Abstract
The COronaVIrus Disease 2019 (COVID-19), which developed into a pandemic in 2020, has become a major healthcare challenge for governments and healthcare workers worldwide. Despite several medical treatment protocols having been established, a comprehensive rehabilitation program that can promote functional recovery is still frequently ignored. An online consensus meeting of an expert panel comprising members of the Taiwan Academy of Cardiovascular and Pulmonary Rehabilitation was held to provide recommendations for rehabilitation protocols in each of the five COVID-19 stages, namely (1) outpatients with mild disease and no risk factors, (2) outpatients with mild disease and epidemiological risk factors, (3) hospitalized patients with moderate to severe disease, (4) ventilator-supported patients with clear cognitive function, and (5) ventilator-supported patients with impaired cognitive function. Apart from medications and life support care, a proper rehabilitation protocol that facilitates recovery from COVID-19 needs to be established and emphasized in clinical practice.
Keywords: Consensus, COVID-19, Infection control, Rehabilitation
The role of rehabilitation and infection precautions in the management of COronaVIrus Disease 2019 infection
Since the end of 2019, COronaVIrus Disease 2019 (COVID-19), a novel infectious disease emerging from Wuhan, China, has continued to spread rapidly, causing an ongoing global outbreak. Patients may exhibit dyspnea, hypoxia, remarkable pneumonia, acute respiratory distress syndrome (ARDS), or even multiple organ failure.1 , 2 In addition to the possible sequelae of pulmonary fibrosis,3 which could impair the survivors' ventilation and oxygenation, many other organs could be affected, especially the cardiovascular system.4 Common complications of the cardiovascular system may include arrhythmia, myocarditis, acute coronary syndrome, venous thromboembolism, cardiogenic shock, and heart failure.5 Furthermore, prolonged inactivity can also affect exercise capacity significantly. Apart from medical treatment and supportive therapy, rehabilitation plays a vital role throughout the entire disease course. An appropriate rehabilitation program could help patients with mild disease maintain exercise capacity and activities of daily living. For patients with advanced disease severity, a well-designed rehabilitation program is even more crucial to improve pulmonary secretion clearance, ameliorates side-effects related to a prolonged bedridden state, and even prevents intensive care unit-acquired weakness. This expert consensus provides recommendations for rehabilitating patients with varying degrees of COVID-19 severity.
Although rehabilitation has multiple benefits for patients, the disease remains highly contagious and poses a substantial threat to medical providers. Hence, proper protective personal equipment (PPE) should be used when caring for patients with COVID-19,6 while patients should always be wearing surgical masks during rehabilitation. Health care workers should be under airborne precautions wearing PPE, including N95 masks, fluid resistant long-sleeved gowns, face shields, and gloves, when performing chest physiotherapy on non-intubated patients or aerosol-generating procedures during ventilator disconnection of intubated patients. Even during early mobilization of intubated patients with a closed ventilator circuit, droplet precautions wearing PPE, including surgical masks, fluid-resistant long-sleeved gowns, face shields and gloves, are still needed. Moreover, health care personnel require extra training regarding infection precautions, such as in the event of accidental endotracheal tube disconnection from the ventilator. Only under proper protection against COVID-19 transmission can rehabilitation programs be safely implemented and function as intended for the management of affected patients. However, the recommendations provided in this expert consensus should neither replace local institutional policies nor substitute clinical decisions established by physicians for any patient.
Risk factors and categorization for patients with COVID-19
Considering that COVID-19 can cause significant morbidity and mortality based on certain risk factors, such risk factors need to be identified in order to establish individualized rehabilitation programs. Data from 44,672 laboratory-confirmed cases of COVID-19 in China have shown that disease severity can be categorized as mild, severe, and critical.1 Approximately 81% of infected patients were categorized as mild and presented without or with mild pneumonia, while approximately 14% were categorized as severe and presented with dyspnea, blood oxygen saturation ≤93%, partial pressure of arterial oxygen to fraction of inspired oxygen (P/F) ratio <300, or lung infiltrates >50% within 24–48 h. The remaining 5% were classified as critical and presented with respiratory failure, septic shock, or multiple organ dysfunction, which resulted in a high mortality rate of 49%. Those with preexisting comorbid conditions, including cardiovascular disease (CVD) (10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6.0%), and cancer (5.6%), displayed a higher case-fatality rate (CFR). Patients without underlying medical conditions had an overall CFR of 0.9%. A recent meta-analysis that assessed the risk for severe infection in 46,248 patients7 found that those with CVD [odds ratio (OR) = 3.42] had the highest risk for severe infection, followed by respiratory system disease (OR = 2.46) and hypertension (OR = 2.36). Moreover, another study outside China showed that older age (OR = 1.06), male gender (OR = 3.68), and hypertension (OR = 2.71) were independently associated with severe disease at admission.8 Altogether, potentially significant risk factors for severe COVID-19 that should be identified and considered when designing rehabilitation programs include old age, male gender, hypertension, diabetes, respiratory disease, and CVD.
The World Health Organization (WHO) had categorized clinical syndromes associated with COVID-19 as mild illness, pneumonia, severe pneumonia, ARDS, sepsis and septic shock.9 However, this expert consensus categorized patients with COVID-19 differently such that outpatients with various risk factors or inpatients with disparate cognitive status should receive distinct rehabilitation programs. Therefore, the current expert consensus categorized patients with COVID-19 into the following five groups: (1) outpatients with mild disease and no risk factors, (2) outpatients with mild disease and epidemiological risk factors, (3) hospitalized patients with moderate to severe disease, (4) ventilator-supported patients with clear cognitive function, and (5) ventilator-supported patients with impaired cognitive function.
Suggestions for the rehabilitation of outpatients with mild disease and no risk factors
Majority of the patients with COVID-19 had mild disease.1 Those with mild disease and no risk factors were allocated to home care, with rehabilitation recommendations similar to those of the American College of Sports Medicine (ACSM) general principles of exercise prescription,10 though infection control is essential.11 , 12 While home-based rehabilitation is recommended for this group of patients, hospital-based rehabilitation may be started only when patients have been (1) at least 10 days since symptom onset (2) at least 24 h since resolution of fever without taking antipyretic drugs and (3) without other COVID-19 related symptoms, according to the recommendation for discontinuation of home isolation from Center for Disease Control and Prevention of United States.13 The objective of rehabilitation is primarily preventing complications of inactivity through conditioning exercises.
Conditioning exercises should include at least three components, namely warm-up, exercise, cool-down and stretching.10 A proper warm-up generally includes light intensity endurance activities for at least 5–10 min. Exercises include both aerobic exercise and resistance training. Aerobic training involves the activation of large muscle groups in a rhythmic movement (e.g., treadmill walking, bicycling, or upper limb ergometer trainings). Training frequency, intensity, and duration should be as follows:
-
-
Frequency: 5 days or more per week
-
-
Intensity: maintaining a heart rate reserve of 40%–59% during exercise, while the heart rate reserve refers to the difference between the predicted maximum heart rate and the resting heart rate14
-
-
Duration: 30–60 min
On the other hand, resistance training involves single- or multi-joint exercises targeting major muscles including the biceps, triceps brachii, pectoralis major, rhomboideus, gluteus, iliopsoas, quadriceps, hamstring, anterior tibialis, and calf muscles, using weight machines, free weights, or body weight. Training frequency, intensity and duration should be as follows:
-
-
Frequency: 2–3 days per week with at least 48-h intervals
-
-
Intensity: strength training involves using a weight equivalent of 60%–70% of the one repetition maximum, while endurance training involves using a weight equivalent to less than 50% of the one repetition maximum. The one repetition maximum refers to the maximum amount of weight that a person can possibly lift for only one time.15
-
-
Duration: 2–4 sets with 8–12 repetitions for strength training; ≤2 sets with 15–25 repetitions for endurance training.
After exercise training, a 5–10 min cool-down consisting of light intensity endurance activities, followed by at least 10 min of stretching exercises, should be performed.
The current COVID-19 management guideline recommends cancelling elective procedures16 and prefers home-based self-monitored rehabilitation, with adequate environmental disinfection. Moreover, emerging studies have found that tele-rehabilitation and self-rehabilitation tutorials may be helpful.17 Certain traditional Chinese health-promoting exercises (Baduanjin qigong, Tai Chi, etc.) have been recommended by Chinese rehabilitation studies for patients with COVID-1918 and could complement formal exercise training. However, patients developing unstable vital signs or respiratory distress must discontinue exercise.10 , 18
Current understanding on COVID-19 suggests that pregnant women present with similar clinical findings as non-pregnant adults.19 Therefore, pregnant women can also maintain their exercise programs as recommended by the ACSM. However, exercise in the supine position should be avoided after week 16 of pregnancy given its tendency to reduce venous return due to the weight of fetus. Furthermore, pregnant women should also avoid contact sports, exercising in hot humid environments, or Valsalva maneuver during exercise. On the other hand, children with COVID-19 usually have less severe symptoms than adults20 and constitute a special group that needs extra physical activity to prevent a sedentary lifestyle. Unlike adults, children need at least 60 min of aerobic training daily. However, due to their immature thermoregulatory mechanism, children also need to avoid exercising in hot humid environments.
Suggestions for the rehabilitation of outpatients with mild disease and epidemiological risk factors
Although most patients with COVID-19 develop mild disease,1 those with preexisting comorbid conditions, such as CVD, diabetes, chronic respiratory disease, and hypertension, are at greater risk for developing critical illness and higher CFR compared to those without such conditions.7 In this group of patients, home-based outpatient programs with proper video instructions and tele-rehabilitation are still recommended to avoid COVID-19 transmission. A comprehensive exercise program including aerobic and resistance training, as previously mentioned, could be provided to patients with comorbidities under the following special consideration:
-
(1)
Hypertension: Post-exercise blood pressure (BP) reduction should be considered especially among older patients receiving anti-hypertensive medicine such as α-blockers and vasodilators. Therefore, exercise termination should be gradual, while the cool-down phase should be extended and monitored carefully until BP and heart rate return to resting levels. Avoid the Valsalva maneuver or breath holding during resistance training and static stretching to avoid excessive BP elevation.
-
(2)
CVD: Exercise training is safe and effective for most patients with CVD. Patient whose angina threshold heart rate had been previously determined by a formal cardiopulmonary exercise test should adjust their exercise intensity to the upper limit of heart rate 10 beats/min below the angina threshold.21 Patients who had not undergone formal exercise testing can exercise at a rated perceived exertion of 4–6 on a 0–10 scale.21 However, a formal exercise test should still be considered in patients with advanced CVD with proper clinical disinfection following CDC11 and WHO12 recommendations. Routine assessment of exercise intolerance symptoms, such as dyspnea, lightheadedness or dizziness, palpitations, chest tightness, and pain, should be carefully performed. For patients with very limited exercise capacities, multiple shorter (i.e., <10 min) exercise sessions may be considered initially. Patients with heart failure should begin aerobic training several weeks before resistance training.10 Some medications used for treatment of COVID-19 may induce heart rhythm problems including QT interval prolongation and conduction block. These medications include hydroxychloroquine, antiviral drugs such as favipiravir and lopinavir/ritonavir, and antibiotics such as azithromycin.22 Despite hydroxychloroquine no longer recommended in treating COVID-19,23 when patients taking these medications experience unusual symptoms of palpitation, formal electrocardiogram should be arranged after cardiologist consultation before further exercise training.
-
(3)
Pulmonary disease: Patients with previous chronic pulmonary diseases could develop much more airway secretions than those without. Airway clearance techniques, which will be described in detail in the next section, should include flutter breathing, autogenic drainage, and cough techniques, such as huff coughing and controlled coughing. Specific exercises, such as Yoga, Tai-chi, Pilates, and trunk core muscle training, can help stabilize the trunk and promote efficient breathing.24 Inspiratory muscle training, with a threshold loading starting at 30% of the maximal inspiratory pressure (MIP), is recommended given evidence suggesting its benefits in reducing dyspnea and improving, exercise capacity and quality of life for patients with COPD.25 During conditioning exercises, intensity should be set at a rated perceived exertion of 4–6 on a 0–10 scale. Exercise in cold environments or those with allergens or pollutants should be limited to avoid triggering bronchoconstriction among susceptible individuals.
-
(4)
Diabetes mellitus (DM): Blood glucose levels should be assessed before and after exercise. Symptoms associated with hypoglycemia, including tingling of the mouth and fingers, tremor, abnormal sweating, anxiety, confusion, amnesia, hunger, and visual disturbances, should be carefully monitored. Individuals with retinopathy should avoid vigorous activities and Valsalva maneuver, which may dramatically elevate BP. Those with polyneuropathy require proper foot care to prevent foot ulcers and the risk of amputation.
Despite home-based rehabilitation is suggested for this group of patients, several contraindications for exercise, as shown in Table 1 ,10 should be reminded for both healthcare providers and patients. In the event of any adverse events encountered by patients during home-based rehabilitation, exercise training should be stopped immediately. For patients with angina symptoms or significant hypertension, sublingual nitroglycerin or short acting calcium channel blocker could be taken respectively. For patients with hypotensive responses, prompt lying done with fluid supply should be implemented. For patients experiencing hypoglycemic symptoms, sugar cubes should be given promptly. For patients with acute exacerbating symptoms of asthma or COPD, short-acting bronchodilator inhalation should be used first. If the patients' vital signs and symptoms still not recover, emergent medical support should be called for help without hesitation.
Table 1.
Contraindications for home exercise training for patients with COVID-19.
| COVID-19 patients group | Contraindications |
|---|---|
| Without underlying diseases | Acute high fever > 39 °C Tachypnea at rest > 30 breaths per minutes |
| With hypertension | Uncontrolled resting hypertension > 180/110 mmHg Orthostatic blood pressure drop of > 20 mmHg with symptoms |
| With DM | Blood sugar < 70 mg/dl Blood sugar > 300 mg/dl with urine ketones |
| With CVD | Unstable angina Uncontrolled sinus tachycardia > 120 beats per minute History of significant aortic stenosis (aortic valve area < 1.0 cm2) History of third-degree atrioventricular block without pacemaker Uncontrolled atrial or ventricular arrhythmias Uncompensated heart failure |
| With pulmonary diseases | Acute exacerbated symptoms of preexisting COPD or asthma |
Abbreviations: CVD, cardiovascular disease; COPD, chronic obstructive pulmonary disease; COVID-19, COronaVIrus Disease 2019; DM, diabetes mellitus.
Suggestions for rehabilitation of hospitalized patients with moderate to severe disease
Approximately 14% of patients with COVID-19 developed moderate to severe disease that required hospitalization and aggressive treatment.1 These individuals usually present with fever, cough, dyspnea, tachycardia, tachypnea, and various degrees of oxygen desaturation necessitating support.2 Studies have shown that early rehabilitation interventions for community-acquired pneumonia and interstitial pneumonia within 2 days of admission reduced in-hospital mortality.26 , 27 The two primary objectives of rehabilitation in this stage are promoting airway clearance and preventing complications of acute illness-related immobilization.
About 33.7% of COVID-19 patients could have copious sputum production.28 Incorporating chest physiotherapy into the medical treatment of patients with lung consolidation plays an important role in helping patients with airway secretions. Proper chest physiotherapy could promote effective expectoration, enhance mucociliary clearance of secretions to the upper airways, and improve cough effectiveness.29 Chest physiotherapy strategies that promote airway clearance include the following:
-
(1)
Positioning: Optimal positioning to reduce dyspnea should be patient specific. For instance, an upright, forward-leaning position with arm support will reduce dyspnea and respiratory distress, particularly among patients with COPD. A side-lying position may optimize perfusion to the good lung during unilateral lung disease, thus improving gas exchange.30
-
(2)
Active cycle of breathing techniques (ACBT): ACBT requires patient's active participation in guided breathing control to mobilize airway secretions and reduce dyspnea.31
-
(3)
Chest percussion and vibration: chest wall oscillation, mechanical vibration and chest percussion facilitate sputum expectoration particularly among patients with copious airway secretions.32 , 33
-
(4)
Huffing and controlled coughing: Huffing is characterized by rapid air exhalation without glottis closure, while controlled coughing aims to avoid shallow and inefficient coughs. Both coughing techniques have been shown to reduce coughing effort and improve airway clearance.34
-
(5)
Flutter breathing: This technique utilizes a device containing a movable steel ball in a sealed pipe. The patient rapidly blows air into the pipe, which shakes the steel ball and produces rhythmic airflow. Flutter breathing could ultimately loosen the sputum within the airway.31
Another important issue in the rehabilitation of patients with moderate to severe disease is preventing deconditioning due to acute illness. Immobilization has been shown to speed functional decline with reduced muscle strength and cardiorespiratory fitness, particularly among elderly individuals and those with comorbidities.1 , 35 Therefore, once medical condition stabilized, early mobilization should be encouraged.36 Rehabilitation interventions for such patients should include the following:
-
(1)
Active or active-assisted range of motion (ROM) exercise: Patients with moderate to severe disease who are able to actively move their extremities are encouraged to engage in active or active-assisted ROM exercises to maintain or improve joint integrity and prevent joint contracture and soft-tissue shortening.37
-
(2)
Mobilization and progressive off-bed activities: early mobilization with progressive mobility training, including off-bed transferring, unsupported sitting, standing, level-surface ambulation, and stair climbing, tailored to the patient's general condition should be carried out once medically stabilized. Proper walking aid may be used to assist in energy conservation to reduce distress during the activity.
-
(3)
Aerobic exercise: aerobic exercise using a stationary bike, arm ergometer, or level-surface walking beginning with light intensity (<3.0 metabolic equivalents) should be performed. Aerobic exercise intensity can also be assessed and modified according to the patient's rating of perceived exertion. The duration of aerobic exercise can be cumulative, starting at 5–10 min per training session, based on the patient's exercise tolerance.
When performing rehabilitation interventions, close monitoring of vital sign changes is imperative given that the patients' condition may progress. For patients with COVID-19 confined to isolation rooms, alternative approaches, such as supervised telerehabilitation, should be incorporated to avoid direct contact between health care workers and the patients.
Suggestions for the rehabilitation of ventilator-supported patients with clear cognitive status
The rehabilitation of ventilator-supported patients with severe COVID-19 is similar to that of patients with respiratory failure caused by other viral pneumonia infections. Intubated patients with a closed ventilator circuit have a lower risk for droplet transmission compared to non-intubated patients. However, certain aerosol-generating procedures during ventilator circuit disconnection, such as oropharyngeal suctioning, cough technique training, and inspiratory muscle training, require proper use of PPE under airborne precautions to reduce the risk of virus transmission. Airborne infection isolation rooms and careful procedure execution should be utilized to minimize the risk of virus exposure during patient contact. Telerehabilitation, computer-assisted rehabilitation, and virtual reality technology might be useful for ventilated patients in intensive care units.38 , 39 However, rehabilitation should be abandoned when patients exhibit decreased oxygen saturation despite inhaled oxygen >50% and positive end expiratory pressure (PEEP) >10 cm H2O, newly onset arrhythmia or coronary ischemia, systolic BP >200 mmHg or mean BP <60 mmHg despite medication, and uncontrolled high fever or seizures.40
The following are the key points and strategies for the rehabilitation of ventilated patients with clear cognitive status:
-
(1)
Activities: In-bed cycling in patients with critical illness has been shown to be a safe and feasible procedure for preserving muscle function41 and muscle fiber cross-sectional area,42 as well as fostering positive mental effect, including the feeling of control, safety, and hope, during the critical stages of the illness.43 Low resistance levels (i.e., approximately 0.5 Nm), are recommended with patient self-selected pedaling rate for 30 min daily.41 Upper-limb resistance training using elastic bands and pulleys can also be utilized. Patients who have stable clinical status can commence out-of-bed mobility depending on their tolerance, which may include sitting on the edge of the bed, moving from bed to chair, standing next to the bed, stepping on the spot, and walking with ambulatory assistive devices.44
-
(2)
Breathing exercises: Inspiratory muscle training, which strengthens the inspiratory muscles through the application of resistance during inspiration, can also be used for intubated patients or those with a tracheostomy. Using a threshold training device, with the threshold set at 50% of the MIP, five sets of six breaths performed once per day are recommended.45 Patients can also be educated on diaphragmatic breathing, which involves the negative pressure generated by the diaphragm instead of the accessory respiratory muscles. Finally, chest expansion and mobilization are important for increasing chest wall mobility and improving thoracic compliance during mechanical ventilation.
-
(3)
Chest care and airway secretions management: Postural drainage, percussion, vibration, and airway suctioning can be used to minimize pulmonary secretion retention and maximize oxygenation. High-frequency chest wall oscillation (HFCWO), which utilizes a percussive vest that replaces manual involvement, can better facilitate mucus movement towards the central airway. The device usually operates between 7 and 15 Hz on intubated patients. Although less effective than intrapulmonary percussive ventilation, HFCWO has been shown to reduce dyspnea and improve pulmonary function.46 Apart from clearing airway secretions, prone positioning, which is best performed early in the disease course (ideally within 48 h) when the P/F ratio is <150 mmHg, continues to play a vital role in the management of ARDS.47 Combined with low tidal volume ventilation (around 6 mL/kg), recommendations suggest that prone positioning be maintained for 16 h daily.47 Prone positioning has been shown to promote significant improvements in gas exchange and oxygenation. A side-lying position with the diseased lung on the top may also help improve ventilation and perfusion.
Suggestions for the rehabilitation of ventilator-supported patients with impaired cognitive status
As mentioned previously, 5% of patients with COVID-19 became critically ill and required admission to intensive care units and mechanical ventilation.1 Despite early rehabilitation within the first 72 h following intubation may benefit patients with acute respiratory failure by preventing intensive care unit-acquired complications,48 limited options are available for patients with impaired cognitive status. The following are the recommended strategies for this group of patients:
-
(1)
For patients with severe ARDS and impaired cognition, prone ventilation is still suggested for 16 h daily, which is to be repeated until a P/F ratio of ≥150 mmHg with a PEEP of ≤10 cm H2O and a fraction of inspired oxygen (FiO2) ≤0.60 are achieved for at least 4 h after supine positioning.49 On the other hand, prone ventilation may increase the risk of pressure sores and endotracheal tube obstruction.50
-
(2)
In cases of hypersecretion and ineffective mucus clearance, airway clearance techniques, such as chest percussion, vibration, and postural drainage every 4–6 h have been widely employed for mechanically ventilated patients.51 Intrapulmonary percussive ventilation52 and HFCWO can also be implemented to help sputum loosening. Sputum suction should be done under airborne precautions.
-
(3)
Diaphragmatic facilitation technique involves exerting a downward and cephalad pressure to the diaphragm during exhalation for the purpose of stretching to facilitate subsequent diaphragmatic contraction during ventilator air pumping.53 This technique can be used for patients with both clear and impaired cognitive function.
-
(4)
Frequent postural change in bed is important for preventing bedsores. Passive ROM exercise involving the major joints of the four limbs is vital for maintaining soft-tissue length and preventing joint contracture. Each upper and lower extremity joint should perform 5–10 repetitions in the supine position once or twice per day.54 , 55 Chest wall mobilization and expansion should also be performed in this group of patients to maintain thoracic compliance.
Conclusions
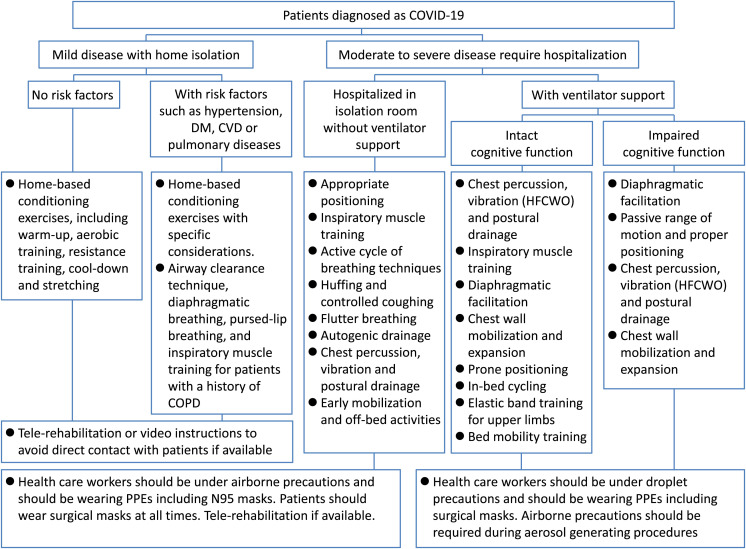
Patients with COVID-19 often suffer from reduced cardiopulmonary endurance and impaired quality of life after recovery because of the possible sequelae of pulmonary fibrosis,3 as well as the inevitable consequences of long-term bedridden status during treatment. On the other hand, patients with mild disease may also become frail due to a sedentary lifestyle during the isolation period. The rehabilitation protocols suggested in this expert consensus, which are summarized in Fig. 1 , improves patients' quality of life after recovery—an aspect that should never be overlooked during the management patients with COVID-19.
Figure 1.
The flowchart of suggested rehabilitation interventions and infection precautions for patients with COVID-19. The rehabilitation protocols for each of the five categories of patients with COVID-19 are summarized in this flowchart, and the infection precautions during contacting these patients are included as well. Abbreviations: COPD, chronic obstructive pulmonary disease; COVID-19, Coronavirus Disease 2019; CVD, cardiovascular disease; DM, diabetes mellitus; HFCWO, high frequency chest wall oscillation; PPE, personal protective equipment.
Funding/Support statement
None declared.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
Acknowledgement
The authors would like to thank Dr. Kai-Hua Chen, the Secretary-General of Taiwan Academy of Cardiovascular and Pulmonary Rehabilitation, for holding discussion meetings, recording the details of the meetings, and miscellaneous tasks related to the publishing of this expert consensus.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sheng G., Chen P., Wei Y., Yue H., Chu J., Zhao J., et al. Viral infection increases the risk of idiopathic pulmonary fibrosis: a meta-analysis. Chest. 2019 doi: 10.1016/j.chest.2019.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M., et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116:1666–1687. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas P., Baldwin C., Bissett B., Boden I., Gosselink R., Granger C.L., et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66:73–82. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi Y., Yu X., Zhao H., Wang H., Zhao R., Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24:108. doi: 10.1186/s13054-020-2833-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization Clinical management of COVID-19: interim guidance. https://www.who.int/publications/i/item/clinical-management-of-covid-19 Available from:
- 10.The American College of Sports Medicine . 10th ed. Lippincott Williams & Wilkins.; Philadelphia, PA: 2016. ACSM's guidelines for exercise testing and prescription. [Google Scholar]
- 11.Centers for Disease Control and Prevention Information for healthcare professionals about coronavirus (COVID-19) https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html Available from:
- 12.World Health Organization Home care for patients with suspected or confirmed COVID-19 and management of their contacts. https://www.who.int/publications/i/item/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts Available from:
- 13.Centers for Disease Control and Prevention Discontinuation of Isolation for persons with COVID-19 not in healthcare settings (Interim Guidance) https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html Available from:
- 14.Weltman A., Snead D., Seip R., Schurrer R., Weltman J., Rutt R., et al. Percentages of maximal heart rate, heart rate reserve and VO2max for determining endurance training intensity in male runners. Int J Sports Med. 1990;11:218–222. doi: 10.1055/s-2007-1024795. [DOI] [PubMed] [Google Scholar]
- 15.Grgic J., Lazinica B., Schoenfeld B.J., Pedisic Z. Test-retest reliability of the one-repetition maximum (1RM) strength assessment: a systematic review. Sports Med Open. 2020;6:31. doi: 10.1186/s40798-020-00260-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention Interim infection prevention and control recommendations for patients with suspected or confirmed Coronavirus Disease 2019 (COVID-19) in healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html Available from:
- 17.Cottrell M.A., Galea O.A., O'Leary S.P., Hill A.J., Russell T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017;31:625–638. doi: 10.1177/0269215516645148. [DOI] [PubMed] [Google Scholar]
- 18.Zhonghua J., He H., Hu H., Zhi Z. Recommendations for respiratory rehabilitation of COVID-19 in adult. 2020;43:E029. doi: 10.3760/cma.j.cn112147-20200228-00206. [DOI] [PubMed] [Google Scholar]
- 19.Rasmussen S.A., Smulian J.C., Lednicky J.A., Wen T.S., Jamieson D.J. Coronavirus Disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020 doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 21.Fletcher G.F., Ades P.A., Kligfield P., Arena R., Balady G.J., Bittner V.A., et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128:873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 22.Naksuk N., Lazar S., Peeraphatdit T.B. Cardiac safety of off-label COVID-19 drug therapy: a review and proposed monitoring protocol. Eur Heart J Acute Cardiovasc Care. 2020;9:215–221. doi: 10.1177/2048872620922784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Food and Drug Administration FDA cautions against use of hydroxychloroquine or chloroquine for COVID-19 outside of the hospital setting or a clinical trial due to risk of heart rhythm problems. https://www.fda.gov/drugs/drug-safety-and-availability/fda-cautions-against-use-hydroxychloroquine-or-chloroquine-covid-19-outside-hospital-setting-or Available from:
- 24.Cavaggioni L., Ongaro L., Zannin E., Iaia F.M., Alberti G. Effects of different core exercises on respiratory parameters and abdominal strength. J Phys Ther Sci. 2015;27:3249–3253. doi: 10.1589/jpts.27.3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beaumont M., Forget P., Couturaud F., Reychler G. Effects of inspiratory muscle training in COPD patients: a systematic review and meta-analysis. Clin Respir J. 2018;12:2178–2188. doi: 10.1111/crj.12905. [DOI] [PubMed] [Google Scholar]
- 26.Sawabe M., Hasebe K., Momosaki R. Effectiveness of early versus delayed physical rehabilitation on in-hospital mortality in interstitial pneumonia: a retrospective cohort study. PM&R. 2020 doi: 10.1002/pmrj.12357. [DOI] [PubMed] [Google Scholar]
- 27.Sawada Y., Sasabuchi Y., Nakahara Y., Matsui H., Fushimi K., Haga N., et al. Early rehabilitation and in-hospital mortality in intensive care patients with community-acquired pneumonia. Am J Crit Care. 2018;27:97–103. doi: 10.4037/ajcc2018911. [DOI] [PubMed] [Google Scholar]
- 28.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strickland S.L., Rubin B.K., Drescher G.S., Haas C.F., O'Malley C.A., Volsko T.A., et al. AARC clinical practice guideline: effectiveness of nonpharmacologic airway clearance therapies in hospitalized patients. Respir Care. 2013;58:2187–2193. doi: 10.4187/respcare.02925. [DOI] [PubMed] [Google Scholar]
- 30.Campbell M.L. Dyspnea. AACN Adv Crit Care. 2011;22:257–264. doi: 10.1097/NCI.0b013e318220bc4d. [DOI] [PubMed] [Google Scholar]
- 31.Uzmezoglu B., Altiay G. The efficacy of flutter((R)) and active cycle of breathing techniques in patients with bronchiectasis: a prospective, randomized, comparative study. Turk Thorac J. 2018;19:103–109. doi: 10.5152/TurkThoracJ.2018.17050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee A.L., Burge A.T., Holland A.E. Airway clearance techniques for bronchiectasis. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD008351.pub3. Cd008351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hill K., Patman S., Brooks D. Effect of airway clearance techniques in patients experiencing an acute exacerbation of chronic obstructive pulmonary disease: a systematic review. Chron Respir Dis. 2010;7:9–17. doi: 10.1177/1479972309348659. [DOI] [PubMed] [Google Scholar]
- 34.Pryor J.A. Physiotherapy for airway clearance in adults. Eur Respir J. 1999;14:1418–1424. doi: 10.1183/09031936.99.14614189. [DOI] [PubMed] [Google Scholar]
- 35.Bowden Davies K.A., Pickles S., Sprung V.S., Kemp G.J., Alam U., Moore D.R., et al. Reduced physical activity in young and older adults: metabolic and musculoskeletal implications. Ther Adv Endocrinol Metab. 2019;10 doi: 10.1177/2042018819888824. 2042018819888824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hadfield J., Bennett L. Determining best outcomes from community-acquired pneumonia and how to achieve them. Respirology. 2018;23:138–147. doi: 10.1111/resp.13218. [DOI] [PubMed] [Google Scholar]
- 37.Wang F., Zhang Q.B., Zhou Y., Chen S., Huang P.P., Liu Y., et al. The mechanisms and treatments of muscular pathological changes in immobilization-induced joint contracture: a literature review. Chin J Traumatol. 2019;22:93–98. doi: 10.1016/j.cjtee.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gerber S.M., Jeitziner M.M., Wyss P., Chesham A., Urwyler P., Muri R.M., et al. Visuo-acoustic stimulation that helps you to relax: a virtual reality setup for patients in the intensive care unit. Sci Rep. 2017;7:13228. doi: 10.1038/s41598-017-13153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murthy S., Gomersall C.D., Fowler R.A. Care for critically ill patients with COVID-19. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.3633. [DOI] [PubMed] [Google Scholar]
- 40.Schmidt U.H., Knecht L., MacIntyre N.R. Should early mobilization be routine in mechanically ventilated patients? Respir Care. 2016;61:867–875. doi: 10.4187/respcare.04566. [DOI] [PubMed] [Google Scholar]
- 41.Kho M.E., Molloy A.J., Clarke F.J., Ajami D., McCaughan M., Obrovac K., et al. TryCYCLE: a prospective study of the safety and feasibility of early in-bed cycling in mechanically ventilated patients. PLoS One. 2016;11:e0167561. doi: 10.1371/journal.pone.0167561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hickmann C.E., Castanares-Zapatero D., Deldicque L., Van den Bergh P., Caty G., Robert A., et al. Impact of very early physical therapy during septic shock on skeletal muscle: a randomized controlled trial. Crit Care Med. 2018;46:1436–1443. doi: 10.1097/CCM.0000000000003263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ringdal M., Warren Stomberg M., Egnell K., Wennberg E., Zatterman R., Rylander C. In-bed cycling in the ICU; patient safety and recollections with motivational effects. Acta Anaesthesiol Scand. 2018;62:658–665. doi: 10.1111/aas.13070. [DOI] [PubMed] [Google Scholar]
- 44.Zhang L., Hu W., Cai Z., Liu J., Wu J., Deng Y., et al. Early mobilization of critically ill patients in the intensive care unit: a systematic review and meta-analysis. PLoS One. 2019;14:e0223185. doi: 10.1371/journal.pone.0223185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bissett B., Leditschke I.A., Green M., Marzano V., Collins S., Van Haren F. Inspiratory muscle training for intensive care patients: a multidisciplinary practical guide for clinicians. Aust Crit Care. 2019;32:249–255. doi: 10.1016/j.aucc.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 46.Nicolini A., Grecchi B., Ferrari-Bravo M., Barlascini C. Safety and effectiveness of the high-frequency chest wall oscillation vs intrapulmonary percussive ventilation in patients with severe COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:617–625. doi: 10.2147/COPD.S145440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scholten E.L., Beitler J.R., Prisk G.K., Malhotra A. Treatment of ARDS with prone positioning. Chest. 2017;151:215–224. doi: 10.1016/j.chest.2016.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schweickert W.D., Pohlman M.C., Pohlman A.S., Nigos C., Pawlik A.J., Esbrook C.L., et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fan E., Del Sorbo L., Goligher E.C., Hodgson C.L., Munshi L., Walkey A.J., et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 50.Munshi L., Del Sorbo L., Adhikari N.K.J., Hodgson C.L., Wunsch H., Meade M.O., et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14 doi: 10.1513/AnnalsATS.201704-343OT. S280-s8. [DOI] [PubMed] [Google Scholar]
- 51.Volsko T.A. Airway clearance therapy: finding the evidence. Respir Care. 2013;58:1669–1678. doi: 10.4187/respcare.02590. [DOI] [PubMed] [Google Scholar]
- 52.Dingemans J., Eyns H., Willekens J., Monsieurs P., Van Houdt R., Cornelis P., et al. Intrapulmonary percussive ventilation improves lung function in cystic fibrosis patients chronically colonized with Pseudomonas aeruginosa: a pilot cross-over study. Eur J Clin Microbiol Infect Dis. 2018;37:1143–1151. doi: 10.1007/s10096-018-3232-8. [DOI] [PubMed] [Google Scholar]
- 53.Daniel Martin A., Smith B.K., Gabrielli A. Mechanical ventilation, diaphragm weakness and weaning: a rehabilitation perspective. Respir Physiol Neurobiol. 2013;189:377–383. doi: 10.1016/j.resp.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moss M., Nordon-Craft A., Malone D., Van Pelt D., Frankel S.K., Warner M.L., et al. A randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med. 2016;193:1101–1110. doi: 10.1164/rccm.201505-1039OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morris P.E., Berry M.J., Files D.C., Thompson J.C., Hauser J., Flores L., et al. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: a randomized clinical trial. JAMA. 2016;315:2694–2702. doi: 10.1001/jama.2016.7201. [DOI] [PMC free article] [PubMed] [Google Scholar]