Abstract
Emerging data show that the health and economic impacts of COVID-19 are being disproportionately borne by individuals who are not only biologically, but also socially vulnerable. Based on preliminary data from Sweden and other reports, in this paper we propose a conceptual framework whereby different factors related to biological and social vulnerability may explain the specific COVID-19 burden among older people. There is already some evidence showing large social disparities in the prevention, treatment, prognosis and/or long-term consequences of COVID-19. The remaining question is to what extent these affect older adults specifically. We provide the rationale to address this question with scientific methods and proper study designs, where the interplay between individuals’ biomedical status and their social environment is the focus. Only through interdisciplinary research integrating biological, clinical and social data will we be able to provide new insights into the SARS-CoV-2 pandemic and inform actions aimed at reducing older adults’ vulnerability to COVID-19 or other similar pandemics in the future.
Keywords: COVID-19, aging, social disparities
1. Introduction
COVID-19 has a clear predilection for aged people. Up to one quarter of the deaths due to COVID-19 have been in older people aged 70-79 years and up to two thirds in those over 80 years, regardless of the incidence of the disease or the completeness in the ascertainment of deaths across countries (Table 1 ). However, we know that “age” is a summary measure of life-long biological, physiological and functional changes partly determined by and in strong interplay with external social, physical, cultural and economic forces. In fact, emerging data show that the health and economic impacts of the virus are being disproportionately borne by people with a poor socioeconomic background.
Table 1.
Cumulative deaths due to COVID-19 by country as of 1-19 May 2020 (depending on the country).
| Country | Age group |
|||||||
|---|---|---|---|---|---|---|---|---|
| <60 years |
60-69 years |
70-79 years |
80+ years |
|||||
| % of all deaths | Death rate / 100,000 | % of all deaths | Death rate / 100,000 | % of all deaths | Death rate / 100,000 | % of all deaths | Death rate / 100,000 | |
| Denmark | 2.90 | 0.37 | 9.62 | 7.99 | 28.49 | 27.82 | 58.98 | 119.34 |
| England & Wales | 7.14 | 5.55 | 10.52 | 59.05 | 23.39 | 167.77 | 58.96 | 702.95 |
| France | 6.46 | 2.30 | 11.96 | 26.14 | 22.68 | 69.66 | 58.90 | 247.80 |
| Germany | 4.49 | 0.60 | 9.19 | 7.08 | 22.43 | 23.15 | 63.88 | 94.00 |
| Italy | 4.68 | 3.32 | 10.46 | 43.26 | 27.49 | 139.82 | 57.37 | 401.89 |
| Netherlands | 3.10 | 1.38 | 8.21 | 22.44 | 27.28 | 102.42 | 61.42 | 439.40 |
| Norway | 4.29 | 0.24 | 7.73 | 3.09 | 22.75 | 12.16 | 65.24 | 65.88 |
| Portugal | 4.33 | 0.73 | 8.98 | 8.70 | 19.49 | 25.19 | 67.20 | 126.69 |
| Spain | 4.72 | 2.54 | 8.84 | 31.62 | 24.17 | 117.09 | 62.27 | 411.19 |
| Sweden | 3.53 | 1.56 | 5.95 | 18.22 | 21.74 | 74.62 | 68.78 | 435.39 |
Source: own elaboration based on publicly available data from the French Institute for Demographic Studies, INED (https://dc-covid.site.ined.fr/en/), and the Swedish National Board of Health and Welfare (https://www.socialstyrelsen.se/statistik-och-data/statistik/statistik-om-covid-19/statistik-over-antal-avlidna-i-covid-19/)
2. Social vulnerability for COVID-19 – First evidence
Recent statistics from health authorities in e.g. New York (The New York Times, 2020), Barcelona (Dell’Olmo et al., 2020) and even Stockholm (The Local, 2020) reveal how the coronavirus outbreak appears to affect immigrant communities and lower-income neighbourhoods the hardest. Death records currently show that African Americans account for more than half of those who have died from the novel coronavirus in cities like Philadelphia or Chicago, far in excess of their representation in the general population. In the UK, early research has shown that the proportion of non-white patients in intensive care units was 2.3 times greater than their share in the general population (The Guardian, 2020), and that people living in more deprived areas have experienced COVID-19 mortality rates more than double those in less deprived areas (Iacobucci, 2020).
Most of the information on social differences in COVID-19 pandemic comes from media reports based on anecdotal or other ad hoc data (Table 2 ). Moreover, the real magnitude of the inequalities is likely to be underestimated due to the inexistence of accurate socioeconomic and ethnicity data across many local authorities and care services (Politico, 2020). Fortunately, scientific inquiries into these questions have already begun. For instance, a range of social indicators such as population density, ethnic diversity, urban/rural setting, level of education, lifestyle and living conditions that can be inferred from people’s area of residence are now starting to be linked to different health and well-being outcomes. Early findings from geographic modelling performed in the US indicate that income inequality was an influential factor in explaining COVID-19 incidence rates across counties (Mollalo et al., 2020).
Table 2.
Examples of social disparities in COVID-19 risk.
| Country, city | Indicator(s) of social vulnerability | Unit of analysis | Outcome | Finding |
|---|---|---|---|---|
| US (APM Research Lab, 2020) | Black ethnicity | State | Death rate from COVID-19 | 2.2 times higher than for Latinos, 2.3 times higher than for Asians, and 2.6 times higher than for Whites |
| US, New York (NYC Department of Health and Mental Hygiene, 2020) | Race minority, income, education level | Borough | Incidence rate, death rate from COVID-19 | 2.0 times higher in poorest vs wealthiest districts |
| UK, England and Whales (UK Office for National Statistics, 2020a) | Index of multiple deprivation | Lower-layer Super Output Areas | Age-standardised death rate from COVID-19 | 1.9 times higher in the most vs least deprived areas |
| UK, England and Whales (UK Office for National Statistics, 2020b) | Occupation | Individual | Age-standardised death rate from COVID-19 | 2.2 times higher in men working in the lowest skilled occupations compared to people of the same sex and age |
| Spain, Madrid (RE-HAB, 2020) | Overcrowding and age | District | Incidence rate | 22% of the variability explained by these indicators |
| Spain, Barcelona (Dell’Olmo et al., 2020) | Income | Neighbourhood | Incidence rate | 26% higher incidence rate in richest vs poorest neighbourhoods |
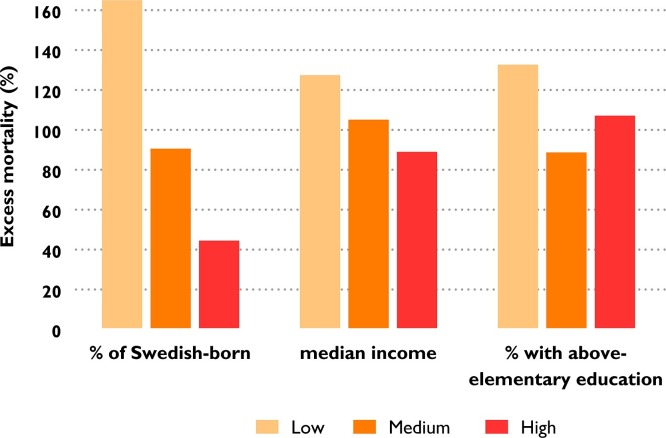
Similarly, preliminary analyses based on publicly available data from Stockholm region (Sweden) show differences in excess mortality for COVID-19 across community measures of country of birth, median income and education one month after the outbreak (Fig. 1 ).
Fig. 1.
Average excess mortality in the 26 municipalities of Stockholm region (Sweden) by levels (low, medium and high tertile) of socioeconomic indicators.
Note: excess mortality calculated comparing the mortality rate between 1-10 April 2020 with the average mortality rate recorded for the corresponding 10-day period during the two previous years. Income refers to employment (acquisition) income. Source: own elaboration based on publicly available data from Statistics Sweden (https://www.scb.se/).
3. Social vulnerability for COVID-19 – Several pathways
Some preliminary data show that social disparities related to COVID-19 take place at different time windows of the disease process. Social differences have been reported in the prevention of the contagion, in the care of the disease and related comorbidities, and in the prognosis and long-term consequences of the infection (Table 3 ). This could be especially relevant for those individuals who experience both a social and biological vulnerability, as is the case of an important share of the older population.
Table 3.
Social vulnerability for COVID-19 through different pathways acting at different time windows of the disease process.
| Prevention of contagion | Care of COVID-19 & comorbidities | Prognosis and long-term consequences |
|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
3.1. Disparities in the prevention of contagion
Social disparities in awareness of the risks and adoption of preventive measures, such as hand hygiene and physical distancing, can be attributed to the shortage of information adapted for minority languages and the unequal access to Internet. These barriers are exacerbated in the communities of older adults, frequently characterized by lower health- and technological literacy. In a survey of more than 600 socio-demographically diverse adults living in Chicago, those who were black, were living below the poverty level, or had low health literacy were less likely to believe that they might become infected; black respondents also felt less prepared for an outbreak than white adults (Wolf et al., 2020).
People in worse socioeconomic circumstances are more likely to experience overcrowding in the household, and it is also more common that different generations cohabit together. The type of jobs that lower-income people tend to have (e.g. care services, transportation, food and restaurant businesses) also put them, and their often cohabiting parents, at an increased risk of contagion, since they are difficult to perform from home and often require proximity with the client. Following quarantine orders could be particularly challenging for those living in smaller, shared, or cramped accommodations. In certain cultures, socially isolating older family members may be viewed as abandonment and will therefore be difficult to adhere to.
Coronavirus testing seems to be socially patterned, too. For example, in Philadelphia (US), individuals living in higher-income communities are reported to have been tested for COVID-19 six times more often than those in lower-income neighbourhoods (The Philadelphia Inquirer, 2020). This is mainly because, for most testing sites, testing is performed from a car and with a referral from the primary care physician to get tested. Many in Philadelphia’s lower-income black neighbourhoods do not have primary care physicians, let alone a car.
3.2. Care disparities for COVID-19 and comorbidities
General access to healthcare has been shown to vary widely across socioeconomic groups. This will be especially relevant in countries without universal health care systems and where large numbers of under- or uninsured people are concentrated in certain areas. In the US, many uninsured patients have been faced with substantial medical billings (The Commonwealth Fund, 2020) or even denied healthcare (Independent, 2020) for COVID-19 treatment. Besides the ease of access to health services, care outcomes may have been influenced by different healthcare system models, and the level of development of primary care, public health, and community medicine, all of which closely interact with individual biological and social factors.
In the context of a shortage of hospital beds, intensive care unit beds and ventilators, implicit involuntary bias on the part of the healthcare system as well as individual providers could affect the care people receive. Much criticism has been voiced against the formulation and implementation of “ageist” policy, whereby resources are prioritized based exclusively on patients’ chronological age (Ayalon et al., 2020). Older people from minority or disadvantaged groups may thus face double discrimination, placing them in an extremely vulnerable situation. The lack of community capacity and mobilization in deprived areas may be a key bottleneck to providing timely assistance to older patients and their affected families (Lowcock et al., 2012).
Moreover, the use of telemedicine for in-person clinical evaluation poses special challenges for older adults, particularly those with sensory or cognitive impairments or who are unfamiliar with new technologies. Despite being the unique form of connection with healthcare services for some, these technology platforms lack rigorous assessment in older adults (van den Berg et al., 2012).
3.3. Disparities in prognosis and long-term consequences
Because older people from lower-income backgrounds are more likely to suffer from chronic conditions (e.g. obesity, diabetes mellitus, chronic lung disease, and cardiovascular disease) (CDC COVID-19 Response Team, 2020), multimorbidity (Barnett et al., 2012) or even frailty (Etman et al., 2012), they are also at a higher risk of COVID-19-associated complications and mortality (Onder et al., 2020; Hewitt et al., 2020). Moreover, older and socially vulnerable persons affected by COVID-19 could be less likely to be recruited for respiratory rehabilitation and monitoring (Liu et al., 2020), especially in those countries with no universal health coverage. Indeed, some of the pulmonary function tests used to follow-up and stratify these patients (e.g. lung plethysmography, carbon monoxide diffusing capacity) are expensive and not easily available through telemedicine.
Those with lower household incomes have been shown to experience significantly greater mental strain as a result of prolonged quarantine, most likely due to over-crowded accommodation as well as to increased risk of losing income (Brooks et al., 2020). Self-isolated older adults are more likely to experience loneliness, poor food availability and unbalanced diet, lack of exercise, and lower cognitive stimulation, which will considerably decrease their levels of resilience, leading to a cascade of physical and mental health problems. Such risk will be exacerbated among poor older people, who rely most on social care and community support. In addition, people’s ability to maintain remote contact with family and friends, which seems essential for long-term mental health, also depends on their access to smart phones, computers and Internet, and above all, their technological literacy, which is especially low among the oldest old.
The pandemic’s toll will reach dramatic levels in those contexts where all above-mentioned vulnerability factors cluster together, as is the case of conflict zones, prisons, and refugee camps. Not to speak about those places where people lack the very access to clean water with which to wash their hands to prevent infections, an intolerable reality for more than 840 million people around the world. The care home sector is another example where several of these factors coexist, which has led to the highest death rates worldwide (European Centre for Disease Prevention and Control, 2020). Aspects related to their congregate nature, the populations served (i.e. older adults with a high burden of morbidity and cognitive and functional impairment), the dominance of private for-profit providers, decreasing quality standards in terms of health promotion and prevention, the often precarious working conditions of the staff, and residents’ limited networks of psychosocial support, have placed nursing homes in the eye of the storm.
4. Discussion and future directions
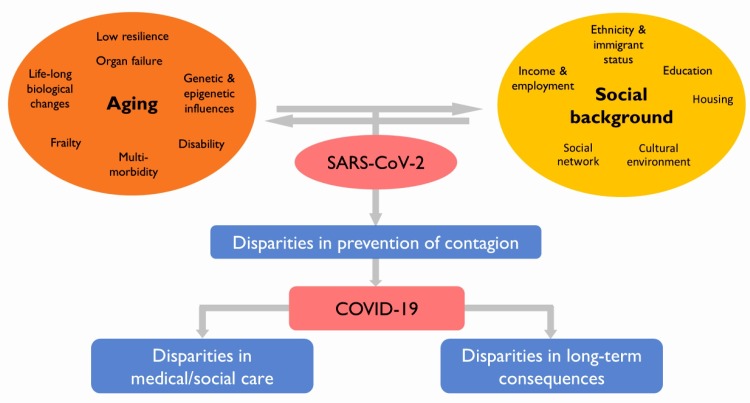
The COVID-19 pandemic is far from being the “great equalizer” that affects all social groups alike, as it has been portrayed. It expresses a disproportionate preference for individuals who are not only biologically, but also socially vulnerable. In fact, it is further amplifying the large social inequalities already existing in the older populations. Yet, this is nothing new. The 1918 flu pandemic also showed a significant geographic variation in mortality driven by socioeconomic factors (Mamelund, 2006). Similarly, during the 2009 H1N1 influenza pandemic, the death rate was found to be three times higher in the poorest compared to the wealthiest quintile of the British population (Rutter et al., 2012). While the European Commission has earmarked €140 million to support research on the diagnosis, treatment, and vaccine development, and another €87 million to produce medical devices and help overburdened healthcare systems and businesses (European Comission, 2020), no funds seem to be specifically allocated to carry out the “social autopsy” of the COVID-19 outbreak. There is an urgent need to address these questions with scientific methods and proper study designs, where the interplay between individuals’ biomedical status and their social environment is the focus. We propose a conceptual framework addressing biological and social differences in COVID-19 burden developed specifically for older people, considering potential disparities in its prevention, treatment, prognosis and/or long-term consequences (Fig. 2 ).
Fig. 2.
Proposed conceptual framework to elucidate the high levels of SARS-CoV-2 virus contagion and severity of COVID-19 in older people.
What is currently missing is research focusing on the interplay between the biological and social backgrounds, which is relevant for all, but especially for older adults’ health when challenged by an acute severe disease as COVID-19. Thus, integrated biological, clinical and social data are urgently needed worldwide to guide actions aimed at reducing older adults’ vulnerability to COVID-19. In the long run, it is societies’ deep-rooted structural inequities as well as the disciplinary fragmentation of research fields – that now seem to have intensified due to this new disease – that we will need to address. Combating this and future pandemics will inevitably mean combating outdated research practices and assuring efficient and egalitarian public healthcare systems within each country and worldwide.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The New York Times. A Month of Coronavirus in New York City: See the Hardest-Hit Areas. https://www.nytimes.com/interactive/2020/04/01/nyregion/nyc-coronavirus-cases-map.html?referringSource=articleShare.
- Dell’Olmo M.M., Gotsens M., Pasarín M.I., et al. Barcelona Societat; 2020. Desigualtats socials i Covid-19 a Barcelona.https://ajuntament.barcelona.cat/dretssocials/sites/default/files/revista/08_op_aspb_bcn26.pdf%0D%0A [Google Scholar]
- The Local. How are Sweden’s foreign residents reacting to the country’s coronavirus approach? https://www.thelocal.se/20200409/why-are-there-so-many-coronavirus-cases-in-stockholms-northern-suburbs.
- The Guardian. UK government urged to investigate coronavirus deaths of BAME doctors. https://www.theguardian.com/society/2020/apr/10/uk-coronavirus-deaths-bame-doctors-bma.
- Iacobucci G. Covid-19: Deprived areas have the highest death rates in England and Wales. BMJ. 2020;(May):m1810. doi: 10.1136/bmj.m1810. [DOI] [PubMed] [Google Scholar]
- Politico. Black doctors blast “woefully anemic” data on minority coronavirus cases. https://www.politico.com/news/2020/04/20/minority-cases-coronavirus-197203.
- Mollalo A., Vahedi B., Rivera K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf M.S., Serper M., Opsasnick L., et al. Awareness, Attitudes, and Actions Related to COVID-19 Among Adults With Chronic Conditions at the Onset of the U.S. Outbreak. Ann Intern Med. 2020;(April) doi: 10.7326/M20-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Philadelphia Inquirer. High-income Philadelphians getting tested for coronavirus at far higher rates than low-income residents. https://www.inquirer.com/news/philadelphia/coronavirus-testing-inequality-poverty-philadelphia-health-insurance-20200406.html.
- The Commonwealth Fund. Update on Federal Surprise Billing Legislation: New Bills Contain Key Differences. https://www.commonwealthfund.org/blog/2020/update-surprise-billing-legislation-new-bills-contain-key-differences.
- Independent. Coronavirus: Teenage boy whose death was linked to COVID-19 “turned away from urgent care for not having insurance.” https://www.independent.co.uk/news/world/americas/coronavirus-teenager-death-california-health-insurance-care-emergency-room-covid-19-a9429946.html.
- Ayalon L., Chasteen A., Diehl M., et al. Aging in Times of the COVID-19 Pandemic: Avoiding Ageism and Fostering Intergenerational Solidarity. J Gerontol B Psychol Sci Soc Sci. 2020;(April) doi: 10.1093/geronb/gbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowcock E.C., Rosella L.C., Foisy J., McGeer A., Crowcroft N. The social determinants of health and pandemic H1N1 2009 influenza severity. Am J Public Health. 2012;102(8):e51–e58. doi: 10.2105/AJPH.2012.300814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg N., Schumann M., Kraft K., Hoffmann W. Telemedicine and telecare for older patients--a systematic review. Maturitas. 2012;73(2):94–114. doi: 10.1016/j.maturitas.2012.06.010. [DOI] [PubMed] [Google Scholar]
- CDC COVID-19 Response Team Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett K., Mercer S., Norbury M., Watt G., Wyke S., Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;6736(12) doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- Etman A., Burdorf A., Van der Cammen T.J.M., Mackenbach J.P., Van Lenthe F.J. Socio-demographic determinants of worsening in frailty among community-dwelling older people in 11 European countries. J Epidemiol Community Health. 2012;66(12):1116–1121. doi: 10.1136/jech-2011-200027. [DOI] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020;(March) doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Hewitt J., Carter B., Vilches-Moraga A., et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;(June) doi: 10.1016/S2468-2667(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Zhang W., Yang Y., Zhang J., Li Y., Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract. 2020;39 doi: 10.1016/j.ctcp.2020.101166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control . ECDC; Stockholm: 2020. Surveillance of COVID-19 in Long-Term Care Facilities in the EU/EEA. [Google Scholar]
- Mamelund S.E. A socially neutral disease? Individual social class, household wealth and mortality from Spanish influenza in two socially contrasting parishes in Kristiania 1918-19. Soc Sci Med. 2006;62(4):923–940. doi: 10.1016/j.socscimed.2005.06.051. [DOI] [PubMed] [Google Scholar]
- Rutter P.D., Mytton O.T., Mak M., Donaldson L.J. Socio-economic disparities in mortality due to pandemic influenza in England. Int J Public Health. 2012;57(4):745–750. doi: 10.1007/s00038-012-0337-1. [DOI] [PubMed] [Google Scholar]
- European Comission . Brussels; 2020. Coronavirus Response Investment Initiative. [Google Scholar]
- APM Research Lab. The color of coronavirus: COVID-19 deaths by race and ethnicity in the U.S. https://www.apmresearchlab.org/covid/deaths-by-race.
- NYC Department of Health and Mental Hygiene. COVID-19: Data. https://www1.nyc.gov/site/doh/covid/covid-19-data.page.
- UK Office for National Statistics . 2020. Deaths involving COVID-19 by local area and socioeconomic deprivation: deaths occurring between 1 March and 17 April.https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand17april [Google Scholar]
- UK Office for National Statistics . 2020. Coronavirus (COVID-19) related deaths by occupation, England and Wales: deaths registered up to and including 20 April.https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/coronaviruscovid19relateddeathsbyoccupationenglandandwales/deathsregistereduptoandincluding20april2020 [Google Scholar]
- RE-HAB. Conclusiones de la territorialización de la pandemia de COVID-19 en el área metropolitana de Madrid. http://vps181.cesvima.upm.es/re-hab/2020/05/12/conclusiones-de-la-territorializacion-de-la-pandemia-de-covid-19-en-el-area-metropolitana-de-madrid/.