Abstract
After lower extremity injury, only half of the injured athletes return to their pre-injury sports level. Even though functional performance tests are often used to make return to sport decisions, it is unknown whether functional performance is associated with return to performance after such injuries. The aim of this systematic review was to identify, critically appraise, and analyze studies that investigated the association of functional performance tests with return to performance after lower extremity injuries in athletes participating in high-impact sports. MEDLINE, Embase, Web of Science, and CINAHL were systematically searched for relevant studies. Articles were independently screened by two authors and data were obtained from each included study using a data extraction form. Two authors independently scored methodological quality using the Quality In Prognosis Studies tool. A qualitative best evidence synthesis was conducted. Eight studies reported the association of functional performance with return to performance after lower extremity injuries, involving 1,246 athletes after anterior or posterior cruciate ligament reconstruction. No studies were found on the association of functional performance with return to performance for lower extremity injuries other than after anterior or posterior cruciate ligament reconstruction. All included studies had a high risk of bias. Two studies found significant but small associations for selected hop tests after anterior cruciate ligament reconstruction. Low evidence of association between functional performance and return to performance was present after anterior cruciate ligament reconstruction for the triple hop for distance, the 6-meter timed hop, the side hop in female athletes, and for the combination of the single and crossover hop for distance. In athletes after posterior cruciate ligament reconstruction, the vertical jump showed a significant but small association with return to performance. There is no high-quality evidence that functional performance is associated with return to performance after lower extremity injuries in athletes practicing high-impact sports. Low quality evidence suggests small associations after anterior and posterior cruciate ligament reconstruction. No evidence exists for lower extremity injuries other than after anterior or posterior cruciate ligament reconstruction. Therefore, research on functional performance associated with return to performance is recommended in high-quality prospective cohort studies including athletes with any type of lower extremity injury.
Key points.
Low quality evidence suggests that functional performance is associated with return to performance after anterior or posterior cruciate ligament reconstruction in athletes participating in high-impact sports.
No evidence exists on the association between functional performance and return to performance for lower extremity injuries other than after cruciate ligament reconstruction.
Small associations between functional performance and return to performance were found for the triple hop for distance, 6-meter timed hop, vertical jump, side hop in female athletes, and the combination of the single and crossover hop for distance.
High-quality prospective cohort studies on the association between functional performance and return to performance, including athletes with any type of lower extremity injury, are needed.
Key words: Functional performance test, hop test, return to pre-injury sports level, high-impact athletes
Introduction
Lower extremity injuries are an important problem in the athletic population with an incidence rate of 11.6 per 10,000 athlete exposures (Nagle et al., 2017). Approximately 90% of sport injuries concern the ankle, knee, and thigh while sprains, strains, contusions, tendinopathies, and fractures comprise 90% of the diagnoses (Nagle et al., 2017). The majority of these injuries occur among athletes practicing high-impact sports (e.g. soccer, volleyball, basketball, hockey) where frequently performed actions are high-speed running, jumping, turning, cutting, pivoting, or changes of direction (van Beijsterveldt et al., 2015; Schmikli et al., 2009). Median time loss due to lower extremity injury is about 16 days, ranging from two to 407 days (van Beijsterveldt et al., 2015).
After injury, athletes commonly wish to return to their pre-injury sports level, defined as return to performance (RTPf) (Ardern et al., 2016). However, RTPf may not be achievable for every athlete. After surgically treated lower extremity injuries, only 31-68% of athletes reach RTPf while 66-91% returned to their pre-injury sport at a lower than desired performance level, defined as return to sport (Ardern, 2015; Ardern et al., 2011a; 2012b; 2013; 2014; 2016; Aune et al., 2014; Barastegui et al., 2018; Grassi et al., 2015; Kvist et al., 2005; Lentz et al., 2012; Lee et al., 2008; Mithoefer et al., 2009; Niederer et al., 2018; Sandon et al., 2015; Steel and DeOrio, 2007). The main reasons for not reaching RTPf after anterior cruciate ligament reconstruction (ACLR) are fear of re-injury/lack of confidence and self-reported knee-related problems such as pain, swelling, instability, and muscle weakness (Grassi et al., 2015; Lee et al., 2008; Lentz et al., 2012; Tjong et al., 2014). When athletes reach RTPf, sport- and game performance significantly deteriorates after surgery compared to before surgery or compared to matched athletes (Busfield et al., 2009; Jack et al., 2019; Lubbe et al., 2018; Niederer et al., 2018). In addition athletes who RTPf after surgery play significantly fewer years, fewer games per season, and fewer minutes per game with a decreased number of goals and number of completed passes compared with their performance before surgery or compared to the performance of healthy athletes (Busfield et al., 2009; Jack et al., 2019; Lubbe et al., 2018; Niederer et al., 2018).
Low rates of athletes who RTPf and decreased performance after RTPf highlights the importance of accurate return to sport decision-making to enhance RTPf (Niederer et al., 2018). However, the number of factors affecting RTPf illustrates the complexity of return to sport decision-making. Younger age (Ardern et al., 2012b; 2014; Barastegui et al., 2018; Brophy et al., 2012), male gender (Ardern et al., 2014; Brophy et al., 2012; Sandon et al., 2015), position on the field (Aune et al., 2014; Menge et al., 2017), lower fear of reinjury (Kvist et al., 2005; Lentz et al., 2012; te Wierike et al., 2013), greater psychological readiness (Ardern et al., 2014; Ardern, 2015), and a more positive subjective assessment of function (Ardern, 2015; Lentz et al., 2012; Sandon et al., 2015) have been reported as factors increasing the probability of RTPf after ACLR.
In the multidimensional return to sport decision-making framework (Ardern et al., 2016; Creighton et al., 2010; Shrier, 2015), functional performance tests are commonly used (Abrams et al., 2014; Barber et al., 1992; Barber-Westin and Noyes, 2011; Manske and Reiman, 2013; Webster and Hewett, 2019). Lower extremity functional performance tests aim to assess the entire lower extremity for the ability to perform specific components of sport functions such as running, hopping, or cutting (Barber et al., 1992; Creighton et al., 2010; Hegedus et al., 2015a; Manske and Reiman, 2013; Narducci et al., 2011). Although functional performance tests were developed and commonly used to support the return to sport decision-making after anterior cruciate ligament injury or ACLR (Barber et al., 1990; Barber-Westin and Noyes, 2011; Hegedus et al., 2015a; Herbst et al., 2015; Hildebrandt et al., 2015; Narducci et al., 2011; Thomee et al., 2011), in clinical practice functional performance tests are also used to make decisions regarding return to sport after hip (Hegedus et al., 2015b), ankle (Hegedus et al., 2015b; Tassignon et al., 2019), and hamstring injuries (van der Horst et al., 2016).
Since functional performance tests are important in the decision-making for return to sport, it is assumed that functional performance could be associated with RTPf. No systematic review has yet been published on this topic. Therefore, this systematic review aimed to identify, critically appraise, and analyze published evidence on the association of functional performance with RTPf after lower extremity injuries in athletes participating in high-impact sports.
Methods
The review protocol was registered in the International Prospective Register of Systematic Reviews (prospero)(CRD42018107770) and was written in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2009).
Search strategy
MEDLINE, Embase, Web of Science, and CINAHL were systematically searched independently by two authors (AV and JJ) for relevant articles from inception to September 10th, 2019. Synonym lists were created with key words for: association, return to performance, lower extremity injury, and sports. In MEDLINE, we used combinations of MeSH terms and free text words (Box 1). The search strategy was subsequently adapted for Embase, Web of Science, and CINAHL. References in full text articles were screened for additional relevant studies. Results of searches were combined and duplicates were removed.
Box 1. Search strategy for MEDLINE.
epidemiologic factors OR prognosis OR risk OR risk factors OR odds ratio OR determinant OR predict* AND return to sport OR return to performance OR return to training OR return to preinjury OR return to pre-injury OR return to competition OR sport return OR sports return AND injur* OR wounds and injuries OR athletic injuries OR leg injuries OR ankle injuries OR foot injuries OR knee injuries OR hip injuries OR soft tissue injuries OR sprains and strains OR tendon injuries OR tendinopathy OR fractures, bone OR joint dislocations OR rupture OR ankle fractures OR fractures, stress OR tibial fractures OR tibial meniscus injuries AND lower extremity OR knee joint OR knee OR hip joint OR hip OR ankle joint OR ankle OR foot OR heel OR leg OR thigh OR groin OR lower body OR quadriceps OR hamstring AND sports OR athletes OR track and field OR baseball OR basketball OR boxing OR football OR gymnastics OR hockey OR martial arts OR racquet sports OR tennis OR skiing OR snow sports OR soccer OR volleyball OR handball OR korfball OR dancing OR boot camp OR crossfit OR futsal
Study selection
Titles and abstracts were screened and full text articles were read by two authors (AV and JJ) independently complying with the following inclusion criteria: (1) functional performance tests were investigated as factors associated with RTPf, (2) participants included adult athletes (18-45 years) after any lower extremity injury performing high-impact sports involving jumping, pivoting, or changes of direction, and (3) comparisons between athletes who did and did not RTPf were quantified. RTPf was defined as returning at or above the pre-injury sports level (Ardern et al., 2016). High-impact sports considered were baseball, basketball, boxing, football, gymnastics, hockey, martial arts, racquet sports, tennis, skiing, snow sports, soccer, volleyball, handball, korfball, dancing, boot camp, crossfit, or futsal (Box 1). No language restrictions were imposed. Disagreements between the two authors regarding eligibility were resolved by discussion until consensus was reached. When necessary, a third author (EvT) made the final decision.
Data extraction
Data were obtained from each included study using a data extraction form developed specifically for this review. First author’s name, year of publication, number of included athletes, type of injury, definition of RTPf, number (percentage) of athletes who RTPf, functional performance test(s), timing of functional performance test(s), timing of follow-up, and outcomes were independently tabulated by two authors (AV and JJ).
Methodological quality assessment
Two authors (AV and IA) independently scored the methodological quality of each included study using the Quality In Prognosis Studies (QUIPS) tool (Hayden et al., 2006; 2013). The QUIPS consists of six domains: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting. Each domain is scored as high risk of bias, moderate risk of bias, or low risk of bias. With regard to classifying a study’s risk of bias, we considered study selection, study attrition, prognostic factor measurement, and outcome measurement as the decisive domains. A study was classified as having a low risk of bias when each of these four domains were scored as low risk of bias. If one or more domains were scored as high risk of bias, the study was classified as having a high risk of bias. There was moderate risk of bias when there was no item classified as high risk of bias and more than one item was moderate (Hayden et al., 2019; Riley et al., 2019; Wolff et al., 2019).
Agreement between authors was calculated using percentages and Cohen’s Kappa, where 0 indicates no agreement, 0.01-0.20 slight agreement, 0.21-0.40 fair agreement, 0.41-0.60 moderate agreement, 0.61-0.80 substantial agreement, 0.81-1.00 almost perfect agreement (Landis and Koch, 1977). Differences in scores between the two authors were discussed until consensus was reached. If necessary, a third author (EvT) was asked to pass judgment.
Data analysis and synthesis
The outcome of interest was the association between functional performance and RTPf. Functional performance can be represented as scores on functional performance tests for the injured and noninjured limbs or as the Limb Symmetry Index (LSI), where the score of the injured limb was divided by the noninjured limb and multiplied by 100% (Barber et al., 1990; Noyes et al., 1991). An association was considered to be present if the functional performance was significantly different between athletes who RTPf and those who did not RTPf (p < 0.05) or, more preferably, functional performance was associated with RTPf in terms of odds ratio (OR) or relative risk (RR) with their 95% confidence interval (95% CI). We assumed a lower bound of the 95% CI around OR or RR <1.5 as a small effect, 1.5-2.0 as a moderate effect, and >2.0 as a large effect (Hayden et al., 2019). An Area Under the Curve (AUC) ≥ 0.70 indicates good differentiation between athletes RTPf or not RTPf (Terwee et al., 2007).
There was strong evidence of association (or of no association) if there were consistent findings among >75% of studies with a low risk of bias. Moderate evidence of association (or of no association) existed when consistent findings were present among 75% of studies with a moderate risk of bias. If only one study with a low or a moderate risk of bias was available, there was limited evidence of association (or of no association). When there were inconsistent findings across studies, conflicting evidence of association (or of no association) was present. In all other cases, evidence was classified as low evidence of association (adapted from Hayden et al. 2019).
Results
Study selection
The database searches yielded a total of 3,264 articles. After removing 1,207 duplicates, 2,057 articles were screened for title and abstract. Based on the title and the abstract respectively 1,913 and 133 articles were excluded, and eleven articles were included for full text eligibility assessment. Three studies were excluded because no association between functional performance and RTPf was investigated (Sousa et al., 2017; Jang et al., 2014; Webster and Feller, 2018). Eight full text articles were included in this review of which seven studies following ACLR (Ardern et al., 2011b; Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018; Webster et al., 2019) and one study after posterior cruciate ligament reconstruction (PCLR) (Lee et al., 2019) (Figure 1). There were no articles regarding lower extremity injuries other than after ACLR or PCLR. There were no disagreements between the two authors on study eligibility.
Figure 1.
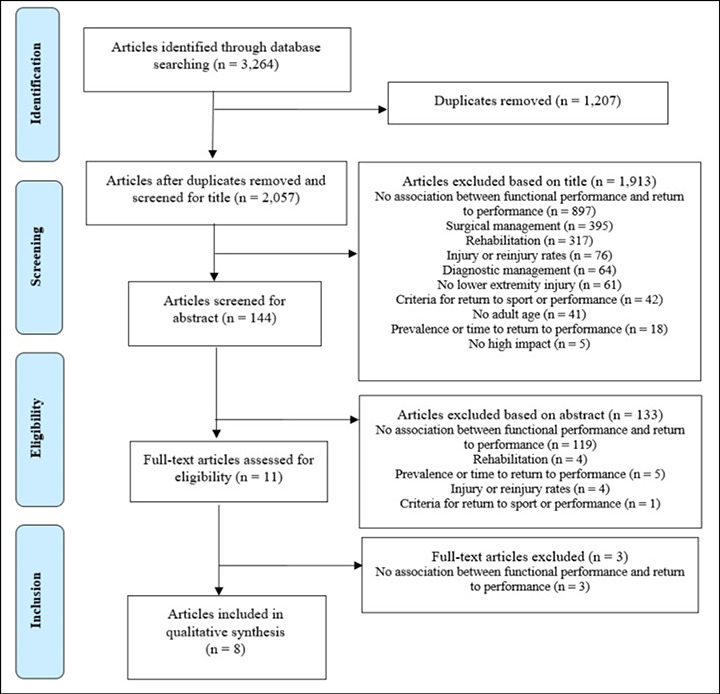
Flow of studies through the review.
Data extraction of included studies
Eight studies were included involving 1,194 athletes after ACLR and 52 athletes after PCLR performing high-impact sports before the injury occurred (Ardern et al., 2011b; Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018; Lee et al., 2019; Webster et al., 2019). RTPf was reported in 578 (46%) of athletes about one year after ACLR or PCLR. Functional performance tests investigated were the single hop for distance (Ardern et al., 2011b; Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018; Webster et al., 2019; Lee et al., 2019), triple hop for distance (Edwards et al., 2018; Muller et al., 2015; Nawasreh et al., 2018), crossover hop for distance (Ardern et al., 2011b; Edwards et al., 2018; Langford et al., 2009; Muller et al., 2015; Webster et al., 2019), vertical jump (Hamrin Senorski et al., 2017; Lee et al., 2019), side hop (Hamrin Senorski et al., 2017), square hop (Muller et al., 2015), and 6 meter timed hop (Edwards et al., 2018; Nawasreh et al., 2018). Performance was measured between 6 and 14 months after ACLR. Follow-up for RTPf was measured at the same time as functional performance testing in four studies (Ardern et al., 2011b; Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Lee et al., 2019), one month after functional performance testing in one study (Muller et al., 2015), 6 and 12 months after functional performance testing in one study (Nawasreh et al., 2018), and two years after functional performance testing in one study (Webster et al., 2019). Data-extraction of included studies is presented in Table 1.
Table 1.
Data-extraction of included studies.
| N Type of injury |
Definition RTPf | Athletes RTPf (%) | Functional performance tests |
Timing functional performance tests | Timing follow-up |
Outcomes | |
|---|---|---|---|---|---|---|---|
| Ardern et al., 2011b | 503 ACLR | Return to full competition |
33.4% attempted full competition (n=168) |
Single hop for distance Crossover hop for distance |
12 months following ACLR |
12 months following ACLR |
Athletes with good results on both hop test were significantly more likely than athletes with poor results to have attempted full competition RR 2.5 (95% CI 1.4-4.4) |
| Edwards et al., 2018 | 113 ACLR | Return to level I or level II on the NSARS |
64% (n=72) | Single hop for Distance Crossover hop for distance Triple hop for distance 6-meter timed hop |
10-14 months following ACLR |
10-14 months following ACLR |
Single hop for distance (LSI %)* RTPf 94.2 ±8.2; No RTPf 77.1 ±17.6 Crossover hop for distance (LSI %)* RTPf 94.0 ±8.2; No RTPf 76.4 ±20.7 Triple hop for distance (LSI %)* RTPf 94.6 ±8.9; No RTPf 77.9 ±19.1 6-meter timed hop (LSI %)* RTPf 94.0 ±8.8; No RTPg 78.4 ±18.6 |
| Hamrin Senorski et al., 2017 | 157 ACLR | Return to pre-injury Tegner |
33% (n=52) | Single hop for distance Vertical jump Side hop |
10 (6-18) months following ACLR |
10 (6-18) months following ACLR |
Men Vertical jump IL (cm/kg)RTPf 0.26 ±0.07; No RTPf 0.27 ±0.07 Vertical jump NL (cm/kg)RTPf 0.29 ±0.05; No RTPf 0.27 ±0.06 Single hop for distance IL (cm/kg)RTPf 2.0 ±0.3; No RTPf 2.0 ±0.3 Single hop for distance NL (cm/kg)RTPf 2.1 ±0.4; No RTPf 2.1 ±0.4 Side hop IL (n/kg)RTPf 0.8 ±0.1; No RTPf 0.7 ±0.2 Side hop NL (n/kg)RTPf 0.8 ±0.1; No RTPf 0.7 ±0.1 Women Vertical jump IL (cm/kg)RTPf 0.23 ±0.04; No RTPf 0.21 ±0.06 Vertical jump NL (cm/kg)RTPf 0.26 ±0.04; No RTPf 0.27 ±0.03 Single hop for distance IL (cm/kg)RTPf 2.1 ±0.4; No RTPf 1.9 ±0.3 Single hop for distance NL (cm/kg)RTPf 2.1 ±0.3; No RTPf 2.0 ±0.3 Side hop IL (n/kg)*RTPf 0.7 ±0.2; No RTPf 0.5 ±0.2 Side hop NL (n/kg)*RTPf 0.8 ±0.2; No RTPf 0.6 ±0.2 |
| Langford et al., 2009 | 65 ACLR | Return to full competition |
52% (n=33) | Single hop for Distance Crossover hop for distance |
12 months following ACLR |
12 months following ACLR |
Single hop for distance (LSI %)RTPf 90.95±8.21; No RTPf 88.87 ±9.77 Crossover hop for distance (LSI %)RTPf 92.32±.50; No RTPf 91.85±10.40 |
| Lee et al., 2019 | 52 PCLR | Previous sports activity level |
9 months following PCLR: 73% (n=38) 24 months following PCLR: 87% (n=45) |
Single hop for distance Vertical jump |
9, 12, and 24 months following PCLR |
29.5 ± 8.6 months following PCLR |
Single hop for distance (LSI%) RTPf 95.8±11.8; No RTPf 88.6±10.5 Vertical jump (LSI%)*RTPf 94.7 ±10.0; No RTPf 87.2 ±9.7* LSI Vertical jump significantly associated with not returning to pre-injury sports activity levels at 9 monthsOR 2.2 (1.212-9.227) |
| Muller et al., 2015 | 39 ACLR | Return to pre-injury level of sport |
79% (n=31) | Single hop for distance Crossover hop for distance Triple hop for distance Square hop |
6 months following ACLR |
7 months following ACLR |
Single hop for distance
(LSI %)* RTPf 85.6 ±20.0; No RTPf 61.7 ±20.5 Crossover hop for distance (LSI %)* RTPf 91.9 ±14.3; No RTPf 75.1 ±18.5 Triple hop for distance (LSI %)* RTPf 88.3 ±10.1; No RTPf 72.1 ±13.1 Square hop (LSI %) RTPf 87.5 ±20.4; No RTPf 83.8 ±44.6 AUC (LSI %) RTPf Single hop for distance 0.823 (75.4) Crossover hop for distance 0.762 (77.2) Triple hop for distance 0.839 (90.2) |
| Nawasreh et al., 2018 | 95 ACLR | Return to pre-injury activity level |
12 months following ACLR: 61% (49/80) 24 months following ACLR: 67% (60/80) |
Single hop for distance Crossover hop for distance Triple hop for distance 6-meter timed hop |
6 months following ACLR |
12 months following ACLR |
Single hop for distance OR (95% CI) 12 months 1.07 (1.01-1.14); 24 months 1.15 (1.05-1.26)* Crossover hop for distance OR (95% CI) 12 months 1.06 (0.99-1.15); 24 months 1.12 (1.03-1.21)* Triple hop for distance OR (95% CI) 12 months 1.11 (1.02-1.20); 24 months 1.17 (1.05-1.31)* 6-meter timed hop OR (95% CI) 12 months 1.13 (1.04-1.22); 24 months 1.18 (1.06-1.31)* |
| Webster et al., 2019 | 222 ACLR | Return to pre-injury sports |
61% (n=135) | Single hop for distance
Crossover hop for distance |
12 and 24 months following ACLR | 3 years (range 2-4 years) |
Average LSI (%) single and crossover hop for distance RTPf 98 ±9; No RTPf 95 ±11 OR 1.03 (95% CI 1.00 – 1.06) |
*Significant difference between return to performance or not (p<0.05), ACLR=Anterior Cruciate Ligament Reconstruction, AUC=Area Under Curve, CI=Confidence Interval, cm=centimeter, IL=Injured Limb, kg=kilogram, LSI=Limb Symmetry Index, NL=Noninjured Limb, NSARS=Noyes Sports Activity Rating Scale, OR=Odds Ratio, ROC=Receiver Operating Curve, RR=Risk Ratio, RTPf=Return to performance.
Methodological quality
All included studies had an overall high risk of bias (Ardern et al., 2011b; Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018; Lee et al., 2019; Webster et al., 2019). High risk of bias regarding prognostic factor measurement (Ardern et al., 2011b; Edwards et al., 2018; Hamrin Senorski et al., 2017; Muller et al., 2015; Nawasreh et al., 2018; Lee et al., 2019; Webster et al., 2019) and study participation was found in seven studies (Ardern et al., 2011b; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018; Webster et al., 2019; Lee et al., 2019). In all studies (Ardern et al., 2011b; Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018; Lee et al., 2019; Webster et al., 2019) outcome measurement was classified as high risk of bias. The methodological quality of included studies is presented in Table 2. Raw agreement between the two authors was 67%. In 31% of the cases consensus was reached while the third author made the final decision on disagreements in one item. Kappa was 0.41, indicating moderate agreement. Agreement of the judgement of the overall risk of bias was 100%.
Table 2.
Methodological quality of included studies.
| Ardern et al. (2011b) |
Edwards et al. (2018) |
Hamrin Senorski et al. (2017) |
Langford et al. (2009) |
Lee et al. (2019) |
Müller et al. (2015) |
Nawasreh et al. (2018) |
Webster et al. (2019) |
|
|---|---|---|---|---|---|---|---|---|
| Study participation | High | High | High | Moderate | High | High | High | High |
| Study attrition | Low | Low | High | High | High | Low | High | High |
| Prognostic factor measurement | High | Moderate | High | High | High | High | High | High |
| Outcome measurement | High | High | High | High | High | High | High | High |
| Study confounding | High | Moderate | High | Moderate | High | Low | Moderate | Moderate |
| Statistical analysis and reporting | Low | High | High | Moderate | High | Moderate | Low | Moderate |
Data analysis and synthesis
Ardern et al. (2011b) found that athletes after ACLR with good hop test results (≥85% on the LSI) were 2.5 times more likely to RTPf than athletes with poor results (<85% on the LSI) [RR 2.5 (95% CI 1.4-4.4)]. With a lower bound of the 95% CI around 1.5 indicating a small association, there is low evidence of association between the combination of the single and crossover hop for distance and RTPf. Webster et al. (2019) also found a small association and low evidence of association for the combination of the single and crossover hop for distance. A greater LSI at 12 months was significantly associated with RTPf three years after ACLR [OR 1.03 (95% CI 1.00-1.06)].
Nawasreh et al. (2018) investigated the outcomes of functional performance tests six months after ACLR and found that the single hop for distance, triple hop for distance, and 6 meter timed hop were associated with RTPf one and two years after ACLR. The crossover hop for distance was only associated with RTPf two years after ACLR. The OR’s and upper bounds of the 95% CI indicate small effect sizes and low evidence of associations.
Muller et al. (2015) found significantly higher LSI’s, good discriminative accuracy, but low evidence of association for the single hop for distance, crossover hop for distance, and triple hop for distance in athletes who RTPf after ACLR compared to athletes who did not RTPf. The LSI for the square hop was higher in athletes who RTPf compared to athletes who did not RTPf, but not significantly different. Edwards et al. (2018) also found that after ACLR athletes who RTPf had significantly higher LSI’s on the single hop for distance, crossover hop for distance, triple hop for distance, and 6-meter timed hop compared to athletes who did not RTPf with low evidence of association between functional performance and RTPf. Contrary to Muller et al. (2015) and Edwards et al. (2018), Langford et al. (2009) found no evidence of association for the single hop for distance and crossover hop for distance after ACLR. Athletes who RTPf had higher LSI’s for the single hop for distance and crossover hop for distance compared to athletes who did not RTPf, but the differences were not significant.
Hamrin Senorski et al. (2017) corrected the outcomes of functional performance tests in centimeters or numbers for body weight and found that female and male athletes who RTPf did not perform significantly differently on the single hop for distance and vertical jump compared to athletes who did not RTPf. There is low evidence of association for the side hop and RTPf in female athletes, as the side hop was significantly higher in athletes who RTPf compared to female athletes who did not RTPf. This difference was not significant in male athletes.
The only study investigating athletes after PCLR (Lee et al., 2019) found that athletes who RTPf scored higher LSI’s on the single hop for distance and vertical jump compared to athletes who did not RTPf. The difference on the vertical jump was significant and the LSI was significantly associated with not RTPf [OR 2.2 (95% CI 1.21-9.23)]. Despite a large effect size, the lower bound of the 95% CI close to 1.0 indicates a small association and there is low evidence of association between the vertical jump and RTPf in athletes after PCLR.
In summary, for athletes following ACLR low evidence of association from high risk of bias studies is present for the association between functional performance and RTPf for the triple hop for distance (Edwards et al., 2018; Muller et al., 2015; Nawasreh et al., 2018), the 6-meter timed hop (Edwards et al., 2018; Nawasreh et al., 2018), the side hop in female athletes (Hamrin Senorski et al., 2017), and the combination of the single and crossover hop for distance (Ardern et al., 2011b; Webster et al., 2019). Conflicting evidence of association exists for the single hop for distance (Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018) and the crossover hop for distance (Edwards et al., 2018; Langford et al., 2009; Nawasreh et al., 2018; Muller et al., 2015). No evidence of association exists for the vertical jump (Hamrin Senorski et al., 2017), the side hop in male athletes (Hamrin Senorski et al.,2017), and the square hop (Muller et al., 2015). For athletes after PCLR, low evidence of association is present for the vertical jump (Lee et al., 2019).
Discussion
The aim of this review was to analyze published evidence on the association of functional performance with RTPf after lower extremity injury in high-impact sports. Eight studies with a high risk of bias reported small associations of functional performance with return to performance after ACLR or PCLR. Although an extensive search was performed, there was no information available on the association of functional performance with RTPf after lower extremity injuries other than after ACLR or PCLR.
Association between functional performance and RTPf after lower extremity injuries
All studies included only athletes who underwent ACLR or PCLR in various competitive and recreational knee-strenuous sports with high-speed running, jumping, turning, cutting, pivoting, or changes of direction. The RTPf rate of our included studies after ACLR ranged from 33% to 79% and after PCLR the RTPf was 87%. These RTPf rates are in accordance with previous studies regarding RTPf. After ACLR 31% to 65% of athletes RTPf (Ardern et al., 2011a; 2012b; 2013; 2014; 2015; 2016; Grassi et al., 2015; Kvist et al., 2005; Niederer et al., 2018; Lee et al., 2008; Lentz et al., 2012; Sandon et al., 2015), while these rates are 52.4% after hip arthroscopy (Barastegui et al., 2018), 61% after meniscectomie (Aune et al., 2014), 68% after cartilage repair of the knee (Mithoefer et al., 2009), and 46% after surgically treated peroneal tendon tears (Steel and DeOrio, 2007).
We found no high-quality evidence that functional performance is associated with RTPf after ACLR or PCLR in athletes practicing high-impact sports. Recent studies also found no relationship between passing functional performance tests and return to sport (Webster and Feller, 2018; Webster et al., 2019; Webster and Hewett, 2019) or between passing functional performance tests and the risk of a reinjury (Losciale et al., 2018; Webster and Hewett, 2019). These results indicate that there is an urgent need to further investigate functional performance in association with successful outcomes (Davies et al., 2020). We recommend conducting high-quality prospective cohort studies on the association between functional performance and RTPf across a broader range of lower extremity injuries, especially after surgically treated lower extremity injuries as only approximately half to two thirds of the athletes RTPf.
Outcome measurement
Although definitions of RTPf varied slightly among the included studies, all were in accordance with the recommended international definition of RTPf (Ardern et al., 2016; Mak and Kum, 2005; D'Amico et al., 2016). Grassi et al. (2015) reported in their systematic review on RTPf after ACLR that an unclear definition or outcome measurement of RTPf could have created bias. For example, Wright et al. (2012) found that the definition ‘satisfaction’ was used where satisfaction was determined simply by asking the athletes whether they were satisfied with the outcome RTPf (Wright et al., 2012). Lentz et al. (2012) also measured RTPf with a nonvalidated self-reported measurement. They reported that a limitation of their study was the use of one question to classify the outcome RTPf or no RTPf (Lentz et al., 2012). In our included studies, the definition of RTPf was generally clear. However, the measurement of achieving RTPf is lacking in all included studies as athletes were only asked if they had returned to the same pre-injury level. During that same assessment, also the pre-injury level of performance was later retrospectively asked possibly leading to recall bias (Kopec and Esdaile, 1990; Vetter and Mascha, 2017). In a systematic review investigating RTPf rates and knee function following ACLR, Ardern et al. (2011a) also reported that almost half of the included studies inadequately reported pre-injury sports participation. To prevent athletes from not remembering their pre-injury performance level, measuring the pre-injury performance level must preferably be performed at initial visit at the orthopedic surgeon or physical therapist (Grimes and Schulz, 2002). Outcome measurement of RTPf should be validated by objectively comparing the pre-injury level with the RTPf level to prevent misclassification due to not remembering the exact pre-injury sports level (D'Amico et al., 2016; Grimes and Schulz, 2002; Lentz et al., 2012; Vetter and Mascha, 2017).
Main biases in RTPf research
Selection bias could not be excluded in all included studies. First, less athletes were actually participating than those that were eligible. Second, athletes were included when they had already returned to their pre-injury level or when rehabilitation was discontinued. Reasons for athletes’ non-participation were not reported and this might have led to selective inclusion potentially leading to biased associations (D'Amico et al., 2016; Laupacis et al., 1994; Vetter and Mascha, 2017). Reasons for loss to-follow up and characteristics of drop-outs should be known to explore attrition bias (D'Amico et al., 2016; Laupacis et al., 1994; Lu, 2009; Mak and Kum, 2005; Mann, 2003; Melamed and Robinson, 2019).
In the eight included studies, prognostic factor and outcome measurements were likely to be biased due to the simultaneous measurement and lack of description regarding blinding and methods to measure functional performance. It is possible that those observers who measured the functional performance tests were aware of the RTPf outcomes and vice versa, potentially leading to overestimation of the associations (D'Amico et al., 2016; Mak and Kum, 2005). Reproducible and clear descriptions of measurement circumstances with independent blind observers for both measuring functional performance and RTPf are required. Furthermore, athletes need to be measured on functional performance before RTPf can be observed (D'Amico et al., 2016; Laupacis et al., 1994; Lu, 2009; Mak and Kum, 2005; Mann, 2003; Melamed and Robinson, 2019).
Of the eight included studies, five measured functional performance and RTPf simultaneously approximately nine to 12 months after ACLR or PRLR. Associations resulting from cross-sectional designs can be misleading (Hanis and Mansori, 2017). Cross-sectional designs might identify possible associations and are often used to generate hypotheses, but a prospective design is preferable (Bahr, 2016). Two studies measured RTPf two to three years after ACLR (Nawasreh et al., 2018; Webster et al., 2019) and one study measured RTPf seven months (Muller et al., 2015) after ACLR. However, a follow-up period of seven months after ACLR may not be long enough to detect RTPf. It is possible that athletes did not reach RTPf yet and were prematurely classified as ‘no RTPf’. For instance, measuring RTPf seven to nine months after ACLR may be too early since it is advised to delay return to sport to at least nine months after ACLR (Beischer et al., 2018; Grindem et al., 2016). Some evidence even suggests to delay return to sport until two years after ACLR (Nagelli and Hewett, 2017). Therefore, follow-up times of two years or even more may be necessary to accurately evaluate RTPf (Ardern et al., 2015; Losciale et al., 2018; Niederer et al., 2018). In a systematic review, Everhart et al. (2015) also warned against the limitation of a too short follow-up period (median 9 months) which led to a decreased ability to detect relationship between prognostic factors and outcomes. We advise the use of prospective study designs with follow-up periods to be at least two years to reach and detect RTPf (Mak and Kum, 2005; D'Amico et al., 2016; Laupacis et al., 1994; Lu, 2009; Mann, 2003; Melamed and Robinson, 2019).
Statistical analysis and reporting was suboptimal in 75% of our included studies (Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Lee et al., 2019; Webster et al., 2019). Mostly p-values were presented for differences in functional performance tests between athletes who RTPf and athletes who did not RTPf (Edwards et al., 2018; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Lee et al., 2019; Webster et al., 2019). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) (Vandenbroucke et al., 2007) and Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) statements (Collins et al., 2015) recommend to report unadjusted and adjusted associations with 95% CI (Collins et al., 2015; Vandenbroucke et al., 2007). Estimations with CI’s measuring the strength of the association are more useful than p-values that only dichotomizes in significant or non-significant differences in results (Mak and Kum, 2005; Gardner and Altman, 1986).
Limitations
This systematic review has two potential limitations. First, when using the QUIPS tool (Hayden et al., 2006; 2013) the weighting of each prompting item for the rating of bias is unclear. Agreement between the two authors was fair and they differed mainly for domain classification in either moderate or high risk of bias. However, despite inconsistencies in domain classification, overall rating of all included studies was consistent. Second, despite our extensive search for relevant studies, reporting bias or publication bias could have influenced our findings. Positive or significant outcomes are more likely to be reported and studies with positive or significant outcomes are more likely to be submitted and more quickly published as full text than studies with negative findings (Riley et al., 2019; Dwan et al., 2008; 2013; Hopewell et al., 2009; Scherer et al., 2016). We cannot rule out that studies with less favorable results were not identified in our search and that our findings of small associations are still overoptimistic.
Clinical implications
There is no high-quality evidence of association between functional performance and RTPf. Consequently, functional performance tests are as yet not suitable for clinicians to guide predictions about successful RTPf. Functional performance tests can still be used to measure function, to guide treatment progression, and to support return to sport decision-making (Barber et al., 1992; Barber-Westin and Noyes, 2011; Hegedus et al., 2015a; Herbst et al., 2015; Hildebrandt et al., 2015; Manske and Reiman, 2013; Mueller et al., 2014; Narducci et al., 2011; Powell et al., 2018; Tassignon et al., 2019). This systematic review focused only on functional performance associated with RTPf. In the return to sport decision-making, not only functional performance is relevant (Creighton et al., 2010; Shrier, 2015). Higher quadriceps strength (Lentz et al., 2015; Hamrin Senorski et al., 2017; Lentz et al., 2012), lower fear of reinjury, and confidence to RTPf (Ardern et al., 2012a; Ardern et al., 2014; Sandon et al., 2015; Tripp et al., 2007; Ardern, 2015; Lentz et al., 2012) may also be associated with RTPf. Physical, psychological, or, more likely, a combination of these factors may contribute to RTPf and are advised to investigate in future prospective cohort studies concerning the association with RTPf (Hayden et al., 2008; Riley et al., 2013). Furthermore, seven of our eight included studies investigated associations in high-impact athletes after ACLR (Ardern et al., 2011b; Hamrin Senorski et al., 2017; Langford et al., 2009; Muller et al., 2015; Nawasreh et al., 2018; Edwards et al., 2018; Webster et al., 2019) and surgically treated lower extremity injuries other than ACLR or PCLR and non-surgical injuries seem underinvestigated regarding RTPf.
Conclusion
There is no high-quality evidence that functional performance is associated with RTPf after ACLR and PCLR nor any evidence for lower extremity injuries other than after ACLR or PCLR, in athletes practicing high-impact sports. For athletes after ACLR, low evidence of association exists for the triple hop for distance, the 6-meter timed hop, the side hop in female athletes, and the combination of the single and crossover hop for distance. The vertical jump showed a significant but small association with RTPf in athletes after PCLR. Further research on physical and psychological factors associated with RTPf is recommended in prospective cohort studies across a broader range of lower extremity injuries, especially after surgically treated lower extremity injuries other than ACLR or PCLR.
Acknowledgements
No sources of funding were used to assist in the preparation of this systematic review. The authors declare that they have no conflicts of interest relevant to the content of this systematic review. The study complied with the laws of the country of the authors’ affiliation.
Biographies

Astrid VEREIJKEN
Employment
SOMT University of Physiotherapy, the Netherlands
Degree
MSc
Research interests
Return to performance, Functional performance tests, Lower extremity injuries, High-impact sports
E-mail: a.vereijken@somtuniversity.nl

Inne AERTS
Employment
SOMT University of Physiotherapy, the Netherlands
Degree
PhD
Research interests
Jump-landing technique, Return to performance, Lower extremity injuries, High-impact sports
E-mail: i.aerts@somtuniversity.nl

Jorrit JETTEN
Employment
Annatommie MC, the Netherlands
Degree
MSc
Research interests
ACL rehabilitation, Injury management and prevention, Return to Performance, Lower extremity injuries
E-mail: j.jetten@somtuniversity.nl
Bruno TASSIGNON
Employment
Human Physiology and Sports Physiotherapy research group, Faculty of Physical Education and Physical Therapy, Vrije Universiteit Brussel
Degree
MSc
Research interests
Musculoskeletal injuries and the brain, Injury prevention, Return to sport decision-making, Fatigue, Motor learning
E-mail: bruno.tassignon@vub.be

Jo VERSCHUEREN
Employment
Human Physiology and Sports Physiotherapy research group, Faculty of Physical Education and Physical Therapy, Vrije Universiteit Brussel
Degree
MSc
Research interests
Sports physiotherapy, Injury prevention, Fatigue, Motor learning
E-mail: jo.verschueren@vub.be
Romain MEEUSEN
Employment
Human Physiology and Sports Physiotherapy research group, Faculty of Physical Education and Physical Therapy, Vrije Universiteit Brussel
Degree
Prof Dr
Research interests
Exercise and the brain in health and disease, Sports physiotherapy
E-mail: romain.meeusen@vub.be

Emiel Van TRIJFFEL
Employment
SOMT University of Physiotherapy, the Netherlands
Degree
PhD
Research interests
Diagnostics, Prognostics, Clinical reasoning
E-mail: e.vantrijffel@somtuniversity.nl
References
- Abrams G. D., Harris J. D., Gupta A. K., McCormick F. M., Bush-Joseph C. A., Verma N. N., Cole B. J., Bach B. R., Jr., (2014) Functional Performance Testing After Anterior Cruciate Ligament Reconstruction: A Systematic Review. The Orthopaedic Journal of Sports Medicine 2(1), 2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern C. L. (2015) Anterior Cruciate Ligament Reconstruction-Not Exactly a One-Way Ticket Back to the Preinjury Level: A Review of Contextual Factors Affecting Return to Sport After Surgery. Sports Health 7(3), 224-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern C. L., Glasgow P., Schneiders A., Witvrouw E., Clarsen B., Cools A., Gojanovic B., Griffin S., Khan K. M., Moksnes H., Mutch S. A., Phillips N., Reurink G., Sadler R., Silbernagel K. G., Thorborg K., Wangensteen A., Wilk K. E., Bizzini M. (2016) 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. British Journal of Sports Medicine 50(14), 853-864. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Taylor N. F., Feller J. A., Webster K. E. (2012a) Fear of re-injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. Journal of Science and Medicine in Sport 15(6), 488-495. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Taylor N. F., Feller J. A., Webster K. E. (2012b) Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. The American Journal of Sports Medicine 40(1), 41-48. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Taylor N. F., Feller J. A., Webster K. E. (2014) Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. British Journal of Sports Medicine 48(21), 1543-1552. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Taylor N. F., Feller J. A., Whitehead T. S., Webster K. E. (2013) Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. The American Journal of Sports Medicine 41(7), 1549-1558. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Taylor N. F., Feller J. A., Whitehead T. S., Webster K. E. (2015) Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. The American Journal of Sports Medicine 43(4), 848-856. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Webster K. E., Taylor N. F., Feller J. A. (2011a) Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. British Journal of Sports Medicine 45(7), 596-606. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Webster K. E., Taylor N. F., Feller J. A. (2011b) Return to the Preinjury Level of Competitive Sport After Anterior Cruciate Ligament Reconstruction Surgery Two-thirds of Patients Have Not Returned by 12 Months After Surgery. American Journal of Sports Medicine 39(3), 538-543. [DOI] [PubMed] [Google Scholar]
- Aune K. T., Andrews J. R., Dugas J. R., Cain E. L. (2014) Return to Play After Partial Lateral Meniscectomy in National Football League Athletes. The American Journal of Sports Medicine 42(8), 1865-1872. [DOI] [PubMed] [Google Scholar]
- Bahr R. (2016) Why screening tests to predict injury do not work-and probably never will…: a critical review. British Journal of Sports Medicine 50(13), 776-780. [DOI] [PubMed] [Google Scholar]
- Barastegui D., Seijas R., Alvarez-Diaz P., Rivera E., Alentorn-Geli E., Steinbacher G., Cusco X., Cugat R. (2018) Assessing long-term return to play after hip arthroscopy in football players evaluating risk factors for good prognosis. Knee Surgery, Sports Traumatology, Arthroscopy 26(3), 963-968. [DOI] [PubMed] [Google Scholar]
- Barber S. D., Noyes F. R., Mangine R., DeMaio M. (1992) Rehabilitation after ACL reconstruction: function testing. Orthopedics 15(8), 969-74. [DOI] [PubMed] [Google Scholar]
- Barber S. D., Noyes F. R., Mangine R. E., McCloskey J. W., Hartman W. (1990) Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clinical Orthopaedics and Related Research (255), 204-214. [PubMed] [Google Scholar]
- Barber-Westin S. D., Noyes F. R. (2011) Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy 27(12), 1697-1705. [DOI] [PubMed] [Google Scholar]
- Beischer S., Senorski E. H., Thomee C., Samuelsson K., Thomee R. (2018) Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Knee Surgery Sports Traumatology Arthroscopy 26(7), 1966-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonazza N. A., Smuin D., Onks C. A., Silvis M. L., Dhawan A. (2017) Reliability, Validity, and Injury Predictive Value of the Functional Movement Screen: A Systematic Review and Meta-analysis. The American Journal of Sports Medicine 45(3), 725-732. [DOI] [PubMed] [Google Scholar]
- Brophy R. H., Schmitz L., Wright R. W., Dunn W. R., Parker R. D., Andrish J. T., McCarty E. C., Spindler K. P. (2012) Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. The American Journal of Sports Medicine 40(11), 2517-2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumitt J., Heiderscheit B. C., Manske R. C., Niemuth P. E., Mattocks A., Rauh M. J. (2018) Preseason Functional Test Scores Are Associated With Future Sports Injury in Female Collegiate Athletes. The Journal of Strength and Conditioning Research 32(6), 1692-1701. [DOI] [PubMed] [Google Scholar]
- Brumitt J., Mattocks A., Loew J., Lentz P. (2019) Preseason Functional Performance Test Measures are Associated with Injury in Female Collegiate Volleyball Players. Journal of Sport Rehabilitationl 32(6), 1692-1701. [DOI] [PubMed] [Google Scholar]
- Busfield B. T., Kharrazi F. D., Starkey C., Lombardo S. J., Seegmiller J. (2009) Performance outcomes of anterior cruciate ligament reconstruction in the National Basketball Association. Arthroscopy 25(8), 825-830. [DOI] [PubMed] [Google Scholar]
- Collins G. S., Reitsma J. B., Altman D. G., Moons K. G. (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Medicine 13, 1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creighton D. W., Shrier I., Shultz R., Meeuwisse W. H., Matheson G. O. (2010) Return-to-play in sport: a decision-based model. Clinical Journal of Sport Medicine 20(5), 379-385. [DOI] [PubMed] [Google Scholar]
- D'Amico G., Malizia G., D'Amico M. (2016) Prognosis research and risk of bias. Internal and Emergency Medicine 11(2), 251-260. [DOI] [PubMed] [Google Scholar]
- Davies W. T., Myer G. D., Read P. J. (2020) Is It Time We Better Understood the Tests We are Using for Return to Sport Decision Making Following ACL Reconstruction? A Critical Review of the Hop Tests. Sports Medicine 50(3), 485-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwan K., Altman D. G., Arnaiz J. A., Bloom J., Chan A. W., Cronin E., Decullier E., Easterbrook P. J., Von Elm E., Gamble C., Ghersi D., Ioannidis J. P., Simes J., Williamson P. R. (2008) Systematic review of the empirical evidence of study publication bias and outcome reporting bias. Plos One 3(8), e3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwan K., Gamble C., Williamson P. R., Kirkham J. J., Group R. B. (2013) Systematic review of the empirical evidence of study publication bias and outcome reporting bias - an updated review. Plol One 8(7), e66844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dönmez G., Korkusuz F., Özçakar L., Karanfil Y., Dursun E., Kudaş S., Doral M. N. (2018) Injuries Among Recreational Football Players: Results of a Prospective Cohort Study. Clinical Journal of Sport Medicine 28(3), 249-254. [DOI] [PubMed] [Google Scholar]
- Edwards P. K., Ebert J. R., Joss B., Ackland T., Annear P., Buelow J. U., Hewitt B. (2018) Patient Characteristics and Predictors of Return to Sport at 12 Months After Anterior Cruciate Ligament Reconstruction The Importance of Patient Age and Postoperative Rehabilitation. Orthopaedic Journal of Sports Medicine, 6(9), 1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everhart J. S., Best T. M., Flanigan D. C. (2015) Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy 23(3), 752-762. [DOI] [PubMed] [Google Scholar]
- Gardner M. J., Altman D. G. (1986) Confidence intervals rather than P values: estimation rather than hypothesis testing. British Medical Journal (Clinical Research Ed.) 292(6522), 746-750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassi A., Zaffagnini S., Marcheggiani Muccioli G. M., Neri M. P., Della Villa S., Marcacci M. (2015) After revision anterior cruciate ligament reconstruction, who returns to sport? A systematic review and meta-analysis. British Journal of Sports Medicine 49(20), 1295-1304. [DOI] [PubMed] [Google Scholar]
- Grimes D. A., Schulz K. F. (2002) Bias and causal associations in observational research. Lancet 359(9302), 248-252. [DOI] [PubMed] [Google Scholar]
- Grindem H., Snyder-Mackler L., Moksnes H., Engebretsen L., Risberg M. A. (2016) Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. British Journal of Sports Medicine 50(13), 804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamrin Senorski E., Samuelsson K., Thomee C., Beischer S., Karlsson J., Thomee R. (2017) Return to knee-strenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surgery, Sports Traumatology, Arthroscopy 25(5), 1364-1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanis S. M., Mansori K. (2017) Is Determination of Predictors by Cross-Sectional Study Valid? The American Journal of Medicine 130(10), e455. [DOI] [PubMed] [Google Scholar]
- Harrison J. J., Yorgey M. K., Csiernik A. J., Vogler J. H., Games K. E. (2017) Clinician-Friendly Physical Performance Tests for the Knee. Journal of Athletic Training 52(11), 1068-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden J. A., Côté P., Bombardier C. (2006) Evaluation of the quality of prognosis studies in systematic reviews. Annals of Internal Medicine 144(6), 427-437. [DOI] [PubMed] [Google Scholar]
- Hayden J. A., Côté P., Steenstra I. A., Bombardier C., Group Q.-L. W. (2008) Identifying phases of investigation helps planning, appraising, and applying the results of explanatory prognosis studies. Journal of Clinical Epidemiology 61(6), 552-560. [DOI] [PubMed] [Google Scholar]
- Hayden J. A., van der Windt D. A., Cartwright J. L., Côté P., Bombardier C. (2013) Assessing bias in studies of prognostic factors. Annals of Internal Medicine 158(4), 280-286. [DOI] [PubMed] [Google Scholar]
- Hayden J. A., Wilson M. N., Riley R. D., Iles R., Pincus T., Ogilvie R. (2019) Individual recovery expectations and prognosis of outcomes in non-specific low back pain: prognostic factor review. Cochrane Database of Systematic Reviews 2019(11), 1-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegedus E. J., McDonough S., Bleakley C., Cook C. E., Baxter G. D. (2015a) Clinician-friendly lower extremity physical performance measures in athletes: a systematic review of measurement properties and correlation with injury, part 1. The tests for knee function including the hop tests. British Journal of Sports Medicine 49(10), 642-648. [DOI] [PubMed] [Google Scholar]
- Hegedus E. J., McDonough S. M., Bleakley C., Baxter D., Cook C. E. (2015b) Clinician-friendly lower extremity physical performance tests in athletes: a systematic review of measurement properties and correlation with injury. Part 2--the tests for the hip, thigh, foot and ankle including the star excursion balance test. British Journal of Sports Medicine 49(10), 649-656. [DOI] [PubMed] [Google Scholar]
- Herbst E., Hoser C., Hildebrandt C., Raschner C., Hepperger C., Pointner H., Fink C. (2015) Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part II: clinical application of a new test battery. Knee Surgery, Sports Traumatology, Arthroscopy 23(5), 1283-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt C., Müller L., Zisch B., Huber R., Fink C., Raschner C. (2015) Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part I: development of a new test battery. Knee Surgery, Sports Traumatology, Arthroscopy 23(5), 1273-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander K., Wellmann K., Eulenburg C. Z., Braumann K. M., Junge A., Zech A. (2018) Epidemiology of injuries in outdoor and indoor hockey players over one season: a prospective cohort study. British Journal of Sports Medicine 52(17), 1091-1096. [DOI] [PubMed] [Google Scholar]
- Hopewell S., Loudon K., Clarke M. J., Oxman A. D., Dickersin K. (2009) Publication bias in clinical trials due to statistical significance or direction of trial results. Cochrane Database of Systematci Reviews (1), MR000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack R. A., Sochacki K. R., Hirase T., Vickery J. W., Harris J. D. (2019) Performance and Return to Sport After Hip Arthroscopy for Femoroacetabular Impingement in Professional Athletes Differs Between Sports. Arthroscopy 35(5), 1422-1428. [DOI] [PubMed] [Google Scholar]
- Jang S. H., Kim J. G., Ha J. K., Wang B. G., Yang S. J. (2014) Functional performance tests as indicators of returning to sports after anterior cruciate ligament reconstruction. Knee 21(1), 95-101. [DOI] [PubMed] [Google Scholar]
- Kilic O., Maas M., Verhagen E., Zwerver J., Gouttebarge V. (2017) Incidence, aetiology and prevention of musculoskeletal injuries in volleyball: A systematic review of the literature. European Journal of Sport Science 17(6), 765-793. [DOI] [PubMed] [Google Scholar]
- Kilic Ö., Van Os V., Kemler E., Barendrecht M., Gouttebarge V. (2018) The 'Sequence of Prevention' for musculoskeletal injuries among recreational basketballers: a systematic review of the scientific literature. The Physician and Sportsmedicine 46(2), 197-212. [DOI] [PubMed] [Google Scholar]
- Kopec J. A., Esdaile J. M. (1990) Bias in case-control studies. A review. Journal of Epidemiology and Community Health 44(3), 179-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvist J., Ek A., Sporrstedt K., Good L. (2005) Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 13(5), 393-397. [DOI] [PubMed] [Google Scholar]
- Kyritsis P., Bahr R., Landreau P., Miladi R., Witvrouw E. (2016) Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. British Journal of Sports Medicine 50(15), 946-951. [DOI] [PubMed] [Google Scholar]
- Landis J. R., Koch G. G. (1977) The measurement of observer agreement for categorical data. Biometrics 33(1), 159-174. [PubMed] [Google Scholar]
- Langford J. L., Webster K. E., Feller J. A. (2009) A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. British Journal of Sports Medicine 43(5), 377-381. [DOI] [PubMed] [Google Scholar]
- Laupacis A., Wells G., Richardson W. S., Tugwell P. (1994) Users' guides to the medical literature. V. How to use an article about prognosis. Evidence-Based Medicine Working Group. Journal of the American Medical Assocation 272(3), 234-237. [DOI] [PubMed] [Google Scholar]
- Lee D. W., Kim J. G., Yang S. J., Cho S. I. (2019) Return to Sports and Clinical Outcomes After Arthroscopic Anatomic Posterior Cruciate Ligament Reconstruction With Remnant Preservation. Arthroscopy 35(9), 2658-2668.e1. [DOI] [PubMed] [Google Scholar]
- Lee D. Y., Karim S. A., Chang H. C. (2008) Return to sports after anterior cruciate ligament reconstruction - a review of patients with minimum 5-year follow-up. Annals of the Academy of Medicine of Singapore 37(4), 273-278. [PubMed] [Google Scholar]
- Lentz T. A., Zeppieri G., Jr., George S. Z., Tillman S. M., Moser M. W., Farmer K. W., Chmielewski T. L. (2015) Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. The American Journal of Sports Medicine 43(2), 345-353. [DOI] [PubMed] [Google Scholar]
- Lentz T. A., Zeppieri G., Jr, Tillman S. M., Indelicato P. A., Moser M. W., George S. Z., Chmielewski T. L. (2012) Return to preinjury sports participation following anterior cruciate ligament reconstruction: Contributions of demographic, knee impairment, and self-report measures. Journal of Orthopaedic and Sports Physical Therapy 42(11), 893-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losciale J. M., Zdeb R. M., Ledbetter L., Reiman M. P., Sell T. C. (2018) The Association Between Passing Return-to-Sport Criteria and Second Anterior Cruciate Ligament Injury Risk: A Systematic Review With Meta-Analysis. Journal of Orthopaedic and Sports Physical Therapy 49(2), 43-54. [DOI] [PubMed] [Google Scholar]
- Lu C. Y. (2009) Observational studies: a review of study designs, challenges and strategies to reduce confounding. The International Journal of Clinical Practice 63(5), 691-697. [DOI] [PubMed] [Google Scholar]
- Lubbe R. J., Freshman R. D., Singh G., Katchko K. M., Schneider A. D., Sharma S., Riederman B., Chang A., Hsu W. K. (2018) Performance Outcomes and Return-to-Sport Rate of National Hockey League Athletes Vary After Common Orthopedic Surgical Procedures. Clinical Journal of Sport Medicine (14), 1-6. [DOI] [PubMed] [Google Scholar]
- Mak K., Kum C. K. (2005) How to appraise a prognostic study. World Jounal of Surgery 29(5), 567-569. [DOI] [PubMed] [Google Scholar]
- Mann C. J. (2003) Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emergency Medical Journal 20(1), 54-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manske R., Reiman M. (2013) Functional performance testing for power and return to sports. Sports Health 5(3), 244-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melamed A., Robinson J. N. (2019) Case-control studies can be useful but have many limitations: Study design: case-control studies. BJOG International Journal of Obstetrics and Gynaecology 126(1), 23. [DOI] [PubMed] [Google Scholar]
- Menge T. J., Bhatia S., McNamara S. C., Briggs K. K., Philippon M. J. (2017) Femoroacetabular Impingement in Professional Football Players: Return to Play and Predictors of Career Length After Hip Arthroscopy. The American Journal of Sports Medicine 45(8), 1740-1744. [DOI] [PubMed] [Google Scholar]
- Mithoefer K., Hambly K., Della Villa S., Silvers H., Mandelbaum B. R. (2009) Return to sports participation after articular cartilage repair in the knee: scientific evidence. The American Journal of Sports Medicine 37 Suppl 1, 167S-76S. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., Group P. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology 62(10), 1006-1012. [DOI] [PubMed] [Google Scholar]
- Mueller L. M., Bloomer B. A., Durall C. J. (2014) Which Outcome Measures Should Be Used to Determine Readiness to Play After ACL Reconstruction? Journal of Sport Rehabilitation 23(2), 158-164. [DOI] [PubMed] [Google Scholar]
- Muller U., Kruger-Franke M., Schmidt M., Rosemeyer B. (2015) Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surgery, Sports Traumatology, Arthroscopy 23(12), 3623-3631. [DOI] [PubMed] [Google Scholar]
- Nagelli C. V., Hewett T. E. (2017) Should Return to Sport be Delayed Until 2 Years After Anterior Cruciate Ligament Reconstruction? Biological and Functional Considerations. Sports Medicine 47(2), 221-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagle K., Johnson B., Brou L., Landman T., Sochanska A., Comstock R. D. (2017) Timing of Lower Extremity Injuries in Competition and Practice in High School Sports. Sports Health 9(3), 238-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narducci E., Waltz A., Gorski K., Leppla L., Donaldson M. (2011) The clinical utility of functional performance tests within one-year post-acl reconstruction: a systematic review. International Journal of Sports Physical Therapy 6(4), 333-342. [PMC free article] [PubMed] [Google Scholar]
- Nawasreh Z., Logerstedt D., Cummer K., Axe M., Risberg M. A., Snyder-Mackler L. (2018) Functional performance 6 months after ACL reconstruction can predict return to participation in the same preinjury activity level 12 and 24 months after surgery. British Journal of Sports Medicine 52(6), 375-382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederer D., Engeroff T., Wilke J., Vogt L., Banzer W. (2018) Return to play, performance, and career duration after anterior cruciate ligament rupture: A case-control study in the five biggest football nations in Europe. Scandinavian Journal of Medicine and Science in Sports 28(10), 2226-2233. [DOI] [PubMed] [Google Scholar]
- Noyes F. R., Barber S. D., Mangine R. E. (1991) Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. The American Journal of Sports Medicine 19(5), 513-518. [DOI] [PubMed] [Google Scholar]
- Plisky P. J., Rauh M. J., Kaminski T. W., Underwood F. B. (2006) Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. Journal of Orthopaedic and Sports Physical Therapy 36(12), 911-919. [DOI] [PubMed] [Google Scholar]
- Powell C., Jensen J., Johnson S. (2018) Functional Performance Measures Used For Return-to-Sport Criteria in Youth Following Lower Extremity Injury. Journal of Sport Rehabilitation 27(6),581-590. [DOI] [PubMed] [Google Scholar]
- Riley R. D., Hayden J. A., Steyerberg E. W., Moons K. G., Abrams K., Kyzas P. A., Malats N., Briggs A., Schroter S., Altman D. G., Hemingway H., Group P. (2013) Prognosis Research Strategy (PROGRESS) 2: prognostic factor research. PLOS Medicine 10(2), e1001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley R. D., Moons K. G. M., Snell K. I. E., Ensor J., Hooft L., Altman D. G., Hayden J., Collins G. S., Debray T. P. A. (2019) A guide to systematic review and meta-analysis of prognostic factor studies. British Medical Journal 364, k4597. [DOI] [PubMed] [Google Scholar]
- Sandon A., Werner S., Forssblad M. (2015) Factors associated with returning to football after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 23(9), 2514-2521. [DOI] [PubMed] [Google Scholar]
- Scherer J. E., Moen M. H., Weir A., Schmikli S. L., Tamminga R., van der Hoeven H. (2016) Factors associated with a more rapid recovery after anterior cruciate ligament reconstruction using multivariate analysis. Knee 23(1), 121-126. [DOI] [PubMed] [Google Scholar]
- Schmikli S. L., Backx F. J., Kemler H. J., van Mechelen W. (2009) National survey on sports injuries in the Netherlands: target populations for sports injury prevention programs. Clinical Journal of Sport Medicine 19(2), 101-106. [DOI] [PubMed] [Google Scholar]
- Shrier I. (2015) Strategic Assessment of Risk and Risk Tolerance (StARRT) framework for return-to-play decision-making. British Journal of Sports Medicine 49(20), 1311-1315. [DOI] [PubMed] [Google Scholar]
- Sousa P. L., Krych A. J., Cates R. A., Levy B. A., Stuart M. J., Dahm D. L. (2017) Return to sport: Does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? Knee Surgery, Sports Traumatology, Arthroscopy 25(5), 1356-1363. [DOI] [PubMed] [Google Scholar]
- Steel M. W., DeOrio J. K. (2007) Peroneal tendon tears: return to sports after operative treatment. Foot and Ankle International 28(1), 49-54. [DOI] [PubMed] [Google Scholar]
- Tassignon B., Verschueren J., Delahunt E., Smith M., Vicenzino B., Verhagen E., Meeusen R. (2019) Criteria-Based Return to Sport Decision-Making Following Lateral Ankle Sprain Injury: a Systematic Review and Narrative Synthesis. Sports Medicine 49(4), 601-619. [DOI] [PubMed] [Google Scholar]
- te Wierike S. C., van der Sluis A., van den Akker-Scheek I., Elferink-Gemser M. T., Visscher C. (2013) Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scandinavian Journal of Medicine and Science in Sports 23(5), 527-540. [DOI] [PubMed] [Google Scholar]
- Terwee C. B., Bot S. D., de Boer M. R., van der Windt D. A., Knol D. L., Dekker J., Bouter L. M., de Vet H. C. (2007) Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology 60(1), 34-42. [DOI] [PubMed] [Google Scholar]
- Thomee R., Kaplan Y., Kvist J., Myklebust G., Risberg M. A., Theisen D., Tsepis E., Werner S., Wondrasch B., Witvrouw E. (2011) Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 19(11), 1798-805. [DOI] [PubMed] [Google Scholar]
- Tjong V. K., Murnaghan M. L., Nyhof-Young J. M., Ogilvie-Harris D. J. (2014) A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: to play or not to play. The American Journal of Sports Medicine 42(2), 336-342. [DOI] [PubMed] [Google Scholar]
- Toole A. R., Ithurburn M. P., Rauh M. J., Hewett T. E., Paterno M. V., Schmitt L. C. (2017) Young Athletes Cleared for Sports Participation After Anterior Cruciate Ligament Reconstruction: How Many Actually Meet Recommended Return-to-Sport Criterion Cutoffs? Journal of Orthopaedic and Sports Physical Therapy 47(11), 825-833. [DOI] [PubMed] [Google Scholar]
- Tripp D. A., Stanish W., Ebel-Lam A., Brewer B. W., Birchard J. (2007) Fear of reinjury, negative affect, and catastrophizing predicting return to sport in recreational athletes with anterior cruciate ligament injuries at 1 year postsurgery. Rehabilitation Psychology 52(1), 74-81. [Google Scholar]
- van Beijsterveldt A. M., Stubbe J. H., Schmikli S. L., van de Port I. G., Backx F. J. (2015) Differences in injury risk and characteristics between Dutch amateur and professional soccer players. Journal of Science and Medicine in Sport 18(2), 145-149. [DOI] [PubMed] [Google Scholar]
- van der Horst N., van de Hoef S., Reurink G., Huisstede B., Backx F. (2016) Return to Play After Hamstring Injuries: A Qualitative Systematic Review of Definitions and Criteria. Sports Medicine 46(6), 899-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenbroucke J. P., von Elm E., Altman D. G., Gøtzsche P. C., Mulrow C. D., Pocock S. J., Poole C., Schlesselman J. J., Egger M., Initiative S. (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 18(6), 805-835. [DOI] [PubMed] [Google Scholar]
- Vetter T. R., Mascha E. J. (2017) Bias, Confounding, and Interaction: Lions and Tigers, and Bears, Oh My!. Anesthesia and Analgesia 125(3), 1042-1048. [DOI] [PubMed] [Google Scholar]
- Vogler J. H., Csiernik A. J., Yorgey M. K., Harrison J. J., Games K. E. (2017) Clinician-Friendly Physical Performance Tests for the Hip, Ankle, and Foot. Journal of Athletic Training 52(9), 861-862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster K. E., Feller J. A. (2018) Return to Level I Sports After Anterior Cruciate Ligament Reconstruction: Evaluation of Age, Sex, and Readiness to Return Criteria. Orthopaedic Journal of Sports Medicine 6(8), 1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster K. E., Hewett T. E. (2019) What is the Evidence for and Validity of Return-to-Sport Testing after Anterior Cruciate Ligament Reconstruction Surgery? A Systematic Review and Meta-Analysis. Sports Medicine 49(6), 917-929. [DOI] [PubMed] [Google Scholar]
- Webster K. E., McPherson A. L., Hewett T. E., Feller J. A. (2019) Factors Associated With a Return to Preinjury Level of Sport Performance After Anterior Cruciate Ligament Reconstruction Surgery. The American Journal of Sports Medicine 47(11), 2557-2562. [DOI] [PubMed] [Google Scholar]
- Whalan M., Lovell R., McCunn R., Sampson J. A. (2019) The incidence and burden of time loss injury in Australian men's sub-elite football (soccer): A single season prospective cohort study. Journal of Science and Medicine in Sport 22(1), 42-47. [DOI] [PubMed] [Google Scholar]
- Wolff R. F., Moons K. G. M., Riley R. D., Whiting P. F., Westwood M., Collins G. S., Reitsma J. B., Kleijnen J., Mallett S., Group P. (2019) PROBAST: A Tool to Assess the Risk of Bias and Applicability of Prediction Model Studies. Annals of Internal Medicine 170(1), 51-58. [DOI] [PubMed] [Google Scholar]
- Wright R. W., Gill C. S., Chen L., Brophy R. H., Matava M. J., Smith M. V., Mall N. A. (2012) Outcome of revision anterior cruciate ligament reconstruction: a systematic review. Journal of Bone and Joint Surgery American volume 94(6), 531-536. [DOI] [PMC free article] [PubMed] [Google Scholar]


