Abstract
Background
Several countries affected by the COVID-19 pandemic have reported a substantial drop in the number of patients attending the emergency department with acute coronary syndromes and a reduced number of cardiac procedures. We aimed to understand the scale, nature, and duration of changes to admissions for different types of acute coronary syndrome in England and to evaluate whether in-hospital management of patients has been affected as a result of the COVID-19 pandemic.
Methods
We analysed data on hospital admissions in England for types of acute coronary syndrome from Jan 1, 2019, to May 24, 2020, that were recorded in the Secondary Uses Service Admitted Patient Care database. Admissions were classified as ST-elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), myocardial infarction of unknown type, or other acute coronary syndromes (including unstable angina). We identified revascularisation procedures undertaken during these admissions (ie, coronary angiography without percutaneous coronary intervention [PCI], PCI, and coronary artery bypass graft surgery). We calculated the numbers of weekly admissions and procedures undertaken; percentage reductions in weekly admissions and across subgroups were also calculated, with 95% CIs.
Findings
Hospital admissions for acute coronary syndrome declined from mid-February, 2020, falling from a 2019 baseline rate of 3017 admissions per week to 1813 per week by the end of March, 2020, a reduction of 40% (95% CI 37–43). This decline was partly reversed during April and May, 2020, such that by the last week of May, 2020, there were 2522 admissions, representing a 16% (95% CI 13–20) reduction from baseline. During the period of declining admissions, there were reductions in the numbers of admissions for all types of acute coronary syndrome, including both STEMI and NSTEMI, but relative and absolute reductions were larger for NSTEMI, with 1267 admissions per week in 2019 and 733 per week by the end of March, 2020, a percent reduction of 42% (95% CI 38–46). In parallel, reductions were recorded in the number of PCI procedures for patients with both STEMI (438 PCI procedures per week in 2019 vs 346 by the end of March, 2020; percent reduction 21%, 95% CI 12–29) and NSTEMI (383 PCI procedures per week in 2019 vs 240 by the end of March, 2020; percent reduction 37%, 29–45). The median length of stay among patients with acute coronary syndrome fell from 4 days (IQR 2–9) in 2019 to 3 days (1–5) by the end of March, 2020.
Interpretation
Compared with the weekly average in 2019, there was a substantial reduction in the weekly numbers of patients with acute coronary syndrome who were admitted to hospital in England by the end of March, 2020, which had been partly reversed by the end of May, 2020. The reduced number of admissions during this period is likely to have resulted in increases in out-of-hospital deaths and long-term complications of myocardial infarction and missed opportunities to offer secondary prevention treatment for patients with coronary heart disease. The full extent of the effect of COVID-19 on the management of patients with acute coronary syndrome will continue to be assessed by updating these analyses.
Funding
UK Medical Research Council, British Heart Foundation, Public Health England, Health Data Research UK, and the National Institute for Health Research Oxford Biomedical Research Centre.
Introduction
Worldwide, the COVID-19 pandemic has resulted in substantial excess mortality arising directly from respiratory failure.1 It has necessitated major reorganisations of emergency care facilities to accommodate the additional workload anticipated with a rapid surge in critically ill patients with COVID-19.2 Cardiologists have reported substantial falls in the number of patients presenting with acute coronary syndromes and in the numbers of emergency coronary procedures in both Europe3, 4, 5, 6 and the USA.7, 8
The first fatality for COVID-19 in the UK was reported on March 5, 2020.9 On March 16, 2020, the UK Prime Minister urged the introduction of physical distancing measures,10 and on March 23, 2020, a nationwide lockdown was announced.11 UK health protection regulations came into force on March 26, 2020,12 which severely restricted movement among all UK citizens, although they still allowed people to leave their homes for essential reasons, including seeking health care. Analyses by Public Health England show a roughly 30% reduction in emergency ambulance calls for chest pain in England13 and a greater than 52% reduction in emergency department attendances for myocardial ischaemia in England in March, 2020, with a subsequent rise.14 Furthermore, surveys of cardiologists in the UK and elsewhere have suggested a substantial reduction in demand for coronary procedures.15 On March 20, 2020, the British Cardiovascular Intervention Society issued guidance on measures to address the potential effect of COVID-19 on cardiology services.16
Research in context.
Evidence before this study
Reports have shown reductions in admissions for acute coronary syndrome and in primary percutaneous coronary intervention (PCI) procedures for acute myocardial infarction during the COVID-19 pandemic in several countries (eg, Austria, Italy, Spain, and the USA). These studies have provided scant information, however, about the time course of the changes in admission rates, the effect on different types of acute coronary syndrome, the treatment of patients admitted with acute coronary syndrome, and the relevance of patients' characteristics to the observed reductions.
Added value of this study
Our study provides quantitative information about the time course of admission patterns and in-hospital management for acute coronary syndromes, including separately for ST-elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI), since January, 2019. There was a 23% (95% CI 16–30) reduction in admissions for STEMI, and a reduction of 42% (38–46) in admissions for NSTEMI, from 2019 to the end of March, 2020. By the end of May, 2020, admission rates for acute coronary syndrome had partly recovered but remained about 16% below baseline levels. The decline in admissions started before the UK lockdown (which happened on March 23, 2020) and was qualitatively similar throughout the country, with only minor variations in the magnitude of the changes in different demographic groups. Our study also identified changes in the management of patients who were admitted with an acute myocardial infarction throughout this period, with both a sustained increase in the proportion of patients receiving PCI on the day of admission and a continued reduction in the median length of stay.
Implications of all the available evidence
Patients who do not go to hospital with an acute coronary syndrome, particularly STEMI, cannot benefit from reperfusion therapy or other appropriate treatments and are at increased risk of complications. The reasons for patients failing to attend emergency departments with acute coronary syndrome and other urgent conditions should be addressed promptly to avoid unnecessary deaths and disability, particularly during subsequent recurrences of COVID-19 in the UK or elsewhere.
To understand the scale, nature, and duration of changes to admissions for different types of acute coronary syndrome, and to evaluate whether in-hospital management of patients has been affected as a result of the COVID-19 pandemic, we sought data for acute coronary syndrome admissions to National Health Service (NHS) acute hospital trusts in England from Jan 1, 2019. We intend to revise these analyses monthly and make them available online to provide an updated summary of changes in such admissions as the response to the COVID-19 pandemic evolves.
Methods
Data collection
All episodes of care for patients admitted to acute NHS hospital trusts in England with acute coronary syndrome, defined using International Classification of Diseases 10th revision (ICD-10) codes, from Jan 1, 2019, to May 24, 2020, were identified in the Secondary Uses Service Admitted Patient Care (SUSAPC) database (appendix pp 2–4). We used the SUSAPC database because it is updated more rapidly than is the Hospital Episodes Statistics database. Admissions were classified as ST-elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), myocardial infarction of unknown type, or other acute coronary syndromes (including unstable angina), according to the recorded ICD-10 codes (appendix p 5).
Procedures
To prevent overcounting of acute coronary syndrome events, episodes of care for every individual were linked into continuous single hospital admissions (spells), and spells were linked between hospitals (superspells). Revascularisation procedures (ie, coronary angiography without percutaneous coronary intervention [PCI], PCI, and coronary artery bypass graft [CABG] surgery) undertaken during these admissions were identified from relevant Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures, 4th revision codes (appendix p 6).17 It is not possible to identify primary PCI in SUSAPC data, so PCI on the day of admission was used as a surrogate for primary PCI among patients with STEMI.
As a result of service reorganisation in response to COVID-19,16 a reduction in the speed and completeness of clinical coding might have happened, which could result in artefactual declines in acute coronary syndrome-related admissions (particularly in the most recent data). For each week after Feb 17, 2020, we investigated this possibility by ascertaining the proportion of all SUSAPC records recorded in each week that contained no diagnostic ICD-10 codes, and an adjustment was made to the numbers of recorded admissions for acute coronary syndrome each week based on these proportions.
Statistical analysis
In all analyses of admission numbers, data are presented for 2019 as median (IQR) weekly recorded numbers. For 2020, a local polynomial regression smoothing function (locally estimated scatterplot smoothing) was fitted through the weekly numbers (using the loess function in R with default settings). From 2020, weekly adjusted numbers (indicating the number of admissions in the preceding 7 days) are plotted along with their approximate SEs (under the assumption that the numbers follow a Poisson distribution). Percentage changes in weekly admissions were calculated by comparing the adjusted weekly admission number for the week commencing March 23, 2020, the week in which the lowest number of admissions was observed, with the mean weekly number during 2019; percentage changes are presented with 95% CIs. Percentage changes in weekly admissions among subgroups were calculated similarly, with tests for heterogeneity or trend across every subgroup presented. Monthly updates of tables and figures are available online. Analyses were produced using R version 3.6.3.
Role of the funding source
The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication.
Results
SUSAPC data were available from all 147 acute NHS hospital trusts in England. Demographic characteristics of patients with acute coronary syndrome during January to May, 2020, were similar to the monthly average for 2019 (table 1 ). In 2019, the average number of acute coronary syndrome admissions per week from February to April, 2019 (3082 per week), was similar to the average number during the other months of the year (2994 per week).
Table 1.
Characteristics of patients admitted to acute National Health Service hospital trusts in England with a diagnosis of any acute coronary syndrome (January, 2019, to May, 2020)
| Monthly average for 2019 (n=13 075) | January, 2020 (n=13 645) | February, 2020 (n=12 443) | March, 2020 (n=10 118) | April, 2020 (n=8739) | May, 2020 (n=9756) | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Female | 4829 (37%) | 5131 (38%) | 4518 (36%) | 3670 (36%) | 3038 (35%) | 3301 (34%) |
| Male | 8245 (63%) | 8513 (62%) | 7921 (64%) | 6441 (64%) | 5652 (65%) | 6404 (66%) |
| Age group | ||||||
| <50 years | 953 (7%) | 1051 (8%) | 953 (8%) | 754 (7%) | 713 (8%) | 799 (8%) |
| 50–59 years | 2082 (16%) | 2156 (16%) | 2013 (16%) | 1686 (17%) | 1516 (17%) | 1760 (18%) |
| 60–69 years | 2723 (21%) | 2821 (21%) | 2553 (21%) | 2203 (22%) | 1931 (22%) | 2136 (22%) |
| 70–79 years | 3353 (26%) | 3556 (26%) | 3184 (26%) | 2558 (25%) | 2171 (25%) | 2456 (25%) |
| ≥80 years | 3963 (30%) | 4061 (30%) | 3740 (30%) | 2917 (29%) | 2408 (28%) | 2605 (27%) |
| Ethnic group | ||||||
| White | 10 313 (79%) | 10 678 (78%) | 9744 (78%) | 7865 (78%) | 6872 (79%) | 7565 (78%) |
| Mixed race | 58 (<1%) | 65 (<1%) | 71 (1%) | 43 (<1%) | 31 (<1%) | 31 (<1%) |
| Asian | 956 (7%) | 998 (7%) | 887 (7%) | 677 (7%) | 510 (6%) | 616 (6%) |
| Black | 196 (2%) | 204 (1%) | 177 (1%) | 149 (1%) | 138 (2%) | 123 (1%) |
| Other or unknown | 1552 (12%) | 1700 (12%) | 1564 (13%) | 1384 (14%) | 1180 (14%) | 1421 (15%) |
| Charlson index | ||||||
| 0 | 3933 (30%) | 4032 (30%) | 3639 (29%) | 3128 (31%) | 2764 (32%) | 3240 (33%) |
| 1 | 3591 (27%) | 3712 (27%) | 3482 (28%) | 2899 (29%) | 2449 (28%) | 2697 (28%) |
| 2 | 2180 (17%) | 2340 (17%) | 2140 (17%) | 1676 (17%) | 1405 (16%) | 1572 (16%) |
| 3+ | 3371 (26%) | 3561 (26%) | 3182 (26%) | 2415 (24%) | 2121 (24%) | 2247 (23%) |
| Region of admission* | ||||||
| Northeast | 705 (5%) | 700 (5%) | 690 (6%) | 550 (5%) | 460 (5%) | 505 (5%) |
| Northwest | 2050 (16%) | 2200 (16%) | 1920 (15%) | 1625 (16%) | 1495 (17%) | 1550 (16%) |
| Yorkshire and Humber | 1510 (12%) | 1635 (12%) | 1435 (12%) | 1245 (12%) | 1040 (12%) | 1180 (12%) |
| East Midlands | 1060 (8%) | 1115 (8%) | 1010 (8%) | 825 (8%) | 655 (7%) | 800 (8%) |
| West Midlands | 1380 (11%) | 1395 (10%) | 1285 (10%) | 1040 (10%) | 890 (10%) | 1080 (11%) |
| East of England | 1380 (11%) | 1400 (10%) | 1380 (11%) | 1035 (10%) | 960 (11%) | 980 (10%) |
| London | 1720 (13%) | 1805 (13%) | 1645 (13%) | 1260 (12%) | 1060 (12%) | 1225 (13%) |
| Southeast | 1750 (13%) | 1860 (14%) | 1690 (14%) | 1410 (14%) | 1235 (14%) | 1415 (15%) |
| Southwest | 1520 (12%) | 1535 (11%) | 1385 (11%) | 1135 (11%) | 945 (11%) | 1020 (10%) |
Data are n (%). Numbers of admissions are unadjusted for incomplete coding (appendix pp 2–4). Percentage changes in admission rates for each subgroup are provided in the appendix (p 7).
Regional numbers are rounded to the nearest multiple of 5.
A decline was seen in hospital admissions for acute coronary syndrome between mid-February, 2020, and the end of March, 2020 (figure 1 ), with the 2019 baseline number of 3017 admissions per week falling to 1813 per week (proportional reduction 40%, 95% CI 37–43; table 2 ). This decline was partly reversed during April and May, 2020, such that by the last week of May, 2020, there were 2522 admissions, representing a 16% (95% CI 13–20) reduction from baseline (figure 1). Reductions were recorded in numbers of admissions for acute myocardial infarction, STEMI, and NSTEMI from the average for 2019, to the end of March, 2020 (figure 1; table 2). The percentage reduction in admissions for all acute myocardial infarctions was 35% (95% CI 32–39), with an average of 2061 admissions per week in 2019, falling to 1335 per week by the end of March, 2020. For STEMI, there were 621 admissions per week in 2019 and 477 per week by the end of March, 2020 (percentage reduction in admissions 23%, 95% CI 16–30). The percentage reduction in admissions for NSTEMI was 42% (95% CI 38–46), with 1267 admissions per week in 2019 and 733 per week by the end of March, 2020. Admissions for both STEMI and NSTEMI rose through April and May, 2020, such that, by the last week of May, 2020, admissions were 10% lower than the 2019 baseline for STEMI (95% CI 2–17; 561 admissions per week) and 24% lower for NSTEMI (95% CI 19–28; 966 admissions per week; figure 1).
Figure 1.
Weekly admissions to acute National Health Service hospital trusts in England with an acute coronary syndrome, by type
For weekly admissions in 2019, boxplots show the median and IQR, with whiskers extending (up to) 1·5 times the IQR above the upper quartile and below the lower quartile, with any weekly counts beyond those ranges indicated by x. For 2020, a locally estimated scatterplot smoothing spline is fitted through the weekly reported counts, with datapoints and SEs plotted. The date of the UK COVID-19 lockdown (March 23, 2020) is shown with a vertical dotted line. STEMI=ST-elevation myocardial infarction. NSTEMI=non-ST-elevation myocardial infarction.
Table 2.
Percent reduction in weekly acute coronary syndrome admissions to acute National Health Service hospital trusts in England, from average weekly admissions in 2019 to admissions week commencing March 23, 2020, the week in which the lowest number of admissions was observed
| All admissions | Any PCI | PCI on day of admission | PCI after day of admission | CABG surgery | Angiography only | |
|---|---|---|---|---|---|---|
| Acute coronary syndrome | ||||||
| 2019 weekly average | 3017 | 909 | 464 | 450 | 93 | 429 |
| March 23–30, 2020 | 1813 | 631 | 392 | 239 | 19 | 172 |
| Percent reduction (95% CI) | 40% (37 to 43) | 31% (25 to 36) | 16% (7 to 24) | 47% (40 to 53) | 80% (68 to 87) | 60% (53 to 65) |
| Acute myocardial infarction | ||||||
| 2019 weekly average | 2061 | 834 | 453 | 386 | 80 | 306 |
| March 23–30, 2020 | 1335 | 594 | 381 | 213 | 17 | 139 |
| Percent reduction (95% CI) | 35% (32 to 39) | 29% (23 to 34) | 16% (7 to 24) | 45% (37 to 52) | 79% (66 to 87) | 55% (46 to 62) |
| STEMI | ||||||
| 2019 weekly average | 621 | 438 | 379 | 63 | 16 | 49 |
| March 23–30, 2020 | 477 | 346 | 309 | 36 | 4 | 34 |
| Percent reduction (95% CI) | 23% (16 to 30) | 21% (12 to 29) | 18% (9 to 27) | 43% (21 to 59) | 75% (33 to 91) | 31% (3 to 51) |
| NSTEMI | ||||||
| 2019 weekly average | 1267 | 383 | 67 | 317 | 63 | 245 |
| March 23–30, 2020 | 733 | 240 | 68 | 172 | 13 | 97 |
| Percent reduction (95% CI) | 42% (38 to 46) | 37% (29 to 45) | −1% (−29 to 20) | 46% (37 to 53) | 79% (64 to 88) | 60% (52 to 68) |
Data are n per week, unless otherwise stated. PCI=percutaneous coronary intervention. CABG=coronary artery bypass graft. STEMI=ST-elevation myocardial infarction. NSTEMI=non-ST-elevation myocardial infarction.
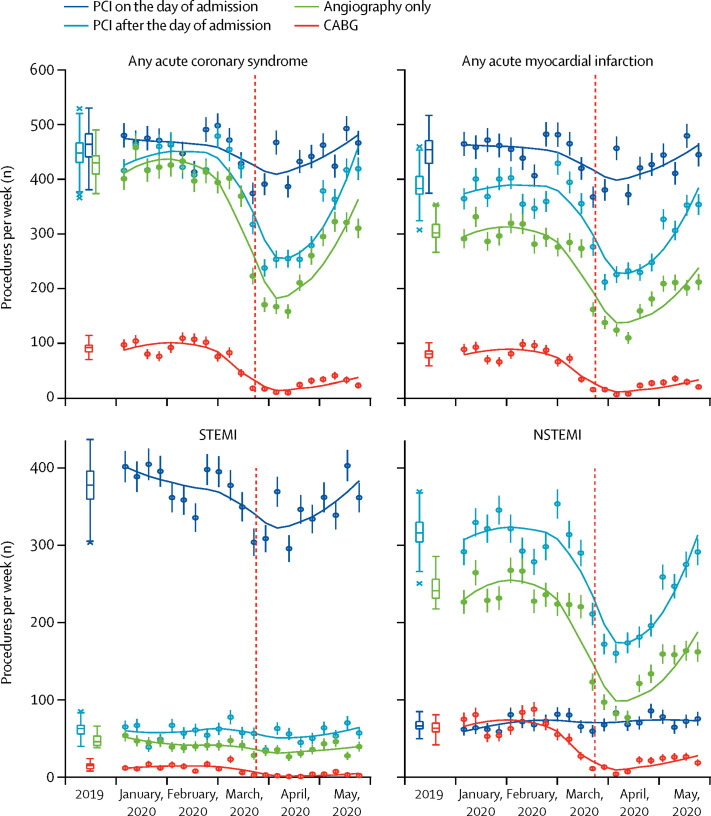
The 23% reduction in admissions for STEMI was accompanied by a slight rise in the proportion of patients admitted to hospital and receiving PCI on the day of admission (figure 2 ). As a result, the absolute number of patients with STEMI receiving PCI on the day of admission fell between 2019 and the end of March, 2020 (from 379 per week to 309 per week), a proportional reduction of 18% (95% CI 9–27; table 2; figure 3 ). The 42% reduction in NSTEMI admissions was accompanied by a slight increase in the proportion who received PCI at any time during admission (table 2; appendix p 8), which translated into a percentage reduction of 37% (95% CI 29–45) and a decrease in absolute numbers receiving PCI from 383 per week in 2019 to 240 per week by the end of March, 2020. For all types of acute coronary syndrome combined, the percentage reduction in patients having angiography without PCI was 60% (95% CI 53–65), with 429 procedures per week in 2019 and 172 per week by the end of March, 2020. CABG surgery during admission had largely ceased by April, 2020 (figure 3), with a percentage reduction of 80% (95% CI 68–87; table 2).
Figure 2.
Weekly admissions to acute National Health Service hospital trusts in England with an acute coronary syndrome receiving PCI on the day of admission
For weekly admissions in 2019, boxplots show the median and IQR, with whiskers extending (up to) 1·5 times the IQR above the upper quartile and below the lower quartile, with any weekly counts beyond those ranges indicated by x. For 2020, a locally estimated scatterplot smoothing spline is fitted through the weekly reported counts or proportions. Vertical lines represent 1 SD for weekly counts or proportions. The date of the UK COVID-19 lockdown (March 23, 2020) is shown with a vertical dotted line. STEMI=ST-elevation myocardial infarction. NSTEMI=non-ST-elevation myocardial infarction. PCI=percutaneous coronary intervention.
Figure 3.
Weekly admissions to acute National Health Service hospital trusts in England with an acute coronary syndrome receiving a coronary procedure
For weekly admissions in 2019, boxplots (coloured according to type of procedure) show the median and IQR, with whiskers extending (up to) 1·5 times the IQR above the upper quartile and below the lower quartile, with any weekly counts beyond those ranges indicated by x. For 2020, a locally estimated scatterplot smoothing spline is fitted through the weekly reported counts, with datapoints and SEs plotted. The date of the UK COVID-19 lockdown (March 23, 2020) is shown with a vertical dotted line. CABG=coronary artery bypass graft. STEMI=ST-elevation myocardial infarction. NSTEMI=non-ST-elevation myocardial infarction. PCI=percutaneous coronary intervention.
By the end of March, 2020, the median length of stay among patients admitted with any acute coronary syndrome fell from 4 days (IQR 2–9) in 2019 to 3 days (1–5; appendix p 9). For STEMI, the reduction in median stay was from 3 days (IQR 2–6) to 2 days (2–4) and for NSTEMI it was from 5 days (3–11) to 3 days (2–6). The length of stay remained lower during April and May, 2020. There was no apparent change in in-hospital mortality among patients admitted with acute coronary syndrome (data not shown).
The relative reductions in weekly numbers of admissions for acute coronary syndrome by the end of March, 2020, were qualitatively similar in all of the subgroups studied, but they seemed slightly larger among patients with a higher (worse) Charlson comorbidity index and for individuals in the London and East Midlands regions of England (appendix pp 7, 10).
Discussion
Previous reports of reduced admissions for acute coronary syndrome and decreased use of coronary procedures in various countries affected by the COVID-19 pandemic3, 4, 5, 6, 7, 8 have indicated that declines in admissions and procedures are widespread. However, those reports have provided scant detail: in particular, only one study8 reported the time course of changes in number of admissions, and there has been a paucity of information about the relative effect on different types of acute coronary syndrome, the acute management of patients admitted with acute coronary syndrome, and the relevance of patients' characteristics. By contrast, in our study, unique access to rapidly available, central NHS health-care data has allowed us to produce near real-time analyses based on all admissions for acute coronary syndrome in all 147 acute hospitals across England. Moreover, we are able to follow emerging trends over time as the response to COVID-19 evolves (eg, with easing of restrictions and any recurrent outbreaks of infection).
Our study provides several key insights into the noted reduction in admissions for acute coronary syndrome. First, by the end of March, 2020, the average weekly number of acute coronary syndrome admissions fell by 40% compared with the average weekly number observed during 2019. The decline seems to have started at least 2 weeks before the first UK death from COVID-19 (on March 5, 2020), and about a month before the UK Government implemented the lockdown (on March 23, 2020). This finding is consistent with a report based on data from US Kaiser Permanente Northern California, which indicated that the reduction in acute myocardial infarction admissions preceded the US shelter-in-place order by about 2 weeks.8 Our study also shows that, beginning in April, 2020, admissions for acute coronary syndrome in England began to return to normal and, by the end of May, 2020, were about 16% below the 2019 baseline level. Measured against this baseline, from January, 2020, until the end of May, 2020, there had been around 8000 fewer admissions for acute coronary syndromes than would be expected, including 5000 fewer admissions for myocardial infarction, and this deficit will continue to grow until weekly admission numbers return to normal.
By mid-February, 2020, UK media were reporting the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in China and in northern Italy. NHS hospitals had been told to prepare for a large influx of patients with COVID-19. As early as Feb 14, 2020, fear-inducing language was noted in the media.18 Taken together with survey data from Hong Kong, in which patients delayed seeking medical help because of worries about acquiring COVID-19,19 it seems likely that fear of contagion has been a major factor underlying the observed reduction in admissions for acute coronary syndrome in our study. The partial recovery in admission rates by the end of May, 2020, suggests that the British Heart Foundation and British Cardiovascular Society publicity campaign in early April, 2020, in which people with heart attack symptoms were encouraged to attend hospital, could have helped to allay such fears.20 The observation that the decline in admissions preceded the UK lockdown and, despite the continuing lockdown, had partly recovered by the end of May, 2020, suggests that environmental changes (eg, reduced air pollution), decreased physical activity, or diminished stress because of lockdown are unlikely to be major contributors to the noted trends in acute coronary syndrome admissions in the current pandemic.21, 22
A second novel finding of our analysis is the clear distinction between the 23% reduction in STEMI admissions compared with the 42% reduction of NSTEMI admissions. Our analyses in an unselected study population are based on much larger numbers of admissions than in any previous study, some of which reported a smaller reduction for STEMI than for NSTEMI (in Italy),5 whereas studies in Austria and northern California did not detect a difference in decreases for different types of myocardial infarction.3, 8 As STEMI is generally associated with severe and unremitting symptoms, patients with STEMI could be less reluctant to seek help irrespective of any fears they might have about attending a hospital, whereas those with NSTEMI might be able to tolerate less severe symptoms and so opt to remain at home.
Third, we were able to document how acute management of admitted patients changed during the pandemic period. In preparation for the COVID-19 pandemic, UK cardiology services were reorganised such that elective PCI and CABG surgery would not be available routinely during the outbreak. Instead, it was recommended that, if current NSTEMI pathways could not be followed because of reduced intensive care unit capacity or other issues, PCI should be used in place of surgery and inpatient stays reduced to 36–48 h.16 Consistent with these recommendations, our results show that patients admitted with NSTEMI were more likely to receive PCI while in hospital (often on the day of admission) and to have shorter hospital stays. However, since the numbers of patients admitted with both NSTEMI and STEMI were reduced, fewer patients with acute coronary syndrome received PCI.
Finally, the large numbers of cases and national coverage of these data allowed us to show that the pattern of reduced admissions was qualitatively similar (albeit slightly different quantitatively) in several important demographic groups. For example, despite the greater risk with COVID-19 among older patients and those with comorbidities, there were similar reductions in the numbers of individuals with acute coronary syndrome admitted at younger ages and without comorbidities, in whom the long-term benefits of cardiovascular interventions would typically be greater. Likewise, despite different COVID-19 admission rates across the UK during the early phase of the pandemic, little difference was seen in the reduction in acute coronary syndrome admissions between different regions. This consistency suggests that drivers of the noted fall in admissions are likely to be common (to a greater or lesser extent) to all patient groups.
Taken together, the substantial reduction in admissions for acute coronary syndrome during the COVID-19 pandemic is a serious concern, because patients with symptoms indicative of acute myocardial ischaemia benefit from rapid in-hospital assessment,23, 24 with the gain being greatest among those with STEMI. Among such patients, there is a substantial risk of out-of-hospital cardiac arrest,25 and the failure of patients with STEMI to be admitted to hospital so they can receive early reperfusion therapy and other appropriate treatments is likely to have resulted in avoidable deaths and complications, such as fatal arrhythmias26 and disabling heart failure.27 Although no overall increase in in-hospital mortality was seen among patients admitted for acute coronary syndrome, a direct comparison between mortality rates before and after mid-March, 2020, is likely to be confounded by differences in underlying risk of admitted patients and by the duration of hospital stay. Moreover, it is not possible to assess directly the deaths and disability that probably occurred among those patients with acute coronary syndrome who were not admitted to hospital because of COVID-19 and, therefore, did not receive treatment that is known to be effective.
What are the implications of our findings for the UK and for other countries, including settings where the COVID-19 pandemic is only just starting, and how can they help inform preparations for any subsequent increases in infection rates now that lockdown restrictions are being relaxed? Our findings confirm the general pattern reported from other countries. Furthermore, the qualitative similarity of decreases in acute coronary syndrome admission rates, irrespective of age, sex, number of comorbidities, and region, suggests that our findings are likely to be generalisable to all patients who are having an acute myocardial infarction, not only in the UK but also elsewhere in the world. If the reduction in hospital admissions is largely or wholly because of fear of exposure to SARS-CoV-2, it seems probable that the same reduction in admissions will be seen wherever there is a rapid increase in COVID-19 cases and public health messaging is not suitably nuanced. Monthly updates of these analyses will continue to monitor the recovery in acute coronary syndrome admissions and provide an early warning of another decline in admission trends during any subsequent recurrence of COVID-19 in the UK. More generally, it would be valuable to establish similar continuous analyses for other serious diseases in the UK and in other locations where centralised electronic health record data are available (eg, China or Sweden, or in US health maintenance organisations), to monitor such trends to ensure that they reverse and do not recur during this pandemic or, indeed, any subsequent ones.
Our study has some limitations. SUSAPC data are timely but incomplete, with some NHS trusts having recorded admissions without a diagnostic code. We have addressed this issue by applying an adjustment (appendix pp 2–4), and we validated our approach by confirming that the adjusted results for March and April, 2020, based on earlier data, accord with unadjusted results based on later data for which the coding for admissions in March and April, 2020, was more complete. This comparison suggests that our approach to adjustment is likely to be generalisable to the study of time trends for other serious conditions.
A further potential limitation of our analysis is that the coding of STEMI and NSTEMI was inferred from ICD-10 codes, which can be somewhat inaccurate. Our results provided a clear contrast between rates of admission for, and management of, STEMI and NSTEMI that have been diagnosed and coded in much the same way throughout 2019 and 2020. As a result, any bias in comparison of acute coronary syndrome rates attributable to misclassification of STEMI and NSTEMI is likely to be modest (other than because of late reporting in the most recent weeks) and, if removed, would yield even more striking differences between the rates for STEMI and NSTEMI. A further limitation is that the SUSAPC data do not allow assessments to be made of any delays in admissions from the onset of symptoms of acute coronary syndrome or of any effect on the rates of complications in the patients admitted with myocardial infarction.
Although a national campaign in the UK to encourage all people experiencing symptoms of acute myocardial ischaemia to call an ambulance immediately20 might have contributed to the partial recovery in admission rates recorded by the end of May, 2020, it remains necessary to address the public's fear that they might contract COVID-19 by going to hospital. Measures to provide relatively clean areas for patients who do not have COVID-19, and reassurance to the public that these areas exist, are needed in both the UK and in other countries. Otherwise, people might continue to be reluctant to call an ambulance, even if experiencing severe symptoms, resulting in unnecessary deaths and disability.
Acknowledgments
Acknowledgments
This work was supported by the UK Medical Research Council, British Heart Foundation, Public Health England, Health Data Research UK and the National Institute for Health Research Oxford Biomedical Research Centre. Monthly updates of all figures and supplementary figures are available at https://www.ctsu.ox.ac.uk/research/covid-19-acute-coronary-syndromes.
Contributors
All authors contributed to study design, data interpretation, and writing of the report. Data were processed for analysis by DG, PC, SH, MB, and CR. Statistical analysis was done by ES, JRE, and RG.
Declaration of interests
BC is the current President of the European Society of Cardiology (2018–20), a British Heart Foundation Chair holder, and lead of the cardiovascular theme of the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre. RC is a British Heart Foundation Chair holder; reports personal fees from UK Biobank, grants from Merck and The Medicines Company, and a prize to Nuffield Department of Population Health for independent research from Pfizer, outside of the submitted work; and has a patent for a statin-related myopathy genetic test licensed to the University of Oxford from Boston Heart Diagnostics (any personal reward has been waived). MJL reports grants from the Medical Research Council, Health Data Research UK, and NIHR Oxford Biomedical Research Centre, during the conduct of the study; and grants from Merck, The Medicines Company, Boehringer Ingelheim, and UK Biobank, outside of the submitted work. MMM reports grants from Medco and Novartis, outside of the submitted work. JRE and CB report grants from Boehringer Ingelheim, outside of the submitted work. All other authors declare no competing interests.
Supplementary Material
References
- 1.Banerjee A, Pasea L, Harris S, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395:1715–1725. doi: 10.1016/S0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Strengthening the health systems response to COVID-19: creating surge capacity for acute and intensive care. April 6, 2020. https://www.euro.who.int/__data/assets/pdf_file/0006/437469/TG2-CreatingSurgeAcuteICUcapacity-eng.pdf?ua=1
- 3.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, et al. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 7.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Solomon MD, McNulty EJ, Rana JS, et al. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020 doi: 10.1056/NEJMc2015630. published online May 19. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health and Social Care CMO for England announces first death of patient with COVID-19. March 5, 2020. https://www.gov.uk/government/news/cmo-for-england-announces-first-death-of-patient-with-covid-19
- 10.Prime Minister's Office Prime Minister's statement on coronavirus (COVID-19) March 16, 2020. https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-16-march-2020
- 11.Prime Minister's Office Prime Minister's statement on coronavirus (COVID-19) March 23, 2020. https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020
- 12.The National Archives The Health Protection (Coronavirus, Restrictions) (England) Regulations 2020. March 26, 2020. https://www.legislation.gov.uk/uksi/2020/350/introduction/made
- 13.Public Health England National ambulance syndromic surveillance: weekly bulletins 2020. June 23, 2020. https://www.gov.uk/government/publications/national-ambulance-syndromic-surveillance-weekly-bulletins-2020
- 14.Public Health England Emergency department syndromic surveillance system: England. June 23, 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/895219/EDSSSBulletin2020wk25.pdf
- 15.Pessoa-Amorim G, Camm CF, Gajendragadkar P, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020 doi: 10.1093/ehjqcco/qcaa046. published online May 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.British Cardiovascular Intervention Society Cardiology services during the coronavirus pandemic. March 23, 2020. https://www.bcis.org.uk/news/cardiology-services-during-the-covid-19-pandemic
- 17.NHS Digital . Stationery Office; Leeds: 2017. National clinical coding standards: OPCS-4 (2017), accurate data for quality information. [Google Scholar]
- 18.Wahl-Jorgensen K. Coronavirus: how media coverage of epidemics often stokes fear and panic. Feb 14, 2020. https://theconversation.com/coronavirus-how-media-coverage-of-epidemics-often-stokes-fear-and-panic-131844
- 19.Tam CF, Cheung KS, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herz N. Why are thousands fewer people being treated for a heart attack? April 23, 2020. https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/behind-the-headlines/coronavirus/coronavirus-and-reduction-in-heart-attack-treatment
- 21.Wright J. Coronavirus doctor's diary: is lockdown good for your heart? May 5, 2020. https://www.bbc.co.uk/news/health-52535044
- 22.Krumholz HM. Where have all the heart attacks gone? May 14, 2020. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html
- 23.Roffi M, Patrono C, Collet J-P, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 24.Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 25.Spaulding CM, Joly LM, Rosenberg A, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336:1629–1633. doi: 10.1056/NEJM199706053362302. [DOI] [PubMed] [Google Scholar]
- 26.Gorenek B, Lundqvist CV, Terradellas JB, et al. Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EHRA, ACCA, and EAPCI task force. EuroIntervention. 2014;10:1095–1108. doi: 10.4244/EIJY14M08_19. [DOI] [PubMed] [Google Scholar]
- 27.Bahit MC, Kochar A, Granger CB. Post myocardial infarction heart failure. JACC Heart Failure. 2018;6:179–186. doi: 10.1016/j.jchf.2017.09.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.