Abstract
Background and objective
Since the first case of the pneumonia caused by 2019 novel coronavirus (COVID-19) is found in Wuhan, there have been more than 70,000 cases reported in China. This study aims to perform the meta-analysis of risk factors for the case fatality rate (CFR) of the 2019 novel coronavirus (COVID-19).
Design and methods
We have searched PubMed, Google scholar and medRxiv for the cohort studies involving risk factors for the CFR of COVID-19. This meta-analysis compares the risk factors of CFR between fatal patients and non-fatal patients.
Results
Two cohort studies are included in this study. After comparing the patients between fatal cases and non-fatal cases, several important factors are found to significantly increase the CFR in patients with COVID-19, and include the age ranging 60–70 (OR = 1.85; 95% CI = 1.62 to 2.11; P < .00001) and especially≥70 (OR = 8.45; 95% CI = 7.47 to 9.55; P < .00001), sex of male (OR = 1.88; 95% CI = 1.30 to 2.73; P = .0008), occupation of retirees (OR = 4.27; 95% CI = 2.50 to 7.28; P < .00001), and severe cases (OR = 691.76; 95% CI = 4.82 to 99,265.63; P = .01). As the advancement of early diagnosis and treatment, the CFR after January 21 (or 22), 2020 is substantially decreased in COVID-19 than before (OR = 0.21; 95% CI = 0.19 to 0.24; P < .00001).
Conclusions
Several factors are confirmed to significantly improve the CFR in patients with COVID-19, which is very important for the treatment and good prognosis of these patients.
Keywords: 2019 novel coronavirus (COVID-19), Risk factor, CFR, Meta-analysis
1. Introduction
In December 2019, the novel coronavirus–infected pneumonia (NCIP) is first found in Wuhan, Hubei Province, China [[1], [2], [3], [4]]. It is highly associated with Huanan Seafood Wholesale Market. As the ongoing spring festival travel in China and the worldwide travel, the number of NCIP patients have been rapidly increased [5]. There are more than 70,000 cases by February 20, 2020 in China. On January 3, 2020, the 2019 novel coronavirus (COVID-19) is identified to result in NCIP, and is a novel betacoronaviruses confirmed by high-throughput sequencing [6,7]. COVID-19 is defined as the seventh member of enveloped RNA coronavirus (subgenus sarbecovirus, Orthocoronavirinae subfamily), and has some similar features of severe acute respiratory syndrome coronavirus (SARS-CoV) [6].
COVID-19 is highly thought to be associated with Huanan Seafood Wholesale Market and delivered to humans from wild animals illegally sold [8]. According to the first 425 confirmed NCIP in Wuhan from December 2019 to January 2020, the epidemiologic characteristics confirmed human-to-human transmission among close contacts since the middle of December 2019 and revealed that the epidemic was doubled in size every 7.4 days in the early stage [3]. The human-to-human transmission of NCIP was also confirmed by case reports and family settings [[9], [10], [11], [12]]. The novel coronavirus was found in stool samples of patients with abdominal symptoms, indicating that fecal-oral transmission might occur for NCIP [13].
Some studies have helped understand the molecular, clinical and epidemiological features of the COVID-19 [6,14,15]. One cohort study conducted in Jin Yin-tan Hospital (Wuhan, China) first reported the epidemiological, clinical, laboratory and radiological characteristics, as well as clinical outcomes in 41 NCIP patients [16]. The clinical features mainly include fever, cough, dyspnea, myalgia, fatigue, sputum production, headache, haemoptysis, and diarrhoea [17,18].
Some underling comorbidities may have some effect on the exacerbation of NCIP, and they include diabetes, hypertension, cardiovascular disease, chronic obstructive pulmonary disease (COPD), malignancy and chronic liver disease etc. [[18], [19], [20], [21]]. In addition, the exacerbations of some cases commonly lead to organ dysfunction such as shock, acute respiratory distress syndrome (ARDS), acute cardiac injury, acute kidney injury and even death [16,22]. Some severe patients with COVID-19 resemble that of SARS-CoV [8,16]. Another cohort study also systematically reported the epidemiological and clinical features of 138 patients with NCIP in Zhongnan Hospital of Wuhan University (Wuhan, China) [18].
Nonpharmaceutical interventions such as shutdown of public gathering places, wearing of facial masks and social distancing are still effectively slow the spread of the disease. There is currently no antiviral treatment or vaccine specifically designed for this virus with field-proven effectiveness, and supportive therapies are mainly used for these patients [23]. There have been more than 2, 000 deaths in China. This meta-analysis is conducted to reveal the risk factors for CFR in patients with COVID-19, which is valuable to improve the treatment and prognosis of these patients.
2. Methods
Ethical approval and patient consent were not required because this was a meta-analysis of previously published studies. Two investigators independently searched the following databases (inception to February 202,020): PubMed, Google scholar, medRxiv and CNKI. The electronic search strategy was performed using with the following keywords: “novel coronavirus” or “COVID-19”, and “epidemiological” or “clinical features” or “clinical characteristics” or “death” or “case fatality rate” or “CFR”.
The following inclusive selection criteria were applied: (i) patients were diagnosed with 2019 novel coronavirus diseases (COVID-19) (ii) study design was the cohort study comparing fatal patients with non-fatal patients (or severe cases versus non-severe cases).
We used a piloted data-extraction sheet, and collected the following information: publication year, first author, number of patients, age, gender and the number of non-severe/severe cases in two groups. Data were extracted independently by two investigators. This meta-analysis focused on the risk factors including baseline characteristics and severity on the CFR of COVID-19. Furthermore, the risk factors that would be analyzed should be compared in both of two included studies.
Odds ratio (OR) with 95% confidence intervals (CI) was used for all dichotomous outcomes. The random-effects model was used regardless of heterogeneity which was assessed by I2 statistic. I2 > 50% indicated significant heterogeneity [24]. Sensitivity analysis was needed when encountering significant heterogeneity. P < .05 suggested statistically significance between two groups. All analysis were conducted using Review Manager Version 5.3.
3. Results
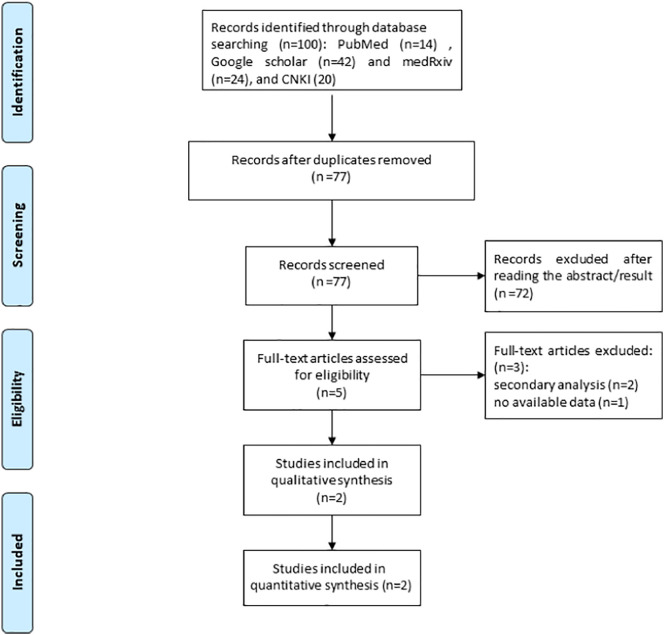
A detailed flowchart of the search and selection results is shown in Fig. 1 . One hundred potentially relevant articles were identified initially, and two cohort studies involving 48,666 patients are finally included in this study [23,25]. Two studies that did not compare the epidemiological and clinical features between fatal cases and non-fatal cases are removed [16,17].
Fig. 1.
Flow diagram of study searching and selection process.
Among the two included cohort studies, one preprint trial reports 8866 patients including 4021 laboratory confirmed patients from 30 provinces through January 26, 2020 [23]. Another study is published in Chinese and involve 44, 672 confirmed patients from the team of Chinese Center for Disease Control and Prevention (CDC). The data collected is from information system for infectious disease reporting through February 11th, 2020 [25].
The main characteristics (e.g. age, gender and severity of patients) of the two cohort studies are presented in Table 1 . After carefully analyzing the two studies, age, sex, occupation and severity are selected for the association with CFR of COVID-19.
Table 1.
Characteristics of included studies
| Study 1: Yang 2020 |
Study 2: CDC 2020 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group | Number | Age | Male | Female | Non-severe/ severe cases (n) | Number | Age | Male (n) | Female (n) | Non-severe/ severe cases (n) |
| Fatal group | 58 | 69 ± 15 | 44 | 14 | 3/55 | 1023 | – | 653 | 370 | 0/1023 |
| Non- fatal group | 3963 | 48 ± 16 | 2169 | 1794 | 3083/880 | 43,649 | – | 22,328 | 21,321 | 36,417/7232 |
3.1. Association analysis between age with CFR
Two studies revealed that severe cases are significantly older than those non-severe cases [17,18]. The study conducted by Guan et al. involving 1099 patients with confirmed novel coronavirus that severe cases have significantly older age than non-severe cases (52.0 (40.0–65.0) versus 45.0 (34.0–57.0), median (range), P < .001) [17]. These indicate that old age may also result in the increase in CFR in these patients.
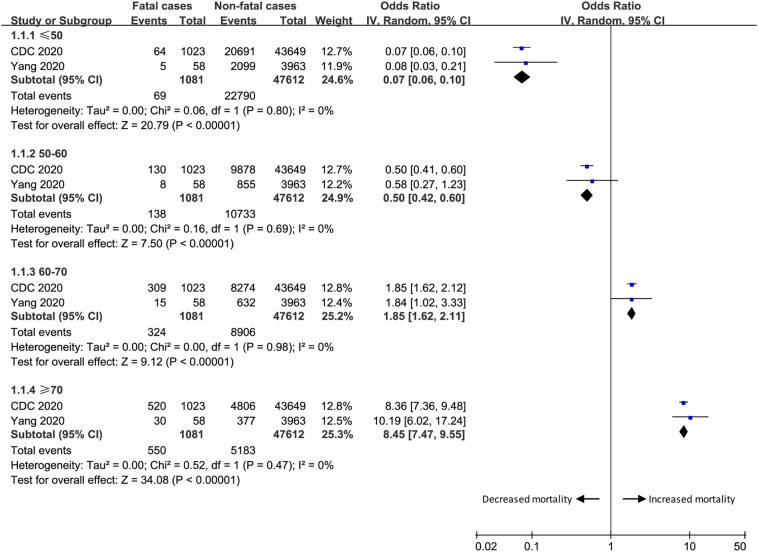
The association analysis between age range with CFR is revealed in Fig. 2 . The age ≤ 50 (OR = 0.07; 95% CI = 0.06 to 0.10; P < .00001) and ranging 50–60 (OR = 0.50; 95% CI = 0.42 to 0.60; P < .00001) is associated with obviously relatively lower incidence of CFR, while the age ranging 60–70 (OR = 1.85; 95% CI = 1.62 to 2.11; P < .00001) and especially≥70 (OR = 8.45; 95% CI = 7.47 to 9.55; P < .00001) results in the significant increase in CFR. These results suggest that age ≥ 60 can be regarded as the risk factor for CFR in patients with COVID-19.
Fig. 2.
The association analysis between age with CFR.
3.2. Association analysis between sex with CFR
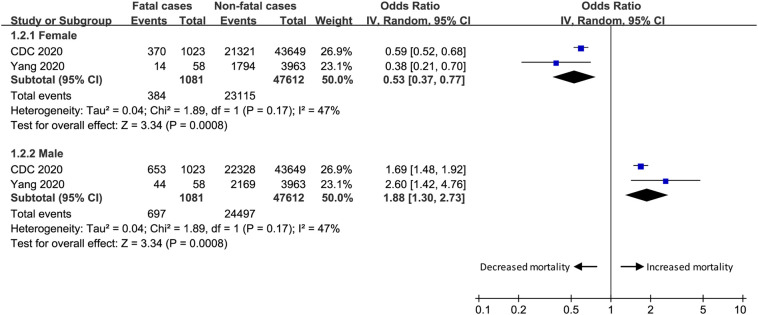
In this study, we mainly find the association between sex and CFR of these patients (Fig. 3 ). This meta-analysis indicates that the sex of female is associated with relatively lower incidence of CFR (OR = 0.53; 95% CI = 0.37 to 0.77; P = .0008), while the sex of male leads to the obvious increase in CFR for COVID-19 (OR = 1.88; 95% CI = 1.30 to 2.73; P = .0008).
Fig. 3.
The association analysis between sex with CFR.
3.3. Association analysis between occupation with CFR
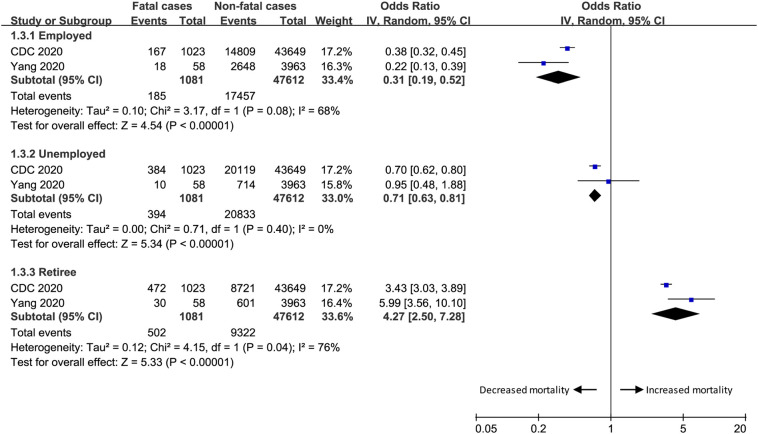
The CDC study reported five kinds of occupation, including service industry, farmer/worker, medical worker, retiree, and others [25]. In order to perform the analysis between occupation with CFR, service industry, farmer/worker, and medical worker are generally regarded as employed persons, while others are generally thought to be unemployed persons.
In our meta-analysis between occupation with CFR (Fig. 4 ), the results indicate that employed persons (OR = 0.31; 95% CI = 0.19 to 0.52; P < .00001) and unemployed persons (OR = 0.71; 95% CI = 0.63 to 0.81; P < .00001) lead to relatively lower incidence of CFR, but retirees have the significant increase in CFR in patient with COVID-19 (OR = 4.27; 95% CI = 2.50 to 7.28; P < .00001).
Fig. 4.
The association analysis between occupation with CFR.
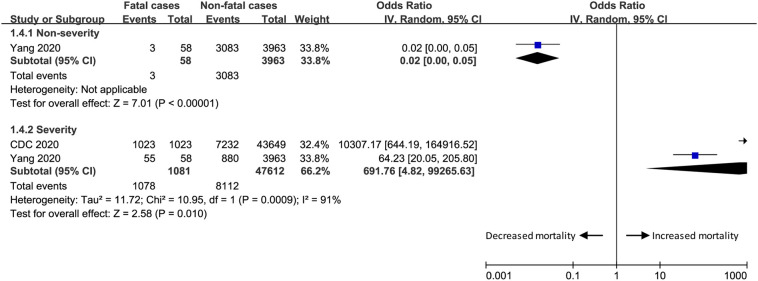
3.4. Association analysis between severity with CFR
It is widely accepted that severe cases receive intensive care unit (ICU) care, while non-severe cases do not receive ICU care. Among 41 admitted hospital patients with COVID-19 in Jin Yin-tan Hospital, Wuhan, China, there are 5 deaths in 13 ICU patients (38%) and 1 death in 28 non-ICU patients (4%), suggesting that severe cases is more likely to die [16].
This meta-analysis also confirms it (Fig. 5 ). Non-severe cases have significantly lower incidence of CFR for COVID-19 (OR = 0.02; 95% CI = 0 to 0.05; P < .00001), while severe cases reveal the remarkable improvement in CFR (OR = 691.76; 95% CI = 4.82 to 99,265.63; P = .01).
Fig. 5.
The association analysis between severity with CFR.
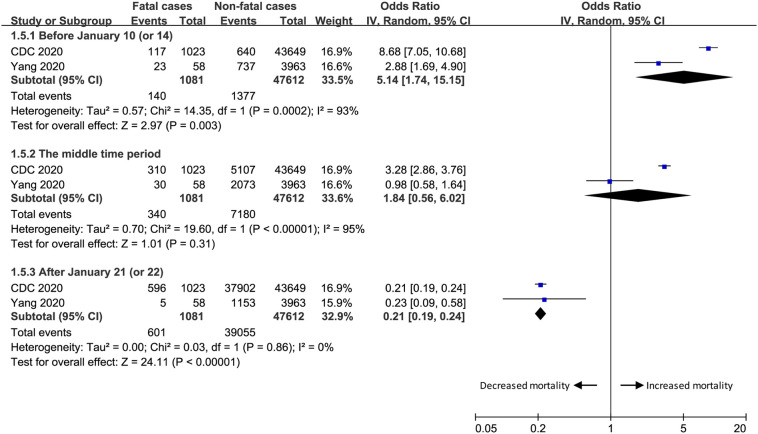
3.5. Association analysis between time periods with CFR
The time periods are generally divided into three periods: before January 10 (or 14), 2020, after January 21 (or 22), 2020 and the middle time period between them. In our meta-analysis (Fig. 6 ), the CFR before January 10 (or 14), 2020 is relatively high (OR = 5.14; 95% CI = 1.74 to 15.15; P = .003), but the CFR is significantly reduced after January 21 (or 22), 2020 (OR = 0.21; 95% CI = 0.19 to 0.24; P < .00001).
Fig. 6.
The association analysis between time period with CFR.
4. Discussion
The transmissibility of COVID-19 is similar to that of SARS-CoV in the range of 2.9–3.3% [23]. The overall adjusted CFR is estimated to be 3.06% for the COVID-19, which is lower than those of SARS-CoV (9.2%) and MERS-CoV (34.4%) [20]. One included study demonstrates that patients in ICU group is significantly older than those in non-ICU group (66 (57–78) versus 51 (37–62), median (IQR), P < .001) [18], which is consistent with the study conducted by Guan et al. [17].
Furthermore, the old age limit ≥65 years may be defined as the risk factor for exacerbation of COVID-19 (P < .001) [17]. Our results reveal that age ranging 60–70 age and especially≥70 is found to have notably increased CFR in these patients, and thus age ≥ 70 can be regarded as the important risk factor for increased CRF. In addition, retirees are revealed to have improved CFR than other occupations of patients with COVID-19 in this meta-analysis, which may be attributed to older age of retirees.
Patients with low immune function such as old age, obesity, presence of comorbidity, HIV infection, longterm use of immune-suppressive agents and pregnant women may have improved CFR [26]. Prompt administration of antibiotics to prevent infection and immune support treatment may reduce the complications and CFR of these patients [8]. The reduced lymphocytes was found in most patients, suggesting that 2019nCoV may mainly damage lymphocytes, especially T lymphocytes, which was similar to SARSCoV. Substantially decreased T lymphocytes might be an important factor for predicting the exacerbations of patients [27].
A descriptive study reported 99 cases of NCIP from Wuhan Jinyintan Hospital from Jan 1 to Jan 20, 2020, and demonstrated that older men with comorbidities was more likely to suffer from NCIP and ARDS. [8]. In contrast, the proportion of men and women showed no statistical difference between ICU patients and non-ICU patients in another study [18]. There are conflicting results regarding the relationship between sex and severity of COVID-19. In this meta-analysis, male patients have significantly higher CFR than female patients. Resembling the SARS-CoV and the Middle East Respiratory Syndrome coronavirus (MERS-CoV), COVID-19 was reported to adversely affect the elderly male subpopulation more than any other subpopulations, as evidenced by both the highest incidence of confirmed patients and the highest CFR [16]. Asian males have higher prevalence of ACE2 receptors in their lungs and the virus acts mainly through binding to ACE2 receptors, which may account for the gender difference [28].
It is generally known that severe cases and patients receiving ICU have higher possibility of death than other patients for diseases. One cohort study involving 1099 patients reported 14 deaths in 173 severe cases (8.1%) and 1 death in 926 non-severe cases (0.1%), and significant difference of CFR is observed between severe cases and non-severe cases [17]. These results are also confirmed in this meta-analysis. Severe cases with COVID-19 have increased CFR than non-severe cases.
Regarding the sensitivity analysis, there is significant heterogeneity for occupation, severity and time period. Several reasons may account for this heterogeneity. Firstly, in the analysis of CDC study, service industry, farmer/worker, and medical worker are generally regarded as employed persons, while others are generally thought to be unemployed persons [25], which may produce the heterogeneity for occupation. Secondly, one study reported the mild pneumonia/non-pneumonia versus severe pneumonia [23], while the CDC study reported the mild cases versus severe/critically ill cases [25], and thus there is lack of clear definition of non-severe versus severe cases, which may cause the heterogeneity for severity analysis. Thirdly, different patient populations in the three time periods are selected in two studies, which may explain the heterogeneity for the analysis of time periods. Fourthly, these two studies are retrospective trials, which also produce some heterogeneity.
One study also confirmed that the patients in ICU group had more comorbid diseases than those patients in non-ICU group [18]. Older age and comorbidity may be risk factors for the exacerbation of NCIP [8]. Furthermore, the comorbid diseases such as cardiovascular diseases, COPD and hypertension may also increase the CFR in COVID-19 patients. Existing antiviral treatments such as lopinavir/ritonavir and remdesivir have been evaluated and used for treating SARS-CoV and MERS-CoV infections [29,30]. They are also considered for the treatment of COVID-19 infections [21]. Clinical trials with large patient sample should be carefully designed and implemented to assess their efficacies.
This meta-analysis has several potential limitations. Firstly, there are only two retrospective cohort studies included, and more studies with larger sample should be conducted to investigate this issue. Secondly, there is significant heterogeneity for occupation, severity and time period, which may be caused by different definition of occupation, severe cases and different patient population in the three time periods. Thirdly, there may be some repetitive data in these two studies, which may have some influence on the pooling results. Fourthly, there may be some confounding relationship between the occupation of retiree and age, but it is not available to adjust the occupation of the retiree by age based on current limited data.
In conclusion, this study reveals the several factors including age ≥ 60, sex of male, occupation of retirees and severe cases can substantially increase the CFR in patients with COVID-19. These findings are of crucial importance for timely treatment and good prognosis of these patients.
Data availability statement
All relevant data are within the manuscript.
Funding
ZJQ was funded by the Foundation of The First Affiliated Hospital of Chongqing Medical University (PYJJ2019–06, https://www.cqmu.edu.cn/) and Natural Science Foundation of Chongqing(cstc2019jcyj-msxmX0281, http://www.csti.cn/govwebnew /). ZJQ conducted the study design, data collection and analysis, decision to publish, and preparation of the manuscript.
Contributors
Jinqiu Zhao and Xiaosong Li conducted the design, Junyi Zheng and Wenxiang Huang conducted the study planning, data analysis and data interpretation, Junyi Zheng and Junyi Zheng wrote and revised the article. All authors read and approved the final manuscript.
Declaration of Competing Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs).
Acknowledgments
None.
References
- 1.Hui D.S., Azhar E.I., Madani T.A., Ntoumi F., Kock R., Dar O. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 Novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections—more than just the common cold. JAMA. 2020 doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 3.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang R., Liu H., Li F., Zhang B., Liu Q., Li X. Transmission and epidemiological characteristics of novel coronavirus (2019-nCoV)-infected pneumonia (NCIP): Preliminary evidence obtained in comparison with 2003-SARS. medRxiv. 2020 [Google Scholar]
- 6.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan J.F.-W., Yuan S., Kok K.-H., K.K.-W. To, Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phan L.T., Nguyen T.V., Luong Q.C., Nguyen T.V., Nguyen H.T., Le H.Q. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382(9):872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang H., Kang Z., Gong H., Xu D., Wang J., Li Z. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. bioRxiv. 2020 [Google Scholar]
- 14.Benvenuto D., Giovannetti M., Ciccozzi A., Spoto S., Angeletti S., Ciccozzi M. The 2019-new coronavirus epidemic: evidence for virus evolution. J Med Virol. 2020;92(4):455–459. doi: 10.1002/jmv.25688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan J.F.-W., Kok K.-H., Zhu Z., Chu H., K.K.-W. To, Yuan S. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerging Microb Infect. 2020;9(1):221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guan W.-j., Ni Z.-y., Hu Y., Liang W.-h., Ou C.-q., He J.-x. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. 2020 2020.02.06.20020974. [Google Scholar]
- 18.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J.Y., Choe P.G., Oh Y., Oh K.J., Kim J., Park S.J. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020;35(5) doi: 10.3346/jkms.2020.35.e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang S., Xia S., Ying T., Lu L. A novel coronavirus (2019-nCoV) causing pneumonia-associated respiratory syndrome. Cell Mol Immunol. 2020;17(5) doi: 10.1038/s41423-020-0372-4. 554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang Y., Lu Q., Liu M., Wang Y., Zhang A., Jalali N. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. medRxiv. 2020 2020.02.10.20021675. [Google Scholar]
- 24.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 25.T.N.C.P.E.R.E. Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. ChinJ Epidemiol. 2020;41(02):145–151. [Google Scholar]
- 26.Wang X.F., Shi G.C., Wan H.Y., Hang S.G., Chen H., Chen W. Clinical features of three avian influenza H7N 9 virus-infected patients in S hanghai. Clin Respir J. 2014;8(4):410–416. doi: 10.1111/crj.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu W.J., Zhao M., Liu K., Xu K., Wong G., Tan W. T-cell immunity of SARS-CoV: implications for vaccine development against MERS-CoV. Antiviral Res. 2017;137:82–92. doi: 10.1016/j.antiviral.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao Y., Zhao Z., Wang Y., Zhou Y., Ma Y., Zuo W. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv. 2020 doi: 10.1164/rccm.202001-0179LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chu C., Cheng V., Hung I., Wong M., Chan K., Chan K. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax. 2004;59(3):252–256. doi: 10.1136/thorax.2003.012658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sheahan T.P., Sims A.C., Leist S.R., Schäfer A., Won J., Brown A.J. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. 2020;11(1):1–14. doi: 10.1038/s41467-019-13940-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript.