Abstract
Initiatives for integration of mental health services into primary care are underway through the World Health Organization’s mental health Gap Action Programme (mhGAP) and related endeavors. However, primary healthcare providers’ stigma against persons with mental illness is a barrier to success of these programs. Therefore, interventions are needed to reduce stigma among primary healthcare providers. We developed REducing Stigma among HealthcAre ProvidErs (RESHAPE), a theoretically-grounded intervention that draws upon the medical anthropology conceptual framework of “what matters most.” RESHAPE addresses three domains of threats to what matters most: survival, social, and professional. In a proof-of-concept study, mental health service users and aspirational healthcare providers (primary healthcare providers actively incorporating mental health services) were trained to co-facilitate the RESHAPE intervention embedded within mhGAP training in Nepal. Two trainings with the RESHAPE anti-stigma component were held with 41 primary healthcare providers in Nepal. Evaluation of the training included four focus groups and 25 key informant interviews. Stigmatizing attitudes and role play-based clinical competency, assessed with the ENhancing Assessment of Common Therapeutic factors tool (ENACT), were evaluated pre-training and followed-up at four and 16 months. The study was conducted from February 2016 through June 2017. In qualitative interviews, primary healthcare providers described changes in perceptions of violence (survival threats) and the ability to treat mental illness effectively (professional threats). Willingness to interact with a person with mental illness increased from 54% pre-training to 81% at 16 months. Observed clinical competency increased from 49% pre-training to 93% at 16-months. This proof-of-concept study supports reducing stigma by addressing what matters most to healthcare providers, predominantly through mitigating survival and professional threats. Additional efforts are needed to address social threats. These findings support further exploration of service user and aspirational figure involvement in mhGAP trainings based on a “what matters most” conceptual framework
Keywords: Developing countries, Discrimination, Medical anthropology, Mental health, Patient participation, Primary health care, Social stigma, Teaching
1. Introduction
1.1. Stigma against mental illness among healthcare professionals
As a social species, human beings react to others’ suffering with empathy and behavioral drives to alleviate distress (de Waal and Preston, 2017). Across societies, certain individuals are recognized for their role helping others in distress. For healthcare professionals, in particular, the alleviation of suffering is a vocational calling. Given these sociobiological drives and professional roles, why do healthcare professionals often ostracize, discriminate against, and fail to provide adequate palliation of suffering for some groups of patients (Henderson et al., 2014; Nyblade et al., 2019)? Persons with infectious diseases are often stigmatized, and among noncommunicable diseases, persons with psychiatric disorders bear the burden of healthcare providers’ prejudice and discrimination. This stigmatization is associated with poor healthcare delivery including inadequate screening, diagnosis, and treatment leading to early mortality, especially in low- and middle-income countries (LMIC) (Kane et al., 2019).
Understanding how to reduce stigma among healthcare providers is now of particular relevance because of the global push to integrate mental health services into primary care in both high-income countries and LMIC. Primary care providers are increasingly involved because of shortages of mental health specialists and the benefits of collaborative care models for both mental and physical health (Kroenke and Unutzer, 2017; World Health Organization, 2016). For settings where primary care providers lack prior mental health training, the World Health Organization (WHO) has developed the mental health Gap Action Programme (mhGAP) intervention guide and training materials (www.who.int/mental_health/mhgap/). However, failure to promote positive attitudes and reduce stigma already has been observed as a barrier to success of mhGAP and similar initiatives: the presence of stigma has been associated with low rates of detecting mental illness and poor clinical competency (Fekadu et al., 2017; Jenkins et al., 2013; Kauye et al., 2014; Kohrt et al., 2018b; Muga and Jenkins, 2008).
1.2. What matters most: an anthropological theory to inform of anti-stigma interventions
Stigma is a heterogeneous concept including a range of behaviors and experiences. Taxonomies of stigma have expanded rapidly in the past decade (Pescosolido and Martin, 2015): “experiential variants” include perceived, endorsed, anticipated, received, and enacted stigma; “action-oriented variants” include self, courtesy, public, provider-based, and structural stigma. Healthcare provider stigma is an example of provider-based stigma, defined as “prejudice and discrimination voiced or exercised, consciously or unconsciously, by occupational groups designated to provide assistance to stigmatized groups,” (Pescosolido and Martin, 2015, p. 92). Traditionally, most interventions for provider stigma are developed from knowledge-attitude-practice (KAP) frameworks, which assume that if a provider has a more accurate biomedical understanding of mental illness, this will result in improved attitudes and behaviors. However, there have been numerous examples of knowledge-based approaches that do not result in attitudinal and behavioral changes, and some have negative impacts (Stuart et al., 2012). Although healthcare providers typically have greater biomedical knowledge of mental illness, this is not protective against stigmatizing attitudes and behaviors (Henderson et al., 2014; Thornicroft et al., 2016; Ungar et al., 2016). Therefore, other approaches are needed to reduce stigma among healthcare providers.
An alternative to the KAP framework is ‘what matters most’, an anthropological theory grounded in the concept of moral experience within one’s local world (Kleinman, 1999). ‘What matter most’ conceptualizes stigma as a moral phenomenon in which threats to personal and group identity within a particular local world lead to stigmatizing behaviors (Keusch et al., 2006; Kleinman, 2006; Yang et al., 2007, 2014a). Healthcare providers’ moral experience is shaped by the structure, symbols, and rituals in a specific healthcare setting (Kleinman and Hall-Clifford, 2009). Ethnographies have been written about medical students conducting psychiatry rotations, psychiatry residents in training, and emergency room staff caring for psychiatric patients, and each of these captures the complex moral experience of mental healthcare within particular local worlds (Konner, 1988; Luhrmann, 2000; Rhodes, 1991). A common narrative is that the social status associated with being a healer and the self-image of being able to alleviate suffering are threatened when facing a patient with mental illness—especially when that health professional does not have the psychiatric training or tools to provide effective care.
Local worlds of healthcare providers also are shaped by broader societal norms, values, and practices (Baer et al., 2003). One cannot consider the local world of a healthcare provider without considering the range of societal attributes that shape other life experience, such as language, religion, caste, gender, age, and economic status. Those values held closely by one’s culture (e.g., religious identity, national identity) will lead to stigmatization when jeopardized (Yang et al., 2014b). For example, in capitalist cultures, economic productivity is an aspect of identity, which can lead to stigmatization of those perceived as burdens on society (Scheff, 2017; Yang et al., 2014a).
1.3. Designing ‘what matters most’ interventions using social contact
Social psychology theory emphasizes social contact as an active ingredient of successful stigma-reduction strategies. Social contact is hypothesized to breakdown in-group versus out-group differences (Pettigrew et al., 2011). During the Civil Rights era in the United States, social psychologists focused on social contact to reduce racial barriers, using activities such as racially-mixed student groups working together toward common goals, e.g., jigsaw classrooms (Allport, 1954). There have been more than 500 experimental and observational studies of social contact, with the majority reporting reduction in prejudice (Pettigrew et al., 2011). Interventions facilitating social contact—outside of a clinical care relationship—between healthcare providers and service users with a stigmatized condition have shown benefit for reducing stigma and discrimination (Corrigan et al., 2012; Henderson et al., 2014; Nyblade et al., 2019). A qualitative synthesis of effective anti-stigma interventions identified multiple forms of social contact as one of the key ingredients (Knaak et al., 2014).
Although social contact interventions hold promise, there are some studies with neutral or negative results, and there are limited data on behavioral change and long-term sustainability of attitudinal change (Thornicroft et al., 2016). This leaves open an opportunity to explore what can be achieved when using social contact to target moral experience as a driver of stigma. A moral experience perspective suggests that interventions would work best when social contact addresses ‘what matters most’ to the stigmatizing group. This will vary based on local cultural and professional beliefs related to perceived threats such as violence, contagion, violation of religious norms, economic dependency, and failure to fulfill expected social and professional roles.
1.4. Objectives of study
We employed the ‘what matters most’ conceptual framework and findings from social psychology to design an intervention for reducing primary care providers stigma against patients with mental illness. We conducted a proof-of-concept testing in rural Nepal including qualitative and quantitative evaluations.
2. Methods
2.1. Setting and context
Recent development of primary care-based mental health services in Nepal provided a platform for developing and testing an anti-stigma intervention (Jordans et al., 2016). Nepal exemplifies settings with a high burden of negative social determinants of health and lack of mental health specialist services outside of urban centers (Luitel et al., 2015). Beginning in 2012, Nepal was one of five LMIC participating in the PRogramme for Improving Mental health carE (PRIME), in which mental health services were introduced into primary care and community settings (Lund et al., 2012). PRIME in Nepal was implemented in Chitwan district by Transcultural Psychosocial Organization (TPO) Nepal, a Nepali non-governmental mental health organization. Within PRIME, a district mental health plan included training for all primary care providers in the government health system. The plan addressed four mental, neurological and substance use (MNS) disorders: depression, psychosis, alcohol use disorder, and epilepsy (Jordans et al., 2016). These four conditions were selected based on a local priority setting exercise that also highlighted the need for stigma reduction for these conditions (Jordans et al., 2013). Primary care providers in government facilities include health assistants, community medical assistants, and auxiliary nurse midwives, all of whom are non-specialists with training ranging from 10 to 30 months. Some health facilities also include medical doctors with bachelor of medicine/bachelor of surgery (MBBS) credentials.
In the Nepal PRIME district plan, primary care providers who had prescribing rights (herein referred to as ‘prescribers’) were trained using mhGAP and a psychosocial curriculum. The training was 10-days for 6.5 h each day (see Supplemental Table S1). The first 4.5 days included psychosocial concepts, verbal and non-verbal communication skills, psychoeducation, emotional support, and case management. The remaining time was focused on mhGAP material for the four priority MNS disorders. Primary care providers who did not have prescribing rights (referred to as ‘non-prescribers’) were trained for 5 days on the same basic psychosocial support skills, and a subset was trained for an additional 5 days in psychological interventions. Both prescribers and non-prescribers were obliged to attend the PRIME trainings by the local government administration. The health workers did not have the option of electing out of the trainings, and all received government rate per-diem for attendance.
2.2. Development of the REducing stigma among HealthcAre ProvidErs (RESHAPE) intervention
We developed an anti-stigma intervention entitled REducing Stigma among HealthcAre ProvidErs (RESHAPE) based on ‘what matters most’ and social contact theories. The development followed three steps: (1) identification of what matters most to primary care providers; (2) selection of components for the intervention; and (3) recruitment and training of service users and other facilitators for the anti-stigma activities.
2.2.1. Identification of ‘what matters most’ to healthcare providers
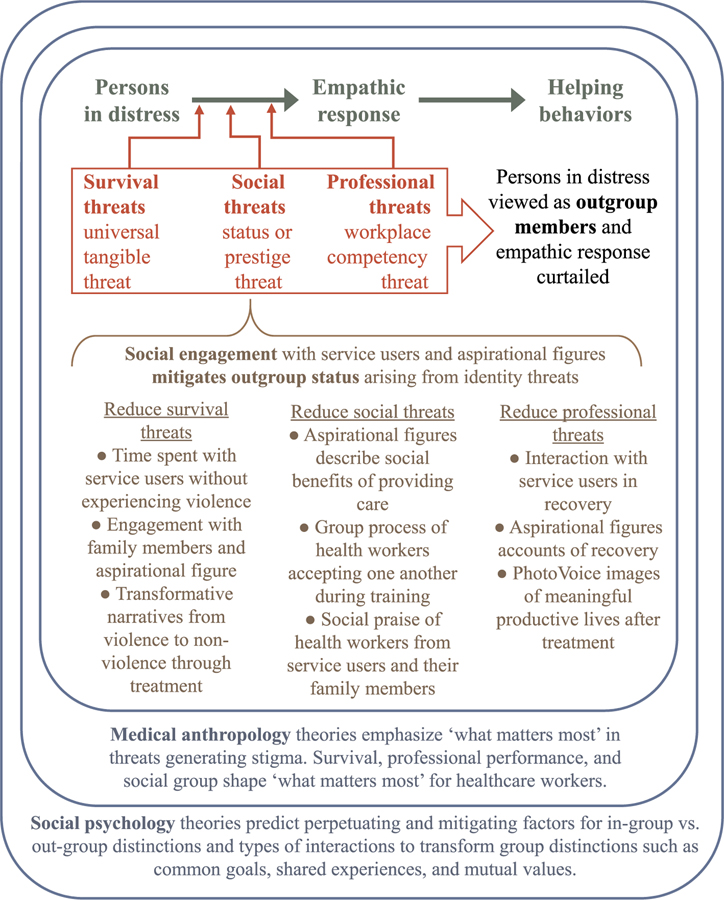
The first step in the RESHAPE process was to identify potential threats to ‘what matters most’. We began with general domains: survival, social, and professional threats (Griffith and Kohrt, 2016; Stangl et al., 2019). We contextualized these threats from ethnographic and other qualitative research on mental illness stigma in Nepal.
Survival threats –
Patients, such as persons with HIV or Ebola, are stigmatized, in part, because of the perceived threat to survival of a healthcare provider. The dominant survival threat when caring for patients with mental illness is typically violence with a potential to injure or kill someone, including healthcare providers. This is a ‘universal tangible threat’ because it can be observed across local worlds of experience (Yang et al., 2013). This is observable in Nepal. In Chitwan, Nepal, more than a third of healthcare providers thought patients with mental illness were too violent to receive treatment in primary care settings (Gartoulla et al., 2015). The association with violence and mental illness is supported by ethnographic studies documenting that mental illness is seen as a problem of the ‘brain-mind’ (Nepali: dimaag), which, when damaged or impaired, leads to a loss of inhibition; both psychosis and substance abuse disorders are associated with this lost inhibition and risk of violence (Kohrt and Harper, 2008).
Social threats –
Social threats jeopardize the status and prestige of a healthcare provider. This is manifest as anticipated stigma that a healthcare provider will be ostracized by co-workers, community members, and their families because of associating with persons with mental illness. There is a concern among health workers that those who treat patients with mental illness are also mentally ill: “paagal ko daktar pani paagal ho” (the doctor of mad patients is also mad). Primary care providers caring for mental health patients fear that they will become stigmatized just as psychiatrists are shunned in society: ‘‘For families, it is a bigger shame to have a child who is a psychiatrist than to have a child who is not a doctor at all,’’ (Kohrt and Harper, 2008, p. 480). Instead of ‘glory and support’ received in some health fields, engaging with persons with mental illness is associated with being stigmatized and discriminated against (Gurung et al., 2017). Because persons with mental illness in rural areas are often excluded from community groups, festivals, and social activities, there is a fear among healthcare providers that they will similarly be excluded (Angdembe et al., 2017).
Professional threats –
Healthcare providers also avoid mental health care because they see it as burdensome and ineffective (Kohrt and Harper, 2008), thus threatening their self-image as a competent professional. In the local world of healthcare providers, self-efficacy in performing one’s clinical duties is at the heart of moral experience. Among health workers in Chitwan, 90% reported that it was not worthwhile to provide care because patients with mental illness will discontinue their medication and not follow-up, and 72% of the health workers thought that patients with mental illness do not have supportive families to assist in their care (Gartoulla et al., 2015). Another attitude in Nepal was that mental health patients cannot understand treatment and do not follow healthcare providers instructions (Kisa et al., 2016). Primary care workers and many of their supervisors also felt that only specialist care or traditional healers would be effective for treatment (Angdembe et al., 2017; Kisa et al., 2016). Fewer than 10% of healthcare providers considered counseling to be effective (Gartoulla et al., 2015). Suicide, in particular, carries a high stigma. This is partly because health professionals inaccurately think suicide is illegal and therefore should be dealt with only by police (Hagaman et al., 2016). In addition, healthcare providers do not ask about suicidality because it is a “hopeless situation” and attribute it to things that cannot be changed such as fate or personality characteristics (Hagaman et al., 2018).
Also regarding professional threats, primary care providers consider mental health patients to be a burden forced upon them by the government and non-governmental organizations (NGOs) (Kisa et al., 2016). Some healthcare providers only attend for the daily payment but do not deliver care because of the perceived burden: “if NGOs add tasks to [primary care providers], then they need incentives to do it. They think NGOs are consuming their time. They may do it initially but, if they are not provided facilities, they may stop doing it,” (Angdembe et al., 2017, p. 11). This is relevant in the context of PRIME in Nepal because the local government obligated all primary care workers to attend the mental health trainings. Additionally, caring for mental health patients in primary care was not seen as valuable because they are not economically productive members of society (Angdembe et al., 2017). Three quarters of health workers in Chitwan thought that patients with mental illnesses—including depression and anxiety—should be barred from work (Gartoulla et al., 2015); therefore, even if one recovers, she/he should not return to work.
These findings were used to frame the content of what matters most for primary care providers in the RESHAPE intervention.
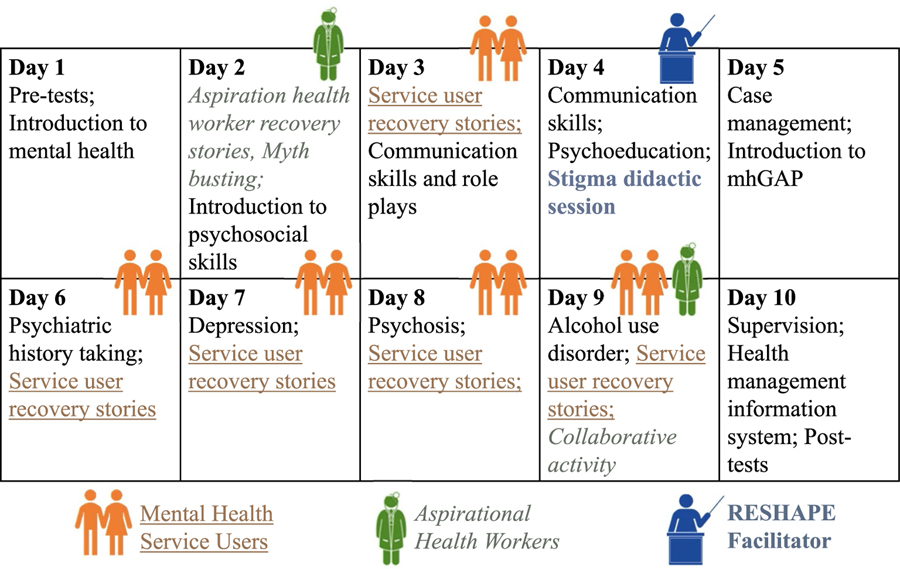
2.2.2. Design of RESHAPE intervention components
Five components (service user recovery stories and social contact; aspirational figures; myth busting; stigma didactics; and collaboration) were selected for the RESHAPE intervention based on evidence-supported elements of anti-stigma interventions (see Fig. 1). The ‘what matters most’ themes were incorporated into each of these components. The anti-stigma components were designed to be embedded within the 10-days training for prescribers (see Fig. 2) and the 5-days training for non-prescribers. The total number of days of prescriber and non-prescriber training were not increased with the addition of RESHAPE elements. Trainers were Nepali psychiatrists and psychosocial counselors employed by TPO Nepal. The NGO had established a memorandum of understanding with the Ministry of Health to provide the PRIME trainings. The psychiatrists and psychosocial counselors had been involved in the Nepali adaptation of mhGAP. Psychosocial counselors serving as trainers had been trained in a 6-month course and had been practicing for at least 5 years prior to serving as trainers in the program.
Fig. 1.
Conceptual model for RESHAPE anti-stigma intervention.
Fig. 2.
RESHAPE curriculum with mental health service users and aspirational health workers integrated into PRIME prescriber training.
Component 1. Service User Recovery Stories and Social Contact:
The term ‘service user’ refers to persons living with mental illness who engage health services. The first component of RESHAPE was delivery of recovery stories by service users and their caregivers. Service users’ participation in social contact interventions has evidence for stigma reduction (Corrigan et al., 2012; Knaak et al., 2014; Nyblade et al., 2019; Pescosolido and Manago, 2018; Pettigrew et al., 2011; Thornicroft et al., 2016; Ungar et al., 2016). Recovery stories were approximately 10 min in duration and were followed by 15 min of questions and answers. Service users stayed throughout the day of their presentation so they could interact with healthcare providers during tea breaks, meals, and energizer activities. In the prescriber training, two service user recovery stories were presented on Day 3 to introduce the experience of service users and caregivers to the health workers. Additional service user recovery stories were included for each of the mhGAP modules: depression, psychosis, alcohol use disorder, and epilepsy (Days 6–9). Eight service users took part in the prescriber training and were present for the full day for five of the ten days of training. For non-prescribers, six service users took part and they were present for three full days of the training.
Recovery stories were developed based on the PhotoVoice method with each story accompanied by photographs taken by the service user (Kaiser et al., 2019; Rai et al., 2018). Recovery narratives were structured in three acts: life before treatment, experience of treatment, and life in recovery, see example in Supplemental Textbox S1. Regarding ‘what matters most’, the recovery narratives highlighted that mental illnesses were treatable and that primary care providers play an important role in this treatment, through both medication and psychosocial services. Another topic was that service users and caregivers were interested in understanding and adhering to the treatment. Consistent across service users’ recovery narratives was also their ability to engage in economically productive activities after sustained participation in treatment. Although not explicitly prompted to include this, most service users included photos of farming, raising goats, and small business opportunities. Younger service users described going back to school. Images also depicted family functioning such as caring for children, helping with homework, and playing with grandchildren. One service user included photos of three healthcare providers and said ‘these are my three goddesses’. PhotoVoice recovery narratives were delivered in person by the service users while she/he displayed a series of photographs through a PowerPoint slide presentation.
Component 2. Aspirational figure recovery stories:
Aspirational figures were local primary care providers who had previously been trained on mhGAP. The aspirational figures were selected based on their work during the PRIME program that preceded RESHAPE. They stood out among other primary care providers in terms of the positive attitudes they expressed toward mental health service users, the number of mental health patients they diagnosed, and the quality and fidelity of the care they provided in their clinics. The aspirational figures were selected to serve as role models for the new batches of primary care providers. We chose to include aspirational figures because the presence of an enthusiastic facilitator is an evidence-supported component (Knaak et al., 2014), and social network theory supports the presence of linking personnel who can bridge health workers with service users (Pescosolido and Manago, 2018). These aspirational figures represented someone “just like me” in relation to the primary care trainees.
Aspirational figures were trained on giving presentations about their experiences within a three-act story structure. However, they did not receive PhotoVoice training and did not use their own photographs during their presentations. The first act described how they treated patients with mental illness before undergoing mhGAP training, the second act described what they learned in the mhGAP training, and the third act described how providing mental healthcare has benefited them and their patients. From the ‘what matters most’ perspective, they demonstrated that involvement in mental healthcare did not result in negative survival, social, or professional consequences. On the contrary, they described how it could be beneficial. We included two to four aspirational figures per training.
Component 3. Myth-busting:
In health messaging and health education, myth-busting refers to describing beliefs about an illness that are common in a particular context and culture. Myth-busting includes an explanation for why these beliefs are incorrect by providing factual information. Example mental illness-related myths are “mental illnesses are contagious” or “asking about suicide makes a person want to kill her/himself.” A review of anti-stigma programs found that myth-busting was a component of effective interventions (Knaak et al., 2014). Based on our ‘what matters most’ themes in Nepal, we developed eight statements for myth busting:
Mental illness cannot be treated.
Mental illness can only be treated with shots and pills.
Psychological counseling is no more helpful than just giving generic advice.
If you ask people about suicide, that increases the risk they will kill themselves.
All people with mental illness are violent.
Mental illnesses are contagious.
Only some people can get mental illness; most people can’t become mentally ill.
Caring for people with mental illness makes health workers mentally ill.
The first four statements address professional threats related to if and how mental illness can be treated, as well as risks of triggering suicide. The next two are survival threats. The last two address social threats related to what type of people do or do not become mental ill, with specific attention to the belief that health workers are ‘crazy’ if they treat mental health patients. The aspirational figures connected the myths and facts to their own clinical experiences.
Component 4. Stigma didactics and discussion:
There is an evidence base for understanding what to do and say in relation to stigma (Knaak et al., 2014). Therefore, one of the program staff members (a TPO employee) provided an hour-long didactic and discussion session to define stigma and discrimination, to discuss why language matters including avoiding stigmatizing mental health terms, and to reflect upon how mental illness stigma is just one type of stigma in society. The goal was for all participants to recognize when they also may have been stigmatized, and thus enhance empathy for service users. A common theme raised (without prompting) by the primary care workers was how some groups in health facilities got special treatment (e.g., local teachers, political party affiliates, and relatives of the health facility management committee) whereas other types of people got lower quality of care. The United Nations Convention on Rights of Persons with Disabilities was also introduced to draw attention to global guidance on social inclusion, e.g., the right for all persons to have opportunities for meaningful civic and occupational engagement.
Component 5. Collaborative activity:
Collaborative problem solving is based on social contact theory where two groups work together toward a common goal (Pettigrew et al., 2011). We focused on the common objective that health workers want to be seen as good providers in their community and that service users want good quality care provided. Modelled after a jigsaw classroom (Allport, 1954), health workers, service users, and aspirational figures worked together on the second to last day of training to address potential barriers when delivering mental health care. The groups brainstormed anticipated problems and came up with joint solutions. For example, primary care providers raised concerns about loss to follow-up, non-adherence, and lack of support from patients’ families. Aspirational figures and service users provided suggestions based on their experience; in addition, service users offered to provide support when needed for patients and families who need help understanding recovery and treatment processes.
2.2.3. Recruitment and training of service users and aspirational figures for RESHAPE facilitation
Working with previously-trained primary care and psychosocial workers in the region, we recruited persons living with mental illness who had received treatment and were currently in some state of recovery. After service users were selected, they participated in 5 sessions (7 days total) of PhotoVoice workshops to develop the three-act photographic recovery narrative and prepare for participation in the primary care worker training (Rai et al., 2018), see online Table S2 for additional details on the PhotoVoice training. The selection criteria for the aspirational figures was that they needed to be health workers at the same career level and with the same professional responsibilities as the anti-stigma program beneficiaries.
2.3. Proof-of-concept evaluation of RESHAPE embedded in PRIME trainings
To evaluate embedding RESHAPE into PRIME trainings of primary care providers, we used proof-of-concept testing using qualitative and quantitative methods. This follows the UK Medical Research Council key elements of design and evaluation for new interventions: a development phase, feasibility/piloting phase, evaluation phase, and implementation phase (Fletcher et al., 2016). The current study was conducted from February 2016 through June 2017. We conducted two proof-of-concept trainings incorporating the RESHAPE intervention: one 10-day training with prescribers and one 5-day training with non-prescribers.
2.3.1. Quantitative data and analysis
All healthcare providers completed a battery of measures at pre-training (T0), post-training (T1), and follow-ups of 4 months (T2) and 16 months (T3). Assessment domains included stigma, knowledge, and clinical competence:
Social Distance Scale (SDS): The primary outcome is the SDS, previously used in Nepal (Kohrt et al., 2018b) and based on select sections of the Stigma in Global Context—Mental Health Study (Olafsdottir and Pescosolido, 2011; Pescosolido et al., 2013). The SDS is a widely used measure to assess willingness to interact with persons from a specific stigmatized group (Bogardus, 1925; van Brakel et al., 2019). We used a 12-item SDS with each item scored on a 6-point scale (1–6) for a total range of 12–72; usage in Nepal shows strong internal consistency (α = 0.80).
mhGAP knowledge assessment: True-false and multiple-choice questions were adapted from mhGAP version 1.0 content for PRIME (Hanlon et al., 2018). These questions address psychosis, depression, alcohol use disorder and epilepsy. The prescriber battery includes 26 questions. Non-prescribers completed 19 questions; medication-related questions were removed.
mhGAP attitudes assessment: Based on mhGAP Intervention Guide version 1.0 questions, PRIME also adapted a series of attitudinal questions about mental illness.
ENhancing Assessment of Common Therapeutic factors (ENACT): The ENACT tool is used by raters observing standardized role plays of trainees (Kohrt et al., 2015). The ENACT was developed in Nepal; it includes 18 items plus assessing diagnosis and treatment. Competency on a single item is based on a score of 2 or 3 on a 3-point scale (Kohrt et al., 2018b).
Changes in summary scores of outcome measures were each compared between pre-training (T0) and follow-up for each of the three post-training time-points (T1, T2 and T3) using Wilcoxon signed-rank tests. Descriptive summaries are also provided for single items drawn from these tools that relate to specific domains of what matters most.
2.3.2. Qualitative data and analysis
We qualitatively evaluated the trainings by conducting four focus group discussions: one before and after each training. In addition, we conducted 25 key informant interviews: six primary care workers (four prescribers and two non-prescribers) were interviewed six-months post training; six trainers (three psychiatrists and three psychosocial trainers) were interviewed after the trainings; nine service users and eight of their caregivers were interviewed over multiple months of the project. Materials were coded in NVivo (QSR International, 2012). See Supplemental Table S3 for Consolidated criteria for reporting qualitative research (COREQ) reporting on qualitative methodology (Tong et al., 2007). In the current analysis, we focus on responses from the primary care providers. Qualitative findings from service users and caregivers have been discussed previously (Rai et al., 2018).
2.4. Ethical approval
The study has been granted ethical approval by Duke University (Pro00055042), the Nepal Health Research Council (110/2014 and 133/2016), and George Washington University (051725). All participants completed a signed consent form in Nepali. Before the start of PhotoVoice training, service users were evaluated by psychiatrists to appraise ability to safely participate in the program. The psychiatrist was available if service users had symptom relapse during the weeks of the PhotoVoice trainings. A psychosocial counselor was present to support service users and caregivers for all PhotoVoice sessions and the healthcare provider trainings.
3. Results
3.1. Participants
Forty-one primary care workers (19 non-prescribers and 22 prescribers, Table 1) participated in the PRIME mental health trainings that included the RESHAPE anti-stigma intervention. Non-prescribers were predominantly female (95%), whereas prescribers were predominantly male (81%).
Table 1.
Demographics of primary care staff participating in the mental health training.
| Demographic characteristics | Primary care non-prescribing staff n = 19, (%) | Primary care prescribing staff n = 22, (%) |
|---|---|---|
| Gender | ||
| Female | 18 (95%) | 8 (19%) |
| Male | 1 (5%) | 14 (81%) |
| Age | ||
| 20–29 years | 5 (26%) | 12 (54%) |
| 30–39 years | 8 (42%) | 7 (32%) |
| 40–49 years | 4 (21%) | 3 (14%) |
| 50+ years | 2 (11%) | 0 (0%) |
| Caste/Ethnicity | ||
| Adibasi janajati (indigenous ethnic groups) | 4 (21%) | 0 (0%) |
| Janajati (hill ethnic groups) | 0 (0%) | 1 (4%) |
| Dalit (lower castes) | 0 (0%) | 2 (14%) |
| Brahman (upper castes) | 11 (58%) | 16 (73%) |
| Chhetri (upper castes) | 4 (21%) | 3 (9%) |
| Education | ||
| School Leaving Certificate not completed (not high school graduate) | 4 (21%) | 0 (0%) |
| School Leaving Certificate graduate) completed (high school graduate) | 7 (37%) | 7 (32%) |
| Intermediate degree (2 years of higher education) | 3 (16%) | 6 (27%) |
| Bachelor’s degree (3 years of higher education) | 2 (10%) | 3 (14%) |
| Bachelor of Medicine, Bachelor of Surgery (MBBS, medical doctor; 5 years of higher education) | 0 (0%) | 5 (23%) |
| Master’s degree | 3 (16%) | 1 (4%) |
| Health Professional Qualification (months training) | ||
| Village health worker (3 months) | 1 (5%) | 0 (0%) |
| Auxiliary health worker (10 months) | 0 (0%) | 10 (45%) |
| Community medical assistant (15–18 months) | 1 (5%) | 1 (5%) |
| Auxiliary nurse midwife (18 months) | 12 (63%) | 0 (0%) |
| Health assistant (30–36 months) | 0 (0%) | 6 (27%) |
| Nurse (36 months) | 5 (26%) | 0 (0%) |
| Medical doctor (60 months) | 0 (0%) | 5 (23%) |
| Health Facility | ||
| Health Post | 14 (74%) | 15 (68%) |
| Urban Health Center | 1 (5%) | 0 (0%) |
| Primary Health Center | 0 (0%) | 3 (14%) |
| Primary care services in hospital | 4 (21%) | 3 (14%) |
| Not currently posted | 0 (0%) | 1 (4%) |
| Years working in healthcare | ||
| < 1 year | 0 (0%) | 3 (14%) |
| 1–5 years | 5 (26%) | 11 (50%) |
| 6–10 years | 3 (16%) | 2(9%) |
| > 10 years | 11 (58%) | 6 (27%) |
| Prior MNS training | ||
| No | 19 (100%) | 21 (96%) |
| Yes | 0 (0%) | 1 (4%) |
| Prior experience treating MNS patient | ||
| No | 19 (100%) | 16 (73%) |
| Yes | 0 (0%) | 6 (27%) |
Abbreviations: MNS, mental, neurological and substance use.
3.2. What matters most themes
The qualitative and quantitative findings are presented below grouped by ‘what matters most’ themes.
3.2.1. Survival threats
Healthcare workers attributed changes in beliefs regarding violence to their interactions with service users in the training. For the majority of health workers, their only formal exposure prior to the PRIME training had been touring an inpatient psychiatric ward.
“In the inpatient department, most of the patients were aggressive and the psychiatric ward was completely like a prison as the doors would be all closed, and the rooms would be locked. So, we used to feel scared. When we had to take histories of psychiatric patients, we used to feel scared even after they were stabilized and normal. We used to feel frightened that they would do something to us. But now, after coming here, I have been able to realize that the patients with psychosis are not that violent, and that we can interact with them normally. We can take their history. I have gained this confidence after coming here … [A]fter seeing them here in person, I have gained the confidence that I can provide treatment to people with such problems.” (Prescriber #4).
“We used to call people mad (Nepali: paagal) or psycho. While sitting and talking to those people, we would say that talking to them was of no use because they were not in the right mind. Our society says the same. We did not know that talking to him/her would help solve the problem. We used to be scared and run away, especially if it was a man. We were scared they might throw stones, shout at us after drinking so much, tease us, speak whatever they want, make noise and such … When we’re alone, we would be scared that they might do us harm.” (Non-prescriber #27)
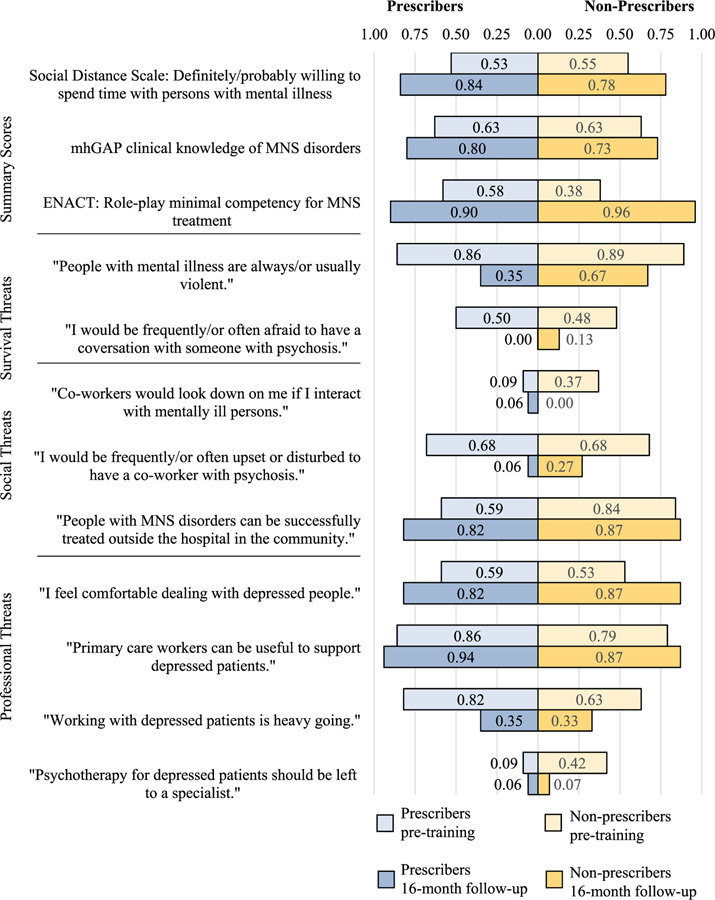
The willingness to interact with persons with mental illness was supported by the quantitative measures. We evaluated within-group change for prescribers and non-prescribers, which demonstrated significant change on the majority of outcome measures (see Table 2). On the SDS at baseline (pre-training), 54% of combined sample (prescribers and non-prescribers) stated that they were definitely willing or probably willing to interact with persons with mental illness on all items of the scale. At 16 months follow-up, 81% were at least probably willing to interact with persons with mental illness (Prescribers: T0 median (interquartile range, IQR) = 32.5(19.2, 47.0), T3 = 15.0(12.0, 21.0), z = −3.1, p = 0.002; Non-prescribers: T0 = 28.8(21.6, 40.8); T3 = 17.0(13.0, 29.0), z = −2.3, p = 0.02). Similarly, there was improvement in a number of single-item scores related to survival threats (see Fig. 3).
Table 2.
Attitudes, knowledge, and clinical competency of prescribers and non-prescribers in PRIME training with RESHAPE anti-stigma component.
| Pre-Training (T0) |
Post-Training (T1) |
4-month Follow-up (T2) |
16-month Follow-up (T3) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Median | IQR | n | Median | IQR | z-scorea (p-value) | n | Median | IQR | z-scorea (p-value) | n | Median | IQR | z-scorea (p-value) | |
| Prescribers | |||||||||||||||
| Primary outcome | |||||||||||||||
| Social Distance (SDS) | 22 | 32.5 | 19.2, 47.0 | 22 | 21.0 | 13.2, 36.0 | −3.2 (0.002) | 20 | 18.0 | 13.0, 37.0 | −2.5 (0.01) | 17 | 15.0 | 12.0, 21.0 | −3.1 (0.002) |
| Secondary outcomes | |||||||||||||||
| mhGAP Knowledge | 22 | 60.0 | 60.0, 70.0 | 22 | 83.3 | 76.7, 83.3 | 4.1 (< 0.001) | 20 | 80.0 | 76.7, 83.3 | 3.9 (<0.001) | 17 | 83.3 | 73.3, 86.7 | 3.6 (< 0.001) |
| mhGAP Attitudes | 22 | 1.7 | 1.6, 1.8 | 22 | 1.5 | 1.4, 1.6 | −3.0 (0.003) | 20 | 1.4 | 1.3, 1.6 | −3.1 (0.002) | 17 | 1.4 | 1.3, 1.5 | −3.3 (0.001) |
| Role-Play Observed Competence (ENACT)b | 22 | 30.0 | 26.0, 32.0 | n/a | 20 | 39.5 | 34.5, 44.0 | 3.8 (< 0.001) | 17 | 47.0 | 35.0, 50.0 | 3.5 (< 0.001) | |||
|
| |||||||||||||||
| Non-prescribers | |||||||||||||||
| Primary outcome | |||||||||||||||
| Social Distance (SDS) | 19 | 28.8 | 21.6, 40.8 | 19 | 21.0 | 14.0, 29.0 | −3.6 (< 0.001) | 18 | 22.0 | 16.0, 32.0 | −2.7 (0.007) | 15 | 17.0 | 13.0, 29.0 | −2.3 (0.02) |
| Secondary outcomes | |||||||||||||||
| mhGAP Knowledge | 19 | 64.0 | 52.0, 72.0 | 19 | 76.0 | 64.0, 80.0 | 3.6 (< 0.001) | 18 | 74.0 | 68.0, 80.0 | 3.1 (0.002) | 15 | 72.0 | 68.0, 76.0 | 2.7 (0.007) |
| mhGAP Attitudes | 19 | 32.0 | 27.6, 35.0 | 19 | 37.0 | 33.0, 38.0 | −3.6 (< 0.001) | 18 | 34.0 | 31.0, 37.0 | −3.6 (< 0.001) | 15 | 37.0 | 33.0, 39.0 | −3.4 (< 0.001) |
| Role-Play Observed Competence (ENACT)b | 19 | 26.0 | 26.0, 27.0 | n/a | 18 | 36.5 | 34.0, 41.0 | 3.7 (< 0.001) | 15 | 45.0 | 38.0, 49.0 | 3.4 (< 0.001) | |||
Abbreviations: PRIME, PRogramme for Improving Mental health carE; RESHAPE, REducing Stigma among HealthcAre ProvidErs; IQR, interquartile range; SDS, Social Distance Scale; mhGAP, mental health Gap Action Programme; ENACT, ENhancing Assessment of Common Therapeutic factors.
Wilcoxon signed-rank test (z-score) for comparison with pre-training (T0) baseline.
Role-play observed competence (ENACT) was not assessed at immediate post-training (T1).
Fig. 3.
Changes in endorsements related to survival, social, and professional threats among prescribers and non-prescribers in RESHAPE.
3.2.2. Social threats
In qualitative interviews conducted immediately after the training, participants remained concerned about social threats. They raised the issue that co-workers at the primary care facility who had not attended the training may be likely to stigmatize those who started providing mental health services.
“But if I do work in a specific mental health center, then I could very well be a subject of humiliation. I personally have heard and listened to people cursing another person like me who works in a mental health center.” (Prescriber #26)
There were comments about wishing that community health volunteers and other health facility staff also had attended similar trainings:
“You have provided us training, but it would have been good if training could be provided to other health workers too … We might tell our co-workers about the situation of the patient, but they might not care about it because they haven’t received training.” (Non-prescriber #4)
In the survey measures, 37% of non-prescribers reported that colleagues would “look down on me if they knew I interacted with persons with MNS disorders.” However, 16-months after the training, 0% of non-prescribers endorsed this statement (see Fig. 3).
One strategy reported to prevent discrimination from colleagues was to share learnings about mental health and help colleagues with family members experiencing MNS disorders:
“There are also cases of epilepsy. One sister who assists us in our health post, her daughter has such a problem. Her husband is alcoholic. She hasn’t been able to provide treatment to her daughter. So, I was thinking that after receiving training, I would be able to provide treatment to her, and I was very happy about it.” (Non-prescriber #3)
3.2.3. Professional threats
There were numerous responses from participants about changes in their beliefs regarding the benefit of providing mental healthcare.
“When such people would come to the clinic, I did not think that they could be cured using medicines. I questioned if they were mad people. But, after the training I came to know that it is possible for them to receive help whatever the reason behind their illness and go back to living normally in the society.” (Prescriber #15)
“I think we became more optimistic. Before we used to have psychiatry posting while doing MBBS. I used to doubt if the patients will really get well, if their condition would improve. So, when seeing those people who have recovered, we got the proof that their condition can improve if they get timely treatment and timely counseling … We got to know how the patients feel and what drives them to do certain things, what triggers depression. We got to interact with patients who previously had postpartum depression and postpartum psychosis … I felt really bad to know about the challenges they face in society. I could empathize with them and realize how they might have felt. So, I felt happy to be able to provide service to people with such problems.” (Prescriber #1)
“The training yesterday was very nice because we got to see the real patients. When we used to see such awareness programs on television, we used to think that it’s fake, we used to think that they were taught to say those things. But while seeing the patients in the training, I felt very happy to know that there can be such improvement …” (Non-prescriber #4)
“The real patients came and shared about the improvement in their condition, one sister shared that she had to drop out of her school, [but after treatment] later she joined again and it was good after that. So, I felt really happy to see the real patients. I could gain this understanding that there can be improvement in their condition.” (Non-prescriber #4).
They also recognized their role in suicide prevention
“While I was working in a government health post, I wasn’t able to do exact diagnosis and that patient committed suicide. That patient had depression, but I was not able to take a concrete history because I didn’t have knowledge about the skill that’s required. That patient came to me a couple of times and she wanted to share about her issues, but I wasn’t able to create that kind of environment. So later, she committed suicide. I wasn’t able to connect all of these points. When I came here, I realized that if I were able to do the correct diagnosis, then I could have saved that person.” (Prescriber #6)
“Regarding suicide, I used to think that we shouldn’t ask about such things but it has been repeatedly emphasized here that we have to ask about it. So, [after the training], we asked patients about it and then the patients told us about suicidal feelings. Some said that they were about to jump in a well, some were about to hang themselves. From this, I realized that some patients may want us to explore on those issues as well.” (Prescriber #4)
3.3. Behavioral outcome: clinical competence
For the ENACT role play measure of clinical competence, 49% of the participants had minimal competence at baseline. At 16-months, 93% of the sample had minimal competence (Prescribers: T0 median (IQR) = 30.0(26.0, 32.0), T3 = 47.0(35.0, 50.0), z = 3.5, p < 0.001; Non-prescribers: T0 = 26.0(26.0, 27.0); T3 = 45.0(38.0, 49.0), z = 3.4, p < 0.001). Many of the skills improved to minimal competency (level 2 or 3) by four months post-training. Other competencies continued to improve from four to six months, such as “involvement of family”, “rapport building,” “harm to self and others,” and “explaining con-fidentiality,” (see Supplemental Figure S1).
4. Discussion
4.1. Role of what matters most in stigma reduction
This proof of concept study explores how a ‘what matters most’ framework can inform anti-stigma initiatives for healthcare providers. ‘What matter most’ takes the perspective that anti-stigma interventions should begin with local values and moral experience. Our qualitative findings suggest that addressing threats within the local world facilitated attitudinal changes and improved clinical behavior. Healthcare workers described their prior assumptions about violence among persons with mental illness, and how the interaction with service users changed this assumption. Similarly, the health workers described their prior beliefs that mental illness could not be treated—especially in primary care, but after the training they felt confident to provide services. The growing emphasis in social psychology on affective mediators in social contact (Pescosolido et al., 2008; Pettigrew et al., 2011) further supports a ‘what matters most’ framing, which predicts that addressing moral experience will be tied to affective engagement.
However, we did not observe changes in all domains. Social threats remained a concern. Participants worried about reactions from other healthcare providers. They emphasized that other providers should receive this training, which suggests that in order for social threats to be reduced, all healthcare providers could need sensitization. This highlights the need to transform local worlds of moral experience, rather than only changing individual member’s attitudes and behaviors. This is consistent with the recommendation that all personnel in health delivery systems should participate in stigma reduction programs (Nyblade et al., 2019).
This study also offers an opportunity to consider how ‘what matters most’ contributes to differences in anti-stigma intervention design compared to what is typically prescribed from a social psychology perspective. Social psychology theories focus on intergroup contact. However, these frameworks are relatively agnostic to content. ‘What matters most’ calls for specific attention to the content of the messaging in relation to moral experience of healthcare providers. The social contact promotes components of moral experience (professional and social identities) within the local world of healthcare providers. For example, the messaging from service users and aspirational figures emphasized the clinical efficacy of healthcare providers for mental health services. This raises the question of whether other perspectives (e.g., a human rights perspective) may have limited impact if that is not core to the professional identity of the target group. Social contact interventions, although more effective than other strategies, still have inconsistent outcomes across some trials, and this may be because of the contact has not targeted ‘what matters most’ for healthcare providers.
In addition, our work supports conclusions (Pettigrew et al., 2011) that not all of Allport’s original intergroup contact criteria are required (Allport, 1954). Specifically, service users and healthcare providers did not share equal status. Some aspects of the PhotoVoice process (e.g., service users presenting their photographs in PowerPoint presentations and working alongside the mhGAP trainers) may have worked to reduce power gaps, but because of the highly hierarchical society in Nepal and the authority of healthcare providers, we cannot assume that we established a level playing field.
One of Allport’s other preconditions was that participation in intergroup contact cannot be forced. However, in the case of government-supported trainings, health workers cannot opt out. This raises the question of whether the ‘what matters most’ framework could have benefited from attending more to autonomy as an important aspect of local worlds of healthcare providers. Governments forcing mental health trainings reduces autonomy. Future stigma reduction could acknowledge the role of autonomy even within these required trainings. For example, aspirational figures’ testimonials could emphasize that when healthcare providers leave the training it is their hands deciding whether or not to put mental health services into practice.
One of the surprising findings was that reductions in social distance were maintained after the training, and there appeared to be continued reduction in social distance through the 16-month follow-up. One of the limitations of anti-stigma research among health workers has been that measurement of positive attitudinal changes appear to be short-term (Henderson et al., 2014). The continued reduction in social distance in our study may be because anti-stigma efforts were embedded in a program introducing new clinical skills, which creates a positive feedback loop. In this positively reinforcing cycle, lower social distance leads to more provision of quality mental health care that leads to more experience with positive outcomes and building of clinical self-efficacy, which could further decrease social distance and encourage more provision of quality care. The possibility of a positively-reinforcing cycle of clinical skills and positive attitudes is supported by continued improvement in clinical competency at each of the follow-up time points as measured by the ENACT.
One consideration for ‘what matters most’ is whether any of the identity threats contradict one another. For example, does helping people who are suicidal go against religious norms? The relationship of religion and suicide is complex in Nepal. Although suicide has negative implications for reincarnation in both Hinduism and Buddhism, there are examples of suicide, especially for women, in traditional practice and religious text (Bennett, 1983). However, our qualitative findings did not suggest that preventing suicide conflicted with ‘what matters most’ regarding religious identity. In contrast, healthcare providers reported that they wished they had mental health training earlier to intervene for their patients who died by suicide.
Our findings are relevant for structural stigma. In the US, structural stigma has been identified as increasing costs and other barriers to accessing care (Yang et al., 2014a). In our study, the collaborative activity demonstrated that service users and healthcare providers were interested in joining forces to address structural barriers such as lack of medication provided by the government, lack of physical space for confidential treatment, and lack of psychosocial counselors in the government workforce. This alliance of service users and healthcare providers could be a key step to change policy, funding, and clinical practice. Service users could also build upon the relationship formed through the experience to create local advocacy organizations and potential sustainable approaches to train others in PhotoVoice. Moreover, continued engagement of service users with health workers has the potential to further strengthen the positive feedback cycle of stigma reduction contributing to improved clinical self-efficacy and quality of care. Ultimately, elevating the status and visibility of actors from a discriminated group changes cultural constructions and contributes to de-stigmatization and improved health (Clair et al., 2016).
Going forward, comprehensively addressing interpersonal, self, and structural stigma requires multi-level approaches (Rao et al., 2019) because stigma in one domain is associated with other domains (Moses, 2010). Only addressing stigma in one domain may lead to that stigma resurfacing out of the other domains. These lessons learned from RESHAPE are also relevant to high-income countries. In high-resource settings, there is still relative ‘low resource’ status of mental health services when compared to higher resources afforded to physical health care. Given the ‘what-matters-most’ framework, there is potential for anti-stigma efforts to improve both personal and structural stigma in these settings as long as the local professional, social, and survival threats underlying stigma are clearly identified and addressed.
4.2. Limitations
Based on the current results, we are unable to make claims about improving outcomes in comparison to standard mhGAP or PRIME trainings, nor are we able to distinguish the relative importance of different components (service users vs. aspirational figures). A controlled trial comparing with standardized training against the training plus RESHAPE has been completed and results will be described in a subsequent publication (Kohrt et al., 2018a).
We also need to evaluate the cost effectiveness to consider sustainability of the program given the training needed by service users and the costs for in-person participation of service users to facilitate social contact.
One potential limitation is the lost-to-follow-up rates. Five prescribers (23% of the original sample) and 4 non-prescribers (21%) were not included in the 16-month follow-up assessment. All participants lost to follow-up were because of either retiring from the government health system or because of re-assignment to a different district. As retirement and re-assignment are not performance-based outcomes, we do not anticipate that these lost-to-follow-up participants biased the 16-month follow-up outcome.
5. Conclusion
Drawing upon medical anthropology and social psychology, we found that facilitated engagement of primary care providers with mental health service users and aspirational figures has the potential to address survival and professional threats, and possibly social threats. According to the UK Medical Research Council, the next step is to evaluate the feasibility and acceptability of the intervention through a pilot trial (Fletcher et al., 2016). The ‘what matters most’ model holds promise to guide what elements are needed and may be applicable to diverse stakeholder groups including health workers, law enforcement, teachers, and social service workers for stigma reduction.
Supplementary Material
Acknowledgements
This document is an output from the PRIME Research Programme Consortium, funded by the UK Department of International Development (DFID) for the benefit of developing countries. RESHAPE is supported by the National Institute of Mental Health (K01MH104310, Principal Investigator: B. Kohrt). The trial sponsors had no role in the study design; study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication. We thank James Griffith, Janice Cooper, and Bernice Pescosolido for initial conceptual contributions. We thank Anup Adhikari, Dristy Gurung, Ashley Hagaman, Bonnie Kaiser, Megan Ramaiya, and Cori Tergesen for their contributions to the RESHAPE project. We acknowledge the Nepal Health Research Council.
Footnotes
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2020.112852.
References
- Allport FH, 1954. The structuring of events: outline of a general theory with applications to psychology. Psychol. Rev 61, 281. [DOI] [PubMed] [Google Scholar]
- Angdembe M, Kohrt BA, Jordans M, Rimal D, Luitel NP, 2017. Situational analysis to inform development of primary care and community-based mental health services for severe mental disorders in Nepal. Int. J. Ment. Health Syst 11, 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer HA, Singer M, Susser I, 2003. Medical Anthropology and the World System. Praeger, Westport, Connecticut. [Google Scholar]
- Bennett L, 1983. Dangerous Wives and Sacred Sisters: Social and Symbolic Roles of High-Caste Women in Nepal. Columbia University Press, New York. [Google Scholar]
- Bogardus ES, 1925. Measuring social distance. J. Appl. Sociol 9, 299–308. [Google Scholar]
- Clair M, Daniel C, Lamont M, 2016. Destigmatization and health: cultural constructions and the long-term reduction of stigma. Soc. Sci. Med 165, 223–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rusch N, 2012. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr. Serv 63, 963–973. [DOI] [PubMed] [Google Scholar]
- de Waal FB, Preston SD, 2017. Mammalian empathy: behavioural manifestations and neural basis. Nat. Rev. Neurosci 18, 498. [DOI] [PubMed] [Google Scholar]
- Fekadu A, Medhin G, Selamu M, Giorgis TW, Lund C, Alem A, et al. , 2017. Recognition of depression by primary care clinicians in rural Ethiopia. BMC Fam. Pract 18, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher A, Jamal F, Moore G, Evans RE, Murphy S, Bonell C, 2016. Realist complex intervention science: applying realist principles across all phases of the Medical Research Council framework for developing and evaluating complex interventions. Evaluation 22, 286–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gartoulla P, Pantha S, Pandey R, 2015. Knowledge status on mental health among health professionals of chitwan district, Nepal. J. Inst. Med 37. [Google Scholar]
- Griffith JL, Kohrt BA, 2016. Managing stigma effectively: what social psychology and social neuroscience can teach us. Acad. Psychiatr 40, 339–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurung D, Upadhyaya N, Magar J, Giri NP, Hanlon C, Jordans MJD, 2017. Service user and care giver involvement in mental health system strengthening in Nepal: a qualitative study on barriers and facilitating factors. Int. J. Ment. Health Syst 11, 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagaman AK, Maharjan U, Kohrt BA, 2016. Suicide surveillance and health systems in Nepal: a qualitative and social network analysis. Int. J. Ment. Health Syst 10, 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagaman AK, Khadka S, Wutich A, Lohani S, Kohrt BA, 2018. Suicide in Nepal: qualitative findings from a modified case-series psychological autopsy investigation of suicide deaths. Cult. Med. Psychiatry 42, 704–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon C, Semrau M, Alem A, Abayneh S, Abdulmalik J, Docrat S, et al. , 2018. Evaluating capacity-building for mental health system strengthening in low-and middle-income countries for service users and caregivers, service planners and researchers. Epidemiol. Psychiatr. Sci 27, 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale-Grant O, et al. , 2014. Mental health-related stigma in health care and mental health-care settings. The Lancet Psychiatr 1, 467–482. [DOI] [PubMed] [Google Scholar]
- Jenkins R, Othieno C, Okeyo S, Aruwa J, Kingora J, Jenkins B, 2013. Health system challenges to integration of mental health delivery in primary care in Kenya-perspectives of primary care health workers. BMC Health Serv. Res 13, 368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans M, Luitel N, Tomlinson M, Komproe I, 2013. Setting priorities for mental health care in Nepal: a formative study. BMC Psychiatr 13, 332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJ, Luitel NP, Pokhrel P, Patel V, 2016. Development and pilot testing of a mental healthcare plan in Nepal. Br. J. Psychiatry 208 (Suppl. 56), s21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser BN, Varma S, Carpenter-Song E, Sareff R, Rai S, Kohrt BA, 2019. Eliciting recovery narratives in global mental health: benefits and potential harms in service user participation. Psychiatr. Rehabil. J 10.1037/prj0000384. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane JC, Elafros MA, Murray SM, Mitchell EMH, Augustinavicius JL, Causevic S, et al. , 2019. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med 17, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauye F, Jenkins R, Rahman A, 2014. Training primary health care workers in mental health and its impact on diagnoses of common mental disorders in primary care of a developing country, Malawi: a cluster-randomized controlled trial. Psychol. Med 44, 657–666. [DOI] [PubMed] [Google Scholar]
- Keusch GT, Wilentz J, Kleinman A, 2006. Stigma and global health: developing a research agenda. Lancet 367, 525–527. [DOI] [PubMed] [Google Scholar]
- Kisa R, Baingana F, Kajungu R, Mangen PO, Angdembe M, Gwaikolo W, et al. , 2016. Pathways and access to mental health care services by persons living with severe mental disorders and epilepsy in Uganda, Liberia and Nepal: a qualitative study. BMC Psychiatr 16, 305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A, 1999. Experience and its moral modes: culture, human conditions, and disorder. Tanner Lect. Hum. Values 20, 355–420. [Google Scholar]
- Kleinman A, 2006. What Really Matters: Living a Moral Life amid Uncertainty and Danger. Oxford University Press, New York. [Google Scholar]
- Kleinman A, Hall-Clifford R, 2009. Stigma: a social, cultural and moral process. J. Epidemiol. Community 63, 418–419. [DOI] [PubMed] [Google Scholar]
- Knaak S, Modgill G, Patten SB, 2014. Key ingredients of anti-stigma programs for health care providers: a data synthesis of evaluative studies. Canadian journal of psychiatry. Rev. Canad. Psychiatr 59, S19–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Harper I, 2008. Navigating diagnoses: understanding mind-body relations, mental health, and stigma in Nepal. Cult. Med. Psychiatry 32, 462–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJD, Rai S, Shrestha P, Luitel NP, Ramaiya M, et al. , 2015. Therapist competence in global mental health: development of the enhancing assessment of common therapeutic factors (ENACT) rating scale. Behav. Res. Ther 69, 11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJD, Turner EL, Sikkema KJ, Luitel NP, Rai S, et al. , 2018a. Reducing stigma among healthcare providers to improve mental health services (RESHAPE): protocol for a pilot cluster randomized controlled trial of a stigma reduction intervention for training primary healthcare workers in Nepal. Pilot and Feasibility Stud 4, 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Mutamba BB, Luitel NP, Gwaikolo W, Onyango Mangen P, Nakku J, et al. , 2018b. How competent are non-specialists trained to integrate mental health services in primary care? Global health perspectives from Uganda, Liberia, and Nepal. Int. Rev. Psychiatr 30, 182–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konner M, 1988. Becoming a Doctor: A Journey of Initiation in Medical School. Penguin Books. [Google Scholar]
- Kroenke K, Unutzer J, 2017. Closing the false divide: sustainable approaches to integrating mental health services into primary care. J. Gen. Intern. Med 32, 404–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhrmann TM, 2000. Of Two Minds : the Growing Disorder in American Psychiatry. Knopf; distributed by Random House, New York. [Google Scholar]
- Luitel N, Jordans M, Adhikari A, Upadhaya N, Hanlon C, Lund C, et al. , 2015. Mental health care in Nepal: current situation and challenges for development of a district mental health care plan. Conflict Health 9, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Tomlinson M, De Silva M, Fekadu A, Shidhaye R, Jordans M, et al. , 2012. PRIME: a programme to reduce the treatment gap for mental disorders in five low-and middle-income countries. PLoS Med./Publ. Libr. Sci 9, e1001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses T, 2010. Being treated differently: stigma experiences with family, peers, and school staff among adolescents with mental health disorders. Soc. Sci. Med 70, 985–993. [DOI] [PubMed] [Google Scholar]
- Muga FA, Jenkins R, 2008. Training, attitudes and practice of district health workers in Kenya. Soc. Psychiatr. Psychiatr. Epidemiol 43, 477–482. [DOI] [PubMed] [Google Scholar]
- Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. , 2019. Stigma in health facilities: why it matters and how we can change it. BMC Med 17, 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olafsdottir S, Pescosolido BA, 2011. Constructing illness: how the public in eight Western nations respond to a clinical description of “schizophrenia. Soc. Sci. Med 73, 929–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA, Martin JK, Lang A, Olafsdottir S, 2008. Rethinking theoretical approaches to stigma: a framework integrating normative influences on stigma (FINIS). Soc. Sci. Med 67, 431–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA, Medina TR, Martin JK, Long JS, 2013. The “backbone” of stigma: identifying the global core of public prejudice associated with mental illness. Am. J. Publ. Health 103, 853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA, Martin J, 2015. The stigma complex. Annu. Rev. Sociol 41, 87–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA, Manago B, 2018. Getting underneath the power of “contact”: revisiting the fundamental lever of stigma as a social network phenomenon. In: Major B, Dovido JF, Link BG (Eds.), The Oxford Handbook of Stigma, Discrimination, and Health. Oxford University Press, pp. 397. [Google Scholar]
- Pettigrew TF, Tropp LR, Wagner U, Christ O, 2011. Recent advances in intergroup contact theory. Int. J. Intercult. Relat 35, 271–280. [Google Scholar]
- International QSR, 2012. NVIVO Qualitative Data Analysis Software. QSR International Pty Ltd, Doncaster, Australia. [Google Scholar]
- Rai S, Gurung D, Kaiser BN, Sikkema KJ, Dhakal M, Bhardwaj A, et al. , 2018. A service user co-facilitated intervention to reduce mental illness stigma among primary healthcare workers: utilizing perspectives of family members and caregivers. Fam. Syst. Health 36, 198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, Go VF, 2019. A systematic review of multi-level stigma interventions: state of the science and future directions. BMC Med 17, 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes LA, 1991. Emptying Beds : the Work of an Emergency Psychiatric Unit. University of California Press, Berkeley. [Google Scholar]
- Scheff TJ, 2017. Being Mentally Ill: A Sociological Study. Routledge. [Google Scholar]
- Stangl AL, Earnshaw VA, Logie CH, van Brakel W, Simbayi C, L, Barré I, et al. , 2019. The Health Stigma and Discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med 17, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart H, Arboleda-Florez J, Sartorius N, 2012. Paradigms Lost: Fighting Stigma and the Lessons Learned. Oxford University Press, New York. [Google Scholar]
- Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. , 2016. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet 387, 1123–1132. [DOI] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, Craig J, 2007. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 19, 349–357. [DOI] [PubMed] [Google Scholar]
- Ungar T, Knaak S, Szeto ACH, 2016. Theoretical and practical considerations for combating mental illness stigma in health care. Community Ment. Health J 52, 262–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Brakel WH, Cataldo J, Grover S, Kohrt BA, Nyblade L, Stockton M, et al. , 2019. Out of the silos: identifying cross-cutting features of health-related stigma to advance measurement and intervention. BMC Med 17, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2016. mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-specialized Health Settings: Mental Health Gap Action Programme (mhGAP) – Version 2.0. World Health Organization, Geneva, Switzerland. [PubMed] [Google Scholar]
- Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B, 2007. Culture and stigma: adding moral experience to stigma theory. Soc. Sci. Med 64, 1524–1535. [DOI] [PubMed] [Google Scholar]
- Yang LH, Purdie-Vaughns V, Kotabe H, Link BG, Saw A, Wong G, et al. , 2013. Culture, threat, and mental illness stigma: identifying culture-specific threat among Chinese-American groups. Soc. Sci. Med 88, 56–67 1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang LH, Chen F. p., Sia KJ, Lam J, Lam K, Ngo H, et al. , 2014a. “What matters most:” A cultural mechanism moderating structural vulnerability and moral experience of mental illness stigma. Soc. Sci. Med 103, 84–93. [DOI] [PubMed] [Google Scholar]
- Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG, 2014b. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing ‘what matters most’to identify culture-specific aspects of stigma. Int. J. Epidemiol dyu039. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.