Abstract
Background: Different surgical procedures are available for transgender women wishing to undergo genital gender-affirming surgery.
Aim: To assess preoperative motivations, the frequency of orchiectomy procedures, and postoperative outcomes of orchiectomy in transgender individuals.
Methods: All transgender individuals who underwent orchiectomy in the period between January 2012 and January 2020 at our institution were retrospectively identified. A chart study was conducted, recording motivations, demographics, perioperative characteristics and surgical outcomes. The frequency of orchiectomy and vaginoplasty procedures during the study period were determined and compared.
Results: During the study period, an increase of performed orchiectomy procedures was observed. The orchiectomy/vaginoplasty ratio was 0.01–0.07 in the period 2012–2018 and 0.24 in 2019. A total of 43 transgender individuals were retrospectively identified. Sixteen (37%) initially wished to undergo a vaginoplasty, but did not meet institutional requirements (nonsmoker, BMI < 30kg/m2) or were not eligible for vaginoplasty surgery because of interfering somatic or mental health issues. Fourteen (33%) individuals who underwent orchiectomy regarded it as a preceding step to a future vaginoplasty procedure. Out of these fourteen, one person is now on the waiting list for vaginoplasty surgery. Thirteen (30%) others did not report a desire to pursue vaginoplasty in the future. This was mostly motivated by the absence of genital dysphoria or motivations related to their gender identity, with a desire to discontinue anti-testosterone treatment. The postoperative course was uncomplicated in 39 (91%) individuals.
Conclusion: In the Netherlands, especially in the last year, the frequency of orchiectomy procedures has increased. Reasons that people chose to undergo this procedure include: not being eligible for a vaginoplasty procedure, seeing it as a preceding step to a possible future vaginoplasty or other identity-related motivations (i.e., non-binary gender identification or absence of genital dysphoria).
Keywords: Gender affirming surgery, gender dysphoria, orchiectomy, sex reassignment procedures, surgery, transgender
Introduction
Over the last several years, there has been an increase in the number of people with gender dysphoria seeking medical and surgical care (Arcelus et al., 2015; Wiepjes et al., 2018). Most transgender individuals who undergo feminizing genital surgery opt for vaginoplasty, which is a combination of penectomy, orchiectomy, urethral shortening, vulvoplasty, and vaginoplasty. This procedure offers the advantages of providing female external genitalia and being able to engage in neovaginal penetrative sexual intercourse. After surgery, a higher quality of life is reported (Buncamper et al., 2015; Lawrence, 2006; Manrique et al., 2018; Papadopulos et al., 2017). There are several surgical techniques available for this purpose and different grafts can be used as a neovaginal lining, such as inverted penile skin flaps, scrotal flaps, skin grafts, pedicled intestinal segments, or peritoneum (Horbach et al., 2015). The surgical gold standard is penile inversion vaginoplasty (Buncamper et al., 2016). However, not all transgender individuals opt for vaginoplasty surgery as genital Gender Affirmative Surgery (gGAS).
Historically, orchiectomy was frequently performed in transgender women as a first step in the transition process or just because of the relative simplicity of the procedure that can be performed by a broad range of surgical caregivers. In recent years, an increase in transgender women opting for orchiectomy as gGAS was observed in our institution. In the current study, we aim to understand the medical reasons and possible underlying motives of transgender individuals in our clinic to opt for orchiectomy, and what the postoperative course is after this form of gGAS.
Materials and methods
Preoperative counseling
The following is the counseling protocol at our institution: prior to surgery, transgender individuals are screened by psychologists and a plastic surgeon or urologist with experience in transgender health. Psychological screening is performed with respect to the WPATH standard of care, meaning that individuals undergoing genital surgery (1) have persistent, well-documented gender dysphoria; (2) are able to make a fully informed decision and to give consent for treatment; (3) are at least 18 years old; (4) have, if present, controlled medical or mental health problems; and (5) at least 12 continuous months of hormone therapy (Coleman et al., 2012). During preoperative surgical counseling, expectations, (dis)advantages and risks are discussed and informed consent is obtained. Physical examination is performed to check the presence and position of the testicles, testicular abnormalities, possible scarring of the operative area, and presence of inguinal hernias and/or hydroceles.
Surgical technique and considerations
Preoperative antibiotics are generally deemed unnecessary as prophylaxis for this procedure. Under general anesthesia or spinal anesthesia, individuals are placed in the lithotomy position. The surgical area is cleaned with an antiseptic solution and sterile draping is performed. The incision pattern can vary between surgeons, but the place of the incision/scar should not hinder a possible future vaginoplasty procedure (Washington et al., 2017). Therefore, physicians performing orchiectomy in transgender individuals should be aware of possible penoscrotal or penile inversion vaginoplasty techniques. Especially in those who view orchiectomy as a preceding step to a future vaginoplasty procedure, scrotal skin and fatty tissue should not be excised. However, in those who do not wish future vaginoplasty, these tissues may be trimmed according to the individual wish or desire. A scrotal midline incision is performed and the tunica dartos is opened in the midline. Subsequently, per testicle, the tunica albuginea is opened and dissection is performed along the spermatic cord until the external inguinal ring. Again, there is a check for manifest inguinal hernias. After they are transfixed, testicles and spermatic cords are subsequently removed. Specimens are sent for histopathological examination (Matoso et al., 2018). Meticulous hemostasis is achieved diathermically. Subsequently, the wound is closed in layers with resorbable sutures.
Retrospective chart review
For gGAS in transgender individuals, the procedures that are performed in our center comprise: penile inversion vaginoplasty, penoscrotal vaginoplasty, skin graft vaginoplasty, scrotal flap vaginoplasty, (laparoscopic) sigmoid, or ileal vaginoplasty, orchiectomy and no-depth vaginoplasty/gender-confirming vulvoplasty. Our hospital is the only institution in The Netherlands that provides a broad (surgical) pallet of transgender healthcare. A prospectively maintained institutional database, in which all genital surgical procedures in transgender individuals are registered, was used to determine the frequency of orchiectomy from January 2012 until January 2020. This was compared to the frequency of performed vaginoplasty procedures in the same period. All individuals with gender dysphoria who underwent orchiectomy in the period from January 2012 until January 2020 were identified from the same database. A retrospective chart study was conducted, recording demographics (age at surgery, Body Mass Index (BMI), history of smoking, history of drug abuse, previous puberty-blocking hormone use, somatic and psychiatric co-existing morbidities, self-reported sexual orientation), individual motivations to undergo this surgery, surgical outcomes (perioperative characteristics) and genital surgical revisions. Postoperative complications were graded using the Clavien-Dindo Classification (Clavien et al., 2009). Underlying motives for orchiectomy are meticulously documented by both psychologist and gender surgeon. Self-reported motivations to undergo orchiectomy were extracted from the psychological and medical chart. Though multiple motivations may play a role in the decision-process for orchiectomy, the chart information provided us with information on primary motives important to the individual.
Statistical analyses
Descriptive statistics used to describe the data were calculated using SPSS v26.0 (IBM Corporation, 2019). Gaussian continuous variables were presented as means with standard deviations, non-Gaussian continuous variables are medians with ranges. Categorical variables were presented as frequencies and percentages. Mann-Whitney U and Chi-square tests were used to compare demographic characteristics between individuals who underwent orchiectomy in 2019 and those who underwent this before 2019.
Ethical considerations
All included individuals provided written informed consent for use of their data in the database and this study. Our institutional Medical Ethical Review Board approved this study and the study protocol (reference number 2014322). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Results
Demographics
A total of 43 transgender individuals were retrospectively identified, who underwent orchiectomy in the period from January 2012 until January 2020. Forty-one participants (95%) underwent the procedure under general anesthesia, and two (5%) under spinal anesthesia. Demographics of the identified group are shown in Table 1.
Table 1.
Demographics of transgender individuals who underwent orchiectomy.
| All included individuals (n = 43) | Surgery between 2012–2018 (n = 21) | Surgery in 2019 (n = 22) | P-value | |
|---|---|---|---|---|
| Age, median (range) | 31 (18-74) | 35 (18-69) | 30 (19-74) | NS* |
| BMI, median (range) | 24.6 (18.7-44.0) | 23.9 (19.1-44.0) | 26.6 (18.7-41.0) | NS* |
| History of smoking or current smoker, n (%) | 14 (33%) | 8 (38%) | 6 (27%) | NS** |
| History of use of puberty blockers, n (%) | 3 (7%) | 3 (14%) | 0 | NS** |
| Sexually attracted to (self-reported) | NS** | |||
|
14 (33%) | 4 (19%) | 10 (45%) | |
|
11 (26%) | 6 (29%) | 5 (23%) | |
|
8 (19%) | 4 (19%) | 4 (18%) | |
|
2 (5%) | 1 (5%) | 1 (5%) | |
|
3 (7%) | 2 (10%) | 1 (5%) | |
|
5 (12%) | 4 (19%) | 1 (5%) | |
| Somatic comorbidity | ||||
|
2 (5%) | 1 (5%) | 1 (5%) | NS** |
|
1 (2%) | 1 (5%) | 0 | NS** |
|
2 (5%) | 0 | 2 (9%) | NS** |
| Co-existing mental health issues | ||||
|
9 (21%) | 3 (14%) | 6 (27%) | NS** |
|
10 (23%) | 6 (29%) | 4 (18%) | NS** |
|
2 (5%) | 2 (10%) | 0 | NS** |
|
1 (2%) | 0 | 1 (5%) | NS** |
|
1 (2%) | 1 (5%) | 0 | NS** |
|
1 (2%) | 0 | 1 (5%) | NS** |
BMI Body Mass Index, NS Not significant.
* Mann-Whitney U test, ** Chi-square test.
Incidence
During the study period, an absolute increase in the number of orchiectomy procedures was observed, especially in the last year. In 2012, one orchiectomy was performed. In 2019, this number increased to 22 (see Figure 1.). When compared to the performed vaginoplasty procedures in the same time period, a relative increase of this procedure was also observed. The orchiectomy/vaginoplasty ratio was 0.01–0.07 in the period 2012–2018 and 0.24 in 2019. The increase could not be exclusively explained by the increase of treated transgender individuals in our center. No statistically significant demographic differences were observed between individuals who underwent orchiectomy in 2019 and those who underwent this before 2019 (Table 1.).
Figure 1.
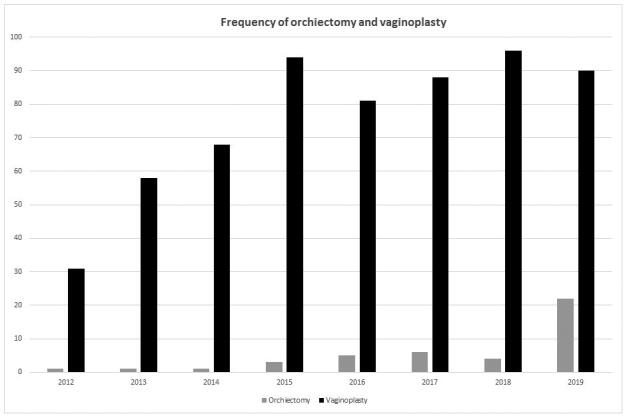
Frequency of orchiectomy and vaginoplasty over the years 2012–2019.
Reasons to undergo orchiectomy
An overview of self-reported motivations to undergo orchiectomy is presented in Table 2. Of all participants who underwent orchiectomy, 16 (37%) actually desired to undergo vaginoplasty, but were not eligible for surgery due to the fact that they did (1) not meet institutional requirements, such as BMI and being a nonsmoker, or (2) were not eligible for vaginoplasty surgery, because of extensive co-existing somatic or mental health issues. Fourteen (33%) persons who underwent orchiectomy thought of it as a preceding step to a future vaginoplasty procedure. A total of 13 (30%) did not opt for a vaginoplasty in the future and were mostly motivated by the absence of genital dysphoria or motivations related to their gender identity or wanted to stop using the anti-testosterone treatment. No statistically significant differences were observed in self-reported motivations to undergo orchiectomy between individuals who underwent orchiectomy in 2019 and those who underwent this before 2019.
Table 2.
Individual reasons to undergo orchiectomy.
| Reasons to undergo orchiectomy | Number of persons (%) |
|---|---|
| Individuals who desired but not eligible for vaginoplasty | 16 (37%) |
| Did not meet institutional requirements for vaginoplasty | 11 (26%) |
|
5 (12%) |
|
4 (9%) |
|
2 (5%) |
| Not eligible for vaginoplasty due to somatic comorbidity | 4 (9%) |
| Severe respiratory problems | 1 (2%) |
| Severe diabetic dysregulation | 1 (2%) |
| Severe cardiac comorbidity | 2 (5%) |
| Not eligible for vaginoplasty due to psychiatric comorbidity | 1 (2%) |
| Severe intellectual disability | 1 (2%) |
| Orchiectomy as a preceding step to a (possible) vaginoplasty | 14 (33%) |
| Wants vaginoplasty later, but does not fit in schedule now | 7 (16%) |
| Is doubting future vaginoplasty, but wants to stop anti-testosterone treatment | 4 (9%) |
| Wants vaginoplasty later abroad | 1 (2%) |
| Wants peritoneal vaginoplasty later (not offered currently in our center) | 1 (2%) |
| Fear of surgery, wants to try minor surgery before major surgery | 1 (2%) |
| Individuals who do not wish vaginoplasty | 13 (30%) |
| No genital dysphoria, but wish to stop using anti-testosterone hormones | 8 (19%) |
| Fear of complications of vaginoplasty | 1 (2%) |
| Vaginoplasty too invasive surgery | 2 (5%) |
| Non-binary gender identity | 1 (2%) |
| Vaginoplasty too much to handle for partner | 1 (2%) |
Surgical outcomes and reoperations
The median postoperative clinical follow-up time was 7.6 months (range 0.4–77.6) months). The postoperative course was uncomplicated in 39 (91%) people. In three individuals a scrotal abscess developed, which was incised and drained under general anesthesia in one patient (Clavien-Dindo grade 3b complication) and under local anesthesia in the other two patients (Clavien-Dindo grade 3a complication). In one patient, superficial surgical site infections treated with oral antibiotics (Clavien-Dindo grade 2 complication). In those who underwent orchiectomy as a preceding step to vaginoplasty, one individual who had quit smoking is now on the waiting list for vaginoplasty surgery. All resected testicles were sent for histopathological examination; no malignancies were found.
Discussion
In this study, the motivations, orchiectomy frequency over the years, and postoperative outcomes of orchiectomy in transgender individuals were described. Orchiectomy is a surgical procedure has been long available for transgender individuals. It causes infertility, decreased sex drive, breast enlargement (in combination with hormonal treatment) and decreased testicular dysphoria. After surgery, individuals can stop using anti-testosterone treatment. It is a simple procedure: easy to perform, not very time-consuming and the postoperative recovery period is short.
Historically, in our center, orchiectomy was not a commonly requested procedure. In recent years, an absolute increase in performed orchiectomy procedures was observed, with a 4 to 5 fold increase in 2019. The exact reason for this is unknown. The increase could not be exclusively explained by the increase of treated transgender individuals in our center (see Figure 1.). One possible reason is that there has been an increase of surgical options for genital surgery and each surgical option is discussed extensively during preoperative counseling. Preoperative psychological and surgical counseling is focused on individual preferences and shared decision making is deemed very important. Where in earlier years, transgender individuals were only offered vaginoplasty surgery as gGAS, which one can call a binary surgical approach, they now have multiple choices, such as non-depth vaginoplasty/vulvoplasty and orchiectomy alone. In our center, institutional requirements for vaginoplasty, besides those established by WPATH (Coleman et al., 2012), comprise of a BMI < 30 and being a nonsmoker. Those are treated as strict selection criteria for surgical eligibility. We oblige people to refrain from smoking 6 weeks before surgery and urinary nicotine concentration is determined at the outpatient clinic. In this study 11 (26%) individuals underwent orchiectomy because they did not meet institutional requirements. It may well be that these people would face a different surgical course in the future, as having a high BMI is currently being debated as being a risk factor for vaginoplasty surgery complications (Ives et al., 2019).
Strengths of this study comprise that it is from a center with a high-volume of transgender surgery procedures, which is the only one of its kind in the country, which makes it ideal as a marker for surgical trends. Another strength is that it focuses on a subgroup of transgender individuals undergoing a specific type of genital surgery about which little is known. Limitations of this study comprise mainly of the retrospective nature and a relatively small sample of patients.
In conclusion, in this study regarding the role of orchiectomy in transgender health care, findings show that orchiectomy is an important surgical option for a subset of transgender individuals and increasingly performed in The Netherlands. Motives to opt and refer for this intervention show to be variable. Some individuals opt for this procedure because they are not eligible for a vaginoplasty procedure, whilst others choose it as a preceding step to a future vaginoplasty. There also seems to be a specific group who do not desire a vaginoplasty based on the absence of genital dysphoria and/or motivations related to their gender identity. The postoperative course is uncomplicated in most.
Disclosure statement
The authors have no conflicts of interest to declare. There are no commercial or financial conflicts of interest to report. No funding was received for the work.
References
- Arcelus, J., Bouman, W. P., Van Den Noortgate, W., Claes, L., Witcomb, G., & Fernandez-Aranda, F. (2015). Systematic review and meta-analysis of prevalence studies in transsexualism. European Psychiatry, 30(6), 807–815. doi: 10.1016/j.eurpsy.2015.04.005 [DOI] [PubMed] [Google Scholar]
- Buncamper, M. E., Honselaar, J. S., Bouman, M. B., Özer, M., Kreukels, B. P., & Mullender, M. G. (2015). Aesthetic and functional outcomes of neovaginoplasty using penile skin in male-to-female transsexuals. The Journal of Sexual Medicine, 12(7), 1626–1634. doi: 10.1111/jsm.12914 [DOI] [PubMed] [Google Scholar]
- Buncamper, M. E., van der Sluis, W. B., van der Pas, R. S. D., Özer, M., Smit, J. M., Witte, B. I., Bouman, M.-B., & Mullender, M. G. (2016). Surgical outcome after penile inversion vaginoplasty: A retrospective study of 475 transgender women. Plastic and Reconstructive Surgery, 138(5), 999–1007. doi: 10.1097/PRS.0000000000002684 [DOI] [PubMed] [Google Scholar]
- Clavien, P. A., Barkun, J., de Oliveira, M. L., Vauthey, J. N., Dindo, D., Schulick, R. D., de Santibañes, E., Pekolj, J., Slankamenac, K., Bassi, C., Graf, R., Vonlanthen, R., Padbury, R., Cameron, J. L., & Makuuchi, M. (2009). The Clavien-Dindo classification of surgical complications. Annals of Surgery, 250(2), 187–196. doi: 10.1097/SLA.0b013e3181b13ca2 [DOI] [PubMed] [Google Scholar]
- Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., DeCuypere, G., Feldman, J., Fraser, L., Green, J., Knudson, G., Meyer, W. J., Monstrey, S., Adler, R. K., Brown, G. R., Devor, A. H., Ehrbar, R., Ettner, R., Eyler, E., Garofalo, R., Karasic, D. H., … Zucker, K. (2012). Standards of care for the health of transsexual, transgender, and gender nonconforming people, version 7. International Journal of Transgenderism, 13(4), 165–232. doi: 10.1080/15532739.2011.700873 [DOI] [Google Scholar]
- Horbach, S. E., Bouman, M. B., Smit, J. M., Özer, M., Buncamper, M. E., & Mullender, M. G. (2015). Outcome of vaginoplasty in male-to-female transgenders: A systematic review of surgical techniques. The Journal of Sexual Medicine, 12(6), 1499–1512. doi: 10.1111/jsm.12868 [DOI] [PubMed] [Google Scholar]
- IBM Corporation. (2019). IBM SPSS statistics for Windows, version 26.0. IBM. [Google Scholar]
- Ives, G. C., Fein, L. A., Finch, L., Sluiter, E. C., Lane, M., Kuzon, W. M., & Salgado, C. J. (2019). Evaluation of BMI as a risk factor for complications following gender-affirming penile inversion vaginoplasty. Plastic and Reconstructive Surgery Global Open, 7(3), e2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence, A. A. (2006). Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Archives of Sexual Behavior, 35(6), 717–727. doi: 10.1007/s10508-006-9104-9 [DOI] [PubMed] [Google Scholar]
- Manrique, O. J., Adabi, K., Martinez-Jorge, J., Ciudad, P., Nicoli, F., & Kiranantawat, K. (2018). Complications and patient-reported outcomes in male-to-female vaginoplasty - where we are today: A systematic review and meta-analysis. Annals of Plastic Surgery, 80(6), 684–691. doi: 10.1097/SAP.0000000000001393 [DOI] [PubMed] [Google Scholar]
- Matoso, A., Khandakar, B., Yuan, S., Wu, T., Wang, L. J., Lombardo, K. A., Mangray, S., Mannan, A. A. S. R., & Yakirevich, E. (2018). Spectrum of findings in orchiectomy specimens of persons undergoing gender confirmation surgery. Human Pathology, 76(), 91–99. doi: 10.1016/j.humpath.2018.03.007 [DOI] [PubMed] [Google Scholar]
- Papadopulos, N. A., Lellé, J.-D., Zavlin, D., Herschbach, P., Henrich, G., Kovacs, L., Ehrenberger, B., Kluger, A.-K., Machens, H.-G., & Schaff, J. (2017). Quality of life and patient satisfaction following male-to-female sex reassignment surgery. The Journal of Sexual Medicine, 14(5), 721–730. doi: 10.1016/j.jsxm.2017.01.022 [DOI] [PubMed] [Google Scholar]
- Washington, S., Bayne, D., Butler, C., & Garcia, M. (2017). Bilateral orchiectomy for transgender patients: an efficient surgical technique that anticipates future vaginoplasty and is associated with minimal morbidity. The Journal of Sexual Medicine, 14(2), e91–e92. doi: 10.1016/j.jsxm.2016.12.203 [DOI] [Google Scholar]
- Wiepjes, C. M., Nota, N. M., de Blok, C. J. M., Klaver, M., de Vries, A. L. C., Wensing-Kruger, S. A., de Jongh, R. T., Bouman, M.-B., Steensma, T. D., Cohen-Kettenis, P., Gooren, L. J. G., Kreukels, B. P. C., & den Heijer, M. (2018). The Amsterdam Cohort of Gender Dysphoria Study (1972–2015). Trends in prevalence, treatment, and regrets. Journal of Sexual Medicine, 15(4), 582–590. doi: 10.1016/j.jsxm.2018.01.016 [DOI] [PubMed] [Google Scholar]


