Abstract
COVID-19 initially an epidemic caused by SARS-CoV-2 has turned out to be a life- threatening global pandemic with increased morbidity and mortality. The presence of cytokine storm has been linked with the pathogenesis of severe lung injury as evinced in COVID-19. Aquaporins (AQPs) are molecular water channels, facilitating water transport across the cell membrane in response to osmotic gradients. Impairment in alveolar fluid clearance due to altered functional expression of respiratory AQPs highlight their pathophysiological significance in pulmonary edema associated respiratory illness. Therefore, we hypothesize that targeted modulation of AQPs in lungs in the intervening period of time, could diminish the dreadful effects of inflammation- induced comorbidity in COVID-19.
Keywords: COVID-19, Cytokine storm, Inflammation, Pulmonary edema, Aquaporin, Aquaporin modulators
Abbreviations: ALI, Acute lung injury; AQP, Aquaporin; IL, Interleukin; INF, Interferon; KO, Knockout; LPS, Lipopolysaccharide; MAPK, Mitogen activated protein kinase; SARS-CoV-2, Severe acute respiratory syndrome corona virus 2; TGF, Transforming growth factor; TNF-α, Tumor necrosis factor alpha
Introduction
The end of December 2019 marked the beginning of the global COVID-19 pandemic with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel corona virus as its etiological agent. Coronaviruses are enveloped single stranded RNA virus with a genome which spans about 27–32 kb encoding the structural and non-structural proteins involved in their entry and replication within the host cell [1]. Based on their distribution in birds and mammals six species of corona virus are known to infect humans. Among them, two strains namely severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) both zoonotic origin and high pathogenicity were linked with global epidemic and fatal illness [2]. Following this thread, the SARS-CoV-2 has sparked the global anxiety through COVID-19 outbreak which at present lacks a permanent cure.
In late December 2019, a cluster of patients with pneumonia were reported in Wuhan, Hubei province, China by its local health facilities. Down the line an emergency response team by Chinese Centre for Disease Control was consigned to puzzle out its causative background and epidemiological incidence [3]. On 2 August 2020, reports published by World Health Organization (WHO) showed 17,660,523 confirmed cases globally which includes 680,894 deaths. Till now, the United States of America continues to be the epicenter with increasing cases followed by countries of Europe, South-East Asia, Eastern Mediterranean, Africa and Western Pacific [4]. Though SARS-CoV-2 has masked the world with COVID-19 pandemic featuring an increased fatality rate, several countries have managed to extricate themselves from the dreadful condition providing a ray of hope to the global community.
Based on its pathobiology, upon inhalation the spike protein of SARS-CoV-2 is likely to bind through its receptor binding domain to ACE- 2 (angiotensin converting enzyme 2) receptor largely found in type II alveolar cells [5]. Following its attachment to the target cell, RNA released by the virion undergoes replication, it multiplies and disseminates thereby infecting other cells in its proximity. Virus propagation down the respiratory tract alongside the conducting airways sets up a strong innate immune response within the host system. At this point the sputum and nasal swabs should contain the virus traces and markers of immune response. With all these happening together the disease is clinically manifested and the individual is regarded as COVID-positive [6].
COVID-19 affects different individuals through distinct ways. The human- human COVID-19 spread is speculated to take place via respiratory droplet transmission or unmediated contact with an infected person. Mild to severe scale symptoms might be elicited within 2–14 days after viral exposure. While symptoms like fever indications, shortness of breath and life-threatening pneumonia occurs, case reports of other respiratory, neurological, gastrointestinal and hepatic illness have also been witnessed [7]. Widespread reports claim elderly people with diminished immune response and individuals with diabetes, hypertension, kidney/ heart diseases or any underlying health conditions as susceptible population towards SARS-CoV-2 [2]. The presence of prominent airway inflammation and a rapidly progressive pulmonary edema are speculated to be one among the various reasons for COVID-19 related deaths.
Respiratory illness in COVID-19
Over the past years, the term ‘cytokine storm’ has been an arcane phenomenon intended to investigate the failure of the immune system in safeguarding the host organism. In the past few months, it has become increasingly apparent that calming of the cytokine storm during SARS-CoV-2 infection is the key to survival [8]. A hyperactive immune response is not exclusive only to COVID-19 also, cancer patients undergoing immunotherapy, individuals with autoimmune diseases or other infections are known to experience similar effects. Cytokine storm denotes a hyperactive immune response, characterized by the release of pro-inflammatory cytokines in superfluous levels being detrimental to cells. A loss of negative feedback on the immune system, creates a positive feedback on immune cells recruiting them in larger amounts with an exponential release of inflammatory key players, resulting in organ damage.
The main class of cytokines involved in this injurious event include interleukins, interferons, chemokines, tumor necrosis factor, colony stimulating factors and other growth factors. These molecules contain their own subclasses namely proinflammatory factors (like TNF, IFNγ, IL-1β, IL-6 and IL-12) and anti-inflammatory factors (such as TGF-β, IL-4, IL-10 and IL-13) that wholesomely showcases the inflammatory cascade amplifying the response. Within the total affected population at least 10% of patients with severe COVID-19 are reported to have lung injury, acute respiratory distress syndrome (ARDS) within 8 to 14 days after the onset of their illness. Respiratory illness in COVID-19 has been evidenced with a series of pathological findings in lung tissues such as inflammatory infiltration, alveolar edema and proteinaceous exudates, diffuse alveolar damage with wall thickening, hyaline membrane formation and pneumocyte desquamation [9]. The relevance of cytokine storm in COVID-19, fueling several deaths with respiratory collapse has gained immense attention that scientific researchers and medical experts are working on to tame the event.
The viral mediated inflammatory response in lungs comprises of epithelial inflammation and dysfunction, undermined surfactant activity and impaired alveolar fluid clearance [10]. Furthermore, conditions such as pneumonia, ARDS, sepsis and septic shock represent severe scale manifestations. Pneumonia, an agonizing lung infection causes the accumulation of exudative fluid in the pulmonary parenchyma imperiling the respiratory function. Inflammatory dysregulation is known to play a causative role in pneumonia where multiple risk factors of this condition might affect the inflammatory pathway that were designed to defend the lungs during infection [11]. ARDS signifies the progress of bilateral pulmonary infiltrates and hypoxemia which follows diffuse alveolar damage. Stimuli like pneumonia, sepsis etc. serve as a causative factor for ARDS. Precisely, the activation of innate immune response in alveoli triggers the release of proinflammatory cytokines and chemokines along with procoagulant factors, resulting in leukocyte recruitment into the alveolar air space. Within these injured alveoli, a paracrine signaling network established between various immune, epithelial and endothelial cells leads to altered permeability and alveolar fluid clearance that eventually results in lung edema [12].
Aquaporins in lung fluid homeostasis
Establishment of fluid homeostasis across the pulmonary epithelium serves as a prerequisite for appropriate functioning of lungs. Together, the formation and maintenance of multifunctional alveolar surface liquid determines the pulmonary physiology. Earlier, the mechanism of water transport across the alveolar epithelial cells were not fully understood. On the positive side, the transendothelial/ transepithelial water flux, a two-step process involving the transport of water through the endothelium, which separates vascular and interstitial compartment followed by water transport across the epithelium came into the limelight [13]. Convincingly, the osmotically driven transcellular water flux through a mercury sensitive water channel in intact sheep lungs unveiled the aquaporin (AQP) mediated water transport in lungs [14].
Identification of a 28 kDa channel forming integral membrane protein (CHIP) [15] expressed in Xenopus laevis oocytes laid the foreground for osmotically driven water permeability in cells, which was later titled ‘Aquaporins (AQPs)’ [16]. AQPs are ubiquitous membrane channel proteins involved in small solute and water transport in response to osmotic gradients. AQPs are known to exist as tetramers while structurally each 30 kDa monomer is made up of six bilayer spanning domain (H1-H6), with two helical segment or loop (HB and HE) partially tucked in opposite orientation into the lipid bilayer with their signature NPA (aspargine- proline- alanine) sequence containing motifs [17]. The AQP superfamily constitutes 13 isoforms (AQP0-12) and based upon their structure and functional features it has been divided into three subfamilies: orthodox/classical aquaporins (AQP0, AQP1, AQP2, AQP4, AQP5) that are strictly water permeable, aquaglyceroporins (AQP3, AQP7, AQP9, AQP10) in addition to water, transports glycerol, urea and other small sized non electrolytes and unorthodox/superaquaporins (AQP6, AQP8, AQP11, AQP12) involved in transport of small uncharged solutes [18].
Out of all AQP isoforms four of them namely AQP1, AQP3, AQP4 and AQP5 are localized in lungs and airways (Table 1 ), and their expression pattern here signifies distinct physiological role in pulmonary fluid maintenance. AQP1 the first isoform to be identified in lung, is expressed in microvascular endothelial cells adjacent to airways and alveoli, in microvessels and mesothelial cells of parietal and visceral pleura. Basal epithelial cells of large airways and nasopharynx are known to express AQP3 in their basolateral membrane and also in human small airway epithelia. AQP4 expression is seen at the basolateral membrane of ciliated columnar epithelial cells of trachea, bronchus and nasopharyngeal region. Type I alveolar epithelial cells of distal lung and acinar cells of nasopharyngeal subepithelial gland shows significant expression of AQP5 on their apical membrane [19]. The tissue, cell specific distribution of AQPs along with their functional characterization have gained considerable scientific interest to investigate their involvement in pathological conditions.
Table 1.
Tissue-cell specific localization of AQPs in lung.
| S.No | AQP isoform | Localization | Reference |
|---|---|---|---|
| 1 | AQP1 | Airways and alveoli- microvascular endothelial cells; Parietal and visceral pleura- microvessels and mesothelial cells. | [19] With original references cited therein. |
| 2 | AQP3 | Large airways and nasopharynx- basolateral membrane of basal epithelial cells; human small airway- epithelia. | |
| 3 | AQP4 | Trachea, bronchus and nasopharyngeal region- basolateral membrane of ciliated columnar epithelial cells. | |
| 4 | AQP5 | Nasopharyngeal subepithelial glands- apical membrane of acinar cells; distal lung- apical membrane of type-I alveolar epithelium |
So far, the proposed AQP inhibitors being mercury compounds are found to be toxic for in- vivo usage. In such a case, lack of reliable AQP inhibitors set the scene for using specific AQP deficient animal models defining their phenotypical changes. Transgenic mice model generated via targeted gene disruption of major lung AQPs signifies their physiological role in pulmonary fluid maintenance. Inference from few AQP knockout (KO) studies in lungs with available relevant literature is summarized in Table 2 .
Table 2.
AQP KO studies in animals highlighting their role in pulmonary water transport.
| S.No | AQP isoform | Experimental model | Study outcomes | Related implications | References |
|---|---|---|---|---|---|
| 1 | AQP1 | Mice lung microvascular endothelial cells | A 10-fold decrease in airspace- capillary osmotic water permeability (Pf) compared to wild-type (WT) and decreased lung fluid accumulation. | AQP1 is involved in transcellular water transport and facilitates hydrostatically driven lung edema. | [20] |
| 2 | AQP1/AQP4 Double KO |
Mice lung microvascular endothelial cells | AQP4KO mice showed no significant effect whereas deletion of AQP4 in AQP1 KO mice showed a 15.3-fold decrease in Pf compared to WT. | AQP4 along with AQP1 contributed to airspace capillary permeability. | [21] |
| 3 | AQP1/AQP5 Double KO |
Mice type I alveolar epithelial cells | AQP5KO mice showed a 10-fold decrease in Pf of airspace- capillary barrier and further 2 to 3-fold reduction in AQP1/AQP5 double KO mice compared to WT. | AQP5 is essential for majority of water transport across the apical surface of alveolar epithelium. | [22] |
Role of aquaporins in lung inflammation and edema
Numerous mechanisms are known to functionally coexist during the clearance of edema from the distal spaces of lung. In context of pulmonary inflammation in mice lung, induced by intratracheal adenoviral infection showed increased mRNA expression of TNF-α and IFN-γ. Histological examination revealed inflamed alveolar wall thickening along with presence of enlarged peribronchial and perivascular spaces consistent with pulmonary edema. Secondly, mRNA and protein expression of AQP1 and AQP5 were decreased significantly. Decrease in both of these isoforms might contribute to edema by reducing the rate of excess water removal resulting in water containment within the alveolar and interstitial spaces [23]. Pseudomonas aeruginosa (PA) induced lung injury in wild type mice showed decreased AQP5 mRNA and protein expression. When compared with the wild type, AQP5 knock out mice exhibited severe lung injury with increased wet/dry weight ratio and endothelial permeability thereby concluding the fact that deletion of AQP5 aggravated the progression of acute lung injury (ALI) [24].
Studies by Gabazza et al., explored the relationship between AQP5 and lung fibrosis. Both AQP5 protein and mRNA expression was downregulated in bleomycin induced lung fibrosis condition. Probably this might be due to chronic lung injury by bleomycin and the decrease in expression of AQP5 might have caused a persistent and chronic pulmonary edema with successive development of lung fibrosis [25]. Experiments with lungs of aged mice showed an altered water transport associated with AQP1 and AQP5 downregulation. The capillary- airway osmotic water transport rate was decreased with significant reduction in lung water accumulation indicating a slower hydrostatically driven lung edema formation [26]. Type II alveolar epithelial cells exposed to hyperoxic condition showed significant increase in expression levels of AQP1 with increased cell volume. This indicates the enhanced water transport as a compensatory mechanism to improvise body’s internal environment. Furthermore, prolonged exposure to a high oxygen atmosphere might have gradually aggravated the lung injury downregulating AQP1 resulting in water transport dysfunction [27].
Aquaporin modulators in lung inflammation and edema: Promising drugs for COVID-19 comorbidity
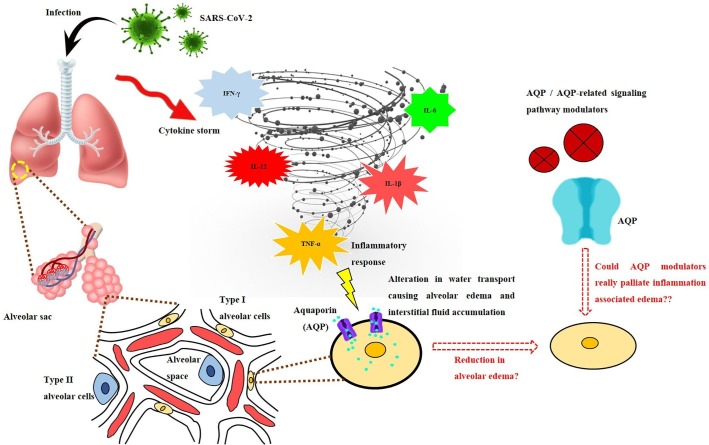
The above- mentioned scientific data unfolds the involvement of AQPs implicating their expressional pattern during pulmonary inflammation, fluid accumulation and clearance. Now the conception, whether direct modulation of AQPs or their related signaling pathway by small molecule inhibitors or modulators could palliate the pathological outcomes of inflammation and associated edema needs to be reviewed (Fig. 1 ).
Fig. 1.
An illustration of hypothesis whether aquaporin (AQP) modulation in lungs could reduce the impact of COVID-19 illness. The cytokine storm effectuated by SARS-CoV-2 sets up a hyperactive immune response with inflammatory mediators at superfluous levels altering AQP expression and associated water movement. Direct modulation of AQPs or their related signaling pathways via small molecule inhibitors/ other modulators could alleviate pulmonary edema formation and interstitial fluid accumulation thereby diminishing the ill-effects of COVID-19 comorbidity.
Mice with LPS induced ALI, when treated with TGN-020 an AQP4 inhibitor showed significant decrease in levels of proinflammatory cytokines, a less severe alveolar wall collapse with reduced inflammatory infiltrates and improved survival rate. Inhibition of IL-17A by downregulating PI3K/Akt signaling with an upregulated SOCS3 protein expression is speculated to be the reason behind the alleviation of ALI [28]. Similarly AQP4 inhibition by TGN-020 in irradiation induced lung injury model was shown to attenuate the progression and severity of lung injury by lowering the expression of proinflammatory cytokines (namely IL-6, IL-17, and TGF-β), chemokines (MIP1a and MCP1), fibrosis related (Col3al and Fn1) genes and inhibiting the activation of M2 macrophages [29].
Modulation of intracellular signaling pathway by inhibiting a focal point, p38 mitogen activated protein kinase (MAPK) by SB239063 in intestinal ischemia reperfusion lung injury, resulted in a decrease in AQP4 expression with subsiding interstitial edema and congestion [30]. Likewise, in primary rat pleural mesothelial cells, a p38 MAPK inhibitor SB203580 halted AQP1 downregulation caused by staphylococcal peptidoglycan (PGN) which might result in functional insufficiency of AQP1 leading to inadequate water transport and accumulation of pleural fluid. [31].
Development of pulmonary edema in lungs of mice with fat embolism syndrome (FES) was reversed by bumetanide (AqB013) an inhibitor of AQP1 and acetazolamide. Furthermore in vitro studies with SB203580 in pulmonary microvascular endothelial cells (PMVEC’s) revealed that free fatty acids induced upregulation of AQP1 was mediated through MAPK signalling pathway [32]. Anti-asthmatic agents like dexamethasone, ambroxol, and terbutaline alleviated pulmonary edema in mouse lungs with ovalbumin (OVA) induced asthma by increasing AQP1 and AQP5 expression. Dexamethasone and ambroxol were known to decrease eosinophilic infiltration, mucus secretion and pulmonary edema while terbutaline only improved the edematic condition [33].
In LPS induced ALI, CGRP8-37 an antagonist of α- calcitonin- gene related peptide receptor significantly decreased AQP1 expression than AQP5 aggravating the development of lung injury through elevated cytokine (IL-1β, IL-10, and TNF-α) release and interstitial edema formation resulting in pulmonary fluid accumulation [34]. Silencing of AQP1 by RNA interference technique (RNAi) in human pulmonary adenocarcinoma A549 cells attenuated the fluid transport capacity into intracellular regions with reduction in osmotic water permeability and cell volume. This disturbance in alveolar fluid clearance might serve as a key factor for developing hyperoxic lung edema [35].
Lipoxine A4 (LXA4) a braking signal in inflammatory response reduced the severity of inflammation and restored alveolar fluid clearance via upregulation of AQP5 in LPS induced lung tissue exhibiting its pro-resolution and anti- edematic activity in alleviating ALI [36]. Inhibition of NF-κB activation by fasudil a selective Rho- kinase (ROCK) inhibitor in LPS induced lung injury restored the expression of AQP5 resulting in predominant reduction in lung water content and pulmonary edema formation [37]. Upregulation of AQP1 and AQP5 expression by dobutamine, a synthetic beta-adrenergic receptor agonist resulted in decreased levels of cytological inflammatory markers and increased alveolar fluid clearance in LPS treated rats leading to resolution of pulmonary edema [38]. Tanshinol a plant-based polyphenol exhibited its protective role in sepsis by upregulating AQP5 expression. Downregulating the expression of proinflammatory cytokines such as TNF-α and IL-6, and subsequent phosphorylation of p38 ameliorated sepsis induced damage to lung tissue [39]. Dose dependent administration of dexmedetomidine inhibited the increase in plasma levels of TNF-α and IL-1β induced by LPS upregulating AQP1 and AQP5 expression alleviating the development of lung edema [40].
Despite of compulsive opportunities available, only a little progress has been witnessed in the field of AQP based therapeutics. The broad range of tissue expression and physiological involvement of various AQP isoforms in glandular fluid secretion, urine concentration, brain water balance, neural function, skin hydration, etc. features them as an important therapeutic target whose modulation might help in the treatment several pathological conditions. Previously, the relevance of AQP4 and AQP2 in treatment strategies for neuromyelitis optica (NMO) and nephrogenic diabetes insipidus (NDI) respectively have been patented. Identifying the utility of small molecule inhibitors/ modulators of AQP function will provide therapeutic resources for treating the comorbidities of inflammation centered COVID-19. In this view, future experiments are needed to validate the proposed salutary effect of AQP- specific modulators for developing AQP- based therapeutics in treating COVID-19 associated comorbidities.
Conclusion
Since the first news on COVID-19 outbreak, an inherent cautious optimism has been instilled among people everywhere. The burden of this pandemic creates a notion that the killer is not the virus but the immune response itself. The scientific community continues to make every effort curtailing this biological catastrophe and improving the survival rate. Increased extravasation of fluid across endothelium or decreased clearance of fluid from the interstitial space contributes to fluid accumulation. The involvement of AQPs in edema formation and resolution in various inflammatory models has been documented earlier. Considering AQPs as elusive drug targets and modulating their respiratory expression levels will help to mitigate the inflammation induced comorbidity in COVID-19.
Author contributions
LFMA: Conceptualization and initial draft. CP: Design and supervision. CP, KA, AK, AP, CL: Critical revision and suggestions. All authors discussed and approved the final manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
LFMA gratefully acknowledge financial assistance as Junior Research Fellowship (IF180563) from Department of Science and Technology (DST) – Innovation in Science Pursuit for Inspired Research (INSPIRE). CP acknowledges Department of Science and Technology (DST) – Science and Engineering Research Board (SERB) for the financial assistance (EMR/2017/003670) and DST-FIST for the infrastructure provided to the Department of Biochemistry, Bharathidasan University. AK acknowledges the financial assistance as Senior Research Fellowship (RBMH/FW/2018/13) from Indian Council for Medical Research (ICMR), New Delhi.
References
- 1.Li F. Structure Function, and evolution of coronavirus spike proteins. Ann Rev Virol. 2016;3:237–261. doi: 10.1146/annurev-virology-110615-042301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gralinski L.E., Menachery V.D. Return of the coronavirus: 2019-nCoV. Viruses. 2020;12:135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization, Coronavirus disease 2019 (COVID-19), WHO, Geneva (2020). Situation Report 195. (https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200802-covid-19-sitrep-195.pdf?sfvrsn=5e5da0c5_2 accessed on 2 August 2020).
- 5.Wan Y., Shang J., Graham R., Baric R.S., Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS Coronavirus. J Virol. 2020;94:e00127–e220. doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mason R.J. Pathogenesis of COVID-19 from a cell biology perspective. Eur Respir J. 2020;55:2000607. doi: 10.1183/13993003.00607-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shanmugaraj B., Siriwattananon K., Wangkanont K., Phoolcharoen W. Perspectives on monoclonal antibody therapy as potential therapeutic intervention for Coronavirus disease-19 (COVID-19) Asian Pac J Allergy Immunol. 2020;38:10–18. doi: 10.12932/AP-200220-0773. [DOI] [PubMed] [Google Scholar]
- 8.Ragab D., Salah Eldin H., Taeimah M., Khattab R., Salem R. The COVID-19 Cytokine Storm; What We Know So Far. Front Immunol. 2020;11:1446. doi: 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lan J., Ge J., Yu J., Shan S. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 10.Thompson B.T., Chambers R.C., Liu K.D. Acute Respiratory Distress Syndrome. N Engl J Med. 2017;377:562–572. doi: 10.1056/NEJMra1608077. [DOI] [PubMed] [Google Scholar]
- 11.Quinton L.J., Walkey A.J., Mizgerd J.P. Integrative Physiology of Pneumonia. Physiol Rev. 2018;98:1417–1464. doi: 10.1152/physrev.00032.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herrero R., Sanchez G., Lorente J.A. New insights into the mechanisms of pulmonary edema in acute lung injury. Ann Transl Med. 2018;6:32. doi: 10.21037/atm.2017.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wittekindt O.H., Dietl P. Aquaporins in the lung. Pflugers Arch. 2019;471:519–532. doi: 10.1007/s00424-018-2232-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Folkesson H.G., Matthay M.A., Hasegawa H., Kheradmand F., Verkman A.S. Transcellular water transport in lung alveolar epithelium through mercury-sensitive water channels. Proc Natl Acad Sci U S A. 1994;91:4970–4974. doi: 10.1073/pnas.91.11.4970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Preston G.M., Agre P. Isolation of the cDNA for erythrocyte integral membrane protein of 28 kilodaltons: member of an ancient channel family. Proc Natl Acad Sci U S A. 1991;88:11110–11114. doi: 10.1073/pnas.88.24.11110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Preston G.M., Carroll T.P., Guggino W.B., Agre P. Appearance of water channels in Xenopus oocytes expressing red cell CHIP28 protein. Science. 1992;256:385–387. doi: 10.1126/science.256.5055.385. [DOI] [PubMed] [Google Scholar]
- 17.Agre P., Preston G.M., Smith B.L. Aquaporin CHIP: the archetypal molecular water channel. Am J Physiol. 1993;265:F463–F476. doi: 10.1152/ajprenal.1993.265.4.F463. [DOI] [PubMed] [Google Scholar]
- 18.Meli R., Pirozzi C., Pelagalli A. New Perspectives on the Potential Role of Aquaporins (AQPs) in the Physiology of Inflammation. Front Physiol. 2018;9:101. doi: 10.3389/fphys.2018.00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Borok Z., Verkman A.S. Lung edema clearance: 20 years of progress: invited review: role of aquaporin water channels in fluid transport in lung and airways. J Appl Physiol. 2002;93:2199–2206. doi: 10.1152/japplphysiol.01171.2001. [DOI] [PubMed] [Google Scholar]
- 20.Bai C., Fukuda N., Song Y., Ma T., Matthay M.A., Verkman A.S. A, Lung fluid transport in aquaporin-1 and aquaporin-4 knockout mice. J Clin Invest. 1999;103:555–561. doi: 10.1172/JCI4138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song Y., Ma T., Matthay M.A., Verkman A.S. Role of aquaporin-4 in airspace-to-capillary water permeability in intact mouse lung measured by a novel gravimetric method. J Gen Physiol. 2000;115:17–27. doi: 10.1085/jgp.115.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma T., Fukuda N., Song Y., Matthay M.A., Verkman A.S. Lung fluid transport in aquaporin-5 knockout mice. J Clin Invest. 2000;105(2000):93–100. doi: 10.1172/JCI8258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Towne J.E., Harrod K.S., Krane K.C.M., Menon A.G. Decreased expression of aquaporin (AQP)1 and AQP5 in mouse lung after acute viral infection. Am J Respir Cell Mol Biol. 2000;22:34–44. doi: 10.1165/ajrcmb.22.1.3818. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Z.Q., Song Y.L., Chen Z.H., Shen Y., Bai C.X. Deletion of aquaporin 5 aggravates acute lung injury induced by Pseudomonas aeruginosa. J Trauma. 2011;71:1305–1311. doi: 10.1097/TA.0b013e3182128528. [DOI] [PubMed] [Google Scholar]
- 25.Gabazza E.C., Kasper M., Ohta K. Decreased expression of aquaporin-5 in bleomycin-induced lung fibrosis in the mouse. Pathol Int. 2004;54:774–780. doi: 10.1111/j.1440-1827.2004.01754.x. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y.W., Bi L.T., Hou S.P., Zhao X.L., Song Y.L., Ma T.H. Reduced lung water transport rate associated with downregulation of aquaporin-1 and aquaporin-5 in aged mice. Clin Exp Pharmacol Physiol. 2009;36:734–738. doi: 10.1111/j.1440-1681.2009.05156.x. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Q.Y., Fu J.H., Xue X.D. Expression and function of aquaporin-1 in hyperoxia-exposed alveolar epithelial type II cells. Exp Ther Med. 2014;8:493–498. doi: 10.3892/etm.2014.1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guo C., Wu T., Zhu H., Gao L. Aquaporin 4 blockade attenuates acute lung injury through inhibition of Th17 cell proliferation in mice. Inflammation. 2019;42:1401–1412. doi: 10.1007/s10753-019-01002-4. [DOI] [PubMed] [Google Scholar]
- 29.Li Y., Lu H., Lv X., Tang Q., Li W., Zhu H. Blockade of aquaporin 4 inhibits irradiation-induced pulmonary inflammation and modulates macrophage polarization in mice. Inflammation. 2018;41:2196–2205. doi: 10.1007/s10753-018-0862-z. [DOI] [PubMed] [Google Scholar]
- 30.Xiong L.L., Tan Y., Ma H.Y. Administration of SB239063, a potent p38 MAPK inhibitor, alleviates acute lung injury induced by intestinal ischemia reperfusion in rats associated with AQP4 downregulation. Int Immunopharmacol. 2016;38:54–60. doi: 10.1016/j.intimp.2016.03.036. [DOI] [PubMed] [Google Scholar]
- 31.Liu L., Du L., Chen Y. Down-regulation of Aquaporin1 (AQP1) by peptidoglycan via p38 MAPK pathways in primary rat pleural mesothelial cells. Exp Lung Res. 2014;40:145–153. doi: 10.3109/01902148.2013.859333. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Y., Tian K., Wang Y., Zhang R., Shang J., Jiang W. The Effects of Aquaporin-1 in pulmonary edema induced by fat embolism syndrome. Int J Mol Sci. 2016;17:1183. doi: 10.3390/ijms17071183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dong C., Wang G., Li B., Xiao K., Ma Z., Huang H. Anti-asthmatic agents alleviate pulmonary edema by upregulating AQP1 and AQP5 expression in the lungs of mice with OVA-induced asthma. Respir Physiol Neurobiol. 2012;181:21–28. doi: 10.1016/j.resp.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 34.Hong-Min F., Chun-Rong H., Rui Z., Li-Na S., Ya-Jun W., Li L. CGRP 8–37 enhances lipopolysaccharide-induced acute lung injury and regulating aquaporin 1 and 5 expressions in rats. J Physiol Biochem. 2016;73:381–386. doi: 10.1007/s13105-017-0563-3. [DOI] [PubMed] [Google Scholar]
- 35.Zhang Q., Fu J., Xue X. Inhibition of the expression of aquaporin–1 by RNA interference in pulmonary epithelial cells and its effects on water transport. Mol Med Rep. 2016;13:281–286. doi: 10.3892/mmr.2015.4519. [DOI] [PubMed] [Google Scholar]
- 36.Ba F., Zhou X., Zhang Y. Lipoxin A4 ameliorates alveolar fluid clearance disturbance in lipopolysaccharide-induced lung injury via aquaporin 5 and MAPK signaling pathway. Thorac Dis. 2019;11:3599–3608. doi: 10.21037/jtd.2019.08.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J.J., Kong H., Xu J., Wang Y.L., Wang H., Xie W.P. Fasudil alleviates LPS-induced lung injury by restoring aquaporin 5 expression and inhibiting inflammation in lungs. J Biomed Res. 2019;33:156–163. doi: 10.7555/JBR.31.20170024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu X.M., Wang H.Y., Li G.F., Zang B., Chen W.M. Dobutamine enhances alveolar fluid clearance in a rat model of acute lung injury. Lung. 2009;187:225–231. doi: 10.1007/s00408-009-9155-5. [DOI] [PubMed] [Google Scholar]
- 39.Xu J., Yang L., Dong L. Tanshinol upregulates the expression of aquaporin 5 in lung tissue of rats with sepsis. Oncol Lett. 2018;16:3290–3296. doi: 10.3892/ol.2018.9026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiang Y.X., Dai Z.L., Zhang X.P., Zhao W., Huang Q., Gao L.K. Dexmedetomidine alleviates pulmonary edema by upregulating AQP1 and AQP5 expression in rats with acute lung injury induced by lipopolysaccharide. J Huazhong Univ Sci Technolog Med Sci. 2015;35:684–688. doi: 10.1007/s11596-015-1490-6. [DOI] [PubMed] [Google Scholar]