high support | 65.6 | −30.5 (−48.3, −12.6) | 27.2 | −12.6 (−20.3, −4.8) | 304.8 | −25.0 (−56.9, 7.0) | 191.6 | −52.8 (−74.4, −31.3) | |
| Controlled for all covariates‡ | Consistently low policy support (reference) | 96.7 | N/A | 40.1 | N/A | 329.1 | N/A | 236.4 | N/A |
| Increasing trajectory of policy support | 79.4 | −17.3 (−35.3, 0.7) | 34.7 | −5.5 (−13.6, 2.7) | 302.0 | −27.1 (−68.2, 14.1) | 214.2 | −21.2 (−49.0, 6.5) | |
| Consistently high policy support | 58.9 | −37.9 (−54.7, −21.0) | 27.6 | −12.5 (−20.4, −4.7) | 305.0 | −24.1 (−64.4, 16.2) | 202.8 | −33.7 (−61.2, −6.2) | |
Note: All outcomes indicate per 10,000 at risk. All covariates standardized to 2008 mean values. Risks derived from covariate-adjusted model-based predicted population marginal effects. RD=Risk Difference; CI=Confidence Interval. Both models adjusted for time.
Covariates include: percent non-Hispanic White adults ages 15–64 per total population ages 15–64; sex ratio among the non-Hispanic White population age 18–64, defined as total non-Hispanic White males divided by females in the population ages 18–64; total number of MSM per total population ages 15–64; total number of religious congregations per total population multiplied by 10,000; percentage of men below of the poverty line; percentage of men ages 25 and up without a high school diploma or equivalent per number of men ages 25 and up; and population density, defined as the total population per the total MSA land area in square miles.
MSAs in states with consistently low policy support had on average 40 covariate-adjusted late diagnoses per 10,000 MSM at risk (Table 2). MSAs in states with increasing trajectory of policy support showed a 13% reduction, with an adjusted average of 35 late diagnoses (RD=−11.7, 95% CI: −21.0, −2.3; ARD=−5.5, 95% CI: −13.6, 2.7); MSAs with consistently high policy support evidenced a 31% reduction, with an adjusted average of 28 late diagnoses (RD=−12.6, 95% CI: −20.3, −4.8; ARD=−12.5, 95% CI: −20.4, −4.7).
MSAs in states with low policy support had an average of 329 covariate-adjusted AIDS diagnoses per 10,000 MSM with HIV (Table 2). MSAs in states with increasing trajectories of policy support and consistently high policy support evidenced reductions in AIDS diagnoses, with an adjusted average of 302 and 305 AIDS diagnoses, respectively; however, the confidence intervals overlapped for all estimates of risk differences, consistent with overall null findings for this outcome (RD for increasing trajectory of policy support=−35.7, 95% CI: −74.2, 2.8; ARD=−27.1, 95% CI: −68.2, 14.1; RD for consistently high policy support=−25.0, 95% CI: −56.9, 7.0; ARD=−24.1, 95% CI: −64.4, 16.2).
Finally, MSAs in states with low policy support had on average 236 covariate-adjusted AIDS deaths per 10,000 MSM with AIDS (Table 2). MSAs in states with increasing trajectories of policy support had a 9% reduction in AIDS deaths, with an adjusted average of 214 AIDS deaths (RD=−40.5, 95% CI: −66.5, −14.6; ARD=−21.2, 95% CI −49.0, 6.5); MSAs with consistently high policy support had a 14% reduction, with an adjusted average of 203 AIDS deaths (RD=−52.8, 95% CI: −74.4, −31.27; ARD=−33.7, 95% CI: −61.2, −6.2).
Results from the PAF analysis (Appendix D) indicated that 27% of HIV diagnoses, 21% of late diagnoses, and 10% of AIDS deaths in the consistently low policy support states were attributable to policy climate.
Discussion
In this 7-year longitudinal analysis, we examined associations between trajectories of state policy support for sexual minorities and HIV outcomes in all large MSAs in the U.S. In all adjusted models, MSAs in states with an increasing trajectory of policy support and with consistently high policy support showed reductions in HIV outcomes relative to MSAs in states with consistently low policy support. Further, MSAs in states with consistently high policy support had reductions in HIV diagnoses, late diagnoses, and AIDS-related mortality, of higher magnitude than states with increasing policy support, indicative of a dose-response relationship. Among MSAs in states with the highest level of policy support, there was a 39% reduction in HIV diagnoses, a 31% reduction in late diagnoses, and a 14% reduction in AIDS mortality compared to low policy support states; among those with an increasing trajectory of policy support, we observed an 18% reduction in HIV diagnoses, a 13% reduction in late diagnoses, and an 9% reduction in AIDS mortality relative to low policy support states. Another indicator of the magnitude of these effects comes from the population attributable fraction; this analysis found that in low policy support states, 27% of HIV diagnoses, 21% of late diagnoses, and 10% of AIDS deaths were attributable to the state policy climate and may have been preventable if these states instead implemented policy climates that were similar to the consistently high policy support states. Our findings are consistent with previous cross-sectional studies that have documented associations between composite indicators of national- and state-level policies and HIV outcomes among MSM,26,27 as well as with panel studies that have shown associations between same-sex marriage policies and rates of syphilis,34–36 an infection that is elevated among MSM in the U.S.
These results raise the question of what mechanisms explain why state-level policy environments may influence HIV outcomes among MSM. One possibility is suggested by recent evidence that MSM conceal their sexual orientation from others at greater levels if they live in countries10,37 and states38 that lack policy protections for sexual minorities. If MSM living with HIV conceal their identities more in states with fewer legal protections, they will be less likely to seek HIV testing and care and, when they do, less likely to receive adequate treatment and achieve an undetectable viral load. This increase in the proportion of MSM living with HIV who are not virally suppressed would theoretically be associated with an increased risk of illness for them, and transmission of HIV to others. Thus, less-supportive states would be more vulnerable to increased HIV incidence, late diagnoses, and AIDS-related mortality, outcomes strongly related to the state policy climate in our analysis.
Our study has several limitations. First, while the longitudinal design represents a methodological strength, we were only able to examine associations between state policies and HIV outcomes over a seven-year period. Second, our study focused on policies that were enacted at the state level, where many significant policy decisions related to sexual minorities are legislated. Our emphasis on distal policy climates at the state level also offers a conservative test, given that more proximal environments are likely to exert stronger effects. This approach, however, does not incorporate within-state heterogeneity, particularly with respect to local, municipal-level policy climates that may differ from those at the state level. Thus, exploring associations between municipal-level policies and HIV outcomes among MSM, as well as the relationships between state- and municipal-level policies in influencing HIV outcomes in this population, could provide additional information.
Third, while we controlled for seven state-level covariates to address potential alternative explanations, the potential for unobserved confounding remains. For instance, it is possible that other state-level policies influence both the passage of legal protections for sexual minorities as well as HIV-related outcomes among MSM, although it is unlikely that such policies would also lead to the dose-response pattern of results across HIV outcomes in MSM observed here. Still, future studies may wish to consider the use of quasi-experimental designs that examine changes in HIV outcomes among MSM following changes in specific state-level policies related to sexual orientation (e.g., a public accommodations law that is inclusive of sexual orientation). These quasi-experimental designs could also be used to examine changes in HIV outcomes among MSM after changes in other individual state-level policies that are unrelated to sexual orientation—for example, variation in Medicaid/Medicare reimbursements and qualifying conditions—but that may nevertheless have a disparate impact on sexual minority populations.
Fourth, a plausible alternative explanation for these findings is that healthier MSM leave states with less supportive climates for sexual minorities, leaving unhealthy respondents behind. To date, however, studies have not found strong support for a relationship between health and mobility patterns among LGB populations,39 suggesting that differential selection by health is unlikely to be responsible for these observed patterns. Fifth, the patterns we observed may operate differently both in rural areas that are not contained within our 94 MSAs, and in the 12 states that did not have any large MSAs and were thus excluded in our analysis; the extent to which our results generalize to these other contexts awaits further study.
Finally, the relatively small number of transgender persons did not permit an analysis of the state-level policy environment on HIV outcomes among this group. Yet, transgender populations are disproportionately affected by HIV,1 and the legislative environment is likely to influence, and potentially potentiate, risk for HIV outcomes among transgender MSM.40 Future analyses should therefore explore how state policy climates related to sexual orientation, gender identity, and race/ethnicity interact to shape HIV risk among MSM with intersectional identities (e.g., racial/ethnic minority MSM and transgender MSM). MSM and transgender persons, however, are not the only groups vulnerable to HIV, and for whom targeted laws and policies may influence transmission. For example, injection drug users are at a higher-risk of HIV than the general population, and policies prohibiting over-the-counter syringe sales—laws that are salient specifically to injection drug users—are related to increased HIV prevalence in this group.41 Similarly, among Black heterosexuals, another higher-risk group for HIV, rates of newly diagnosed HIV are influenced by state-level variation in minimum wage laws, which disproportionately impact Black Americans.42 Future research should continue to consider the impact of policy environments relevant to other at-risk populations when assessing determinants of HIV outcomes among those groups.
The U.S. recently launched an ambitious new initiative for addressing HIV in this country, called the Ending the HIV Epidemic Initiative.43 Our findings, together with those of other studies,26,27 suggest that state policies conferring legal protections for sexual minorities could potentially influence the likelihood of achieving the goals put forward in this Initiative.
Supplementary Material
Acknowledgements
We thank Gary Gates for providing the estimates of MSM from the Gallup survey data. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of Interest and Source of Funding: Funding for this study was provided by R01 DA037568 from the National Institute on Drug Abuse (NIDA). The authors have no conflicts of interest to declare
References
- 1.CDC. HIV and Gay and Bisexual Men; 2018. [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; Vol. 29; 2018. [Google Scholar]
- 3.Hess KL, Hu X, Lansky A, Mermin J, Hall HI. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27(4):238–243. doi: 10.1016/j.annepidem.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. 2016. Conference on Retroviruses and Opportunistic Infections. [Google Scholar]
- 5.Krieger N Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30(4):668–677. doi: 10.1093/ije/30.4.668 [DOI] [PubMed] [Google Scholar]
- 6.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aneshensel C, Phelan J. The sociology of mental health In: Aneshensel CS, Phelan JC, eds. Handbook of the Sociology of Mental Health. New York, NY: Springer; 1999:3–18. [Google Scholar]
- 8.Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325(7357):188–188. doi: 10.1136/bmj.325.7357.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans WN, Farrelly MC, Montgomery E. Do Workplace Smoking Bans Reduce Smoking? Am Econ Rev. 1999;89(4):728–747. doi: 10.1257/aer.89.4.728 [DOI] [Google Scholar]
- 10.Levy BL, Levy DL. When love meets hate: The relationship between state policies on gay and lesbian rights and hate crime incidence. Soc Sci Res. 2017;61:142–159. doi: 10.1016/J.SSRESEARCH.2016.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatzenbuehler ML, Schwab-Reese L, Ranapurwala SI, Hertz MF, Ramirez MR. Associations Between Antibullying Policies and Bullying in 25 States. JAMA Pediatr. 2015;169(10):e152411. doi: 10.1001/jamapediatrics.2015.2411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raifman J, Moscoe E, Austin SB, Hatzenbuehler ML, Galea S. Association of State Laws Permitting Denial of Services to Same-Sex Couples With Mental Distress in Sexual Minority Adults. JAMA Psychiatry. 2018;75(7):671. doi: 10.1001/jamapsychiatry.2018.0757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hainmueller J, Lawrence D, Martén L, et al. Protecting unauthorized immigrant mothers improves their children’s mental health. Science. 2017;357(6355):1041–1044. doi: 10.1126/science.aan5893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13(1):482. doi: 10.1186/1471-2458-13-482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson BT, Redding CA, DiClemente RJ, et al. A Network-Individual-Resource Model for HIV Prevention. AIDS Behav. 2010;14(S2):204–221. doi: 10.1007/s10461-010-9803-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–1044. https://linkinghub.elsevier.com/retrieve/pii/S0277953605000237. Accessed August 5, 2019. [DOI] [PubMed] [Google Scholar]
- 17.Wohlfeiler D Structural and environmental HIV prevention for gay and bisexual men. AIDS. 2000;14:S52–S56. doi: 10.1097/00002030-200006001-00008 [DOI] [PubMed] [Google Scholar]
- 18.Blankenship KM, Bray SJ, Merson MH. Structural Interventions in Public Health. Vol 14; 2000. http://californiaptc.com/wp-content/uploads/2016/06/Structural_interventions_in_public_health.3.pdf. Accessed August 5, 2019. [DOI] [PubMed] [Google Scholar]
- 19.Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural Interventions: Concepts, Challenges and Opportunities for Research. J Urban Heal. 2006;83(1):59–72. doi: 10.1007/s11524-005-9007-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blankenship KM, Reinhard E, Sherman SG, El-Bassel N. Structural Interventions for HIV Prevention Among Women Who Use Drugs. JAIDS J Acquir Immune Defic Syndr. 2015;69:S140–S145. doi: 10.1097/QAI.0000000000000638 [DOI] [PubMed] [Google Scholar]
- 21.Rosser BRS, Horvath KJ. Predictors of Success in Implementing HIV Prevention in Rural America: A State-Level Structural Factor Analysis of HIV Prevention Targeting Men who have Sex with Men. AIDS Behav. 2008;12(2):159–168. doi: 10.1007/s10461-007-9230-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singer M, Stopka T, Shaw S, et al. Lessons from the Field: From Research to Application in the Fight Against AIDS among Injection Drug Users in Three New England Cities. Hum Organ. 2005;64(2):179–191. http://www.jstor.org/stable/44127253. [Google Scholar]
- 23.Hatzenbuehler ML. Structural stigma: Research evidence and implications for psychological science. Am Psychol. 2016;71(8):742–751. doi: 10.1037/amp0000068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Link B, Hatzenbuehler ML. Stigma as an Unrecognized Determinant of Population Health: Research and Policy Implications. J Health Polit Policy Law. 2016;41(4):653–673. doi: 10.1215/03616878-3620869 [DOI] [PubMed] [Google Scholar]
- 25.Hatzenbuehler ML. Structural stigma and health In: Major B, Dovidio JF, Link BG, eds. The Handbook of Stigma, Discrimination and Health. Oxford: Oxford University Press; 2017:105–212. [Google Scholar]
- 26.Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, et al. State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS. 2015;29(7):837–845. doi: 10.1097/QAD.0000000000000622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pachankis JE, Hatzenbuehler ML, Hickson F, et al. Hidden from health. AIDS. 2015;29(10):1239–1246. doi: 10.1097/QAD.0000000000000724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Surveillance Systems | Statistics Center | HIV/AIDS | CDC. https://www.cdc.gov/hiv/statistics/surveillance/systems/index.html. Published 2015. Accessed August 5, 2019. [Google Scholar]
- 29.Ram N, Grimm KJ. Growth Mixture Modeling: A Method for Identifying Differences in Longitudinal Change Among Unobserved Groups. Int J Behav Dev. 2009;33(6):565–576. doi: 10.1177/0165025409343765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin C-K, Chen S-T. Estimation and application of population attributable fraction in ecological studies. Environ Heal. 2019;18(1):52. doi: 10.1186/s12940-019-0492-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miettinen OS. Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol. 1974;99(5):325–332. doi: 10.1093/oxfordjournals.aje.a121617 [DOI] [PubMed] [Google Scholar]
- 32.Muthén LK, Muthén BO. MPlus: Statistical Analysis With Latent Variables; 1998. www.StatModel.com. Accessed August 18, 2019. [Google Scholar]
- 33.R Core Team. R: A language and environment for statistical computing. 2013. http://www.r-project.org/. [Google Scholar]
- 34.Francis AM, Mialon HM, Peng H. In sickness and in health: Same-sex marriage laws and sexually transmitted infections. Soc Sci Med. 2012;75(8):1329–1341. doi: 10.1016/J.SOCSCIMED.2012.05.037 [DOI] [PubMed] [Google Scholar]
- 35.Dee TS. Forsaking All Others? the Effects of Same‐Sex Partnership Laws on Risky Sex. Econ J. 2008;118(530):1055–1078. doi: 10.1111/j.1468-0297.2008.02160.x [DOI] [Google Scholar]
- 36.Leichliter JS, Grey JA, Cuffe KM, et al. Geographic correlates of primary and secondary syphilis among men who have sex with men in the United States. Ann Epidemiol. 2019;32:14–19.e1. doi: 10.1016/J.ANNEPIDEM.2019.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pachankis JE, Bränström R. Hidden from happiness: Structural stigma, sexual orientation concealment, and life satisfaction across 28 countries. J Consult Clin Psychol. 2018;86(5):403–415. doi: 10.1037/ccp0000299 [DOI] [PubMed] [Google Scholar]
- 38.Riggle E, Rostosky S, Horne S. Does It Matter Where You Live? Nondiscrimination Laws and the Experiences of LGB Residents. Sex Res Soc Policy. 2010;7:168–175. doi: 10.1007/s13178-010-0016-z [DOI] [Google Scholar]
- 39.Hatzenbuehler ML, Flores AR, Gates GJ. Social Attitudes Regarding Same-Sex Marriage and LGBT Health Disparities: Results from a National Probability Sample. J Soc Issues. 2017;73(3):508–528. doi: 10.1111/josi.12229 [DOI] [Google Scholar]
- 40.White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222–231. doi: 10.1016/j.socscimed.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Friedman SR, Perlis T, Des Jarlais DC. Laws prohibiting over-the-counter syringe sales to injection drug users: relations to population density, HIV prevalence, and HIV incidence. Am J Public Health. 2001;91(5):791–793. doi: 10.2105/ajph.91.5.791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cloud DH, Beane S, Adimora A, et al. State minimum wage laws and newly diagnosed cases of HIV among heterosexual black residents of US metropolitan areas. SSM - Popul Heal. 2019;7:100327. doi: 10.1016/J.SSMPH.2018.100327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV Epidemic. JAMA. 2019;321(9):844. doi: 10.1001/jama.2019.1343 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


