Abstract
Background
The Stop the Bleed (STB) program was developed to bring military bleeding control techniques into wider use among American civilians. It was introduced in Japan in case of mass casualty events during the Tokyo Olympic/Paralympic Games in 2021, and its effectiveness was prospectively evaluated.
Methods
Japanese physicians certified as STB instructors held bleeding control basic training courses from April to July 2019. Participants’ knowledge was assessed using pre-training and post-training tests comprising five questions. One point was awarded for each correct answer, giving a maximum total score of 5. (Q1) What is the most common preventable trauma death?; (Q2) Which actions should be prioritized for bleeding victims?; (Q3) Which patients should be transferred to hospital first?; (Q4) How should a tourniquet be applied?; (Q5) How should pain associated with a tourniquet be managed?
Results
The study involved 157 participants (20 physicians/nurses, 82 medical students, 33 emergency services personnel, 22 police officers/security personnel). The mean±SD scores were 2.1±1.1 before training and 3.2±1.0 after training (p<0.01). The respective percentages of correct answers before and after training were 58% and 75% for Q1, 10% and 13% for Q2, 38% and 55% for Q3, 73% and 89% for Q4, and 33% and 91% for Q5. Q2 had the lowest percentage of correct answers and the poorest improvement.
Discussion
The STB program improved tourniquet knowledge. However, it was less effective in improving knowledge about which actions to prioritize for bleeding victims. This may be because the participants were well trained in basic life support and therefore expected to immediately commence cardiopulmonary resuscitation for patients in shock. The STB program is valuable in preparing Japanese people for mass casualty events during the Tokyo Olympic/Paralympic Games in 2021.
Level of evidence
IV.
Study type
Therapeutic.
Keywords: tourniquets, education, hemorrhage
Background
The Sandy Hook Elementary School shootings in the United States (US) resulted in the creation of the Hartford consensus in 2013.1 In addition, it was recognized that the most common cause of preventable trauma death was bleeding.2 3 Therefore, the Stop the Bleed (STB) program was created to educate the public on hemostatic techniques. The STB program has spread worldwide, with 500,000 participants in 71 countries.4
In Japan, it is illegal for the general public to own guns, and terrorist attacks and shootings are extremely rare. There were 21,424 trauma deaths registered in the Japan National Trauma Databank in 2015, only 180 of which were secondary to any homicidal attempt.5 The most common mechanism of trauma death in Japan was a fall (7927 deaths), and the most common preventable trauma death was bleeding.6 Thus, few Japanese healthcare professionals have treated bombing and shooting injuries. However, there is growing awareness among Japanese healthcare professionals that preparation is required for potential mass casualty incidents during the Tokyo Olympics/Paralympics scheduled for 2021. As the STB program was developed based on experience with mass casualty incidents in the US, the STB program may be helpful to educate the Japanese healthcare professionals, police officers, and security guards who will be the first responders to mass casualty incidents.
Japanese surgeons who were certified as STB instructors in the US introduced the bleeding control basic training course (part of the STB program) to Japan in 2018. They trained some Japanese trauma care providers, including surgeons, emergency medicine physicians, and emergency medical technicians (EMTs). These trainees were certified as STB instructors and held bleeding control basic training courses throughout Japan.
The effects of the bleeding control basic training course in the US for laypersons have been reported.7–9 However, no studies have evaluated the effects of the bleeding control basic training course in Japan. The present study aimed to prospectively evaluate the effects of the bleeding control basic training course for Japanese participants who were unfamiliar with mass casualty incidents. The present results may be used to create learning methods that are effective in preparing Japanese people for potential mass casualty incidents during the Tokyo Olympics/Paralympics.
Methods
Setting, instructors, and participants
Japanese physicians or EMTs who were certified STB instructors held bleeding control basic training courses at Teikyo University Hospital and Tokyo Medical and Dental University Hospital between April and July 2019.
The bleeding control basic training course was conducted using the slides, videos, and booklet downloaded from the STB homepage.4 These items were translated to Japanese, and the instructors spoke in Japanese. Participants were recruited from Teikyo University and Tokyo Medical and Dental University. Informed consent was obtained from all participants.
Participants completed a pre-training test just prior to attending the bleeding control basic training lecture. After the lecture, the participants completed a practical session comprising tourniquet application (Combat Application Tourniquet and Special Operation Force Tactical Tourniquet) and gauze packing of a standardized injured extremity (Z-Medica, Wallingford, CT). All participants then undertook a post-training test. Each session took approximately 1.5 hours (15 min pre-training test, 20 min lecture, 40 min practical session, and 15 min post-training test).
Pre- and post-training tests
Online supplementary table 1 shows the pre-training and post-training tests. The tests comprised the following questions: (Q1) What is the most common cause of preventable trauma death? (answer: bleeding); (Q2) Which actions should be prioritized for bleeding victims? (answer: stop the bleeding before considering cardiopulmonary resuscitation); (Q3) Which patients should be transferred to hospital first? (answer: patients with internal bleeding in the torso); (Q4) How should a tourniquet be applied?; (Q5) How should the pain associated with a tourniquet be managed? (answer: reassure the patient).
tsaco-2020-000490supp001.pdf (48.9KB, pdf)
Each correct answer was awarded 1 point, giving a maximum score of 5. The pre-training and post-training test scores were compared for each participant and each type of participant.
Statistical analysis
Parametric data were analyzed by the χ2 test. Non-parametric data were analyzed by the paired t-test. Statistical analyses were performed using PASW Statistics 18 (IBM Corporation, NY, USA). P values of less than 0.05 were considered to indicate statistically significant differences.
Results
During the study period, eight bleeding control basic training sessions were held in Tokyo. A total of 157 participants were involved, comprising 14 physicians, 6 nurses, 33 EMTs, and 22 police officers or security personnel who voluntarily applied, and 82 medical students who took the course as part of their emergency medicine rotation. The median years of work was 14 (range 2–27) for physicians, 4 (range 2–34) for nurses, 5 (range 1–27) for EMTs, 9 (2–25) for police officers or security personnel, and 5 (range 1–6) for medical students (the length of medical school in Japan is 6 years).
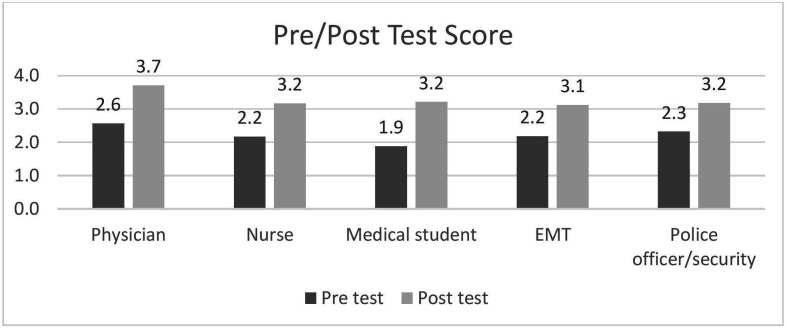
The mean±SD pre-training and post-training test scores were 2.1±1.1 and 3.2±1.0, respectively (p<0.01). Figure 1 shows the mean pre-training and post-training test scores by type of participant. All types of participants achieved higher scores in the post-training test than in the pre-training test. Of all the types of participants, physicians achieved the highest scores in both the pre-training and post-training tests. Medical students achieved the lowest pre-training test score of all the participant types; however, medical students showed the greatest improvement in pre-training versus post-training test scores (mean improvement of 1.3 points).
Figure 1.
Pre-training and post-training test scores by type of participant.
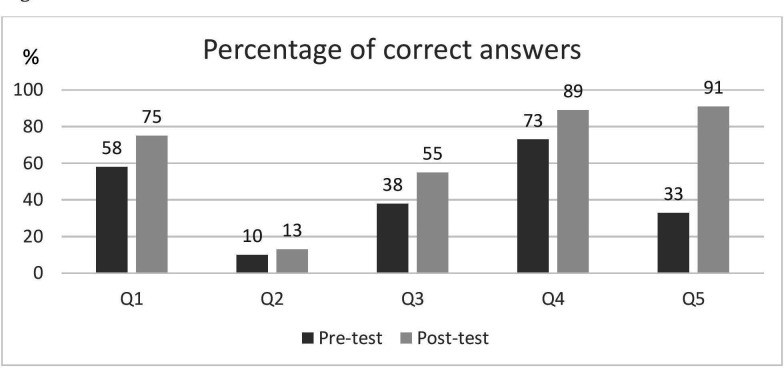
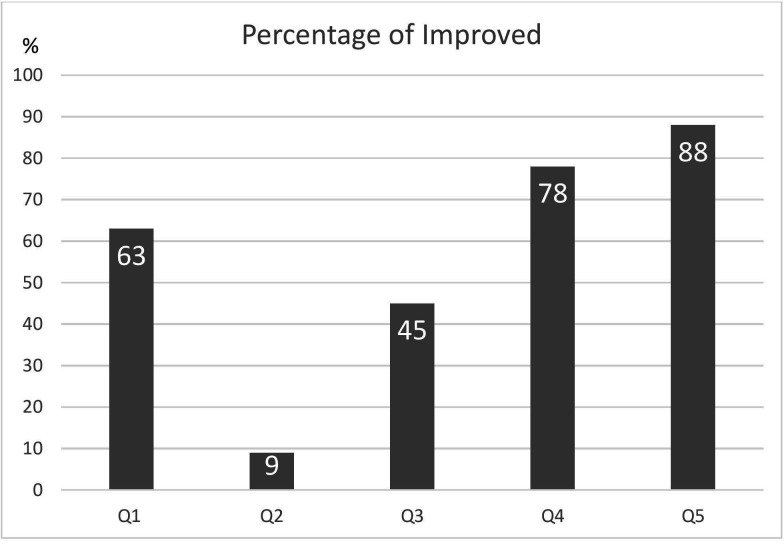
The percentage of correct answers before and after training are shown in figure 2. The lowest percentage of correct answers was seen for Q2. About 90% of participants answered Q4 and Q5 correctly after training. Figure 3 shows the percentage of participants who answered each question incorrectly in the pre-training test and correctly in the post-training test. The improvement rate was the largest for Q5 and the lowest for Q2. Table 1 shows the pre-training and post-training test results.
Figure 2.
Correct answer rates in the pre-training and post-training tests by question.
Figure 3.
Percentage of participants who improved their scores by question.
Table 1.
Pre-training and post-training test scores by question and type of participant
| Physicians (n=14) |
Nurses (n=6) |
Medical students (n=82) | Emergency medical technicians (n=33) | Police officers/security personnel (n=22) |
|
| Pre-training test | |||||
| Q1 correct | 13 (93%) | 3 (50%) | 36 (44%) | 24 (73%) | 15 (68%) |
| Q2 correct | 1 (7%) | 1 (17%) | 8 (10%) | 4 (12%) | 1 (5%) |
| Q3 correct | 9 (64%) | 3 (50%) | 33 (40%) | 8 (24%) | 7 (32%) |
| Q4 correct | 9 (64%) | 3 (50%) | 60 (73%) | 25 (76%) | 17 (77%) |
| Q5 correct | 4 (29%) | 2 (33%) | 22 (27%) | 12 (36%) | 11 (50%) |
| Post-training test | |||||
| Q1 correct | 12 (86%) | 5 (84%) | 67 (82%) | 20 (61%) | 14 (64%) |
| Q2 correct | 1 (7%) | 1 (17%) | 10 (12%) | 4 (12%) | 4 (18%) |
| Q3 correct | 13 (93%) | 3 (50%) | 45 (55%) | 16 (49%) | 10 (46%) |
| Q4 correct | 13 (93%) | 4 (67%) | 71 (87%) | 31 (94%) | 20 (91%) |
| Q5 correct | 13 (93%) | 6 (100%) | 70 (85%) | 32 (97%) | 22 (100%) |
| Improved (from incorrect to correct) | |||||
| Q1 | 1/1 (100%) | 2/3 (67%) | 35/46 (76%) | 2/9 (22%) | 2/7 (29%) |
| Q2 | 0 | 0 | 7/74 (10%) | 2/29 (7%) | 3/21 (14%) |
| Q3 | 5/5 (100%) | 1/3 (33%) | 22/49 (45%) | 11/25 (44%) | 5/11 (33%) |
| Q4 | 4/5 (80%) | 2/3 (67%) | 16/22 (73%) | 8/8 (100%) | 3/5 (60%) |
| Q5 | 9/10 (90%) | 4/4 (100%) | 49/60 (82%) | 20/21 (95%) | 11/11 (100%) |
Regarding Q2, physicians and nurses showed no improvement in the post-training test score; the percentage of other types of participants whose answer to Q2 improved from incorrect in the pre-training test to correct in the post-training test was 7%–14%. Regarding the questions about tourniquet application (Q4 and Q5), EMTs had higher correct answer rates in both the pre-training and post-training tests than the other types of participants.
Discussion
In the current study, all types of Japanese participants achieved significantly better scores in the post-training test than the pre-training test. The lowest percentage of correct answers and the poorest improvement were observed for Q2, which concerned the prioritization of actions for bleeding patients. Approximately 90% of participants answered Q4 (how should a tourniquet be applied?) and Q5 (how should pain associated with a tourniquet be managed?) correctly after the bleeding control basic training course. Even the participants who were not healthcare professionals (medical students and police officers/security guards) showed marked improvement in the post-training test compared with the pre-training test, suggesting that the bleeding control basic training program may be effective in educating the Japanese general public, as was seen in the US.
A study of more than 200 American laypersons reported a significant improvement in the participants’ comfort levels regarding tourniquet use after bleeding control basic training.8 Similarly, another study reported that tourniquet-based hemostasis techniques were well acquired by 10 American non-healthcare professional volunteers who completed the bleeding control basic training course.7 Weinman recommended offering refresher training within 6 months of initial course completion to ensure that the skills are retained.9 These studies primarily evaluated the ability of the general public to learn techniques such as tourniquet application, but did not evaluate their knowledge on the prioritization of actions for bleeding patients.
The reason for the low correct answer rate for Q2 in the present study may be due to the low requirement for trauma care in Japan. A Japanese national report of ambulance transport in 2017 found that only 23% of 6,342,147 emergency transports involved trauma patients.10 In addition, the Japan Trauma Data Bank Report 2013–2017 reported that of the 161,586 trauma patients registered, the mechanism of injury was a fall in approximately 50% of patients, traffic accident in 30%, and stab wounds/cut wounds/impalement in 2%; only 34 wounds were due to firearm injury, accounting for less than 0.1% of the total.5 Overall, there is a very low incidence of penetrating trauma in Japan.
Most of the physicians and nurses who participated in the present study worked in the emergency department. As most emergency patients in Japan have non-traumatic etiologies, these healthcare professionals have rarely seen patients with persistent bleeding due to acute injury. In contrast, cardiopulmonary resuscitation is performed on a daily basis; therefore, if Japanese healthcare professionals encountered a patient who had collapsed, they might start cardiopulmonary resuscitation regardless of the presence of bleeding.
Japanese medical students receive very thorough basic life support education and training. Basic life support courses are widely spread not only to Japanese healthcare professionals but also to the general public, and police officers and security guards have basic life support knowledge. Japanese EMTs are trained in the use of tourniquets as a pre-hospital treatment. As EMTs are trained on a daily basis, the rate of correct answers to Q4 and Q5 was higher for EMTs than for other types of participants. However, a textbook used by Japanese EMTs states that tourniquets should be loosened every 30 min to prevent lower limb ischemia.11 This differs from the protocol taught in the bleeding control basic training course, which states that tourniquets should not be loosened until arrival at the hospital. Therefore, this difference was specifically explained in the lecture.
The confusion in the prioritization of treatments for bleeding patients, even for healthcare professionals, may be because Japanese healthcare providers have little experience with acute bleeding. Knowledge about the appropriate prioritization of treatments did not improve even after the present participants attended the bleeding control basic training course, which suggests that it is very difficult for physicians and nurses to change their habitual practice style. In future, the bleeding control basic training course for Japanese participants must emphasize that hemostasis should be prioritized above all other treatments.
The main limitation of the present study was the heterogeneous group of participants. Most participants were medical professionals, while the bleeding control basic training course was actually developed for the general public. In mass casualty events, police officers and security guards on the scene are more likely to be the first responders than the physicians and nurses who will treat the victims after arrival at the hospital. If the STB information is not disseminated to the general public, the victims may not be saved at the scene. In the US, a National STB Day held to disseminate the STB program to the general public achieved great success in enhancing the knowledge of STB activities.12 This type of activity will need to include not only healthcare professionals but also the general public in Japan. In addition, as Japan has little experience with acute bleeding, the teaching method must emphasize the priority of dealing with bleeding.
Another study limitation was that the pre-training and post-training tests each comprised only five questions. Because of the course time schedule, the time for the pre-training and post-training tests could not be extended, and so the number of questions was limited. To analyze the difference between pre-training and post-training test scores more precisely without affecting the onsite time schedule, it might be beneficial to use online pre-training and post-training tests with more than five questions.
In conclusion, the bleeding control basic training course improved the knowledge of Japanese participants regarding tourniquet application. However, it was less effective in improving knowledge about which actions to prioritize for bleeding patients. This may be because the Japanese participants were well trained in basic life support and therefore expected to start cardiopulmonary resuscitation immediately when encountering patients who had collapsed. The bleeding control basic training course is a valuable way to prepare Japanese people for potential mass casualty events during the Tokyo Olympic/Paralympic Games in 2021.
Acknowledgments
The authors would like to thank Kazuhide Matsushima, MD, FACS (Department of Surgery, University of Southern California, USA), for his support of the Stop the Bleed activities in Japan.
Footnotes
Presented at: This study was presented at the 49th Critical Care Congress in Orlando, FL on February 18, 2020.
Contributors: Conception and design: KI. Acquisition of data: KI, KM, KH, MY, NK. Analysis and interpretation of data: KI. Drafting of the manuscript: KI. Critical revision of the manuscript: KM, TT, TN, AT, KH, MY, NK, YM, TS. Statistical expertise: KI. Supervision: YM, TS.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the Institutional Review Board of Teikyo University, Tokyo, Japan (approval no. TUIC-COI 19-264).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Joint Committee to Create a National Policy to Enhance Survivability from Mass Casualty Shooting Events Improving survival from active shooter events: the Hartford consensus. J Trauma Acute Care Surg 2013;74:1399–400. 10.1097/TA.0b013e318296b237 [DOI] [PubMed] [Google Scholar]
- 2.Eastridge BJ, Mabry RL, Seguin P, Cantrell J, Tops T, Uribe P, Mallett O, Zubko T, Oetjen-Gerdes L, Rasmussen TE, et al. Death on the battlefield (2001–2011): implications for the future of combat casualty care. J Trauma Acute Care Surg 2012;73:S431–7. 10.1097/TA.0b013e3182755dcc [DOI] [PubMed] [Google Scholar]
- 3.Butler FK. Two decades of saving lives on the battlefield: tactical combat casualty care turns 20. Mil Med 2017;182:e1563–8. 10.7205/MILMED-D-16-00214 [DOI] [PubMed] [Google Scholar]
- 4.Stop the Bleed Stop the Bleed: home. https://www.stopthebleed.org (30 Mar 2020).
- 5.Trauma Registry Committee Japan Trauma Data Bank Report, 2018. [Google Scholar]
- 6.Endo A, Shiraishi A, Matsui H, Hondo K, Otomo Y. Assessment of progress in early trauma care in Japan over the past decade: achievements and areas for future improvement. J Am Coll Surg 2017;224:191–8. 10.1016/j.jamcollsurg.2016.10.051 [DOI] [PubMed] [Google Scholar]
- 7.Pasley AM, Parker BM, Levy MJ, Christiani A, Dubose J, Brenner ML, Scalea T, Pasley JD. Stop the Bleed: does the training work one month out? Am Surg 2018;84:1635–8. 10.1177/000313481808401020 [DOI] [PubMed] [Google Scholar]
- 8.Ross EM, Redman TT, Mapp JG, Brown DJ, Tanaka K, Cooley CW, Kharod CU, Wampler DA. Stop the Bleed: the effect of hemorrhage control education on laypersons' willingness to respond during a traumatic medical emergency. Prehosp Disaster Med 2018;33:127–32. 10.1017/S1049023X18000055 [DOI] [PubMed] [Google Scholar]
- 9.Weinman S. Retention of tourniquet application skills following participation in a bleeding control course. J Emerg Nurs 2020;46:154–62. 10.1016/j.jen.2019.10.020 [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Internal Affairs and Communications Japanese Ministry of Internal Affairs and Communications Report, 2017. [Google Scholar]
- 11.Yamamoto Y. How to stop hemostasis. Tokyo, Japan: Pason Shobou, 2019. [Google Scholar]
- 12.Fisher AD, Carius BM, Lacroix J, Dodge PM, Dodd J, Soderlund E, Thompson D, Loos P, Fannin J, Montgomery HR, et al. National Stop the Bleed Day: the impact of a social media campaign on the Stop the Bleed program. J Trauma Acute Care Surg 2019;87:S40–3. 10.1097/TA.0000000000002341 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2020-000490supp001.pdf (48.9KB, pdf)