Background: During the coronavirus disease 2019 (COVID-19) pandemic, many health systems are postponing outpatient visits and shifting services to telehealth (1). However, the extent to which in-person visits have been reduced and replaced by telehealth visits remains unclear.
Objective: To describe changes in the number of in-person, telephone, and video visits at U.S. Department of Veterans Affairs (VA) outpatient facilities during the initial 10 weeks of the COVID-19 pandemic, both overall and stratified by VA clinic.
Methods and Findings: The VA is the largest health care provider in the United States and has implemented a robust COVID-19 plan in response to the pandemic. We analyzed data from the VA Corporate Data Warehouse, a national repository of electronic health records from visits to any VA facility that is updated nightly and has been previously assessed for reliability and accuracy (2).
The study population included the cohort of adults who visited any VA health care facility between 2008 and 2018. Outcomes included the weekly number of VA outpatient visits, stratified by in-person, telephone, and video visits (based on VA clinic stop codes) and by clinic (based on the substation identifier where the encounter occurred). We limited visits to those classified by the VA as a completed patient encounter, which requires that the provider interacted with the patient and documented a diagnosis or procedure code and treatment plan and that the VA counted the visit toward the provider's workload.
We described trends in weekly counts of each outcome during the first 20 weeks of 2016 to 2019 and of 2020. In addition, we reported changes in the count of each outcome during the initial 10-week pandemic period (weeks 11 to 20 of 2020, corresponding to 11 March to 19 May) versus the prior 10 weeks (weeks 1 to 10 of 2020, corresponding to 1 January to 10 March), both overall and by VA clinic.
Analyses were done in Stata, version 15 (StataCorp). The Subcommittee for Human Studies at the VA New York Harbor Healthcare System (#01413) approved this study and waived patient informed consent.
The number of in-person visits to a VA outpatient facility among patients in our cohort decreased from 18 898 656 in weeks 1 to 10 of 2020 to 8 408 268 in weeks 11 to 20, a reduction of 10 490 388 visits (−55.5%) (Figure 1). During the same period, the number of telephone visits increased from 2 539 685 to 6 070 362 (a 139.0% increase from weeks 1 to 10) and the number of video visits increased from 425 495 to 734 547 (a 72.6% increase from weeks 1 to 10). Overall, the total number of VA outpatient in-person and telehealth visits decreased from 21 863 836 in weeks 1 to 10 of 2020 to 15 213 177 in weeks 11 to 20, a reduction of 6 650 659 visits (−30.4%) (Figure 1). In contrast, the number of in-person, telephone, video, and overall outpatient visits did not change between weeks 1 to 10 and 11 to 20 of 2016 to 2019 (Figure 1).
Figure 1. Number of VA outpatient visits per week in 2016 to 2019 and 2020.
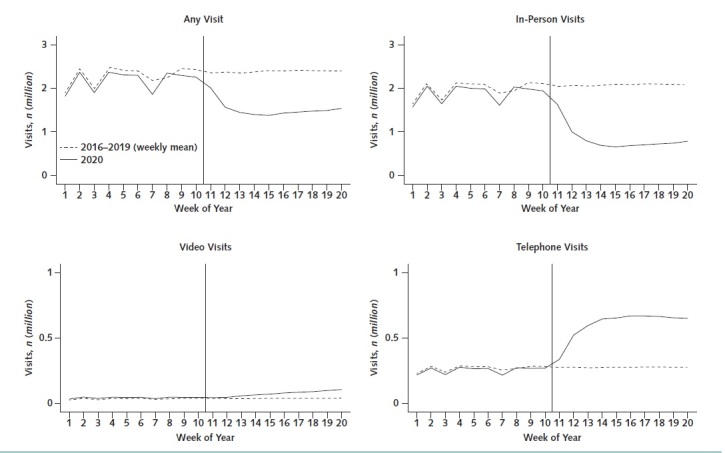
The solid line represents the total number of VA outpatient (any, in-person, video, and telephone) visits per week during 2020. The dashed line represents the weekly mean of the total number of VA outpatient (any, in-person, video, and telephone) visits per week in 2016 to 2019. Multiple outpatient records for the same person that shared the same date, clinic site, and primary clinic stop code were counted as 1 visit. The vertical line represents the week in 2020 when the COVID-19 pandemic began. COVID-19 = coronavirus disease 2019; VA = U.S. Department of Veterans Affairs.
Decreases in in-person visits and increases in telehealth visits were observed in 92.8% of VA clinics (Figure 2). Across clinics, the number of in-person visits declined by a median of −60.1% (interquartile range, −48.7% to −73.3%), and the number of telehealth visits increased by a median of 116.4% (interquartile range, 55.2% to 210.3%).
Figure 2. Percentage of change in in-person and telehealth outpatient visits during the COVID-19 pandemic, by VA clinic.
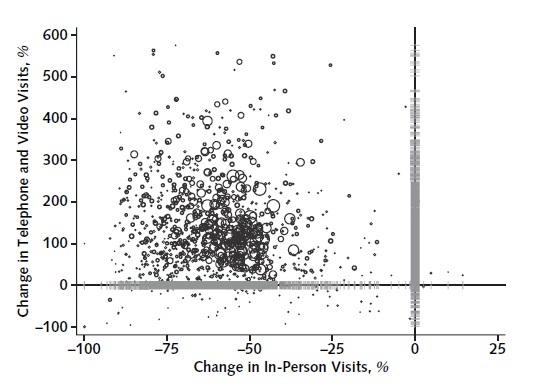
Each circle represents a clinic, and the area of the circle is proportionate to the clinic's size (defined as number of unique patients who visited the clinic during 2019). The horizontal gray lines along the y-axis show the univariate distribution of the percentage of change in telephone and video visits across clinics, and the vertical gray lines along the x-axis show the univariate distribution of the percentage of change in in-person visits across clinics. COVID-19 = coronavirus disease 2019; VA = U.S. Department of Veterans Affairs.
Discussion: In this retrospective study of adults using VA care, there were 10 490 388 fewer in-person visits to VA outpatient facilities during the initial 10 weeks of the COVID-19 pandemic than the preceding 10 weeks. The 56% decline in in-person visits was partly offset by a more than 2-fold increase in the number of telephone and video visits, but overall there was still a 30% decline in the number of outpatient visits. Limitations of this study include that veterans are predominantly male and older compared with the overall adult U.S. population and that we did not observe visits to non-VA providers. Further research is needed to understand how decreased access to in-person care and increased use of telehealth services during the pandemic may affect patient outcomes (3–5).
Footnotes
This article was published at Annals.org on 10 August 2020
References
- 1.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679-1681. [PMID: 32160451] doi:10.1056/NEJMp2003539 [DOI] [PubMed]
- 2.Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33:1203-11. [PMID: 25006147] doi:10.1377/hlthaff.2014.0054 [DOI] [PubMed]
- 3.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457-502. [PMID: 16202000] [DOI] [PMC free article] [PubMed]
- 4.Basu S, Berkowitz SA, Phillips RL, et al. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179:506-514. [PMID: 30776056] doi:10.1001/jamainternmed.2018.7624 [DOI] [PMC free article] [PubMed]
- 5.Baum A, Barnett ML, Wisnivesky J, et al. Association between a temporary reduction in access to health care and long-term changes in hypertension control among veterans after a natural disaster. JAMA Netw Open. 2019;2:e1915111. [PMID: 31722027] doi:10.1001/jamanetworkopen.2019.15111 [DOI] [PMC free article] [PubMed]


