ABSTRACT
Background:
The motor functions of Rett syndrome patients degrade during the course of the disease. Some patients, however, are able to maintain their motor functions by undertaking exercise programs.
Case:
A 2-year-old girl was diagnosed with Rett syndrome after the identification of a mutation in the gene encoding the methyl-CpG-binding protein. The patient started weekly rehabilitation therapy; however, over time, this reduced to monthly sessions, and subsequently, because of worsening epileptic seizures, even fewer sessions were possible. When the patient was 12 years old, intensive rehabilitation therapy was undertaken for 1 month; therapy involved 80 min of in-hospital therapy on weekdays and walking exercises at home at the weekend. An accelerometer (Actiwatch 2, standard type, Philips Respironics) indicated that more than 60 min of daily training at an intensity of 3 metabolic equivalents (METs) or more was achieved at weekends. The patient took the 10-m walk test, and the average time reduced from 18.6 to 13.5 s and the number of steps reduced from 32 to 23 between the start and finish of the first 1-month intensive training regime. After being discharged from the hospital, the patient maintained walking exercises at school during weekdays and performed more than 50 min/day of activity at at least 3 METs at home on weekends, in addition to a weekly home-visit rehabilitation therapy and the annual in-hospital 1-month rehabilitation therapy. Four years later, the patent’s average time and number of steps required to walk 10 m remained lower (12.7 s, 24 steps) than those recorded at the first evaluation.
Discussion:
Periodic rehabilitation therapy and proactive walking exercises at more than 3 METs for a duration of up to 50 min/day were instrumental in maintaining the motor functions of a Rett syndrome patient.
Keywords: motor function, rehabilitation therapy, Rett syndrome
INTRODUCTION
Rett syndrome is a genetic disorder that mainly affects girls1,2) and is characterized by a loss in motor and intellectual functions. The developmental progress of the disease at an initial age of 1 year may be slow, but the characteristic features of Rett syndrome appear subsequently along with degradation in motor and intellectual functions.3) However, in some patients, motor functions can be maintained and even improved beyond the regression period.3)
Herein, we report the case of a girl with Rett syndrome who maintained motor function for 4 years by following a proactive walking routine and undergoing a periodic rehabilitation therapy program in a hospital and at home. Using an accelerometer, we also evaluated the amount and intensity of exercise that the patient performed.
CASE
Our patient was a 17-year-old girl who, before the periodic medical checkup at 1.5 years old, had achieved certain physical milestones (rolling over, crawling on all fours, kneeling, and pulling herself upright) and achieved the ability to toddle several steps on her own. At the 1.5-year checkup, hand movements characteristic of Rett syndrome were noted. Subsequently, standing became difficult for her, and support was needed with hand-holding even when walking two or three steps. When the patient was 2 years old, a mutation in the gene encoding methyl-CpG-binding protein was found and she was diagnosed with Rett syndrome.
Following the diagnosis, the patient began rehabilitation therapy. She attended a development support center near her home; this facility provides rehabilitation therapy to children with developmental disabilities. Therapy was scheduled once a week during the preschool period, and once a month after elementary school was started. As the patient grew older, she developed a visible dystonic posture, tonic seizures, hyperventilation, and breath-holding behaviors. In 2011, when the patient was 9 years old, the first clonic seizure was observed in the left arm, and topiramate was administered. In 2012, breath-holding behavior began to appear and was treated by increasing the dose of topiramate. In 2013, because of the persistence of breath-holding behaviors, topiramate was replaced with phenobarbital and sodium valproate, and this treatment led to a decrease in the frequency of symptoms. The first menstruation occurred in 2013 when the patient was 11 years old, and after that, the frequency of hyperventilation and muscle stiffness increased and worsened. Increasing the dose of sodium valproate was not effective, but starting lamotrigine in 2014 reduced the frequency of hyperventilation and muscle stiffness. Because of the above-mentioned symptoms, her attendance at the Development Support Center decreased from once a month to less than once every 2 months. She kept attending school, but the opportunities for rehabilitation therapy were reduced.
The patient was first admitted to a hospital in 2014 at 12 years of age to undergo intensive rehabilitation therapy in an attempt to delay motor function degradation. Her height and weight on admission to hospital were 130.0 cm and 18.3 kg. She had scoliosis in the thoracic and lumbar spine: the spine was convex to the left at the thoracic spine (Th) from Th3 to Th11 and convex to the right at the thoracic to lumbar spine (L) from Th12 to L5. The Cobb angle was not measured at this time. The patient could roll-over by herself, but required assistance to pull herself up when sitting on the bed; furthermore, support from behind was needed when she stood up. She could walk several steps when held by either hand, but tended to bend to the right, with her torso leaning backward. Her cognitive function was evaluated using the Kyoto Scale of Psychological Development 2001.4) The developmental ages (DAs) for each of the three categories in the test were 11 months for Postural-Motor (fine and gross motor functions), the DA was too low to be calculated for Cognitive-Adaptive (nonverbal reasoning or visuospatial perceptions assessed using materials such as blocks, miniature cars, or marbles), and 5 months for Language-Social (interpersonal relationships, socialization, and verbal abilities); the overall DA was 5 months. The developmental quotients (DQs) for each of the three categories, calculated using the DAs of each category and the overall DA divided by the child’s chronological age and multiplied by 100, was 8 for Postural-Motor, not available for Cognitive-Adaptive, and 3 for Language-Social. The DQ for the overall DA was 3.
Physiological and occupational therapy were each delivered for 40 min every day from Monday to Friday. Therapies included exercises lying over a peanut-shaped ball to relax the tensed muscles of the torso. Furthermore, exercises were performed to enhance flexibility around shoulders. During these, the patient held with both hands a pulley hanging from a bar above her head and moved the pulley upwards and downwards alternatively. This exercise expanded not only the range of shoulder movements but also the range of torso movements as the patient moved her upper body in all directions. Because rehabilitation therapies were not scheduled on Saturdays and Sundays at the hospital, the patient and her mother went home every Friday afternoon and stayed there until Monday morning. During the weekends, the patient’s mother was instructed by the therapists to ensure that the patient continued the exercises for at least 80 min, i.e., the same duration as the applied hospital therapy. Consequently, the mother actively encouraged the patient to walk while performing daily activities, for instance, urging her to walk from her room to the toilet or taking her out shopping or to a local park. The child repeated this routine for 4 weeks, i.e., rehabilitation therapy at the hospital during the week and walking while performing daily activities at home on the weekends.
After 4 weeks of intensive training, the patient did not require support from behind when standing up, but holding one of her hands was still required. The patient was able to remain standing without support for a longer time than she could before admission to the hospital. The patient was discharged from the hospital and her mother followed the instructions for continued home care provided by the therapists. The patient was encouraged to continue walking while performing daily activities, e.g., walking a distance of 400 m from home to the bus stop every morning to catch the bus to the special education school, walking from her classroom to the toilet at a distance of about 50 m, and undertaking routine weekend walks to a shopping center or to a nearby park. Moreover, a weekly home-visit rehabilitation program was commenced.
From 2014 to 2018, the patient annually repeated the 1-month-long rehabilitation program at the hospital. Her height and weight increased from 130.0 cm to 142.0 cm and from 18.3 kg to 22.9 kg during these 4 years. The Cobb angle was 23.8° and 19.8° in 2016 and 2017, respectively, as measured using X-ray images with the patient in the standing position. The therapy program conducted each year at the hospital remained largely the same as that administered during the first admission in 2014, i.e., 40 min each of physiotherapy and occupational therapy per day; furthermore, the routine walk to the park or to the shopping center was undertaken every weekend from home.
During the first and last weeks of the first hospital admission in 2014, the patient took the 10-m walk test to evaluate changes in motor function. Four consecutive trials of the test were undertaken and the mean values of the time and steps required to walk 10 m were calculated. The 10-m walk test was again taken during the fifth hospital admission in 2018.
During the first admission in 2014 and the fifth admission in 2018, using an accelerometer (Actiwatch 2, standard type, Philips Respironics), we assessed the amount and intensity of exercise the patient was performing at home each weekend. The Actiwatch 2 detects horizontal and vertical motions greater than 0.025 g acceleration at a sampling rate of 32 Hz. The activity count for every minute was recorded. The mother was advised to keep the instrument attached to the patient’s wrists and ankles for the whole day. An activity count exceeding 450/min signified an exercise intensity of greater than 3 metabolic equivalents (METs).5) The time for which the activity counts were >450/min on either extremity were summed to estimate the total duration of activities performed at an intensity >3 METs. The data evaluated in the present study were collected on Saturdays and Sundays between 06:00 and 23:59.
During the first hospital admission in 2014, the amount of time spent with an activity count exceeding 450/min averaged 83 min/day on the first weekend, 53 min on the second weekend, 54 min on the third weekend, and 64 min on the fourth weekend, with a mean value of 63 min (Table 1). During the fifth admission in 2018, the amount of active time calculated for each weekend was 46 min, 46 min, and 67 min, with an average value of 53 min.
Table 1. Total time per day during which activity exceeded 450 counts/min as measured using an Actiwatch 2 on upper and lower extremities.
| Year | First week (min/day) |
Second week (min/day) |
Third week (min/day) |
Fourth week (min/day) |
Mean (min/day) |
| 2014 | 83 | 53 | 54 | 64 | 63 |
| 2018 | 46 | 46 | 67 | N/E | 53 |
N/E: Not examined.
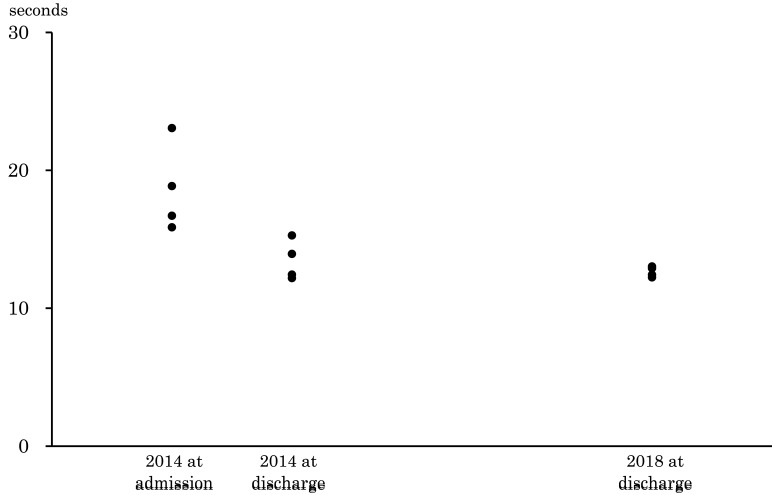
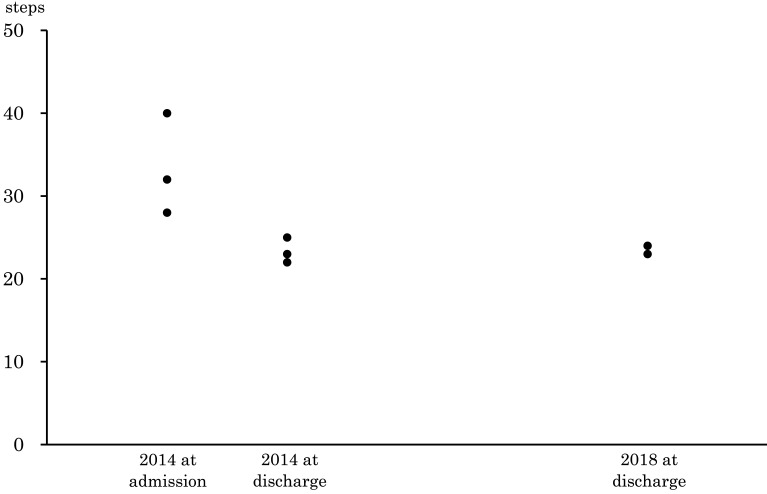
The results of the four consecutive trials of the 10-m walk test are shown in Figs. 1, 2. During the first week of the first admission in 2014, the times required by the patient to walk 10 m were 15.9 s, 16.7 s, 23.1 s, and 18.9 s (Fig. 1), with a mean value of 18.6 s (not shown). In the last week of the 2014 admission, the results were 12.2 s, 12.4 s, 13.9 s, and 15.3 s, with a mean value of 13.5 s (not shown). The patient was tested again during the 2018 admission, and the results were 12.2 s, 12.4 s, 12.9 s, and 13.0 s, with a mean value of 12.7 s (not shown). Similarly, during the first week of the 2014 admission, the numbers of steps required to walk 10 m were 28, 28, 40, and 32 (Fig. 2), and the average number was 32 (not shown). In the last week of the 2014 admission, the numbers of steps required were 23, 22, 25, and 25, and the average was 23 (not shown). The results in 2018 were 24, 23, 24, and 23 steps, and the average was 24 steps (not shown). Informed consent to publish the patient’s data was obtained from her mother.
Fig. 1.
Changes in the time required to walk 10 m.
Fig. 2.
Changes in the number of steps required to walk 10 m.
DISCUSSION
In the present report, a patient affected by Rett syndrome improved her motor function by following an intensive rehabilitation therapy program conducted from Monday to Friday at a hospital and, on the instruction of her therapists, the patient undertook a proactive walking routine on weekends at home. The amount and intensity of exercise were measured at up to 1 h/day of motion at an intensity greater than 3 METs. In 2014, the time and number of steps required by the patient to walk 10 m at discharge from a 1-month hospital-based rehabilitation program had decreased compared with the same parameters measured at admission.
The results of the 10-m walk test in 2018 remained better than those of the first test in 2014, which suggests that the patient’s motor function had improved and had been maintained for 4 years (2014–2018) by undertaking daily walking activities of more than 50 min/day on average with an intensity greater than 3 METs. Activities involved weekly home-visit rehabilitation programs and annual 1-month rehabilitation programs at the hospital.
The clinical features of many Rett syndrome patients develop in four clinical stages;6) the second and fourth stages are characterized by rapid regression of acquired abilities. Between these two stages lies the pseudo-stationary stage, in which the speed of regression slows. During this period, characteristic hand movements and visual contact behavior become prominent and breathing irregularities, such as the Valsalva maneuver, bruxism while awake, or dystonic posture, may become frequent. All of the above-mentioned behaviors were observable in our patient, which suggested that she was in the pseudo-stationary stage.
During the pseudo-stationary stage, in most cases, motor regression progresses slowly, rather than halting completely.3) Some of the comorbidities that affect this stage are the development of epilepsy and scoliosis, which lead to a reduction in the range of daily motor activities performed.7,8) The adolescent and adult years are most often the time when rehabilitation therapy services are reduced and are less available,9) which may also contribute to the regression of motor functions. Before the first intensive rehabilitation therapy program was undertaken in 2014, the motor function in our patient was also degrading because of frequent epilepsy attacks. Before this time, although the patient had been undergoing rehabilitation programs once a month, the therapies or exercises might have been too few or of too low in intensity.
Despite the debilitating characteristics of the disease and the related socio-medical challenges, some studies have, against expectations, reported improvements in motor skills as a result of regular daily activities,3) regular physiotherapy sessions,10) or treadmill exercises.11) Just as in Rett syndrome, Down syndrome is caused by a chromosomal abnormality and causes low muscle tone and difficulties in achieving motor skills at a young age. A recent meta-analysis conducted across 27 articles covering 842 subjects reported that physical interventions had positive effects on muscle strength in both the upper and lower limbs.12) In our case, the introduction of a daily walking routine and a regular rehabilitation therapy program after the first hospital admission may have contributed to the maintenance of our patient’s motor functions for 4 years.
The amount and intensity of exercise required to maintain or improve motor function in Rett syndrome patients are not clear. In our patient, in addition to daily school activities, walking exercises with an intensity of more than 3 METs for about 1 h/day seem to have improved motor functions, and the same exercises for more than 50 min/day helped to maintain them. In a report investigating 170 elderly subjects aged more than 65 years, it was found that fitness levels were maintained by continuing habitual activities of more than 20 min/day at an intensity of 3 METs or more.13) Although it is uncertain whether the data for elderly subjects can be applied to Rett syndrome patients, we may assume that low levels of physical activity are the key factor behind decreased motor functions for both types of subject, and we postulate that a certain level of regular exercise may help in maintaining the motor functions of these patients. Further research is required to clarify this issue.
In conclusion, proactive exercises and periodic rehabilitation therapies were useful in maintaining the motor functions of a Rett syndrome patient. Further studies are required to assess the importance of the amount and intensity of exercise in improving or maintaining such patients’ motor functions.
ACKNOWLEDGMENTS
The authors thank the nurses and other health-care professionals of the Division of Pediatric Medicine, Ibaraki Prefectural University of Health Sciences Hospital, for their cooperation in this study.
Footnotes
CONFLICTS OF INTEREST: All authors declare that there are no conflicts of interest.
REFERENCES
- 1.Amir RE,Van Den Veyver IB,Schultz R,Malicki DM,Tran CQ,Dahle EJ,Philippi A,Timar L,Percy AK,Motil KJ,Lichtarge O,O’Brian Smith E,Glaze DG,Zoghbi HY: Influence of mutation type and X chromosome inactivation on Rett syndrome phenotypes. Ann Neurol 2000;47:670–679. [DOI] [PubMed] [Google Scholar]
- 2.Amir RE,Van den Veyver IB,Wan M,Tran CQ,Francke U,Zoghbi HY: Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat Genet 1999;23:185–188. 10.1038/13810 [DOI] [PubMed] [Google Scholar]
- 3.Foley KR,Downs J,Bebbington A,Jacoby P,Girdler S,Kaufmann WE,Leonard H: Change in gross motor abilities of girls and women with Rett syndrome over a 3- to 4-year period. J Child Neurol 2011;26:1237–1245. 10.1177/0883073811402688 [DOI] [PubMed] [Google Scholar]
- 4.Koyama T,Osada H,Tsujii H,Kurita H: Utility of the Kyoto Scale of Psychological Development in cognitive assessment of children with pervasive developmental disorders. Psychiatry Clin Neurosci 2009;63:241–243. 10.1111/j.1440-1819.2009.01931.x [DOI] [PubMed] [Google Scholar]
- 5.Lee P,Tse CY: Calibration of wrist-worn ActiWatch 2 and ActiGraph wGT3X for assessment of physical activity in young adults. Gait Posture 2019;68:141–149. 10.1016/j.gaitpost.2018.11.023 [DOI] [PubMed] [Google Scholar]
- 6.Smeets EE,Pelc K,Dan B: Rett syndrome. Mol Syndromol 2011;2:113–127. 10.1159/000337637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ager S,Fyfe S,Christodoulou J,Jacoby P,Schmitt L,Leonard H: Predictors of scoliosis in Rett syndrome. J Child Neurol 2006;21:809–813. 10.1177/08830738060210091501 [DOI] [PubMed] [Google Scholar]
- 8.Jian L,Nagarajan L,de Klerk N,Ravine D,Christodoulou J,Leonard H: Seizures in Rett syndrome: an overview from a one-year calendar study. Eur J Paediatr Neurol 2007;11:310–317. 10.1016/j.ejpn.2007.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stewart DA,Law MC,Rosenbaum P,Willms DG: A qualitative study of the transition to adulthood for youth with physical disabilities. Phys Occup Ther Pediatr 2002;21:3–21. 10.1080/J006v21n04_02 [DOI] [PubMed] [Google Scholar]
- 10.Larsson G,Witt Engerström I: Gross motor ability in Rett syndrome – the power of expectation, motivation and planning. Brain Dev 2001;23(Suppl 1):S77–S81. 10.1016/S0387-7604(01)00334-5 [DOI] [PubMed] [Google Scholar]
- 11.Lotan M,Hanks S: Physical therapy intervention for individuals with Rett syndrome. Sci World J 2006;6:1314–1338. 10.1100/tsw.2006.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruiz-González L,Lucena-Antón D,Salazar A,Martín-Valero R,Moral-Munoz JA: Physical therapy in Down syndrome: systematic review and meta-analysis. J Intellect Disabil Res 2019;63:1041–1067. 10.1111/jir.12606 [DOI] [PubMed] [Google Scholar]
- 13.Aoyagi Y,Park H,Watanabe E,Park S,Shephard RJ: Habitual physical activity and physical fitness in older Japanese adults: the Nakanojo Study. Gerontology 2009;55:523–531. 10.1159/000236326 [DOI] [PubMed] [Google Scholar]