Abstract
Introduction
Little information exists on the status of oral hygiene behavior (OHB) and socioeconomic inequalities in developing countries like Iran. The aim of this study was to assess OHB and its determinants and socioeconomic inequality among schoolchildren in western Iran during 2018.
Methods
A cross-sectional survey was conducted on 1,457 students aged 12–15 years living in Kermanshah city, western Iran. We used multistage sampling to select the samples. A self-administrated questionnaire was used to collect data on OHB, sociodemographic characteristics, and economic status of the households of students. Multivariate logistic regression was used to examine the association between OHB and its determinants. We used the relative concentration index, normalized (RCIn) and a concentration curve (CC) to examine socioeconomic-related inequality in OHB.
Results
The study indicated that crude and age-adjusted prevalence of good OHB was 14.61% (95% CI 12.89%–16.53%) and 15.17% (95% CI 13.22%–17.35%), respectively. Logistic regression analysis showed that sex, mother’s education, socioeconomic status, and oral health literacy had a statistically significant positive impact on OHB. RCIn (0.2582, 95% CI0.1770–0.3395) values and the CC indicated that good OHB was more concentrated among the richer children.
Conclusion
This study provides evidence that good OHB was less prevalent, signifying that oral health remains a public-health concern in Iran. Effective polices aimed at improving the socioeconomic status of households and mother’s education can contribute positively and to the prevention of oral disorders among schoolchildren.
Keywords: schoolchildren, oral health behaviors, concentration curve, logistic regression
Introduction
Despite oral health playing a key role in determining the quality of life, overall health status and well-being of people, poor oral hygiene (OH) remains one of the major public-health concerns globally.1 While an overall improvement in oral health has been reported, prevalence of dental caries is still high, especially among those in low socioeconomic households.2,3
Dental caries is preventable disease. To control dental caries, the World Health Organization (WHO) recommends that proper OH care, decreased sugar intake, and regular oral health checkups by dental providers are among the main OH behaviors (OHBs) to prevent dental diseases.4 Recent studies have found strong associations between oral health status and such OHB as tooth brushing, tooth flossing, and regular checkups.5,6 Although the status of OHB and its determinants among schoolchildren has been examined extensively,5,7-9 evidence on inequalities in OHB and its determinants are rarely documented.10,11 However, previous work hashighlighted that OHB is influenced by several factors, including sociodemographic factors, socioeconomic status of households, and parents’ education.
While oral health status is a public-health concerns, especially among schoolchildren, there is limited information about OHB and its socioeconomic-related inequalities among schoolchildren in Iran.10,12 To fill this gap in the literature, this study aimed to explore prevalence, determinants, and socioeconomic inequality in OHB among 12- to 15-year-old students in Kermanshah city, western Iran. This information should help policy-makers in designing effective interventions to increase the prevalence of preventive OHB and prevent oral diseases.
Methods
Study Setting and Sampling Method
This cross-sectional survey was carried out from October to November 2018 in Kermanshah city, the capital of Kermanshah province, western Iran. The study population was schoolchildren aged 12–15 years. For sample-size estimation, we used a formula based on the prevalence of good OHB:13
 |
where n is the sample size, calculated at the 95% level of significance (Z=1.96), p the prevalence of good OHB, equal to 0.5 (to obtain maximum samples), and d precision of 0.025. To improve the generalizability of the study findings, we added 40 students to theobtained sample size. Multistage sampling was used to select samples. For this purpose, firstly Kermanshah city was divided into five areas (central, western, eastern, southern, and northern) to select our sample. Secondly, from each geographic area, we randomly selected at least one girls’ school and one boys’ school. Finally, using a census method, we included all students aged 12–15 years enrolled in the selected schools in our sample. When the number of students in a school was insufficient, we invited another school to participate in the study. The final sample consisted of 1,577 students from 14 schools: eight girls’ schools and six boys’ schools. We invited the students to complete a structured questionnaire administered by two trained public-health students. Due to uncompleted questionnaires, 120 samples were excluded from the analysis, which resulted in a final sample of 1,457 schoolchildren for statistical analysis.
Data and Variables
A self-constructed questionnaire was used for data collection. The questionnaire had three parts. The first part focused on sociodemographic characteristics: age and sex of students, mother’s education, father’s education, sex of head of household, and place of birth. The second part focused on housing:, eg, eg, rooms per capita, type of ownership, size, and durable assets, eg, house, car, computer/laptop, access to Internet, freezer, dishwasher, TV. The third part focused on student’s OHB, eg, regular daily brushing, regular daily flossing, visiting dentist every 6 months, and oral health literacy). The outcome of interest, OHB, was a binary variable indicating whether or not students had good OHB. As per existing literature,4,12 OHB was defined as good if the students cleaned their teeth by brushing and flossed once daily, as well as visiting a dentist every 6 months.
Principal-component analysis was used to construct the wealth index. Items included in the wealth index are ownership of a car, color TV, computer/laptop, mobile phone, freezer, dishwasher, microwave, vacuum cleaner, motorcycle, and bicycle, in addition to number of rooms per capita, type of house ownership, and house size. Based on wealth scores obtained, we divided the samples into five quintiles from the poorest to the richest.14 Based on existing literature,7,9,12,15 age of children, sex of children, mother’s education, father’s education, sex of head of household, constructed wealth index of household (as a proxy for socioeconomic status of household), and oral health literacy were used as determinants of the students’ OHB.
Statistical Analysis
Socioeconomic Determinants of Good OHB
Because the outcome variable was binary, we used multivariate logistic regression to assess associations between good OHB and explanatory variables included in the study:
 |
where y is good OHB, age age of the children, edum mother’s education, eduf father’s education, genhh the sex of head of household, ses the socioeconomic status of household, ohlit oral health literacy, and  the residual.
the residual.
Measuring Socioeconomic Inequality in Oral Health Behaviors
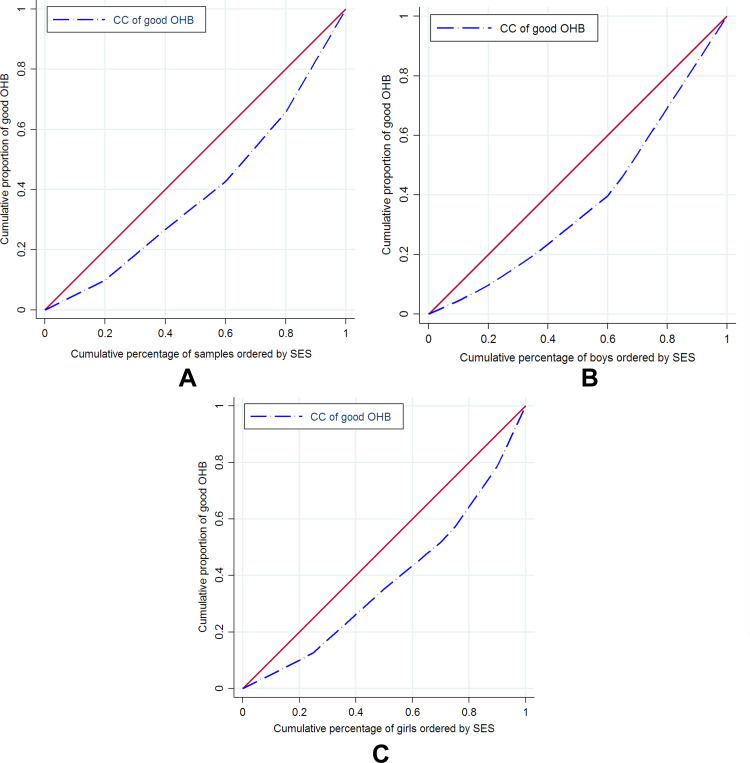
We used a concentration curve (CC) and relative concentration index (RCI) to assess the magnitude of socioeconomic-related inequality in good OHB.16 The CC is a graph that plots the cumulative percentage of samples ranked by socioeconomic status on the x-axis against the cumulative percentage of the outcome variable (good OHB in this study) on the y-axis. If the CC lies above (under) the perfect-equality line, good OHB was more concentrated among poor (rich) samples. The RCI has values of −1 to +1. If the RCI were negative (positive), this suggested that the prevalence of good OHB was more prevalent among the poor (rich) samples.
The RCI can be computed thus:
 |
where is the mean or the proportion of good OHB, yi shows good OHB, and ri is the fractional rank in the socioeconomic distribution for the ith students. As the outcome variable was binary (0 and 1) in this study, RCI values were not –1 to +1, and thus we normalized the (RCIn) by multiplying the estimate by  .17 We used Stata version 14.2 (Stata Corp, College Station, TX, USA) for analysis, and findings were deemed statistically significant at p<0.05.
.17 We used Stata version 14.2 (Stata Corp, College Station, TX, USA) for analysis, and findings were deemed statistically significant at p<0.05.
Results
Table 1 presents the descriptive analysis of our sample. A total of 1,457 schoolchildren (512 boys and 945 girls) participated in the study. Mean age of the study population was 13.1±0.9 years. Crude and adjusted prevalence of good OHB was 14.61% (95% CI 12.89%–16.53%) and 15.17% (95% CI 13.22%–17.35%), respectively. Crude prevalence of OHB between boys and girls was different: 14.25% (95% CI 11.48%–17.57%) for boys and 14.81% (95% CI 12.68%–17.23%) for girls.
Table 1.
Descriptive Characteristics and Prevalence of Good OHB Among Schoolchildren in Kermanshah City, Western Iran, 2018
| n (%) | Prevalence of Good OHB (%) | ||
|---|---|---|---|
| Crude OR (95% CI) | Age-adjusted OR (95% CI) | ||
| Age | 1,457 (100) | 14.61 (12.89–16.53) | 15.17 (13.22, 17.35) |
| Sex | |||
| Boys | 512 (35.14) | 14.25 (11.48, 17.57) | 15.39 (12.15, 19.30) |
| Girls | 945 (64.86) | 14.81 (12.68, 17.23) | 15.30 (12.89, 18.07) |
| Mother’s education | |||
| Uneducated or elementary | 643 (44.13) | 10.26 (8.13, 12.86) | 10.39 (8.05, 13.33) |
| Academic degree | 814 (55.87) | 18.05 (15.56, 20.85) | 19.33 (16.43, 22.60) |
| Father’s education | |||
| Uneducated or elementary | 501 (34.39) | 11.37 (8.87, 14.47) | 12.15 (8.41, 9.07) |
| Academic degree | 956 (65.61) | 16.31 (14.10, 18.80) | 16.95 (14.45, 19.78) |
| Sex of household head | |||
| Male | 1,390 (95.40) | 14.96 (13.18, 16.94) | 15.53 (13.52, 17.77) |
| Female | 67 (4.60) | 7.46 (30.68, 17.04) | 4.62 (2.02, 10.21) |
| Wealth index of households | |||
| Poorest | 292 (20.04) | 7.19 (4.72, 10.80) | 5.78 (3.79, 8.71) |
| Poor | 291 (19.97) | 12.37 (9.03, 16.70) | 14.86 (10.43, 20.73) |
| Middle | 293 (20.11) | 11.60 (8.39, 15.83) | 11.97 (8.15, 17.25) |
| Rich | 290 (19.90) | 16.89 (12.98, 21.68) | 16.92 (12.84,21.97) |
| Richest | 291 (19.97) | 25.08 (20.41, 30.41) | 25.09 (20.29, 30.60) |
| IOral health of similar importance to that of rest of body | |||
| Yes | 1,333 (91.6) | 13.95 (12.19, 15.92) | 14.34 (12.38, 16.56) |
| No | 122 (8.4) | 21.31 (14.85, 29.59) | 26.12 (17.25, 37.49) |
Abbreviation: OHB, oral hygiene behavior.
Table 2 presents the relationship between good OHB and the explanatory variables included in the logistic regression model. There was a statistically significant positive relationship between the sex of children and good OHB. The probability of having good OHB was higher among children with educated mothers than their peers wwith uneducated mothers (adjusted OR 1.62; 95% CI 1.08–2.41). The results also showed a direct association between prevalence of good OHB and wealth status. For example, the prevalence of good OHB was more than 4.9 times higher (adjusted OR 4.87, 95% CI 2.65–8.94)] among children belonging to the richest quintile compared to the children from the poorest quintile. Perspectives of students on oral health literacy was another significant factor affecting good OHB.
Table 2.
Associations Between Independent Variables and Good OHB (Logistic Regression Model)
| OR | ||||
|---|---|---|---|---|
| Crude (95% CI) | p-value | Adjusted (95% CI) | p-value | |
| Age | 1.08 (0.93,1.25) | 0.28 | 1.05 (0.91, 1.23) | 0.75 |
| Sex | ||||
| Boys | 1 (reference) | 1 (reference) | ||
| Girls | 1.04 (0.77, 1.42) | 0.290 | 1.80 (1.26, 2.55) | 0.001 |
| Mother’s education | ||||
| Uneducated or elementary | 1 (reference) | 1 (reference) | ||
| Academic degree | 1.92 (1.41, 2.62) | 0.001 | 1.62 (1.08, 2.41) | 0.018 |
| Father’s education | ||||
| Uneducated or elementary | 1 (reference) | 1 (reference) | ||
| Academic degree | 1.51 (1.09, 2.10) | 0.012 | 0.80 (0.52, 1.22) | 0.304 |
| Sex of household head | ||||
| Male | 1 (reference) | 1 (reference) | ||
| Female | 0.45 (0.18, 1.15) | 0.098 | 0.52 (0.20, 1.31) | 0.163 |
| Wealth index of households | ||||
| Poorest | 1 (reference) | 1 (reference) | ||
| Poor | 1.82 (1.03, 3.20) | 0.037 | 1.78 (1.00, 3.17) | 0.05 |
| Middle | 1.69 (0.95, 2.99) | 0.070 | 1.69 (0.92, 3.08) | 0.085 |
| Rich | 2.62 (1.52, 4.50) | 0.001 | 2.71 (1.51, 4.88) | 0.001 |
| Richest | 4.32 (2.57, 7.24) | 0.001 | 4.87 (2.65, 8.94) | 0.001 |
| Oral health of similar importance to that of rest of body | ||||
| No | 1 (reference) | 1 (reference) | ||
| Yes | 1.67 (1.05, 2.64) | 1.99 (1.23, 3.21) | 0.005 | |
Abbreviation: OHB, oral hygiene behavior.
Prevalence of good OHB among the poorest socioeconomic groups was 7.19% (95% CI 4.72%–0.80%) compared to 25.08% (95% CI 20.41%–30.41%) for the richest groups. RCIn values for good OHB for the whole sample of boys and girls are presented in Table 3. As indicated in Table 3, good OHB was more prevalent among students from richer families (RCIn 0.2582, 95% CI 0.1770–0.3395). RCIn values for both boys and girls were positive and statistically significant, suggesting that prevalence of good OHB for both boys and girls was more concentrated among the better-off samples. Figure 1 shows the CC for good OHB for the whole sample. As illustrated, the CCs is under the perfect-equality line, meaning that good OHB was more prevalent among the richer students.
Table 3.
RCIn Values for Good OHB for Entire Sample Kermanshah City, Western Iran, 2018
| RCIn | p-value | 95% CI | |
|---|---|---|---|
| Whole sample | 0.2582 | 0.001 | 0.1770, 0.3395 |
| Boys | 0.2745 | 0.001 | 0.1387, 0.4104 |
| Girls | 0.2798 | 0.001 | 0.1801, 0.3795 |
Abbreviations: OHB, oral hygiene behavior; RCIn, relative concentration index, normalized.
Figure 1.
Concentration curve of good OHB for the whole samples (A), boys (B), and girls (C) in Kermanshah, western Iran, 2018.
Discussion
Although oral health status has improved in all age-groups in developed countries over the past few decades, oral disorders remaina public-health concern in developing countries like Iran. Having sufficient information on factors affecting OHB and its inequalities is crucial to design programs and interventions to improve OHB and decrease oral disorders. This study examined the status of OHB and socioeconomic-related inequality among schoolchildren in Kermanshah city. In our study, the overall prevalence of good OHB was 14.6% among schoolchildren. It was different between boys and girls, and prevalence of good OHB among girls (14.8%) was more than boys (14.2%). Our study indicated that prevalence of regular brushing, flossing, and regular checking every 6 months was 84.3%, 38.5%, and 26.3%, respectively. Goodarzi et al12 found that 55.3%% of female students aged 10–12 years brushed at least twice per day, 22.4% used dental floss, and 23% reported a routine dental visit every 6 months. Prevalence of flossing or mouthwash use among dental students is 49.7% in China18 and that of OHB among schoolchildren 26.7% in Cambodia.19
The findings of the regression analysis indicated that sex, mother’s education, socioeconomic status of households, and oral health literacy (ie, oral health of similar importance to that of rest of body) were the main factors affecting good OHB among schoolchildren. Research from Iran also showed that associations between mother’s education, father’s job, and family income and regular brushing were positive and significant.12 Mishra et al20 reported education level and awareness of parents in relation to OHB as a key factor affecting oral health of their children. Others have also revealed positive associations of being female and older with OHB.19 A study in China21 indicated that mother’s education and being female were the main factors affecting good OHB among middle school students aged 12–15 years. Hernández-Palacios et al found that a positive association exists between poor oral health condition and lower education status.22 One reason for this is associated with the environment and community conditions where children are born and grown up.
In terms of socioeconomic-related inequality, the current study demonstrated that prevalence of good OHB was more concentrated among students with higher socioeconomic status, similar to Mashoto et al in Tanzania,23 Vereecken et al in Belgium,24 and Maes et al.25 Similar results were also found for boy and girl students separately. A national study10 in Iran showed that prevalence of tooth brushing increased with improvement in socioeconomic quintiles (groups). Their study indicated that the gap in frequency of tooth brushing between the first and fifth socioeconomic groups was 20%. Others have shown a significant prorich inequality in tooth brushing for both boys and girls.26 Furthermore, a positive association between poor oral health and lower socioeconomic status was also foundby Hosseinpoor et al27 Pothidee et al28 in Thailand, Martins et al29 in Brazil, and Moradi et al30 in Kurdistan.
The current study provides useful information on the status of OHB, related factors, and inequalities among children 12–15 years old in western Iran. These findings can be used for designing and implementing effective interventions to improve oral health and reduce inequalities in oral health outcomes. However, despite its contribution to the knowledge base on OHB status for improved oral health in Iran, this study had some limitations that need to be considered. Firstly, the data used were collected based on self-report and thus subject to recall bias. Secondly, the design was cross-sectional, and so we are not able establish any causal link between good OHB and explanatory variables included in the analysis. Thirdly, it was carried out in one city only, and thus its generalizability to other provinces and Iran as a whole is limited.
Conclusion
The current study explored the status of OHB, determinants, and socioeconomic-related inequality among schoolchildren 12–15 years old in west of Iran. We found that prevalence of good OHB was very low (<25% of study population). Female sex, mother’s education, higher socioeconomic, status and oral health literacy were identified as the main determinants of good OHB. This suggests that government action when it comes to targeted awareness campaigns for oral health might help close the inequality gap in oral health literacy. We also found there was a prorich distribution of good OHB among students. However, it is recommended that designing any interventions to improve oral health or prevent oral disorders should be done based on main determinants of good OHB. Based on determinants of OHB and inequalities therein, a holistic approach is required to increase OHB, improve oral health, and decrease oral health inequalities in any oral health reform. Further works to identify explanatory variables contributing to inequality in OHB are highly recommended.
Acknowledgments
We would like to thank the school principals for their role in obtaining parental consent for this study. The authors also would like to thank Dr Abraha Woldemichael from the College of Health Sciences, Mekelle University, Ethiopia for helpful comments on the paper.
Funding Statement
This work was funded by Kermanshah University of Medical Sciences (code 97413). The funders had no role in study design, data analysis, decision to publish, or preparation of the manuscript.
Abbreviations
OHB, oral hygiene behavior; CC, concentration curve; RCIn, relative concentration index, normalized.
Data-Sharing Statement
All necessary data are presented within the manuscript. All other materials and data are available upon reasonable request to the corresponding author.
Ethics Approval and Consent to Participate
The study protocol was reviewed and approved by the ethics committee of the Deputy of Research, Kermanshah University of Medical Sciences (KUMS.REC.1397.436). Verbal informed consent, confirmed by the ethics committee, was obtained from each student after obtaining informed consent from school principals and parents of the students. The study was conducted in accordance with the Declaration of Helsinki.
Author Contributions
SR contributed to the research idea, study design, and performing the study. SR and HRYA contributed to data analysis and interpretation and writing the manuscript. HRYA revised the manuscript critically for important intellectual content. The authors gave final approval to the version to be published, agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work. All authors made a significant contribution to the work reported, whether in conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval to the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
- 1.Peres MA, Macpherson LM, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–260. doi: 10.1016/S0140-6736(19)31146-8 [DOI] [PubMed] [Google Scholar]
- 2.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661–669. doi:/S0042-96862005000900011 [PMC free article] [PubMed] [Google Scholar]
- 3.Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102(3):411–418. doi: 10.2105/AJPH.2011.300362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organization WH. WHO information series on school health–document 11–oral health promotion: an essential element of a health-promoting school. Geneva: World Health Organization; 2003. Available from: www who int/oral_health/media/en/orh_school_doc11 pdf. Last Accessed November6, 2017. [Google Scholar]
- 5.Qiu RM, Tao Y, Zhou Y, Zhi QH, Lin HC. The relationship between children’s oral health-related behaviors and their caregiver’s social support. BMC Oral Health. 2016;16(1):86. doi: 10.1186/s12903-016-0270-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen PE. Global policy for improvement of oral health in the 21st century–implications to oral health research of World Health Assembly 2007, World Health Organization. Community Dent Oral Epidemiol. 2009;37(1):1–8. doi: 10.1111/j.1600-0528.2008.00448.x [DOI] [PubMed] [Google Scholar]
- 7.Bozorgmehr E, Hajizamani A, Malek Mohammadi T. Oral health behavior of parents as a predictor of oral health status of their children. ISRN Dent. 2013;2013:1–5. doi: 10.1155/2013/741783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neamatollahi H, Ebrahimi M. Oral health behavior and its determinants in a group of Iranian students. Indian J Dent Res. 2010;21(1):84. doi: 10.4103/0970-9290.62820 [DOI] [PubMed] [Google Scholar]
- 9.Vakili M, Rahaei Z, Nadrian H, YarMohammadi P. Determinants of oral health behaviors among high school students in Shahrekord, Iran based on Health Promotion Model. Am Dent Hyg Assoc. 2011;85(1):39–48. [PubMed] [Google Scholar]
- 10.Safiri S, Kelishadi R, Heshmat R, et al. Socioeconomic inequality in oral health behavior in Iranian children and adolescents by the Oaxaca-Blinder decomposition method: the CASPIAN-IV study. Int J Equity Health. 2016;15(1):143. doi: 10.1186/s12939-016-0423-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomson W, Poulton R, Milne B, Caspi A, Broughton J, Ayers K. Socioeconomic inequalities in oral health in childhood and adulthood in a birth cohort. Community Dent Oral Epidemiol. 2004;32(5):345–353. doi: 10.1111/j.1600-0528.2004.00173.x [DOI] [PubMed] [Google Scholar]
- 12.Goodarzi A, Heidarnia A, Tavafian SS, Eslami M. Predicting oral health behaviors among Iranian students by using health belief model. J Educ Health Promot. 2019;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6(1):14. [PMC free article] [PubMed] [Google Scholar]
- 14.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459–468. doi: 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- 15.Cheema S, Maisonneuve P, Al-Thani MH, et al. Oral health behavior and factors associated with poor oral status in Qatar: results from a national health survey. J Public Health Dent. 2017;77(4):308–316. doi: 10.1111/jphd.12209 [DOI] [PubMed] [Google Scholar]
- 16.O’Donnell O, O’Neill S, Van Ourti T, Walsh B. Conindex: estimation of concentration indices. Stata J. 2016;16(1):112–138. doi: 10.1177/1536867X1601600112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wagstaff A. The concentration index of a binary outcome revisited. Health Econ. 2011;20(10):1155–1160. doi: 10.1002/hec.1752 [DOI] [PubMed] [Google Scholar]
- 18.Yao K, Yao Y, Shen X, Lu C, Guo Q. Assessment of the oral health behavior, knowledge and status among dental and medical undergraduate students: a cross-sectional study. BMC Oral Health. 2019;19(1):26. doi: 10.1186/s12903-019-0716-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peltzer K, Tepirou C, Pengpid S. Prevalence and correlates of perceived teeth health status and oral health behavior among school-going adolescents in Cambodia. Nagoya J Med Sci. 2016;78(4):493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mishra A, Pandey R, Chopra H, Arora V. Oral health awareness in school-going children and its significance to parent’s education level. J Indian Soc Pedod Prev Dent. 2018;36(2):120–124. doi: 10.4103/JISPPD.JISPPD_1172_17 [DOI] [PubMed] [Google Scholar]
- 21.Deng L, Cai T, Li Y-H, Zhou Z, Yang Z-Y. Tooth brushing behavior and its influencing factors among middle school students in Chongqing, China. Int J Clin Exp Med. 2019;12(7):8957–8963. [Google Scholar]
- 22.Hernández-Palacios RD, Ramírez-Amador V, Jarillo-Soto EC, Irigoyen-Camacho ME, Mendoza-Núñez VM. Relationship between gender, income and education and self-perceived oral health among elderly Mexicans. An exploratory study. Cien Saude Colet. 2015;20:997–1004. doi: 10.1590/1413-81232015204.00702014 [DOI] [PubMed] [Google Scholar]
- 23.Mashoto KO, Astrom AN, Skeie MS, Masalu JR. Socio-demographic disparity in oral health among the poor: a cross sectional study of early adolescents in Kilwa district, Tanzania. BMC Oral Health. 2010;10(1):7. doi: 10.1186/1472-6831-10-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vereecken CA, Maes L, De Bacquer D. The influence of parental occupation and the pupils’ educational level on lifestyle behaviors among adolescents in Belgium. J Adolesc Health. 2004;34(4):330–338. doi: 10.1016/S1054-139X(03)00301-X [DOI] [PubMed] [Google Scholar]
- 25.Maes L, Vereecken C, Vanobbergen J, Honkala S. Tooth brushing and social characteristics of families in 32 countries. Int Dent J. 2006;56(3):159–167. doi: 10.1111/j.1875-595X.2006.tb00089.x [DOI] [PubMed] [Google Scholar]
- 26.Levin K, Currie C. Inequalities in toothbrushing among adolescents in Scotland 1998–2006. Health Educ Res. 2009;24(1):87–97. doi: 10.1093/her/cym096 [DOI] [PubMed] [Google Scholar]
- 27.Hosseinpoor A, Itani L, Petersen P. Socio-economic inequality in oral healthcare coverage: results from the World Health Survey. J Dent Res. 2012;91(3):275–281. doi: 10.1177/0022034511432341 [DOI] [PubMed] [Google Scholar]
- 28.Pothidee T, Sringernyuang L, Tuongratanaphan S. Inequity in access to oral health service of primary students: a case study of a dental fund in a central region province. Kasetsart J Soc Sci. 2016;37(3):175–181. doi: 10.1016/j.kjss.2016.08.006 [DOI] [Google Scholar]
- 29.Martins MT, Sardenberg F, Vale MP, Paiva SM, Pordeus IA. Dental caries and social factors: impact on quality of life in Brazilian children. Braz Oral Res. 2015;29(1). doi: 10.1590/1807-3107BOR-2015.vol29.0133 [DOI] [PubMed] [Google Scholar]
- 30.Moradi G, Moinafshar A, Adabi H, Sharafi M, Mostafavi F, Bolbanabad AM. Socioeconomic inequalities in the oral health of people aged 15–40 years in Kurdistan, Iran in 2015: a cross-sectional study. J Prev Med Public Health. 2017;50(5):303. doi: 10.3961/jpmph.17.035 [DOI] [PMC free article] [PubMed] [Google Scholar]