Abstract
Background
Preeclampsia is a complex syndrome that is considered a disorder specific to pregnancy. However, research indicates that diffuse maternal endothelial damage may persist after childbirth. On the other hand, women who had a history of pre-eclampsia are at an increased risk of vascular disease. Considering that the multifactorial nature of pre-eclampsia in a remote health setting, knowledge of risk factors of preeclampsia gives epidemiological significance specific to the study area. Therefore, this study aimed to identify the determinants of preeclampsia among pregnant women attending perinatal service in Omo district Hospitals in southern Ethiopia.
Methods
An institution-based unmatched case-control study design was conducted among women visiting for perinatal service in Omo District public hospitals between February to August 2018. A total of 167 cases and 352 controls were included. Data were collected via face-to-face interviews. Bivariable and multivariable logistic regression analysis were computed to examine the effect of the independent variable on preeclampsia using Statistical Package for Social Sciences version 26 window compatible software. Variables with a p-value of less than 0.05 were considered statistically significant.
Results
Factors that were found to have a statistically significant association with pre-eclampsia were primary relatives who had history of chronic hypertension (AOR 2.1, 95% CI: 1.06–4.21), family history of diabetes mellitus (AOR 2.35; 95% CI: 1.07–5.20), preterm gestation(AOR = 1.56, 95%CI, 1.05–2.32), and pre-conception smoking exposure (AOR = 4.16, 95%CI, 1.1–15.4).
Conclusions
The study identified the risk factors for pre-eclampsia. Early detection and timely intervention to manage pre-eclampsia, and obstetric care providers need to emphasize women at preterm gestation and a history of smoking before pregnancy.
Keywords: Pre-eclampsia, Hospitals, Determinants, Women, Ethiopia
Background
Pre-eclampsia is a unique form of life-threatening medical disorder that is clinically characterized by an elevated systolic blood pressure greater than or equal to 140 mmHg or diastolic blood pressure greater than or equal to 90 mmHg, on two occasions at least 4 h apart in a previously normotensive woman, proteinuria, or the presence of severity sign [1–3], new onset of visual disturbance, pulmonary edema, and thrombocytopenia (platelet count< 100,000/μL).
The cause of pre-eclampsia is still unknown [4]. Nevertheless, the pathogenesis of different pre-eclampsia phenotypes has not been completely elucidated [5]. Research indicates that arterial stiffness indices were found to be elevated among women who had pre-eclampsia before 34 weeks compared to normotantive mothers. This indicated that women who develop pre-eclampsia at earlier gestation exhibit impaired endothelial dysfunction [6, 7]. If detection is delayed, it progresses into a multi-organ dysfunction is more evident [8]. Recent update on preeclampsia indicates that multiple maternal organ dysfunction includes renal insufficiency, hepatic involvement, neurological or hematological complications, uteroplacental dysfunction, or fetal growth restriction may be resulted from severe preeclampsia [9].
Pre-eclampsia occurs in 3–5% of pregnancies [10]. The WHO (World Health Organization) report indicates that about 20 to 40% and 11 to 37% of pre-eclampsia occurs in women who had earlier exposure to pre-eclampsia [11]. Despite the efforts that have been made to prevent, diagnose, and manage pre-eclampsia, it continues to become a major public health problem [9, 12]. An annual report indicated that pre-eclampsia alone accounts for 70, 000 maternal deaths [13]. In women with pre-eclampsia, the risk of fetal morbidity and mortality was found to be high; indeed, it was the major cause of stillbirth and early neonatal death [14]. In Ethiopia, pre-eclampsia alone attributes 16% of pregnancy-related deaths. A report revealed an increasing trend of maternal morbidity and mortality due to pre-eclampsia [6]. Besides, it has healthcare implications for women who have preeclampsia are at increased risk of chronic illness later in life [15]. In low-income countries, especially in sub-Saharan African countries, under-reporting influences the preventive measure to lowers the burden of the disease [16].
The common factors that have been suggested to increase the risk of pre-eclampsia among women include pre-existing chronic illnesses, excessive weight gain, primiparity, advanced maternal age, first or second-degree relatives with a history of pre-eclampsia, and other environmental genetic related factors [17–19]. However, there is no single excellent factor to predict pre-eclampsia [20–22]. Although it is an inexpensive and quick way to predict the occurrence of pre-eclampsia [23, 24], in a developing nation, further investigation and validation of the existing evidence are helpful.
However, those that have been conducted have often had inadequate controls and smaller sample sizes or were not adjusted for potential confounders [18, 25, 26], this could mask the finding of previous studies. In Ethiopia, a mortality analysis conducted on mothers during the perinatal period has revealed that the new onset of pre-eclampsia has increased [6]. Therefore, this study aimed to identify the determinants of pre-eclampsia in women attending perinatal services in hospitals of Omo district, Southern Ethiopia.
Methods
Study area and period
A facility-based unmatched case-control study design was conducted in Omo districts in six public hospitals from February to August 2018. Based on the national 2007 census, the district houses an estimated total population of more than five and a half million [27]. The source population for this study was all women attending labor and delivery services in Arbaminch General, Konso district, Sawla district, Chencha district, Jinka General, and Gidole district hospitals. Data were collected from randomly selected pregnant women attending antenatal and delivery in all hospitals.
Inclusion criteria
Cases were defined in two alternative ways. First, when a woman was confirmed to have an elevated blood pressure of 140/90mmHG, measured at rest or 5 min after arrival, was detected at least 4 to 6 h apart. Plus, a urine dipstick value of 2+ proteinuria and/or two random urine concentrations of 100 mg/dl collected 4 h apart after 20 completed weeks of gestation in a previously normotensive client [28], (Table 1).
Table 1.
Diagnostic criteria used for the study on determinants of pre-eclampsia among women attending hospitals in Omo district, Southern Ethiopia, 2018
| Diagnostic criteria for pre-eclampsia [28] | |
|---|---|
| The onset of symptoms after 20 weeks’ gestation with remission by 6–12 weeks postpartum* | |
| Mild pre-eclampsia: | |
| • Hypertension (Systolic Blood Pressure(SBP) ≥ 140 mmHg or Diastolic Blood Pressure(DBP) ≥ 90 mmHg), may be superimposed on chronic hypertension | |
| • Proteinuria (proteinuria ≥300 mg/24 h, or significant increase from baseline) | |
| Severe pre-eclampsia if one or more of the following: | |
| • Sustained Systolic Blood Pressure(SBP) ≥ 160 mmHg or Diastolic Blood Pressure(DPB) ≥ 110 mmHg (measured twice, at least 6 h apart) | |
| • Evidence of other end-organ damage | |
| • Deteriorating renal function including nephrotic range proteinuria ≥3 g/24 h or 3+ on urine dipstick or sudden oliguria, especially with elevated creatinine† | |
| • Central Nervous System(CNS) disturbance (altered vision, headache) | |
| • Pulmonary edema (3% of patients) | |
| • Liver dysfunction | |
| • Epigastric/right upper quadrant pain (stretching of hepatic capsule) | |
| • Thrombocytopenia (15–30% of patients) | |
| • HELLP syndrome is characterized by Hemolysis Elevated Liver enzymes and Low platelet count which may occur without proteinuria. | |
| • Evidence of fetal compromise (Intrauterine Growth Restriction-IUGR, oligohydramnios, non-reasoning fetal testing) |
Second, if the urine dipstick value became negative, the data collector also asked for the presence of severity signs. Women with elevated blood pressure and having one of the following symptoms (severe fronto-occipital headache unresponsive to antipain, right upper quadrant tenderness, epigastric pain, oliguria, upper extremity edema, facial edema, and blurring of vision) were used as an alternative to diagnose pre-eclampsia. Only if it was confirmed by a physician.
For new cases, the data collector had observed for proper measurement of blood pressure (using different parameters such as checking the functionality of the blood pressure apparatus, the tightness of the cuff comfortably over the study participant’s arm, the lower edge of the cuff was 2–3 cm above the elbow line, and whether the patient’s arm was at the level of the heart.
Controls were a woman with other cases after 20 completed weeks of gestation and who were not diagnosed with pre-eclampsia. All cases and controls were observed by the physician in the hospitals.
Exclusion criteria
To make the study comparable, women who were not from Omo districts were excluded. In this study, women with severe medical conditions and who could not confer informed consent and with known hypertension and renal disease status were excluded from the study.
Sample size determination
EPI INFO version 7.2 was used to compute the sample size using the double population proportion formula by assuming student occupation as a risk factor with an odds ratio of 2.65 and 5.79% among controls and exposed from the literature reviewed [29]. With corresponding assumptions of the 95% confidence interval, 5% marginal error, and 80% power, the calculated sample size was 494. Considering 5% possible non-respondents, the final sample size of 519(167 cases and 352 controls) was estimated.
Sampling techniques and procedures
All hospitals in Omo district, such as Konso primary Hospital, Arbaminch, and Jinka General Hospitals, Chencha, Gidole, and Sawla District Hospitals, were selected purposely because of a small number of cases. For each identified hospitals, proportional to size allocation based on previous year hospital reports in a similar period of the study was considered to estimate the target population. However, due to the limited number of cases, all women who fulfilled the inclusion criteria were taken to be compared with systematically addressed controls.
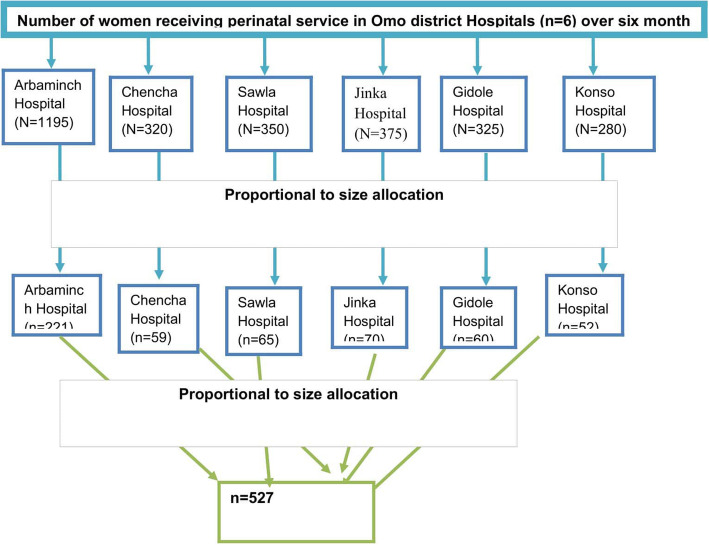
According to the 2017 annual report, the average number of women who had attended perinatal service per month was 478, 128, 150, 130, 112, and 140 in Arbaminch General Hospital, Chencha General Hospital, Jinka Hospital, Gidole Hospital, Konso Hospital, and Sawla hospitals, respectively, (Fig. 1). Considering the average number of pregnant women attending perinatal service per day in each hospital, control were selected using a systematic random sampling technique immediately.
Fig. 1.
Pictorial presentation of women enrolled for a case control study on determinants of pre-eclampsia among pregnant women, Omo district hospitals,southern Ethiopia
Data collection procedure
Data were collected using a pre-tested, structured, and interview administered questionnaire. Besides, Patient cards were also reviewed further for the variables listed in the diagnostic criteria and to extract laboratory investigation results. The questionnaire encompasses different parts of questions related to socio-demographic variables, obstetric, medical, and behavioral-related variables. All the aforementioned variables were adopted by referring to different scholarly articles [30–38]. The questionnaires were prepared in English, translated into Amharic (Federal Government Working Language), and then translated back to English by a language expert to keep uniformity. Twelve fluent Amharic speaking Bachelor degree midwives from the health center of each town were used as data collectors. Upon arrival at the data collection site, the enumerator identified the case from antenatal and delivery booking. Then, it was cross-checked for the assurance of the diagnosis by the duty physician. The data collector also had a duty to crosscheck the diagnosis with the case definition used for this study, particularly for newly diagnosed ones.
Data were collected after the women stabilized(within 4 to 6 h of childbirth) and comfortable to respond. Six general practitioners (medical doctor) supervisors supervised the entire data collection in coordination with the principal investigator. The principal investigator coordinated the data collection team and give the necessary support. After the pre-test, the questionnaire was corrected for illogically ordered and some ambiguous and miss-leading terminologies.
Data quality assurance
Data collectors were trained on the purpose of the study, selection of exposed and unexposed, how to keep confidentiality of patient information, the contents of the questionnaire, and data quality management by the principal investigators. The training was based on the guide that was developed for clarifying the interview administered questionnaires.
Throughout data collection, the supervisors checked the questionnaire for completeness, clarity, and consistency daily. The data collectors were oriented to correct missing data before the discharge of the patient from the hospital. Fully completed data with a few missing items were coded and duly reported to the investigator. The reliability coefficient of the tool was checked and it was 0.76. Data were entered by a trained and experienced clerk on a priory created Epi-info template.
Data management, analysis, and interpretation
The collected data were cleaned, coded, and entered into Epi-Info version 7.2 and exported to SPSS version 26.0 for further analysis. The frequency was checked to see the accuracy, consistency, variables, and missed values. Descriptive statistics were computed and used to describe the study population using tables compared between cases and controls.
Binary and multivariable logistic regression models were fitted to identify the association between explanatory and outcome variables. Variables with a p-value of less than 0.20, biological plausibility, and previous study findings were considered for inclusion in the multivariable logistic regression analysis where confounders can be controlled. Multicollinearity was checked among independent variables using a variance inflation factor.
The necessary assumptions of logistic regression were made by checking Hosmer and Lemeshow goodness of fit test statistics. Variables with a p-value of less than 0.05 in the multivariable logistic regression analysis were considered as a statistically significant determinant. The adjusted odds ratio with the 95% CI was calculated to measure the strength of the association between the explanatory variables and the outcome variable.
Results
Socio-demographic characteristics of the study participants
A total of five hundred twenty-seven women were enrolled. Nine of the items had missed important variables, this gives a response rate of 98.3%. The mean age of the patients was 25 years with SD (±5.5). The majority of 110(65.9%) of cases were between 20 and 34 years of age, followed by 45(26.9%) of cases whose ages less than 20 years. The majority of 236 (67.3%) of the control groups fell in these age groups. More than 161(96%) and 234(66%) cases and controls were married. Regarding educational status, the majority of the cases (28.14%) and 30.2% of controls had completed primary education. Nearly one-fourth of cases (28.1%) and 25.3% of controls had higher education. Ninety-three 55.7% of cases were housewives compared to one hundred eighty controls, on which they had a similar role (Table 2).
Table 2.
Sociodemographic characteristics of women attending public health hospitals in Omo District for antenatal and delivery services, Southern Ethiopia, 2018 (n = 519)
| Variables |
Case n = 167 |
Control n = 352 |
P-value | ||
|---|---|---|---|---|---|
| Age | No | % | No | % | |
| Less than 20 | 45 | 26.9 | 80 | 22.7 | 0.19 |
| 20–34 | 110 | 65.9 | 237 | 67.3 | 0.39 |
| Above 34 | 12 | 7.2 | 35 | 10 | 1:00 |
| Marital status | |||||
| Married | 161 | 96.4 | 325 | 92.3 | 0.08 |
| Unmarried | 6 | 3.6 | 27 | 7.7 | 1:00 |
| Residence | |||||
| Urban | 89 | 53.3 | 201 | 57.1 | 0.41 |
| Rural | 78 | 46.7 | 151 | 42.9 | 1:00 |
| Educational Status | |||||
| No formal education | 41 | 24.6 | 77 | 21.9 | 1:00 |
| Primary | 47 | 28.0 | 106 | 30.1 | 0.48 |
| Secondary | 39 | 23.4 | 97 | 27.6 | 0.30 |
| College and above | 40 | 24.0 | 72 | 20.4 | 0.88 |
| Religion | |||||
| Orthodox | 85 | 50.9 | 180 | 51.1 | 0.14 |
| Protestant | 66 | 39.5 | 142 | 40.3 | 0.10 |
| Muslim | 9 | 5.4 | 24 | 6.9 | 0.11 |
| Others | 7 | 4.2 | 6 | 1.7 | 1:00 |
| Maternal Occupation | |||||
| Housewife | 94 | 56.3 | 180 | 51.1 | 0.47 |
| Merchant | 26 | 15.6 | 49 | 13.9 | 0.49 |
| Gov’t employee | 15 | 8.9 | 49 | 13.9 | 0.67 |
| Private worker | 8 | 4.8 | 25 | 7.1 | 0.76 |
| Student | 16 | 9.6 | 28 | 8.0 | 0.44 |
| Others | 8 | 4.8 | 21 | 6.0 | 1:00 |
| Paternal Occupation | |||||
| Gov’t employee | 45 | 22.8 | 98 | 29.63 | 0.30 |
| Merchant | 43 | 33.5 | 114 | 28.77 | 0.13 |
| Farmer | 59 | 31.7 | 96 | 29.10 | 0.74 |
| Private | 8 | 6.6 | 27 | 6.84 | 0.12 |
| Others | 12 | 5.4 | 17 | 5.70 | 1:00 |
Personal and family history-related characteristics
In this study, approximately 24% of patients had a family history of chronic hypertension compared to 16.8% of controls. Regarding the family history of diabetes mellitus, cases and controls had only a 3% difference, where 7.2% [11] and 10% [29] of the cases and controls had a family history of diabetes mellitus, respectively. On the other hand, the difference in the percentage of the personal history of diabetes mellitus during the last pregnancy in both cases and controls was not significant. Approximately 7 and 5% of cases and controls had diabetes mellitus during the last pregnancy, respectively. Similarly, the proportion of patients who had asthma during their last pregnancy had a 2.1 difference. Regarding the personal history of severe pre-eclampsia or eclampsia, 24(14.4%) were accounted for cases while 34(9.7%) of the controls had symptoms due to the preceding confirmed diagnosis of pre-eclampsia (Table 3).
Table 3.
Personal and family history-related characteristics of women attending public health hospitals in Omo District for antenatal and delivery services, Southern Ethiopia, 2018 (n = 519)
| Variables |
Case n = 167 |
Control n = 352 |
P-value | ||
|---|---|---|---|---|---|
| Family history of hypertension | No | % | No | % | |
| No relatives history | 126 | 75.4 | 293 | 83.3 | 1:00 |
| 1st degree relatives history | 19 | 11.4 | 23 | 6.5 | 0.05 |
| 2nd degree relatives history | 22 | 13.2 | 36 | 10.2 | 0.23 |
| Family history of Diabetes Mellitus | |||||
| Yes | 12 | 7.2 | 35 | 9.90 | 0.31 |
| No | 155 | 92.8 | 317 | 90.1 | 1:00 |
| Personnel history of Diabetes Mellitus | |||||
| Yes | 11 | 6.6 | 19 | 5.4 | 0.59 |
| No | 156 | 93.4 | 333 | 94.6 | 1:00 |
| Personel history of Asthma | |||||
| Yes | 13 | 7.8 | 20 | 5.7 | 0.36 |
| No | 154 | 92.2 | 332 | 94.3 | 1:00 |
| Personel history of Pre-eclampsia | |||||
| Yes | 24 | 14.4 | 34 | 9.7 | 0.11 |
| No | 143 | 85.6 | 318 | 90.3 | 1:00 |
Reproductive-related characteristics
More than half (50.3%) of the cases had a history of pregnancy twice comparable to 57.3% of controls. The difference in the proportion of cases and controls was equivalent to 1%. Most of the 68.9 of cases and 57.8% of the controls had preterm birth before the data collection period. The number of having had ANC follow-up at least ones during the last pregnancy was 31.7% among cases with new ANC follow-up, while it became 34.5% in controls (Table 4).
Table 4.
Obstetric characteristics of women attending public health hospitals in Omo District for antenatal and delivery services, Southern Ethiopia, 2018 (n = 519)
| Variable | Case (n = 167) | Control (n = 352) | P-value | ||
|---|---|---|---|---|---|
| No | % | No | % | ||
| Gravidity | |||||
| Primigravida | 71 | 42.5 | 127 | 36.2 | 0.12 |
| Multigravida | 84 | 50.3 | 187 | 57.3 | 0.32 |
| Gravid multi-gravida | 12 | 7.2 | 38 | 10.5 | 1:00 |
| Number of gestation | |||||
| Singleton | 156 | 93.4 | 326 | 92.9 | 0.74 |
| Multiple | 11 | 6.6 | 26 | 7.1 | 1:00 |
| Gestational Age | |||||
| Less than 37 weeks | 115 | 68.9 | 201 | 57.3 | 0.01 |
| 37 and above weeks | 52 | 31.1 | 151 | 42.7 | 1:00 |
| ANC follow up | |||||
| New | 53 | 31.7 | 121 | 34.5 | 0.55 |
| Repeated | 114 | 68.3 | 232 | 65.5 | 1:00 |
| Pregnancy interval | |||||
| No interval | 63 | 37.7 | 115 | 32.7 | 0.13 |
| Less than 2 yrs. | 33 | 19.8 | 58 | 16.5 | 0.16 |
| 2 years and above | 71 | 42.5 | 179 | 50.9 | 1:00 |
| Abortion | |||||
| Yes | 31 | 18.6 | 69 | 19.7 | 0.78 |
| No | 136 | 81.4 | 283 | 80.3 | 1:00 |
| Contraceptive before conception | |||||
| No modern contraception used | 88 | 52.7 | 178 | 50.7 | 1:00 |
| Injectable | 53 | 31.7 | 104 | 29.5 | 0.89 |
| Long acting reversible | 17 | 10.2 | 49 | 13.9 | 0.25 |
| Oral pills | 9 | 5.4 | 22 | 5.9 | 0.73 |
| Conception from a new partner | |||||
| Yes | 34 | 20.4 | 66 | 18.8 | 0.66 |
| No | 133 | 79.6 | 286 | 81.2 | 1:00 |
| Counseling during pregnancy | |||||
| Yes | 148 | 88.6 | 327 | 93.2 | 0.11 |
| No | 19 | 11.4 | 25 | 6.8 | 1:00 |
| Body Mass Index | |||||
| Underweight | 18 | 10.8 | 22 | 6.2 | 1:00 |
| Normal | 100 | 59.9 | 230 | 65.3 | 0.06 |
| Overweight | 42 | 25.1 | 94 | 26.8 | 0.10 |
| Obese | 7 | 4.2 | 6 | 1.7 | 0.58 |
Behavioral and nutritional related characteristics
It was indicated that the percentage of cases who had a history of smoking before conception was 4.2%. Concerning alcohol intake during pregnancy, 48(28.7%) of cases and 89(25.4%) controls had consumed at least once. The majority, (110[65.9%] of cases and 239[68.1%] of controls had taken a cup of coffee during their course of pregnancy at least. More than 92% of both cases and controls had a habit of snack fruit while they were pregnant. Similarly, 158(94.6%) cases and 342(97.4%) controls were taken as green leafy vegetables at least once during their pregnancy. A habit to have non-strenuous physical exercise during pregnancy was responded, 83(49.7%) of cases, and 174(49.6%) controls were engaged in non-strenuous physical exercise during pregnancy.
Determinants of preeclampsia identified
Degree of relatives with history of diabetes mellitus, gravidity, sesonality and habit of green leaf vegetable intake during antenatal follow-up were not incorporated in the multivariable analysis due to colleniearity. In model one, a family history of hypertension, women with a history of smoking before pregnancy, and a family history of diabetes were variables that found to have a significant statistical association with pre-eclampsia. However, marital status and personal stories of hypertension showed no association with pre-eclampsia. In the second model, similar variables with model one remained to have a significant statistical association with pre-eclampsia together with gestational age.
Primary relatives who had history of chronic hypertension were more than two times at increased risk for developing preeclampsia (AOR 2.1, 95% CI: 1.06–4.21).
The probability of developing preeclmpsia among women with family history of diabetes mellitus increases more than twice (AOR 2.35; 95% CI: 1.07–5.20).
Referring to gestational age at delivery, the odds of having preeclampsia increased among women who had preterm gestation(AOR = 1.56, 95%CI, 1.05–2.32) and pre-conception smoking exposure (AOR = 4.16, 95%CI, 1.1–15.4) (Table 5).
Table 5.
Bivariable and multivariable analysis on determinants of pre-eclampsia women attending public health hospitals in Omo District for antenatal and delivery services, Southern Ethiopia, 2018 (n = 519)
| Variable | Outcome variable | COR-95% Confidence Interval | AOR-95% Confidence Interval | P-value | |
|---|---|---|---|---|---|
| Pre-eclampsia | Controls | ||||
| Family History of hypertension | |||||
| No family history® | 126(75.4%) | 293(83.3%) | 1:00 | 1:00 | – |
| 1st degree relatives history | 19(11.4%) | 23(6.5%) | 1.92(1.01–3.65) | 2.11(1.06–4.21) | 0.03 |
| 2nd degree relatives history | 22(13.2%) | 36(10.2%) | 1.42(0.80–2.51) | 1.42(0.78–2.58) | 0.26 |
| Personel History of Preeclampsia | |||||
| Yes | 24(14.4%) | 34(9.7%) | 1.6(0.89–2.74) | 0.59(0.32–1.09) | 0.09 |
| No® | 143(85.6%) | 318(90.3%) | 1:00 | 1:00 | |
| Family History of Diabetes Mellitus | |||||
| Yes | 12(7.2%) | 35(9.90%) | 0.70(0.35–1.13) | 2.35(1.07–5.20) | 0.03 |
| No® | 155(92.8%) | 317(90.1%) | 1:00 | 1:00 | |
| Marital Status | |||||
| Married | 161(96.4%) | 325(92.3%) | 2.23(0.90–5.51) | 2.28(0.90–5.77) | 0.08 |
| Unmarried® | 6(3.6%) | 27(7.7%) | 1:00 | 1:00 | |
| Gestational age | |||||
| Less than 37 weeks | 115(68.9%) | 201(57.3%) | 1.7(1.13–2.45) | 1.56(1.05–2.32) | 0.03 |
| 37 and Above weeks® | 52(31.1%) | 151(42.7%) | 1:00 | 1:00 | – |
| History of Smoking before pregnancy | |||||
| No® | 96(57.5%) | 216(61.4%) | 1:00 | – | |
| Passive smoker | 64(38.3%) | 132(37.5%) | 1.09(0.74–1.60) | 1.14(0.77–1.67) | 0.51 |
| Active smoker | 7(4.3%) | 4(1.14%) | 3.94(1.13–13.8) | 4.16(1.12–15.4) | 0.03 |
Note:®-reference
Discussion
This study aimed to assess socio-demographic, medical disease, obstetric history, and behavioral determinants of pre-eclampsia. We found that having preterm gestation, and a history of smoking appeared to be a risk factor for pre-eclampsia.
A population-based study reported that preeclampsia has a strong familial tendency [39]. As a single gene hypothesis indicated, it remains an interplay of multiple factors where the effect of close relatives can be considered [40]. Besides, different scholars had tempted to characterize maternal predisposition because of genetic inheritance [41–43]. For instance, a daughter born from a pre-eclamptic mother may carry the risk for a genetic predisposition in which a gene from parents operate during uterine life through the offspring [34, 42].
Further, relatives who were not born after a pregnancy complicated by preeclampsia carries more risk [44, 45]. But, women born from mothers with the previous episode of preeclampsia were more likely to trigger severe preeclampsia in their pregnancy [41]. A stronger genetic predisposition may explain the clinical severity of preeclampsia [46]. Besides, strong single gene expression from the maternal side has more influence on preeclampsia than its relationship to the fetal association.
Like other studies [47, 48], this research has found a positive association with a family history of chronic hypertension and diabetes mellitus. In this study, women with a previous family history of hypertension and diabetes Mellitus had more than twice more likely to develop pre-eclampsia, respectively. Many population-based studies found a significant statistical association between pre-eclampsia and family history of chronic hypertension and diabetes mellitus. This finding is in line with studies conducted in Brazil [49], Sudan [50], Pakistan [51], Sweden [52], and Uganda [53]. Recent studies done during pregnancy noted that diabetes mellitus may involve in the development of preeclampsia in which insulin resistance may play a role in the cause of preeclampsia [54]. Several other studies revealed that women with a family history of diabetes mellitus were more likely to develop preeclampsia [38, 55–57]. It shows that family history of diabetes mellitus could be a considerable risk factor of preeclampsia.
This study showed that women at earlier gestations are at an increased risk of pre-eclampsia. Preterm gestational age attributes a higher probability of developing a severe form of pre-eclampsia than the later gestational age. This finding of this result is consistent with another study [58]. This is supported by several research findings [59, 60], in which women with PTB reported as a factor to develop PE as evidenced by many systemic inflammatory markers that appeared positive in this particular group.
Besides, an excess risk of preeclampsia was seen in women with recurrent preterm birth [58, 61]. Several other studies have suggested that early-onset and late-onset pre-eclampsia, often termed mild and severe pre-eclampsia, maybe two different entities with different causes [9, 46, 62], whereas others suggest that the risk profiles are similar for these groups [63]. In this study preterm birth was significantly higher in women with preeclampsia than without. It was indicated that 68.9% of women who had preeclampsia gave birth before 37 weeks of gestation than 57.3% of women without preeclampsia. Similar findings were observed in different parts of the world such as China [64] and Porchugese [65]. For example, a study conducted in China indicated that the difference in the rate of preeclampsia among preterm births were more than 22% compared to those without. This is supported because the risk of pre-eclampsia is inversely correlated with gestational age; the closer the gestation to 20 weeks, the more pregnant women could develop pre-eclampsia [66]. This is evidenced by a hypothesis that a common pathophysiologic mechanism, suggesting that a significant proportion of preterm births are caused by improper remodeling of the uterine spiral arteries, in earlier gestation pre-eclampsia may happen for a similar reason [67].
Another possible reason why pre-term gestation is a factor for PE may be that both conditions are due to generalized systemic inflammation, which could lead to endothelial dysfunction [68, 69]. However, it has to be underlined that neither has the possible cause and effect relationship exists between preterm gestation and preeclampsia.
Statistically speaking, our data suggest that ceasing smoking before conception did alter the risk of pre-eclampsia. Women who quit smoking before pregnancy were more than three times more likely to exhibit preeclampsia. In support of this, women who stopped smoking before pregnancy had an increased risk of pre-eclampsia compared to those who never did [70, 71]. On the other hand, women who had previous smoking exposure before pregnancy compared to non-smokers were about six times more likely to develop pre-eclampsia [72]. Research has also speculated that the probability of developing hypertension was increased among women whose ages were above 35 years [73].
The underlying mechanism that increased the risk of pre-eclampsia among women who smoked before pregnancy remains unclear. Evidence indicates that the absence of a temporary protective factor-like carbon monoxide due to low tobacco exposure could be the possible reason [72].
Evidence indicated that smoking has associated with endothelial-dependent vascular dilation [74, 75]. A decreased mRNA and protein expression of the Nitric oxide synthase activity in endothelial cells are the suggested mechanism in research from preeclamptic pregnancies [76, 77]. Women who smoke before conception may have lower nitric oxide levels [78], leads to increased vascular tension, smoking may act through this mechanism to increase the risk of preeclampsia.
Moreover, preeclamptic women have reported having more release of syncytiotrophoblastic cellular particles and syncytial cellular debris in maternal circulation, this could result from endothelial dysfunction [79–81]. In the placentas of preeclamptic women, the rate of syncytiotrophoblastic proliferation and apoptosis is higher [82]. In women with smoking exposure before conception, it has reported that an increased focal syncytial apoptosis, cytotrophoblastic hyperplasia, loss or distortion of the placental barrier, decreased syncytial pinocytotic vessels, loss of the microvilli, decreased degeneration of cytoplasmic organelles, and increased collagen in the vascular stroma are related with preeclampsia [83–86]. Evidence of syncytial damage, knots, and focal necrosis is higher in smokers [84].
Any understanding must consider the multifactorial and complex nature of pre-eclampsia pathogenesis involving genetic, environmental, and immunologic related factors. Although there is much evidence in favor of this finding, due to the smallness of cases reported smoking [26, 53], But, the association between smoking and preeclampsia should be interpreted consciously. As smoking before conception is subject to recall bias, misreporting is likely. In this regard, the true effect of smoking on preeclampsia may be masked [87, 88].
Strengths of the study and limitations of the study
We used a clear, understandable, variety of diagnostic criteria to make the diagnosis of pre-eclampsia more accurate. We triangulate observations with a patient card review for a detailed overview of the information needed to reach the diagnosis, other than a senior physician consultation, was used. Also, we take all cases attending the hospitals included in this study during the study period.
However, we were unable to evaluate the risk of pre-eclampsia with some factors such as maternal physical activity during pregnancy, length of the sexual relationship after marriage, mechanical contraceptives before conception, and paternal smoking. Evidence indicates that there is no relationship between paternal smoking and hypertension [89].
Regardless of the findings in this study, research speculated that women who had a history of smoking with preeclampsia cause a significant adverse perinatal outcome [90]. Therefore, a pregnant woman should be advised to quit smoking. However, better awareness of the mechanism by which smoking affects the pathogenesis of preeclampsia may give insight into the upcoming therapeutic measures planned to be considered.
Considering that six hospitals in this study make the study population heterogeneous, therefore the results may not be reflective of the real condition, particularly for each setting. Besides, this study did not consider hospitals as a factor, and there may be a difference in care provision. Thus, this has to be noted for future work.
We did not consider women who might develop pre-eclampsia after 48 h to 6 weeks after delivery for two reasons. First, it was difficult to trace women after discharge because most of them had their post-partum care visits at the health center. Second, women may be delayed both from home to the health center and during referral; therefore, they may develop eclampsia fits by the time they had arrived at the hospital, which was not incorporated in this study. Due to logistic reasons, we needed to focus on pre-eclampsia alone.
Conclusions
This study revealed that women with first degree relatives who had history of chronic hypertension, family history of diabetes mellitus, preterm gestation, and pre-conception smoking exposure were variables statistically significant determinants of pre-eclampsia in the Omo district hospitals.
Identification of women who had close relatives with history of chronic hypetenion and diabetes mellitus would be helpful in the diagnosis, monitoring, and timely mangment of women preeclampsia and its complications.
Clinicians could prompt pregnant women to avoid smoking exposure before pregnancy recognition and address barriers to perinatal care adherence during pregnancy. Besides, planning and monitoring clients are given the impact of smoking, and prematurity on pre-eclampsia could be addressed through community-based health education. Researchers should have the insight to conduct further studies on the link between smoking and pre-eclampsia.
Carefully examine preterm gestation and suspected cases of pre-eclampsia, detect and intervene as timely as possible. Working to provide enthusiastic counseling for a woman found to have a smoking history holistically may be considered during the perinatal care service provision for pregnant women. Seeking medical advice from trained health-care providers on how to cease smoking is necessary.
Acknowledgments
We appreciate Arbaminch University, College of Medicine and Health Science, Research coordination office for opening the door to conduct research. We are also grateful to the Gamo Goffa health bureau for the willingness made in providing baseline information and relevant documents.
We want to express our indebted to fellows for their constructive comments and ideas. Our sincere heartfelt will go to Mrs. Lauren Smith for her contribution to editing this manuscript voluntarily.
Declarations
We, the undersigned, agree to accept responsibility for the scientific, ethical, and technical conduct of the research project mentioned below and for the provision of required progress reports and financial settlements as per the terms and conditions of the University if the grant is awarded as the result of this application.
Abbreviations
- ANC
Antenatal Care
- AOR
Adjusted Odds Ratio
- BMI
Body Mass Index
- BP
Blood Pressure
- COD
Crude Odds Ratio
- CI
Confidence Interval
- DIC
Disseminated Intravascular Coagulation
- SBP1
Systolic Blood Pressure
- WHO
World Health Organization
Authors’ contributions
KF has a role in the conception, planning, carrying out data collection, analyzing and writing up of the work, and manuscript development. FG, FG, NC, and DM contributed to data collection, editing, and revision of the final manuscript. All authors have read and approved the final manuscript.
Funding
The research reported in this manuscript has been funded by the College of Medicine and Health Sciences Research Coordination Office, Arbaminch University.
Availability of data and materials
On presumable requests, the data sets used for analysis during the current study are available from the corresponding author.
Ethics approval and consent to participate
Ethical approval was obtained from the ethical review committee of the College of Medicine and Health Sciences, Arbaminch University in December 2018 (GOV/AMU/TH.1.1./CMHS/MID/03/2018).
An official letter of cooperation was written to each hospital to get permission. Formal written consent was also obtained from the study participants. Similarly, the participants were informed about the purpose of the study, privacy, and confidentiality issues. Participation was involved only if she said so, she had the right to be off any time she wants to. If she did, the study assures that she had nothing to lose from the service she expected to receive. As if all information gained during data collection was kept confidential and any personal identification was not recorded on the questionnaire. Rather, it was kept under password protection, where the primary investigator had access to.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kassahun Fikadu, Email: kasfika@gmail.com, Email: kassahun.fikadu@amu.edu.et.
Feleke G/Meskel, Email: fgfpeace@gmail.com, Email: feleke.gebremeskel@amu.edu.et.
Firdawek Getahun, Email: getahunfirdawek@ymail.com, Email: firdawek.getahun@amu.edu.et.
Nega Chufamo, Email: negachufa@gmail.com, Email: nega.chufamo@amu.edu.et.
Direslign Misiker, Email: diresmisker@gmail.com, Email: direslgne.misker@amu.edu.et.
References
- 1.SAaGK W. Prevalence and Risk Factors for Symptoms Suggestive of Pre-Eclampsia in Indian. JWHIC. 2014;3(6):2–9. [Google Scholar]
- 2.Duley L, Meher S, Abalos E. Management of pre-eclampsia. BMJ (Clinical research ed) 2006;332(7539):463–468. doi: 10.1136/bmj.332.7539.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstetrics and gynecology. 2013;122(5):1122–31. [DOI] [PubMed]
- 4.Singh HJ. Pre-Eclampsia: is it all in the placenta? Malaysian J Med Sci. 2009;16(1):7–15. [PMC free article] [PubMed] [Google Scholar]
- 5.McNally R, Alqudah A, Obradovic D, McClements L. Elucidating the Pathogenesis of Pre-eclampsia Using In Vitro Models of Spiral Uterine Artery Remodelling. Current Hypertension Rep. 2017;19(11):93. doi: 10.1007/s11906-017-0786-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yinon Y, Kingdom JC, Odutayo A, Moineddin R, Drewlo S, Lai V, et al. Vascular dysfunction in women with a history of preeclampsia and intrauterine growth restriction: insights into future vascular risk. Circulation. 2010;122(18):1846–1853. doi: 10.1161/CIRCULATIONAHA.110.948455. [DOI] [PubMed] [Google Scholar]
- 7.Oylumlu M, Oylumlu M, Yuksel M, Yildiz A, Bilik MZ, Akil MA, et al. A simple method for the assessment of arterial stiffness in pre-eclamptic patients. Clin. Exp. Hypertens (New York, NY : 1993) 2014;36(8):531–537. doi: 10.3109/10641963.2014.913608. [DOI] [PubMed] [Google Scholar]
- 8.LaMarca B. Endothelial dysfunction; an important mediator in the pathophysiology of hypertension during preeclampsia. Minerva Ginecol. 2012;64(4):309–320. [PMC free article] [PubMed] [Google Scholar]
- 9.Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet (London, England) 2005;365(9461):785–799. doi: 10.1016/S0140-6736(05)17987-2. [DOI] [PubMed] [Google Scholar]
- 10.Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ (Clinical research ed) 2013;347:f6564. doi: 10.1136/bmj.f6564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim K-H, Ramus RM. Preeclampsia. 2011. [Google Scholar]
- 12.Ota E, Ganchimeg T, Mori R, Souza JP. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low-and middle-income countries: a WHO secondary analysis. PLoS One. 2014;9(3):e91198. doi: 10.1371/journal.pone.0091198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066–1074. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 14.WHO. Recommendations for Prevention and Treatment of Preeclampsia and Eclampsia: Department of Maternal and Child Health; 2011.
- 15.Bellamy L, Casas J-P, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ (Clinical research ed) 2007;335(7627):974. doi: 10.1136/bmj.39335.385301.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thornton C, Dahlen H, Korda A, Hennessy A. The incidence of preeclampsia and eclampsia and associated maternal mortality in Australia from population-linked datasets: 2000–2008. Am J Obstet Gynecol. 2013;208(6):476. doi: 10.1016/j.ajog.2013.02.042. [DOI] [PubMed] [Google Scholar]
- 17.Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ (Clinical research ed) 2005;330(7491):565. doi: 10.1136/bmj.38380.674340.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee CJ, Hsieh TT, Chiu TH, Chen KC, Lo LM, Hung TH. Risk factors for pre-eclampsia in an Asian population. Int J Gynaecol Obstet. 2000;70(3):327–333. doi: 10.1016/s0020-7292(00)00240-x. [DOI] [PubMed] [Google Scholar]
- 19.Mahomed K, Williams MA, Woelk GB, Jenkins-Woelk L, Mudzamiri S, Madzime S, et al. Risk factors for preeclampsia-eclampsia among Zimbabwean women: recurrence risk and familial tendency towards hypertension. J Obstet Gynaecol. 1998;18(3):218–222. doi: 10.1080/01443619867344. [DOI] [PubMed] [Google Scholar]
- 20.Gabbay-Benziv R, Oliveira N, Baschat A. Optimal first trimester preeclampsia prediction: a comparison of multimarker algorithm, risk profiles and their sequential application. Prenat Diagn. 2016;36(1):34–39. doi: 10.1002/pd.4707. [DOI] [PubMed] [Google Scholar]
- 21.Gallo D, Poon LC, Fernandez M, Wright D, Nicolaides KH. Prediction of preeclampsia by mean arterial pressure at 11-13 and 20-24 weeks' gestation. Fetal Diagn Ther. 2014;36(1):28–37. doi: 10.1159/000360287. [DOI] [PubMed] [Google Scholar]
- 22.Halscott TL, Ramsey PS, Reddy UM. First trimester screening cannot predict adverse outcomes yet. Prenat Diagn. 2014;34(7):668–676. doi: 10.1002/pd.4407. [DOI] [PubMed] [Google Scholar]
- 23.Meads C, Cnossen J, Meher S, Juarez-Garcia A, Ter Riet G, Duley L, et al. Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling. 2008. [DOI] [PubMed] [Google Scholar]
- 24.Leslie K, Thilaganathan B, Papageorghiou A. Early prediction and prevention of pre-eclampsia. Best Pract Res Clin Obstet Gynaecol. 2011;25(3):343–354. doi: 10.1016/j.bpobgyn.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Reyes LM, García RG, Ruiz SL, Camacho PA, Ospina MB, Aroca G, et al. Risk factors for preeclampsia in women from Colombia: a case-control study. PLoS One. 2012;7(7):e41622. doi: 10.1371/journal.pone.0041622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conde-Agudelo A, Belizán JM. Risk factors for pre-eclampsia in a large cohort of Latin American and Caribbean women. BJOG. 2000;107(1):75–83. doi: 10.1111/j.1471-0528.2000.tb11582.x. [DOI] [PubMed] [Google Scholar]
- 27.Development CSA-MoFaE . Ethiopia - Population and Housing Census of 2007. 2007. p. 01. [Google Scholar]
- 28.Practice ACoO Practice bulletin# 33: diagnosis and management of preeclampsia and eclampsia. Obstet Gynecol. 2002;99(1):159–167. doi: 10.1016/s0029-7844(01)01747-1. [DOI] [PubMed] [Google Scholar]
- 29.Grum T, Seifu A, Abay M, Angesom T, Tsegay L. Determinants of pre-eclampsia/Eclampsia among women attending delivery Services in Selected Public Hospitals of Addis Ababa, Ethiopia: a case control study. BMC Pregnancy Childbirth. 2017;17:307. doi: 10.1186/s12884-017-1507-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.al Se. A multicentre matched case control study of risk factors for Preeclampsia in healthy women in Pakistan. BMC Women's Health. 2010;10:14. [DOI] [PMC free article] [PubMed]
- 31.AMA Abstracts from the 38th Annual Meeting of the Society of General Internal Medicine. J Gen Intern Med. 2015;30(Suppl 2):45–551. doi: 10.1007/s11606-015-3271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duckitt KHD. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005;330:565. doi: 10.1136/bmj.38380.674340.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.John JHZS, Yudkin P, et al. Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: a randomized controlled trial. Lancet. 2002;359:1969. doi: 10.1016/s0140-6736(02)98858-6. [DOI] [PubMed] [Google Scholar]
- 34.Lie RTRS, Brunborg H, et al. Fetal and maternal contributions to risk of pre-eclampsia: population based study. BMJ. 1998;316:1343. doi: 10.1136/bmj.316.7141.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sutapa Agrawal GKW. Prevalence and risk factors for Pre-eclampsia in Indian women: a national cross sectional study.
- 36.Tebeu PMFP, Mbu R, Fosso G, Biyaga PT, Fomulu JN. Risk factors for hypertensive disorders in pregnancy: a report from the Maroua regional hospital, Cameroon. J Reprod Infertil. 2011;12(3):227–234. [PMC free article] [PubMed] [Google Scholar]
- 37.Yogev YMN, Bardin R, et al. Pregnancy outcome at extremely advanced maternal age. Am J Obstet Gynecol. 2010;203:558.e1. doi: 10.1016/j.ajog.2010.07.039. [DOI] [PubMed] [Google Scholar]
- 38.Tessema GA, Tekeste A, Ayele TA. Preeclampsia and associated factors among pregnant women attending antenatal care in Dessie referral hospital, Northeast Ethiopia: a hospital-based study. BMC Pregnancy Childbirth. 2015;15:73. doi: 10.1186/s12884-015-0502-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cooper DW, Brennecke SP, Wilton AN. Genetics of pre-eclampsia. Hypertension Pregnancy. 1993;12(1):1–23. [Google Scholar]
- 40.Chesley LC, Cooper DW. Genetics of hypertension in pregnancy: possible single gene control of pre-eclampsia and eclampsia in the descendants of eclamptic women. BJOG. 1986;93(9):898–908. doi: 10.1111/j.1471-0528.1986.tb08006.x. [DOI] [PubMed] [Google Scholar]
- 41.Skjærven R, Vatten LJ, Wilcox AJ, Rønning T, Irgens LM, Lie RT. Recurrence of pre-eclampsia across generations: exploring fetal and maternal genetic components in a population based cohort. Obstet Gynecol Surv. 2006;61(3):162–163. doi: 10.1136/bmj.38555.462685.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Esplin MS, Fausett MB, Fraser A, Kerber R, Mineau G, Carrillo J, et al. Paternal and maternal components of the predisposition to preeclampsia. Engl J Med. 2001;344(12):867–872. doi: 10.1056/NEJM200103223441201. [DOI] [PubMed] [Google Scholar]
- 43.Nilsson E, Salonen Ros H, Cnattingius S, Lichtenstein P. The importance of genetic and environmental effects for pre-eclampsia and gestational hypertension: a family study. BJOG. 2004;111(3):200–206. doi: 10.1111/j.1471-0528.2004.00042x.x. [DOI] [PubMed] [Google Scholar]
- 44.El-Moselhy EA, Khalifa HO, Amer SM, Mohammad KI, Abd E-AH. Risk factors and impacts of pre-Eclampsia: an epidemiological study among pregnant mothers in Cairo, Egypt. Am J Sci. 2011;7(5):311–323. [Google Scholar]
- 45.Bezerra PC, Leão MD, Queiroz JW, Melo EM, Pereira FV, Nóbrega MH, et al. Family history of hypertension as an important risk factor for the development of severe preeclampsia. Acta Obstet Gynecol Scand. 2010;89(5):612–617. doi: 10.3109/00016341003623720. [DOI] [PubMed] [Google Scholar]
- 46.Vatten LJ, Skjærven R. Is pre-eclampsia more than one disease? BJOG. 2004;111(4):298–302. doi: 10.1111/j.1471-0528.2004.00071.x. [DOI] [PubMed] [Google Scholar]
- 47.Ness RB, Markovic N, Bass D, Harger G, Roberts JM. Family history of hypertension, heart disease, and stroke among women who develop hypertension in pregnancy. Obstet Gynecol. 2003;102(6):1366–1371. doi: 10.1016/j.obstetgynecol.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 48.Wilson BJ, Watson MS, Prescott GJ, Sunderland S, Campbell DM, Hannaford P, et al. Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: results from cohort study. Bmj. 2003;326(7394):845. doi: 10.1136/bmj.326.7394.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dalmáz CA, dos Santos KG, Botton MR, Roisenberg I. Risk factors for hypertensive disorders of pregnancy in southern Brazil. Revista da Associação Médica Brasileira (English Edition) 2011;57(6):678–682. doi: 10.1590/s0104-42302011000600018. [DOI] [PubMed] [Google Scholar]
- 50.Adam I, Elhassan EM, Mohmmed AA, Salih MM, Elbashir MI. Malaria and pre-eclampsia in an area with unstable malaria transmission in Central Sudan. Malar J. 2011;10(1):258. doi: 10.1186/1475-2875-10-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shamsi U, Hatcher J, Shamsi A, Zuberi N, Qadri Z, Saleem S. A multicentre matched case control study of risk factors for preeclampsia in healthy women in Pakistan. BMC Womens Health. 2010;10(1):14. doi: 10.1186/1472-6874-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Qiu C, Williams MA, Leisenring WM, Sorensen TK, Frederick IO, Dempsey JC, et al. Family history of hypertension and type 2 diabetes in relation to preeclampsia risk. Hypertension. 2003;41(3):408–413. doi: 10.1161/01.HYP.0000056996.25503.F5. [DOI] [PubMed] [Google Scholar]
- 53.Kiondo P, Wamuyu-Maina G, Bimenya GS, Tumwesigye NM, Wandabwa J, Okong P. Risk factors for pre-eclampsia in Mulago hospital, Kampala, Uganda. TMIH. 2012;17(4):480–487. doi: 10.1111/j.1365-3156.2011.02926.x. [DOI] [PubMed] [Google Scholar]
- 54.Sierra-Laguado J, García RG, Celedón J, Arenas-Mantilla M, Pradilla LP, Camacho PA, et al. Determination of insulin resistance using the homeostatic model assessment (HOMA) and its relation with the risk of developing pregnancy-induced hypertension. Am J Hypertens. 2007;20(4):437–442. doi: 10.1016/j.amjhyper.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 55.El-Nakhal S. Case-control study of risk factors associated with preeclampsia in the Gaza strip. J Med Medical Sci. 2015;6(9):229–233. [Google Scholar]
- 56.Hu R, Li Y-x, Di H-h, Li Z-w, Zhang C-h, Shen X-p, et al. Risk factors of hypertensive disorders among Chinese pregnant women. J Huazhong Univ Sci Technol [Medical Sciences] 2015;35(6):801–807. doi: 10.1007/s11596-015-1510-6. [DOI] [PubMed] [Google Scholar]
- 57.Aksornphusitaphong A, Phupong V. Risk factors of early and late onset pre-eclampsia. J Obstet Gynaecol Res. 2013;39(3):627–631. doi: 10.1111/j.1447-0756.2012.02010.x. [DOI] [PubMed] [Google Scholar]
- 58.Lykke JA, Paidas MJ, Langhoff-Roos J. Recurring complications in second pregnancy. Obstet Gynecol. 2009;113(6):1217–1224. doi: 10.1097/AOG.0b013e3181a66f2d. [DOI] [PubMed] [Google Scholar]
- 59.Redman CW, Sargent IL. Pre-eclampsia, the placenta and the maternal systemic inflammatory response--a review. Placenta. 2003;24(Suppl A):S21–S27. doi: 10.1053/plac.2002.0930. [DOI] [PubMed] [Google Scholar]
- 60.Romero R, Xu Y, Plazyo O, Chaemsaithong P, Chaiworapongsa T, Unkel R, et al. A role for the Inflammasome in spontaneous labor at term. Am J Reprod Immunol. 2016. [DOI] [PMC free article] [PubMed]
- 61.Rasmussen S, Ebbing C, Irgens LM. Predicting preeclampsia from a history of preterm birth. PLoS One. 2017;12(7):e0181016. doi: 10.1371/journal.pone.0181016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Clausen T, Djurovic S, Henriksen T. Dyslipidemia in early second trimester is mainly a feature of women with early onset pre-eclampsia. BJOG. 2001;108(10):1081–1087. doi: 10.1111/j.1471-0528.2001.00247.x. [DOI] [PubMed] [Google Scholar]
- 63.Bodnar LM, Catov JM, Klebanoff MA, Ness RB, Roberts JM. Prepregnancy body mass index and the occurrence of severe hypertensive disorders of pregnancy. Epidemiology. 2007;18(2):234–239. doi: 10.1097/01.ede.0000254119.99660.e7. [DOI] [PubMed] [Google Scholar]
- 64.Ye C, Ruan Y, Zou L, Li G, Li C, Chen Y, et al. The 2011 survey on hypertensive disorders of pregnancy (HDP) in China: prevalence, risk factors, complications, pregnancy and perinatal outcomes. PloS one. 2014;9(6):e100180. doi: 10.1371/journal.pone.0100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Póvoa A, Costa F, Rodrigues T, Patrício B, Cardoso F. Prevalence of hypertension during pregnancy in Portugal. Hypertension Pregnancy. 2008;27(3):279–284. doi: 10.1080/10641950802000943. [DOI] [PubMed] [Google Scholar]
- 66.Mostello D, Kallogjeri D, Tungsiripat R, Leet T. Recurrence of preeclampsia: effects of gestational age at delivery of the first pregnancy, body mass index, paternity, and interval between births. Am J Obstet Gynecol. 2008;199(1):55. doi: 10.1016/j.ajog.2007.11.058. [DOI] [PubMed] [Google Scholar]
- 67.Ghidini A, Salafia CM. Histologic placental lesions in women with recurrent preterm delivery. Acta Obstet Gynecol Scand. 2005;84(6):547–550. doi: 10.1111/j.0001-6349.2005.00694.x. [DOI] [PubMed] [Google Scholar]
- 68.Aagaard K, Ma J, Antony KM, Ganu R, Petrosino J, Versalovic J. The placenta harbors a unique microbiome. Sci Transl Med. 2014;6(237):237ra65. doi: 10.1126/scitranslmed.3008599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cotechini T, Komisarenko M, Sperou A, Macdonald-Goodfellow S, Adams MA, Graham CH. Inflammation in rat pregnancy inhibits spiral artery remodeling leading to fetal growth restriction and features of preeclampsia. J Exp Med. 2014;211(1):165–179. doi: 10.1084/jem.20130295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sibai BM, Gordon T, Thom E, Caritis SN, Klebanoff M, McNellis D, et al. Risk factors for preeclampsia in healthy nulliparous women: a prospective multicenter study. Am J Obstet Gynecol. 1995;172(2):642–648. doi: 10.1016/0002-9378(95)90586-3. [DOI] [PubMed] [Google Scholar]
- 71.Perni UC, Wikström A-K, Cnattingius S, Villamor E. Interpregnancy change in smoking habits and risk of preeclampsia: a population-based study. Am J Hypertens. 2012;25(3):372–378. doi: 10.1038/ajh.2011.225. [DOI] [PubMed] [Google Scholar]
- 72.Luo Z-C, Julien P, Wei S-Q, Audibert F, Smith GN, Fraser WD, et al. Plasma cotinine indicates an increased risk of preeclampsia in previous and passive smokers. Am J Obstet Gynecol. 2014;210(3):232. doi: 10.1016/j.ajog.2013.09.041. [DOI] [PubMed] [Google Scholar]
- 73.Chang JJ, Strauss JF, III, Deshazo JP, Rigby FB, Chelmow DP, Macones GA. Reassessing the impact of smoking on preeclampsia/Eclampsia: are there age and racial differences? PLoS One. 2014;9(10):e106446. doi: 10.1371/journal.pone.0106446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Poredoš P, Orehek M, Tratnik E, Poredoš P. Smoking is associated with dose-related increase of intima-media thickness and endothelial dysfunction. Angiology. 1999;50(3):201–208. doi: 10.1177/000331979905000304. [DOI] [PubMed] [Google Scholar]
- 75.Lekakis J, Papamichael C, Vemmos C, Stamatelopoulos K, Voutsas A, Stamatelopoulos S. Effects of acute cigarette smoking on endothelium-dependent arterial dilatation in normal subjects. Am J Cardiol. 1998;81(10):1225–1228. doi: 10.1016/s0002-9149(98)00098-8. [DOI] [PubMed] [Google Scholar]
- 76.Sooranna SR, Morris NH, Steer PJ. Placental nitric oxide metabolism. Reprod Fertil Dev. 1995;7(6):1525–1531. doi: 10.1071/rd9951525. [DOI] [PubMed] [Google Scholar]
- 77.Wang Y, Gu Y, Zhang Y, Lewis DF. Evidence of endothelial dysfunction in preeclampsia: decreased endothelial nitric oxide synthase expression is associated with increased cell permeability in endothelial cells from preeclampsia. Am J Obstet Gynecol. 2004;190(3):817–824. doi: 10.1016/j.ajog.2003.09.049. [DOI] [PubMed] [Google Scholar]
- 78.Wang XL, Sim AS, Wang MX, Murrell GA, Trudinger B, Wang J. Genotype dependent and cigarette specific effects on endothelial nitric oxide synthase gene expression and enzyme activity. FEBS Lett. 2000;471(1):45–50. doi: 10.1016/s0014-5793(00)01356-9. [DOI] [PubMed] [Google Scholar]
- 79.Goswami D, Tannetta D, Magee L, Fuchisawa A, Redman C, Sargent I, et al. Excess syncytiotrophoblast microparticle shedding is a feature of early-onset pre-eclampsia, but not normotensive intrauterine growth restriction. Placenta. 2006;27(1):56–61. doi: 10.1016/j.placenta.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 80.Sargent I, Germain S, Sacks G, Kumar S, Redman C. Trophoblast deportation and the maternal inflammatory response in pre-eclampsia. J Reprod Immunol. 2003;59(2):153–160. doi: 10.1016/s0165-0378(03)00044-5. [DOI] [PubMed] [Google Scholar]
- 81.Knight M, Redman CW, Linton EA, Sargent IL. Shedding of syncytiotrophoblast microvilli into the maternal circulation in pre-eclamptic pregnancies. BJOG Int J Gynecol Obstet. 1998;105(6):632–640. doi: 10.1111/j.1471-0528.1998.tb10178.x. [DOI] [PubMed] [Google Scholar]
- 82.Huppertz B, Kingdom JC. Apoptosis in the trophoblast—role of apoptosis in placental morphogenesis. JAMA J Soc Gynecol Investig. 2004;11(6):353–362. doi: 10.1016/j.jsgi.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 83.Van der Veen F, Fox H. The effects of cigarette smoking on the human placenta: a light and electron microscopic study. Placenta. 1982;3(3):243–256. doi: 10.1016/s0143-4004(82)80002-7. [DOI] [PubMed] [Google Scholar]
- 84.Demir R, Demir A, Yinanc M. Structural changes in placental barrier of smoking mother a quantitative and ulstrastructural study. Pathol Res Pract. 1994;190(7):656–667. doi: 10.1016/s0344-0338(11)80744-2. [DOI] [PubMed] [Google Scholar]
- 85.Van der Velde W, Peereboom-Stegeman JC, Treffers P, James J. Structural changes in the placenta of smoking mothers: a quantitative study. Placenta. 1983;4(3):231–240. doi: 10.1016/s0143-4004(83)80002-2. [DOI] [PubMed] [Google Scholar]
- 86.Van der Velde W, Copius J, Stegeman P, Treffers P, James J. Basal lamina thickening in the placentae of smoking mothers. Placenta. 1985;6(4):329–340. doi: 10.1016/s0143-4004(85)80042-4. [DOI] [PubMed] [Google Scholar]
- 87.Conde-Agudelo A, Althabe F, Belizán JM, Kafury-Goeta AC. Cigarette smoking during pregnancy and risk of preeclampsia: a systematic review. Am J Obstet Gynecol. 1999;181(4):1026–1035. doi: 10.1016/s0002-9378(99)70341-8. [DOI] [PubMed] [Google Scholar]
- 88.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086–1093. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Parazzini F, Ricci E, Chatenoud L, Tozzi L, Rosa C, Nicolosi AE, et al. Maternal and paternal smoking and pregnancy-induced hypertension. Eur J Obstet Gynecol Reprod Biol. 2003;109(2):141–144. doi: 10.1016/s0301-2115(03)00006-x. [DOI] [PubMed] [Google Scholar]
- 90.Newman MG, Lindsay MK, Graves W. Cigarette smoking and pre-eclampsia: their association and effects on clinical outcomes. J Matern-Fetal Neonatal Med. 2001;10(3):166–170. doi: 10.1080/714904321. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
On presumable requests, the data sets used for analysis during the current study are available from the corresponding author.