Abstract
To reduce viral spread during the first months of the COVID-19 pandemic, most communities across the U.S. engaged in some form of stay-at-home restrictions or lockdowns that limited social interaction and movement outside the home. To determine the effect of these restrictions on suicidal ideation, a total of 3,120 individuals completed the Patient Health Questionnaire (PHQ-9) at one of three time points from April through June 2020. The percentage of respondents endorsing suicidal ideation was greater with each passing month for those under lockdown or shelter-in-place restrictions due to the novel coronavirus, but remained relatively stable and unchanged for those who reported no such restrictions. Public health policy and routine clinical care need to address the potential for increased suicidal thinking among those experiencing prolonged restrictions of normal social contact.
Dear editor,
Beginning in March 2020, the United States initiated nationwide efforts to contain the spread of the novel coronavirus, SARS-CoV-2. Because of the high transmissibility of the virus, communities across the nation rapidly implemented dramatic restrictions on human movement and activity. In the months since the initial outbreak, it has become clear that the pandemic and accompanying social restrictions have been associated with significant mental health consequences, including increased anxiety, stress, depression, and insomnia (Sher, 2020). Prolonged social isolation during the stay-at-home directives has been associated with increased loneliness (Killgore et al., 2020), and reduced interpersonal connectedness and social identity, potentially increasing the risk for suicide (Gratz et al., 2020). To assess the effects of prolonged lockdown/stay-at-home efforts on mental health, we collected data on suicidal ideation from a large sample of participants over a three-month period near the outset of the COVID-19 pandemic in the U.S.
Beginning in April 2020, we conducted three monthly cross-sectional data collections (total N=3,120) involving an online set of questionnaires that included the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001). The battery also included several measures of stress, psychopathology, political opinions, and attitudes surrounding the pandemic (not discussed here). Data were collected using the Amazon Mechanical Turk (MTurk) online crowdsourcing platform. The study was advertised on MTurk as a survey about individual perceptions of the COVID-19 pandemic, and participants were financially compensated for their time. Independent data collections occurred approximately one month apart (i.e., April 9-10, 2020, n=1,013 (reported previously in Killgore et al., 2020); May 11-14, 2020, n=1,037; June 10-13, 2020, n=1,070). Participants were English speaking adults from all 50 U.S. states and the District of Columbia (18-84 years old; 54.2% female; 45.3% male). Informed consent was obtained from all participants and the study was approved by the University of Arizona Institutional Review Board.
First, we determined the proportion of participants in each sample who reported they were “sheltering-in-place.” We found that self-reported lockdown restrictions declined over the three-month period (i.e., April=93.6%, May=78.8%, June=44.8%). To assess the effects of prolonged stay-at-home restrictions on mental health, particularly suicidal ideation, we collected responses to item 9 of the PHQ-9, which asks participants to consider how often they have been bothered in the past two weeks by: “thoughts that you would be better off dead, or hurting yourself in some way,” (“not at all”=0; “several days”=1; “more than half the days= 2; “nearly every day”=3). We first classified individuals as showing any evidence of suicidal ideation (item 9≥1). Additionally, we also identified those showing moderate to severe suicidal ideation (item 9≥2). The independent variables included month of assessment (April, May, or June 2020) and current stay-at-home status (i.e., “currently on a stay-at-home, shelter-in-place, or lockdown order,” or otherwise “currently sheltering-in-place”). Data were analyzed with a 2 (lockdown status) x 3 (month) between-groups analysis of variance (ANOVA).
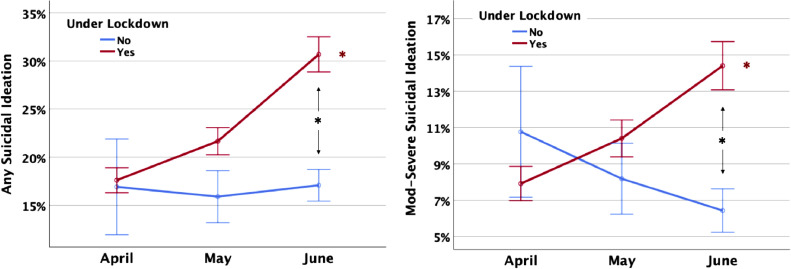
As evident in the left panel of Fig. 1 , there was a significant interaction between lockdown status and month of assessment on suicidal ideation (F 2,3114=3.60, p=.027, partial η 2=.002). Specifically, the percentage of individuals reporting any suicidal ideation did not differ across the three-month period for groups of individuals who were not under lockdown at the time of assessment (F 2,873=0.08, p=.923, partial η 2=.000), ranging from 15.9% in April to 17.1% in June. However, for those under lockdown or sheltering-in-place, the percentage of individuals reporting any suicidal ideation increased significantly over the three-month period, from 17.6% in April to 30.7% by June (F 2,2241=16.13, p<.00001, partial η 2=.014). The groups did not differ significantly in April or May, but the difference was highly significant by June (F 1,1068=28.15, p<.00001, partial η 2=.026).
Fig. 1.
Percentage of participants endorsing suicidal ideation on item 9 of the the PHQ-9 over the first three months since early COVID-19 lockdown/shelter-in-place restrictions. Left: The percentage of respondents endorsing any suicidal ideation (i.e., scores > 0). Right: The percentage of respondents endorsing moderate to severe suicidal ideation (i.e., scores ≥ 2). Red *p < .0001 for simple effect of month for those under lockdown. Black *p < .0001 lockdown between-group difference in June.
When considering only more severe levels of suicidal ideation (i.e., moderate to severe scores), we found essentially the same pattern reported above, with greater prevalence of suicidal ideation at later timepoints only for those self-reporting being under lockdown restrictions (Fig. 1, right). Specifically, there was a significant interaction between lockdown status and month of assessment on moderate to severe suicidal ideation (F 2,3114=4.37, p=.013, partial η 2=.003). For those who were not under lockdown at the time of the assessment, the percentage of moderate to severe suicidal ideation did not differ across the three monthly data collections (F 2,873=1.041, p=.354, partial η 2=.002), ranging from 10.8% in April to 6.4% in June. However, for those under lockdown, the percentage reporting suicidal ideation was 7.9% in April but was significantly higher (i.e., 14.4%) in June (F 2,2241=7.39, p<.001, partial η 2=.007). The difference between the lockdown and non-restricted groups only reached significance during the month of June (F 1,1068=18.99, p=.00001, partial η 2=.017).
It is also possible that the greater suicidal ideation observed for those under lockdown may actually have been driven by other factors, such as living in a region with higher pandemic impact (e.g., greater risk of infection or death, or greater financial impact), which would tend to coincide with greater shelter-in-place restrictions. To address these potential confounds, we re-ran the previous analyses again while statistically controlling for state location, fear of the virus, and primary job loss. These included dummy-coded covariates for state location, a 7-point Likert scale question about fear (i.e., “I am gravely afraid of catching the COVID-19 virus”), and a binary question asking “have you lost your primary job due to COVID-19.” However, even after controlling for these variables, the previously described effects remained significant (p<.05) for both analyses.
Prior research has suggested that suicidal ideation during the early weeks of the pandemic shutdown remained stable and was not significantly elevated, even though most people were staying at home (Bryan et al., 2020). Consistent with those findings, our data suggest that suicidal ideation in April was, in fact, similar between those who were sheltering-in-place and those who were not. After that time, however, there was a clear monthly trend toward increasing severity of suicidal ideation among those who reported sheltering-in-place. By June, the percentage of individuals reporting any suicidal ideation was 1.8 times greater among those under stay-at-home restrictions compared to those who were not, and the rate was 2.25 times greater for those indicating moderate to severe suicidal thinking.
The reasons why the increase in suicidal ideation would be most evident in those who are under stay-at-home restrictions are not entirely known, but emerging evidence suggests that the pandemic and lockdowns have been associated with increased depression, anxiety, and loneliness (Killgore et al., 2020), and it is not difficult to see how physical isolation may reduce meaningful aspects of social support, one's sense of purpose within the larger society, and hope for the future, all of which may affect outlook and suicidal thinking. Of course, there are limitations to our findings, including our reliance on self-report methods and cross-sectional data collection. Consequently, causality cannot be inferred from a naturalistic design of this type. Nonetheless, the findings raise the possibility that a significant number of individuals may be experiencing increased suicidal ideation during prolonged stay-at-home efforts.
By July 2020, there has been a resurgence of COVID-19, leading to a necessary reactivation of community restrictions in many locations, and there is a significant potential for these trends to persist or even increase in the months to come. Suicidal ideation needs to be considered as a serious public health issue during the pandemic. At a minimum, assessment for suicide should be included in routine clinical encounters, particularly for patients who are under lockdown or prolonged shelter-in-place restrictions. In the longer term, it will be important to consider effective ways to bolster social support, enhance connectedness through technology, and strengthen psychological resilience within the population, so that we are better able to maintain mental health during periods of prolonged social isolation.
Funding
None.
Declaration of Competing Interest
None.
References
- Bryan, C.J., Bryan, A.O., Baker, J.C., 2020. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID-19 pandemic. Suicide and life-threatening behavior. e12653, published online June 26. [DOI] [PMC free article] [PubMed]
- Gratz, K.L., Tull, M.T., Richmond, J.R., Edmonds, K.A., Scamaldo, K., Rose, J.P., 2020. Thwarted belongingness and perceived burdensomeness explain the associations of COVID-19 social and economic consequences to suicide risk. Suicide and life-threatening behavior, ahead of print, published online June 26. [DOI] [PMC free article] [PubMed]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020 doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]